Abstract
Pericardial effusion is a common finding in everyday clinical practice. The first challenge to the clinician is to try to establish an etiologic diagnosis. Sometimes, the pericardial effusion can be easily related to a known underlying disease, such as acute myocardial infarction, cardiac surgery, end-stage renal disease or widespread metastatic neoplasm. When no obvious cause is apparent, some clinical findings can be useful to establish a diagnosis of probability. The presence of acute inflammatory signs (chest pain, fever, pericardial friction rub) is predictive for acute idiopathic pericarditis irrespective of the size of the effusion or the presence or absence of tamponade. Severe effusion with absence of inflammatory signs and absence of tamponade is predictive for chronic idiopathic pericardial effusion, and tamponade without inflammatory signs for neoplastic pericardial effusion. Epidemiologic considerations are very important, as in developed countries acute idiopathic pericarditis and idiopathic pericardial effusion are the most common etiologies, but in some underdeveloped geographic areas tuberculous pericarditis is the leading cause of pericardial effusion. The second point is the evaluation of the hemodynamic compromise caused by pericardial fluid. Cardiac tamponade is not an “all or none” phenomenon, but a syndrome with a continuum of severity ranging from an asymptomatic elevation of intrapericardial pressure detectable only through hemodynamic methods to a clinical tamponade recognized by the presence of dyspnea, tachycardia, jugular venous distension, pulsus paradoxus and in the more severe cases arterial hypotension and shock. In the middle, echocardiographic tamponade is recognized by the presence of cardiac chamber collapses and characteristic alterations in respiratory variations of mitral and tricuspid flow. Medical treatment of pericardial effusion is mainly dictated by the presence of inflammatory signs and by the underlying disease if present. Pericardial drainage is mandatory when clinical tamponade is present. In the absence of clinical tamponade, examination of the pericardial fluid is indicated when there is a clinical suspicion of purulent pericarditis and in patients with underlying neoplasia. Patients with chronic massive idiopathic pericardial effusion should also be submitted to pericardial drainage because of the risk of developing unexpected tamponade. The selection of the pericardial drainage procedure depends on the etiology of the effusion. Simple pericardiocentesis is usually sufficient in patients with acute idiopathic or viral pericarditis. Purulent pericarditis should be drained surgically, usually through subxiphoid pericardiotomy. Neoplastic pericardial effusion constitutes a more difficult challenge because reaccumulation of pericardial fluid is a concern. The therapeutic possibilities include extended indwelling pericardial catheter, percutaneous pericardiostomy and intrapericardial instillation of antineoplastic and sclerosing agents. Massive chronic idiopathic pericardial effusions do not respond to medical treatment and tend to recur after pericardiocentesis, so wide anterior pericardiectomy is finally necessary in many cases.
Keywords: Pericardial effusion, Etiology, Diagnosis, Therapy
INTRODUCTION
Pericardial effusion is a relatively common finding in everyday clinical practice. Sometimes the clinical picture of the patient leads directly to the search for pericardial effusion, as occurs in patients with chest pain of pericarditic characteristics or in patients with underlying diseases that can cause pericardial involvement (renal failure, chest irradiation) and thoracic complaints. Other patients, without previous known diseases, seek medical attention because of dyspnea or nonspecific chest discomfort and the thoracic X-ray shows the presence of an enlarged cardiac silhouette with clear lungs. Finally, an unexpected cardiomegaly can be fortuitously found in asymptomatic patients during routine medical control for job or insurance purposes or for unrelated complaints. In any case, the finding of cardiomegaly with clear lungs should raise the suspicion of a pericardial effusion. The echocardiogram is the most available and reliable technique in order to verify the presence and the amount of a pericardial effusion; in addition, the echocardiogram offers valuable data for evaluation of hemodynamic repercussion. Mild pericardial effusion (sum of echo-free spaces in the anterior and posterior pericardial sac of less than 10 mm) is a relatively frequent finding, especially in elderly women[1]. In fact, this finding does not always correspond to true effusion, but to pericardial fat. In these cases, computed tomography (CT) is a reliable method to precisely identify the nature of this echocardiographic finding[2].
Although echocardiography is the standard and most available method for the evaluation of pericardial effusion, CT[2] and magnetic resonance imaging (MRI) can offer some advantages. These imaging techniques allow assessment of the entire chest and detection of associated abnormalities in the mediastinum, lungs and adjacent structures. CT and MRI are also less operator dependent and delineate more precisely the spacial distribution of pericardial effusion in complex pericardial collections. In addition, multidetector CT scanners and MRI may provide valuable information about the function and dynamics of the heart and pericardium. Some of the reported limitations of echocardiography are generally not present with CT, including the possibility of false-positive findings due to adjacent pathologic conditions that may simulate pericardial effusion. Another advantage of CT and MRI is the possibility of identifying hemorrhagic effusions or clots within the pericardium.
The aim of this article is to give a comprehensive review of the etiology, hemodynamic repercussion, and management of moderate (sum of echo-free spaces in anterior and posterior pericardial sac between 10 and 20 mm) and severe (more than 20 mm) pericardial effusion.
