Abstract
Clopidogrel is approved for reduction of atherothrombotic events in patients with cardiovascular (CV) and cerebrovascular disease. Dual antiplatelet therapy with aspirin and clopidogrel decreases the risk of major adverse cardiac events after acute coronary syndrome or percutaneous coronary intervention, compared with aspirin alone. Due to concern about gastrointestinal bleeding in patients who are receiving clopidogrel and aspirin therapy, current guidelines recommend combined use of a proton pump inhibitor (PPI) to decrease the risk of bleeding. Data from previous pharmacological studies have shown that PPIs, which are extensively metabolized by the cytochrome system, may decrease the ADP-induced platelet aggregation of clopidogrel. Results from retrospective cohort studies have shown a higher incidence of major CV events in patients receiving both clopidogrel and PPIs than in those without PPIs. However, other retrospective analyses of randomized clinical trials have not shown that the concomitant PPI administration is associated with increased CV events among clopidogrel users. These controversial results suggest that large specific studies are needed. This article reviews the metabolism of clopidogrel and PPIs, existing clinical data regarding the interaction between clopidogrel and PPIs, and tries to provide recommendations for health care professionals.
Keywords: Antiplatelet therapy, Aspirin, Clopidogrel, Proton pump inhibitor
INTRODUCTION
Clopidogrel is approved for reduction of atherothrombotic events in patients with acute coronary syndrome (ACS)[1]. Clopidogrel usually is prescribed as an alternative to aspirin for patients with unstable angina or non-ST-segment elevation myocardial infarction (MI) who are intolerant of aspirin. A few randomized trials in patients with ACS have shown that clopidogrel plus aspirin produces significant relative risk (RR) reductions of 10%-20% in cardiovascular (CV) events compared with aspirin alone[2,3]. Current guidelines recommend clopidogrel plus aspirin for ≥ 1 mo after a bare metal coronary artery stent, ≥ 1 year after a drug-eluting stent (DES), ≥ 1 mo and ideally ≥ 1 year after unstable angina or non-ST-elevation MI managed without intervention, and 1 year after ST-elevation MI[4-6]. These antiplatelet agents have recognizable risks of gastrointestinal (GI) complications such as ulceration and related bleeding. These risks may be further compounded by the ancillary use of other adjunctive medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and anticoagulants. Given the high prevalence of antiplatelet therapy in clinical practice, coupled with an increased emphasis on their extended use, especially after implantation of a DES[7-9], it is important that physicians should know the potential benefits and the associated risks of antiplatelet therapy for secondary prevention of cardiac ischemic events.
Recently, two relevant cautions about clopidogrel therapy have been raised if one intends to administer aspirin and clopidogrel therapy together. One is antiplatelet non-responsiveness or resistance, and the other relates to interaction between clopidogrel and proton pump inhibitors (PPIs). Previous experience has found that the expected antiplatelet effect from oral aspirin and/or clopidogrel does not occur, and a significant number of patients experience increased risks of adverse ischemic events despite antiplatelet therapy. This phenomenon is considered to be aspirin and/or clopidogrel non-responsiveness or resistance[10-14]. The reported mean prevalence of clopidogrel resistance is 21% (95% CI: 17%-25%) in a systemic review[15]. The issue of clopidogrel resistance has been discussed elsewhere [10,11,14-18]. This paper does not discuss clopidogrel resistance, but focuses on interaction between clopidogrel and PPIs.