CLINICAL APPROACH TO ETIOLOGIC DIAGNOSIS
When a clinician is faced with a patient who presents with a pericardial effusion, the first challenge is to identify its etiology. In some instances, it can be easily related to an associated condition or medical procedure (Table 1). This happens, for example, in patients who develop pericardial effusion in the course of acute myocardial infarction[3,4], in patients with end-stage renal failure, in patients receiving chest radiation, or in patients recently submitted to an invasive cardiac procedure with endocavitary catheters. However, even in these contexts, the possibility of unrelated etiologies should be considered. The finding of a pericardial effusion in patients with underlying malignancy creates a more complex dilemma, as not infrequently pericardial effusion is due to alternative causes and not to direct neoplastic pericardial involvement. In Posner’s series[5] malignant pericardial disease was diagnosed in 18 (58%) of 31 patients with underlying cancer and pericarditis, while 32% of the patients had idiopathic pericarditis and 10% had radiation induced pericarditis. Porte et al[6] studied 114 patients with recent or remote history of cancer and a pericardial effusion of unknown origin requiring drainage for diagnostic or therapeutic purposes. Pericardioscopy was performed in 112 patients with pericardial fluid analysis and biopsy of abnormal structures or deposits under direct visual control. Malignant pericardial disease was found in 44 (38%) patients, while 70 (61%) patients had non-malignant pericardial effusions (idiopathic in 33 patients, radiation-induced in 20 patients, infectious effusion in 10 patients, and hemopericardium as a result of coagulation disorders in 8 patients). These studies are important since they show that, in more than half of the patients with underlying cancer, a pericardial effusion is due to causes different than direct neoplastic involvement. Therefore, the precise etiology of these effusions needs to be clarified, as obvious prognostic and therapeutic consequences ensue. Pericardioscopy may be helpful in selected cases[7,8]. Imaging techniques such as CT, MRI and positron emission tomography may also be very useful in the investigation of the presence and extension of neoplastic disease.
Table 1.
Causes of pericardial effusion
| Secondary to underlying known disease |
| Acute myocardial infarction |
| Cardiac surgery |
| Trauma |
| Widespread known neoplasia |
| Chest radiation |
| End-stage renal failure |
| Invasive cardiac procedures |
| Hypothyroidism |
| Autoimmune diseases |
| Without underlying known disease |
| Acute inflammatory pericarditis (infectious, autoimmune) |
| Previously unknown neoplasia |
| Idiopathic |
In many patients the etiology is initially difficult to establish as no apparent cause is present at the time a pericardial effusion is first identified. Although the final diagnosis of the cause of a pericardial effusion should be based on specific data, some simple clinical indicators may be useful in suggesting a likely etiologic category. Agner et al[9], in a retrospective series of 133 patients, observed that hemodynamic compromise, cardiomegaly, pleural effusion, and a large pericardial effusion were more common in patients with tuberculous or malignant pericardial disease than in patients with idiopathic pericarditis. Hemorrhagic pericardial effusion has been associated with neoplasia in some studies[10], but hemorrhagic effusions can also be seen in patients with idiopathic pericarditis. In fact, the predictive value of these different clinical findings for assessing the etiology of pericardial effusions has not been established. We hypothesized that some simple clinical findings such as the presence of underlying disease, development of cardiac tamponade, and presence or absence of inflammatory signs (typical pericarditic chest pain, fever, pericardial friction rub), might be helpful in classifying the patients into a major etiologic diagnostic category. We prospectively studied 322 patients with moderate and severe pericardial effusion[11]. In 60% of these patients a known previous condition that could cause pericardial effusion was present. The pericardial effusion was demonstrated to be related to the underlying disease in all but 7 of these patients. In the patients with no apparent cause of pericardial effusion at the time of diagnosis (40%) we found that the presence of inflammatory signs (characteristic chest pain, pericardial friction rub, fever or typical electrocardiographic changes) was predictive for acute idiopathic pericarditis (P < 0.001, likelihood ratio 5.4), irrespective of the size of the effusion and the presence or absence of tamponade. Furthermore, severe effusion with absence of inflammatory signs and absence of tamponade was predictive for chronic idiopathic pericardial effusion (P < 0.001, likelihood ratio 20), and tamponade without inflammatory signs for neoplastic pericardial effusion (P < 0.001, likelihood ratio 2.9). The search for evidence of previous chronic effusion can be particularly helpful, as it may make it possible to distinguish neoplastic disease from chronic idiopathic pericardial effusion, which sometimes presents with tamponade. Therefore, although the final etiologic diagnosis should certainly be based on specific clinical data in individual patients, we think that the data afforded by this study may be helpful in the initial assessment and in the decision to perform invasive pericardial studies. Tuberculous pericarditis deserves special attention. Most patients with acute pericarditis will be finally diagnosed with idiopathic pericarditis, but a few cases will correspond to tuberculous pericarditis. Identification of these cases is important due to obvious therapeutic implications. The diagnosis can be established through general examination, including the search of tubercle bacilli in sputum or gastric aspirate or by means of pericardial fluid or pericardial tissue examination (indicated in patients with tamponade or with persistent active illness for more than 3 wk).
EVALUATION OF HEMODYNAMIC COMPROMISE
Clinical tamponade is the most severe manifestation of hemodynamic compromise caused by a tense pericardial effusion (Figure 1). The picture is easily recognized through the presence of the typical findings of dyspnea, tachycardia, jugular venous distension, pulsus paradoxus, and in the more severe cases arterial hypotension and even shock.
Figure 1.
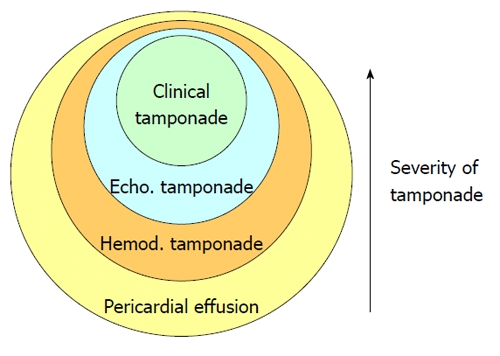
Grading of severity of hemodynamic compromise caused by pericardial effusion. Most pericardial effusions cause abnormalities in hemodynamic parameters as measured in the Cath lab. Some of these patients have echocardiographic findings of tamponade, while only a relative minority of these patients have overt clinical tamponade. Therefore, clinical tamponade represents the highest degree of severity in the spectrum of hemodynamic compromise caused by pericardial effusion. Echo: Echocardiographic; Hemod: Hemodynamic.
Not infrequently the echocardiogram shows findings suggestive of hemodynamic compromise (chamber collapses, characteristic alterations in mitral and tricuspid flows) in patients with moderate and severe pericardial effusion that, on the other hand, do not exhibit any clinical sign of tamponade[12,13]. Cardiologists are puzzled about the clinical relevance of these findings, especially regarding the indication of pericardial drainage. Studies correlating clinical, echocardiographic and catheterization data helped to clarify this problem. For instance, in the study of Mercé et al[14], that included 110 patients with moderate or severe pericardial effusion, 34% of 72 patients without clinical tamponade showed collapse of one or more cardiac chambers. In particular right atrial collapse had a low positive predictive value (52%) for clinical cardiac tamponade, while combined right atrial and right ventricular collapse was more specific (positive predictive value of 74%). However, these patients consistently showed elevation of intrapericardial pressure when submitted to a catheterization study. In the study by Levine et al[15], 50 consecutive medical patients with pericardial effusion associated with diastolic right atrial and/or right ventricular collapse, underwent combined right-sided cardiac catheterization and percutaneous pericardiocentesis. Right atrial collapse was present in 92%, and right ventricular collapse in 57% of patients, respectively. Symptoms that led referring physicians to order the echocardiographic study included dyspnea in 44 patients (83%), pleuritic chest pain in 22 (42%), cough in 5 (9%) and hypotension in 2 patients. At physical examination systolic blood pressure was higher than 100 mmHg in 94% of patients, elevation of the jugular venous pressure was suspected in only 74%, hepatomegaly was present in 28%, and pulsus paradoxus was appreciated in only 36% of patients. In fact, clinical suspicion of tamponade was established in only 50% of the patients. At cardiac catheterization the initial pericardial pressure was elevated in all patients (range 3 to 27 mmHg) and was equal to right atrial pressure (therefore, with hemodynamic criteria of tamponade) in 84% of patients. In comparison with the series of Guberman et al[16], that included patients in which the decision to proceed to invasive drainage of the pericardial space was made on the basis of clinical findings indicative of hemodynamic compromise, the patients in the series of Levine et al[15] had a significantly lower prevalence of hypotension, abnormal pulsus paradoxus, jugular venous pressure elevation and hepatomegaly. All these findings suggest that echocardiography can identify patients with pericardial effusion causing elevation of pericardial pressure before overt hemodynamic embarrassment develops, as the majority of these patients had only mild to moderate clinical tamponade. Even patients with asymptomatic large pericardial effusion without echocardiographic collapses show criteria of hemodynamic tamponade; that is elevation of intrapericardial pressure which equalizes with right atrial pressure and becomes normal after pericardiocentesis together with increase of cardiac output[17]. Experimental[18-21] and clinical studies[22,23] have shown that cardiac tamponade is not an “all-or-none” phenomenon, as previously thought by clinical observation, but a continuum that goes from slight elevations of intrapericardial pressure with subtle hemodynamic repercussion to a situation of severe hemodynamic embarrassment and even death. The concept of continuum was elegantly illustrated by Reddy et al[23] based on hemodynamic observations of 77 patients with pericardial effusion submitted to pericardiocentesis. Patients were classified into 3 groups based on the equilibration of intrapericardial, right atrial and pulmonary arterial wedge pressures. They found that even in patients with an intrapericardial pressure lower than the right atrial pressure, pericardiocentesis produced a significant decrease in intrapericardial pressure, right atrial pressure, pulmonary arterial wedge pressure and the inspiratory decrease in arterial systolic pressure. Obviously, these changes were greater in the patients with higher levels of intrapericardial pressure, but, in any case, illustrate the fact that subtle elevations of intrapericardial pressure have hemodynamic consequences. Reddy et al[23] concluded that the severity of hemodynamic derangement rather than its presence or absence should be assessed in patients with pericardial effusion.
ETIOLOGIC SPECTRUM OF MODERATE AND LARGE PERICARDIAL EFFUSIONS
A wide variety of conditions may result in pericardial effusion (Table 2). All types of acute pericarditis can be associated with pericardial effusion. In a hospital series[24] pericardial effusion was present in 50% of patients with acute idiopathic or viral pericarditis. Pericarditis secondary to immunologic processes such as systemic lupus erythematosus or rheumatoid arthritis, and pericarditis of physical origin (post-radiation, post-traumatic) are frequently accompanied by pericardial effusion. In addition, pericardial effusion of varying amounts can be seen in other conditions such as neoplasia (with or without direct pericardial involvement), myxoedema, renal failure, pregnancy, aortic or cardiac rupture, chylopericardium, or in the setting of chronic sodium and water retention from many causes, including chronic heart failure, nephrotic syndrome and hepatic cirrhosis. The relative prevalence of these etiologies largely depends on the source of the population studied, the relative size and activity of the different departments in a general hospital (especially the number of patients with neoplastic disease or chronic renal insufficiency who attend each hospital), the study protocol applied, and, of course, on the frequency distribution of the different etiologies of pericardial diseases in each geographic area. For instance, in outpatient populations of the western world the most frequent etiologies are probably idiopathic/viral pericarditis and idiopathic pericardial effusion, while in hospital series neoplastic pericarditis, uremic pericarditis and iatrogenic disease are prominent etiologies of pericardial effusion. In developing countries, especially in Subsaharan Africa, tuberculous pericarditis is the leading cause of pericardial effusion[25].
Table 2.
Moderate-large pericardial effusion trials
| Corey et al[26] | Colombo et al[10] | Sagristà-Sauleda et al[11] | Corey et al[27] | |
| Effusion | > 5 mm | > 10 mm | > 10 mm | Not reported |
| n | 57 | 25 | 322 | 106 |
| Tamponade (%) | Not reported | 44 | 37 | Not reported |
| Idiopathic (%) | 7 | 32 | 201 | 25 |
| Chronic idiopathic effusion (%) | ? | ? | 9 | ? |
| Neoplastic (%) | 23 | 36 | 13 | 37 |
| Uremia (%) | 12 | 20 | 6 | 4 |
| Iatrogenic (%) | 0 | 0 | 16 | 0 |
| Post-acute myocardial infarction (%) | 0 | 8 | 8 | 0 |
| Viral (%) | 14 | 0 | 0 | 7 |
| Collagen vascular disease (%) | 12 | 0 | 5 | 5 |
| Tuberculosis (%) | 0 | 0 | 2 | 2 |
| Other (%) | 9 | 4 | 21 | 202 |
Acute idiopathic pericarditis;
Includes 12 patients with bacterial pericardial effusion; ?: No distinction between acute idiopathic pericarditis and idiopathic chronic pericardial effusion.
Four major studies[10,11,26,27] have addressed one of the commonest clinical problems in the setting of pericardial diseases that the cardiologist is faced with: to investigate the etiology of large pericardial effusions of unknown origin. These studies (Table 1) were prospective and were done in general medical centers, but differ in respect to the criteria used to define a pericardial effusion as large, in the number of patients included and, especially, in the study protocol applied to the patients. For instance, Colombo et al[10] consider effusions of > 10 mm by M-mode echocardiography as large, and Corey et al[26] include as large effusions those > 5 mm, while in the series by Sagristà-Sauleda et al[11] moderate effusions were defined as an echo-free space of anterior plus posterior pericardial spaces of 10-20 mm during diastole, and severe effusions as a sum of echo-free spaces > 20 mm. The series by Colombo et al[10] includes 25 male patients all of whom were submitted to an invasive pericardial procedure. Of these patients, 44% presented with cardiac tamponade. The most frequent etiologies of pericardial effusion were: neoplastic (36%), idiopathic (32%), and uremic (20%). Corey et al[26] investigated the etiology of pericardial effusion in 57 patients. The prevalence of cardiac tamponade was not reported. Each patient was assessed by a comprehensive preoperative evaluation followed by subxiphoid pericardiotomy. Microscopic examination of the samples of pericardial fluid and tissue was done and they were also cultured for aerobic and anaerobic bacteria, fungi, mycobacteria, mycoplasma, and viruses. An etiologic diagnosis was made in 53 patients (93%). The most common diagnoses were malignancy (23%), viral infection (14%), radiation–induced inflammation (14%), collagen-vascular disease (12%), and uremia (12%). In only 4 patients no diagnosis was made. However, some of the diagnoses consisted of the isolation by culture of pericardial fluid or tissue of unexpected organisms of doubtful clinical relevance, and this series was probably biased toward the inclusion of immunocompromised patients. The study by Sagristà-Sauleda et al[11] included 322 patients, 132 with moderate and 190 with severe pericardial effusion. Cardiac tamponade was present in 37%. The patients were studied following our own protocol for the management of pericardial diseases[28], in which invasive pericardial procedures were not systematically performed but were only undertaken under precisely defined indications. In this series, the most common diagnosis was acute idiopathic pericarditis which accounted for 20% of patients. The next most prevalent diagnoses were iatrogenic effusion (16%), neoplastic effusion (13%), and chronic idiopathic pericardial effusion (9%).
The study by Levy et al[27], mainly devoted to investigating infectious causes of pericardial effusion, constitutes a paradigmatic example of the possibility of obtaining specific etiologies by using a sophisticated and costly study protocol with systematic use of molecular biology techniques in patients with pericardial effusion accompanying acute pericarditis. These authors investigated 106 pericardial fluid specimens using conventional and molecular methods (PCR) of analysis. A positive etiologic diagnosis of pericardial disease was obtained in 80 of the 106 patients. However, the majority of these diagnoses were obtained with conventional methods commonly used for the assessment of pericardial diseases, either invasive (cytologic examination or culture of effusion) or non-invasive (clinical history, general clinical assessment, serology). In fact, the implementation of the highly complex molecular diagnosis procedure had a net benefit of 4 specific treatments being given in a population of 106 patients.
In addition to the source of the patients and the extension of the study protocol applied, the severity of the hemodynamic repercussion of pericardial effusion has also etiologic implications. In the series of Guberman et al[16], that included patients with clinical cardiac tamponade, the most common etiology was metastatic cancer in 18 patients, followed by idiopathic pericarditis in 8 and uremic in five. In the study by Levine et al[15], that included 50 patients with echocardiographic tamponade (thus of lower degree of severity than Guberman’s series), malignancy was also the most frequent etiology.
MEDICAL TREATMENT
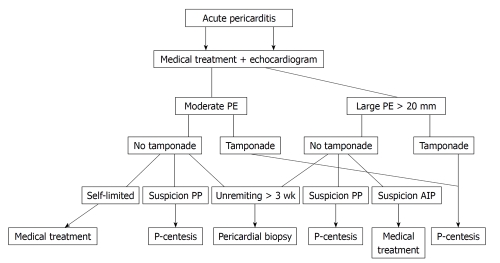
Patients with acute inflammatory signs (fever, chest pain, pericardial friction rub) should receive aspirin or non-steroid anti-inflammatory drugs. In the setting of acute inflammatory pericarditis steroids should be avoided as they increase the possibility of relapses[29,30]. Colchicine is an established indication in patients with relapsing pericarditis[8], and has also been suggested to be useful in the first episode of acute pericarditis in order to avoid the appearance of recurrences[30]. The patients with acute viral or idiopathic pericarditis can be managed on an out-of-hospital basis unless they have clinical predictors of poor prognosis (cardiac tamponade, severe pericardial effusion, immunosuppression, oral anticoagulant therapy or fever > 38°C[31]. The global management of acute pericarditis is shown schematically in Figure 2. When specific etiology is found (bacterial, tuberculous) the treatment should be directed against the causative agent with pericardial drainage if hemodynamic compromise is present. Strict control in the first weeks or months is necessary because of the possibility of evolution to constrictive pericarditis[32,33]. When acute idiopathic or viral pericarditis is accompanied by moderate to severe effusion new echocardiographic controls should be performed (initially every week) until resolution of the disease. The management of neoplastic pericarditis has been excellently reviewed in this Journal recently[34].
Figure 2.
Proposed management strategy for patients with moderate or severe pericardial effusion accompanying acute pericarditis. PE: Pericardial effusion; PP: Purulent pericarditis; AIP: Acute idiopathic pericarditis; P-centesis: Pericardiocentesis.
INDICATIONS FOR PERICARDIAL DRAINAGE PROCEDURES
Pericardial drainage procedures can be performed for diagnostic or therapeutic purposes (patients with cardiac tamponade). In patients without hemodynamic compromise the diagnostic yield of pericardial fluid or pericardial tissue is very low[24]. In a study by our group[35], which included 71 patients with large pericardial effusion without clinical tamponade, we found that pericardial drainage procedures (performed in 26 patients) had a diagnostic yield of only 7%. On the other hand, no patients developed cardiac tamponade or died as a result of pericardial disease, nor did any new diagnosis become apparent in the 45 patients who did not undergo pericardial drainage initially. Furthermore, moderate or large effusions persisted in only 2 of 45 patients managed conservatively. Even patients with echocardiographic collapses rarely require pericardial drainage for therapeutic purposes during the initial admission. Therefore, pericardial drainage procedures are not justified on a routine basis in patients without hemodynamic compromise. Three exceptions to this rule should be noted. Patients with a strong suspicion of purulent or tuberculous pericarditis merit invasive pericardial procedures. On the other hand, in patients with underlying malignancies examination of pericardial fluid is indicated in order to determine whether the effusion is secondary to neoplastic pericardial involvement or is an epiphenomenon (non-malignant effusion) related to the management of the cancer (such as previous thoracic irradiation) or effusions of unknown origin. Lastly, we recommend pericardiocentesis in asymptomatic patients with massive idiopathic chronic pericardial effusion because some of these patients develop unexpected overt tamponade.
SELECTION OF PERICARDIAL DRAINAGE PROCEDURES
A variety of procedures, ranging from simple needle pericardiocentesis to open surgical drainage, are useful for pericardial drainage (Table 3). The selection of a particular procedure largely depends on the etiology of the pericardial effusion. In patients with idiopathic or viral pericarditis simple pericardiocentesis is usually sufficient as the illness is self-limited in days or a few weeks and tamponade rarely relapses. Purulent pericarditis should be drained surgically, usually through subxiphoid pericardiotomy.
Table 3.
Procedures of pericardial drainage
| Pericardiocentesis only |
| Indwelling pericardial catheter |
| Percutaneous ballon pericardiotomy |
| Subxiphoid pericardiotomy |
| Pleuropericardial window |
| Partial pericardiectomy |
| Wide anterior pericardiectomy |
The management of cardiac tamponade in patients with neoplastic pericardial involvement merits a special comment. The goals of the treatment are relief of tamponade and prevention of reaccumulation of fluid, which is frequent in these patients. As a rule, less invasive procedures should be preferred, especially in patients with advanced disease and poor general condition. Simple pericardiocentesis alleviates symptoms in most cases but pericardial effusion relapses in as many as 40%-50% of patients[36]. Therefore, pericardiocentesis is the procedure of choice in terminal patients, when recurrence of effusion is not a real issue. In patients with a longer expected survival the treatment has to contemplate possible fluid reaccumulation. Indwelling pericardial catheters have a success rate (defined as alleviation of tamponade and no need of further procedures) of 75% approximately. The catheter should be maintained as long as the amount of drainage is greater than 25 mL/d. In different series[37-40] the duration of catheter drainage averaged 4.8 d. Catheter infection is a potential complication but in our experience we have not observed any case with such a complication. The aims of a prolonged indwelling pericardial catheter are to achieve a complete pericardial drainage and to provoke adherence between the two layers of the pericardium in order to prevent recurrence of pericardial effusion. This goal can be favoured by intrapericardial sclerosis with tetracycline or other agents. However, some authors[41] have observed no additional advantages over indwelling pericardial catheters and sclerosing agents can provoke “excessive” sclerosis with evolution to constrictive pericarditis with clinical repercussion. Therefore, we think that instillation of sclerosing agents should be avoided in patients with relatively good life expectancy. Balloon pericardiotomy is an alternative to surgical creation of a pericardial window. Access to the pericardial space is gained via a conventional subxiphoid pericardiocentesis. A guide wire is advanced into the pericardium, and a balloon catheter is straddled across the pericardium and inflated to create a window[42]. The fluid drains into the pleura or the peritoneal spaces. This technique has been especially adopted for patients with malignancy and reduced life expectancy, and it is successful in more than 80% of cases[42-45]. Reported complications include fever, pneumothorax, left pleural effusion and bleeding from pericardial blood vessels[44,45].
Surgical drainage procedures should be considered in some patients. Some confusion exists about the precise surgical technique of the different procedures (complete pericardiectomy, partial pericardiectomy, subxiphoid pericardiotomy, anterior transthoracic window, pleuropericardial window) but probably all these procedures have a similar efficacy in relieving pericardial effusion (80%-90%). However, inherent perioperative risks, especially if performed under general anesthesia, are a concern. In fact, the overall 30 d mortality for surgical drainage of malignant pericardial effusion has been reported to be 19.4%[46]. In general, the more complex the procedure, the higher the mortality rate.
Our personal attitude in patients with neoplastic pericardial effusion is to begin with an indwelling pericardial catheter. This procedure can be repeated in cases of relapse. The second option would be a subxiphoid percutaneous pericardiotomy or instillation of sclerosing agents. In our experience, surgical drainage techniques are rarely required. The global management strategy is shown schematically in Figure 3.
Figure 3.
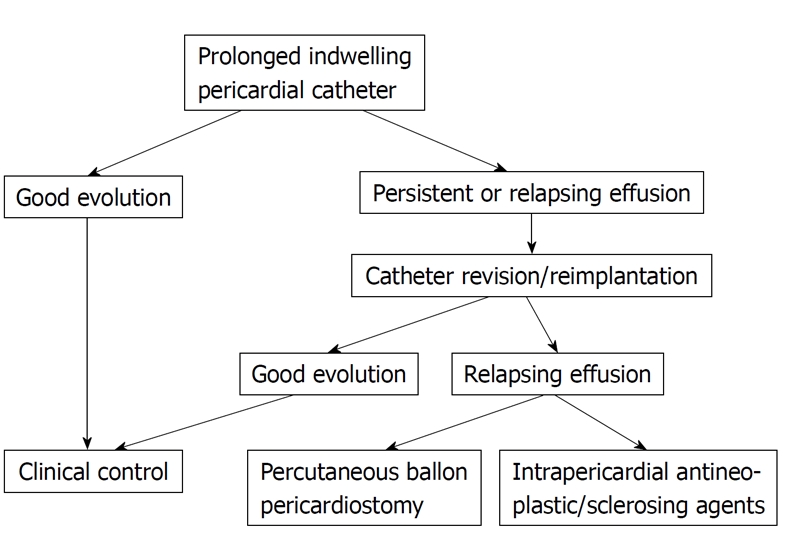
Proposed management strategy for patients with neoplastic pericardial effusion.
Some patients show persistence of clinical findings of systemic venous hypertension after effective drainage of the pericardial effusion. In these cases, a possible component of additional constriction physiology should be suspected (“effusive-constrictive pericarditis”)[47].
IDIOPATHIC CHRONIC PERICARDIAL EFFUSION
Most patients with a large (more than 20 mm), chronic (longer than 3 mo), idiopathic pericardial effusion are asymptomatic and may remain clinically stable for many years. However, this condition may entail a less than good prognosis, as unexpected overt tamponade can develop in up to 29% of such patients[17]. The trigger of tamponade is unknown, but hypovolemia, paroxysmal tachyarrhythmias, and intercurrent acute pericarditis may precipitate tamponade; accordingly, these events should be vigorously managed. Medical therapy, particularly corticosteroids, colchicine or antituberculous therapy, is not useful.
Pericardiocentesis is the first option in patients with overt tamponade. We think that elective pericardial drainage has to be performed as well in asymptomatic patients as a prophylactic measure to prevent unexpected tamponade. In these patients pericardiocentesis should drain as much pericardial fluid as possible. In cases with relapsing effusion, a second pericardiocentesis is warranted. This sequence may result in definitive disappearance of chronic pericardial effusion as was the case in 8 of 19 patients with effusions present for at least 4 years[17]. When a large pericardial effusion relapses after two pericardiocenteses we recommend surgical drainage with wide anterior pericardiectomy even in asymptomatic patients. In our experience this procedure is safe (no mortality has been observed) and is very effective in the long-term[17,48].
PROGNOSIS
The prognosis of pericardial effusion depends on the underlying etiology[10,11,15,16] being especially poor in patients with neoplastic pericardial effusion secondary to lung cancer and positive cytologic study (presence of malignant cells) in pericardial fluid. Prognosis is very good in idiopathic/viral pericarditis. In patients with tuberculous or purulent pericarditis the prognosis depends on the precocity of the diagnosis and adequate treatment, but purulent pericarditis frequently occurs in patients with underlying debilitating disease (diabetes mellitus, liver cirrhosis, widespread infections). The prognosis is good in chronic idiopathic pericardial effusion but tamponade can occur.
Footnotes
Peer reviewers: Yves D Durandy, MD, Perfusion and Intensive Care, Pediatric Cardiac Surgery, Institut Hospitalier J. Cartier, Avenue du Noyer Lambert, Massy 91300, France; Bernhard L Gerber, MD, PhD, Division of Cardiology, Department of Cardiovascular Diseases, Cliniques Universitaires St Luc UCL, Av Hippocrate 10/2806, B-1200 Woluwe St Lambert, Brussels, Belgium
S- Editor Cheng JX L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Savage DD, Garrison RJ, Brand F, Anderson SJ, Castelli WP, Kannel WB, Feinleib M. Prevalence and correlates of posterior extra echocardiographic spaces in a free-living population based sample (the Framingham study) Am J Cardiol. 1983;51:1207–1212. doi: 10.1016/0002-9149(83)90370-3. [DOI] [PubMed] [Google Scholar]
- 2.Restrepo CS, Lemos DF, Lemos JA, Velasquez E, Diethelm L, Ovella TA, Martinez S, Carrillo J, Moncada R, Klein JS. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics. 2007;27:1595–1610. doi: 10.1148/rg.276065002. [DOI] [PubMed] [Google Scholar]
- 3.Galve E, Garcia-Del-Castillo H, Evangelista A, Batlle J, Permanyer-Miralda G, Soler-Soler J. Pericardial effusion in the course of myocardial infarction: incidence, natural history, and clinical relevance. Circulation. 1986;73:294–299. doi: 10.1161/01.cir.73.2.294. [DOI] [PubMed] [Google Scholar]
- 4.Figueras J, Juncal A, Carballo J, Cortadellas J, Soler JS. Nature and progression of pericardial effusion in patients with a first myocardial infarction: relationship to age and free wall rupture. Am Heart J. 2002;144:251–258. doi: 10.1067/mhj.2002.123840. [DOI] [PubMed] [Google Scholar]
- 5.Posner MR, Cohen GI, Skarin AT. Pericardial disease in patients with cancer. The differentiation of malignant from idiopathic and radiation-induced pericarditis. Am J Med. 1981;71:407–413. doi: 10.1016/0002-9343(81)90168-6. [DOI] [PubMed] [Google Scholar]
- 6.Porte HL, Janecki-Delebecq TJ, Finzi L, Métois DG, Millaire A, Wurtz AJ. Pericardoscopy for primary management of pericardial effusion in cancer patients. Eur J Cardiothorac Surg. 1999;16:287–291. doi: 10.1016/s1010-7940(99)00204-3. [DOI] [PubMed] [Google Scholar]
- 7.Nugue O, Millaire A, Porte H, de Groote P, Guimier P, Wurtz A, Ducloux G. Pericardioscopy in the etiologic diagnosis of pericardial effusion in 141 consecutive patients. Circulation. 1996;94:1635–1641. doi: 10.1161/01.cir.94.7.1635. [DOI] [PubMed] [Google Scholar]
- 8.Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587–610. doi: 10.1016/j.ehj.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Agner RC, Gallis HA. Pericarditis: differential diagnostic considerations. Arch Intern Med. 1979;139:407–412. doi: 10.1001/archinte.139.4.407. [DOI] [PubMed] [Google Scholar]
- 10.Colombo A, Olson HG, Egan J, Gardin JM. Etiology and prognostic implications of a large pericardial effusion in men. Clin Cardiol. 1988;11:389–394. doi: 10.1002/clc.4960110606. [DOI] [PubMed] [Google Scholar]
- 11.Sagristà-Sauleda J, Mercé J, Permanyer-Miralda G, Soler-Soler J. Clinical clues to the causes of large pericardial effusions. Am J Med. 2000;109:95–101. doi: 10.1016/s0002-9343(00)00459-9. [DOI] [PubMed] [Google Scholar]
- 12.Shiina A, Yaginuma T, Kondo K, Kawai N, Hosoda S. Echocardiographic evaluation of impending cardiac tamponade. J Cardiography. 1979;9:555–563. [Google Scholar]
- 13.Engel PJ, Hon H, Fowler NO, Plummer S. Echocardiographic study of right ventricular wall motion in cardiac tamponade. Am J Cardiol. 1982;50:1018–1021. doi: 10.1016/0002-9149(82)90411-8. [DOI] [PubMed] [Google Scholar]
- 14.Mercé J, Sagristà-Sauleda J, Permanyer-Miralda G, Evangelista A, Soler-Soler J. Correlation between clinical and Doppler echocardiographic findings in patients with moderate and large pericardial effusion: implications for the diagnosis of cardiac tamponade. Am Heart J. 1999;138:759–764. doi: 10.1016/s0002-8703(99)70193-6. [DOI] [PubMed] [Google Scholar]
- 15.Levine MJ, Lorell BH, Diver DJ, Come PC. Implications of echocardiographically assisted diagnosis of pericardial tamponade in contemporary medical patients: detection before hemodynamic embarrassment. J Am Coll Cardiol. 1991;17:59–65. doi: 10.1016/0735-1097(91)90704-d. [DOI] [PubMed] [Google Scholar]
- 16.Guberman BA, Fowler NO, Engel PJ, Gueron M, Allen JM. Cardiac tamponade in medical patients. Circulation. 1981;64:633–640. doi: 10.1161/01.cir.64.3.633. [DOI] [PubMed] [Google Scholar]
- 17.Sagristà-Sauleda J, Angel J, Permanyer-Miralda G, Soler-Soler J. Long-term follow-up of idiopathic chronic pericardial effusion. N Engl J Med. 1999;341:2054–2059. doi: 10.1056/NEJM199912303412704. [DOI] [PubMed] [Google Scholar]
- 18.Leimgruber PP, Klopfenstein HS, Wann LS, Brooks HL. The hemodynamic derangement associated with right ventricular diastolic collapse in cardiac tamponade: an experimental echocardiographic study. Circulation. 1983;68:612–620. doi: 10.1161/01.cir.68.3.612. [DOI] [PubMed] [Google Scholar]
- 19.Klopfenstein HS, Cogswell TL, Bernath GA, Wann LS, Tipton RK, Hoffmann RG, Brooks HL. Alterations in intravascular volume affect the relation between right ventricular diastolic collapse and the hemodynamic severity of cardiac tamponade. J Am Coll Cardiol. 1985;6:1057–1063. doi: 10.1016/s0735-1097(85)80309-0. [DOI] [PubMed] [Google Scholar]
- 20.Rifkin RD, Pandian NJ, Funai JT, Wang SS, Sharma SC, Lojeski EW, Levine HJ. Sensitivity of right atrial collapse and right ventricular diastolic collapse in the diagnosis of graded cardiac tamponade. Am J Noninvasive Cardiol. 1987;1:73–80. [Google Scholar]
- 21.Gonzalez MS, Basnight MA, Appleton CP. Experimental pericardial effusion: relation of abnormal respiratory variation in mitral flow velocity to hemodynamics and diastolic right heart collapse. J Am Coll Cardiol. 1991;17:239–248. doi: 10.1016/0735-1097(91)90733-p. [DOI] [PubMed] [Google Scholar]
- 22.Singh S, Wann LS, Schuchard GH, Klopfenstein HS, Leimgruber PP, Keelan MH, Brooks HL. Right ventricular and right atrial collapse in patients with cardiac tamponade--a combined echocardiographic and hemodynamic study. Circulation. 1984;70:966–971. doi: 10.1161/01.cir.70.6.966. [DOI] [PubMed] [Google Scholar]
- 23.Reddy PS, Curtiss EI, Uretsky BF. Spectrum of hemodynamic changes in cardiac tamponade. Am J Cardiol. 1990;66:1487–1491. doi: 10.1016/0002-9149(90)90540-h. [DOI] [PubMed] [Google Scholar]
- 24.Permanyer-Miralda G, Sagristá-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patients. Am J Cardiol. 1985;56:623–630. doi: 10.1016/0002-9149(85)91023-9. [DOI] [PubMed] [Google Scholar]
- 25.Strang JI, Nunn AJ, Johnson DA, Casbard A, Gibson DG, Girling DJ. Management of tuberculous constrictive pericarditis and tuberculous pericardial effusion in Transkei: results at 10 years follow-up. QJM. 2004;97:525–535. doi: 10.1093/qjmed/hch086. [DOI] [PubMed] [Google Scholar]
- 26.Corey GR, Campbell PT, Van Trigt P, Kenney RT, O'Connor CM, Sheikh KH, Kisslo JA, Wall TC. Etiology of large pericardial effusions. Am J Med. 1993;95:209–213. doi: 10.1016/0002-9343(93)90262-n. [DOI] [PubMed] [Google Scholar]
- 27.Levy PY, Fournier PE, Charrel R, Metras D, Habib G, Raoult D. Molecular analysis of pericardial fluid: a 7-year experience. Eur Heart J. 2006;27:1942–1946. doi: 10.1093/eurheartj/ehl025. [DOI] [PubMed] [Google Scholar]
- 28.Soler-Soler J, Permanyer-Miralda G, Sagristà-Sauleda J. Pericardial Disease. New Insights and Old Dilemmas. Appendix I. Protocol for the diagnosis and management of pericardial diseases. Dordrecht: Kluwer Academic Publishers; 1990. pp. 217–222. [Google Scholar]
- 29.Soler-Soler J, Sagristà-Sauleda J, Permanyer-Miralda G. Relapsing pericarditis. Heart. 2004;90:1364–1368. doi: 10.1136/hrt.2003.026120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation. 2005;112:2012–2016. doi: 10.1161/CIRCULATIONAHA.105.542738. [DOI] [PubMed] [Google Scholar]
- 31.Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042–1046. doi: 10.1016/j.jacc.2003.09.055. [DOI] [PubMed] [Google Scholar]
- 32.Sagristà-Sauleda J, Permanyer-Miralda G, Soler-Soler J. Tuberculous pericarditis: ten year experience with a prospective protocol for diagnosis and treatment. J Am Coll Cardiol. 1988;11:724–728. doi: 10.1016/0735-1097(88)90203-3. [DOI] [PubMed] [Google Scholar]
- 33.Sagristà-Sauleda J, Barrabés JA, Permanyer-Miralda G, Soler-Soler J. Purulent pericarditis: review of a 20-year experience in a general hospital. J Am Coll Cardiol. 1993;22:1661–1665. doi: 10.1016/0735-1097(93)90592-o. [DOI] [PubMed] [Google Scholar]
- 34.Lestuzzi C. Neoplastic pericardial disease: Old and current strategies for diagnosis and management. World J Cardiol. 2010;2:270–279. doi: 10.4330/wjc.v2.i9.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mercé J, Sagristà-Sauleda J, Permanyer-Miralda G, Soler-Soler J. Should pericardial drainage be performed routinely in patients who have a large pericardial effusion without tamponade? Am J Med. 1998;105:106–109. doi: 10.1016/s0002-9343(98)00192-2. [DOI] [PubMed] [Google Scholar]
- 36.Vaitkus PT, Herrmann HC, LeWinter MM. Treatment of malignant pericardial effusion. JAMA. 1994;272:59–64. [PubMed] [Google Scholar]
- 37.Wei JY, Taylor GJ, Achuff SC. Recurrent cardiac tamponade and large pericardial effusions: management with an indwelling pericardial catheter. Am J Cardiol. 1978;42:281–282. doi: 10.1016/0002-9149(78)90911-6. [DOI] [PubMed] [Google Scholar]
- 38.Lock JE, Bass JL, Kulik TJ, Fuhrman BP. Chronic percutaneous pericardial drainage with modified pigtail catheters in children. Am J Cardiol. 1984;53:1179–1182. doi: 10.1016/0002-9149(84)90658-1. [DOI] [PubMed] [Google Scholar]
- 39.Kopecky SL, Callahan JA, Tajik AJ, Seward JB. Percutaneous pericardial catheter drainage: report of 42 consecutive cases. Am J Cardiol. 1986;58:633–635. doi: 10.1016/0002-9149(86)90290-0. [DOI] [PubMed] [Google Scholar]
- 40.Patel AK, Kosolcharoen PK, Nallasivan M, Kroncke GM, Thomsen JH. Catheter drainage of the pericardium. Practical method to maintain long-term patency. Chest. 1987;92:1018–1021. doi: 10.1378/chest.92.6.1018. [DOI] [PubMed] [Google Scholar]
- 41.Spodick DH. Neoplastic pericardial disease. In: Spodick DH, editor. The pericardium: A Comprehensive Textbook. New York: Marcel Dekker; 1997. pp. 301–313. [Google Scholar]
- 42.Palacios IF, Tuzcu EM, Ziskind AA, Younger J, Block PC. Percutaneous balloon pericardial window for patients with malignant pericardial effusion and tamponade. Cathet Cardiovasc Diagn. 1991;22:244–249. doi: 10.1002/ccd.1810220403. [DOI] [PubMed] [Google Scholar]
- 43.Ziskind AA, Pearce AC, Lemmon CC, Burstein S, Gimple LW, Herrmann HC, McKay R, Block PC, Waldman H, Palacios IF. Percutaneous balloon pericardiotomy for the treatment of cardiac tamponade and large pericardial effusions: description of technique and report of the first 50 cases. J Am Coll Cardiol. 1993;21:1–5. doi: 10.1016/0735-1097(93)90710-i. [DOI] [PubMed] [Google Scholar]
- 44.Wang HJ, Hsu KL, Chiang FT, Tseng CD, Tseng YZ, Liau CS. Technical and prognostic outcomes of double-balloon pericardiotomy for large malignancy-related pericardial effusions. Chest. 2002;122:893–899. doi: 10.1378/chest.122.3.893. [DOI] [PubMed] [Google Scholar]
- 45.Swanson N, Mirza I, Wijesinghe N, Devlin G. Primary percutaneous balloon pericardiotomy for malignant pericardial effusion. Catheter Cardiovasc Interv. 2008;71:504–507. doi: 10.1002/ccd.21431. [DOI] [PubMed] [Google Scholar]
- 46.Piehler JM, Pluth JR, Schaff HV, Danielson GK, Orszulak TA, Puga FJ. Surgical management of effusive pericardial disease. Influence of extent of pericardial resection on clinical course. J Thorac Cardiovasc Surg. 1985;90:506–516. [PubMed] [Google Scholar]
- 47.Sagristà-Sauleda J, Angel J, Sánchez A, Permanyer-Miralda G, Soler-Soler J. Effusive-constrictive pericarditis. N Engl J Med. 2004;350:469–475. doi: 10.1056/NEJMoa035630. [DOI] [PubMed] [Google Scholar]
- 48.Loire R, Goineau P, Fareh S, Saint-Pierre A. [Apparently idiopathic chronic pericardial effusion. Long-term outcome in 71 cases] Arch Mal Coeur Vaiss. 1996;89:835–841. [PubMed] [Google Scholar]