PPIs are often prescribed prophylactically with initiation of clopidogrel to reduce the risk of GI bleeding while taking dual-antiplatelet therapy. A randomized, double blind OCLA (Omeprazole Clopidogrel Aspirin) study that assessed the influence of omeprazole on clopidogrel efficacy has demonstrated that omeprazole significantly decreases the clopidogrel inhibitory effect on platelet P2Y12, as demonstrated by vasodilator-stimulated phosphoprotein phosphorylation test[19]. It suggests that PPIs reduce the inhibitory effect of clopidogrel on platelet aggregation. In a population-based study, we have reported that concomitant use of PPIs and clopidogrel is associated with an increased risk of rehospitalization (HR: 1.23, 95% CI: 1.07-1.41, P = 0.003) and mortality (HR: 1.65, 95% CI: 1.35-2.01, P < 0.001)[20]. It was consistent with previous studies that concomitant use of clopidogrel and PPIs is associated with a higher risk of acute MI, death or target vessel failure[21,22]. Similarly, three larger retrospective cohort studies of 38 531 patients have reported an increased risk of CV events for patients receiving combined PPI and clopidogrel compared with clopidogrel alone[23-25]. In contrast, results of the retrospective analyses of three large clinical trials of 41 000 clopidogrel-treated patients [Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel Thrombolysis in Myocardial Infarction 38 (TRITON-TIMI 38), Platelet Inhibition and Patient Outcomes (PLATO), Clopidogrel Optimal Loading Dose Usage to Reduce Recurrent Events/Optimal Antiplatelet Strategy for Interventions (CURRENT-OASIS 7)] have shown no significant effect of concomitant PPI administration on the clinical efficacy of clopidogrel therapy[26-28]. Due to the fact that these studies had conflicting results, it opens the question of whether the efficacy of clopidogrel is influenced by concomitant use of PPIs. This report aims to review the metabolism of clopidogrel and PPIs, relevant articles of clinical and pharmacological studies, and tries to provide recommendations for the combined use of clopidogrel and PPIs.
CLOPIDOGREL METABOLISM
Clopidogrel, a thienopyridine, is a prodrug that is transformed to an active metabolite, which subsequently blocks platelet activation and aggregation. After ingestion of clopidogrel, the majority (85%) of the prodrug is immediately inactivated by plasma esterases to an inactive from (SR26334). Approximately 15% of an absorbed clopidogrel dose is converted to an active thiol metabolite (R-130964); mainly by the hepatic cytochrome P450 isoenzymes[19,29]. The metabolism of clopidogrel is a complex process that involves a number of cytochrome P450 isoenzymes to varying degrees. The active metabolite is formed in the liver through the cytochrome P450 (CYP) system after two sequential reactions that involve CYP1A2, CYP2B6, CYP2C9, CYP2C19 and CYP3A4, with CYP2C19 playing a major role (Figure 1)[29-32]. Clopidogrel and its active metabolite are relatively short lived in plasma. With repeated 75 mg daily doses, plasma concentrations of the parent compound and its active metabolite fall below the lower limit of quantification after 2 h[29-33]. Despite a short half-life, the irreversible binding of the active metabolite of clopidogrel to the platelet receptor leads to a prolonged pharmacodynamic effect. Inhibition of platelet aggregation by clopidogrel lasts for several days, with platelet function returning to baseline about 5 d after stopping the drug[34].
Figure 1.
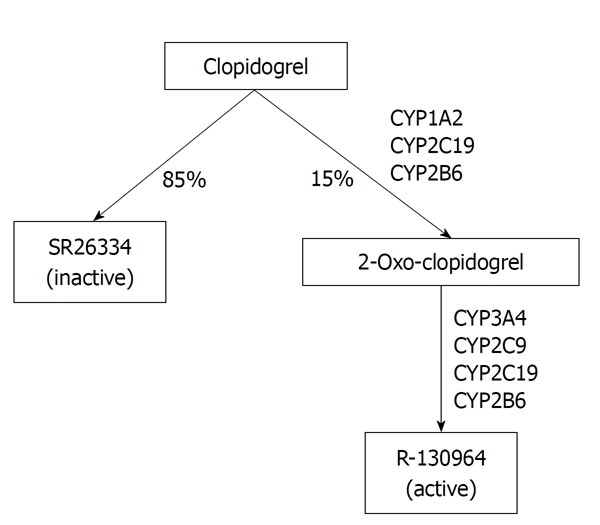
Metabolism of clopidogrel. Clopidogrel undergoes two-step metabolism that can involve several different cytochrome P450 enzymes (from[29], reproduced with permission from the publisher of Annals of Pharmacotherapy, Copyright 2011).
It has been reported that patients with reduced-function genetic polymorphisms of CYP2C19 are associated with reduced conversion of clopidogrel to its active metabolite and a reduction in inhibition of ADP-induced platelet aggregation by clopidogrel[29,30].
Another report has shown that the effect of clopidogrel in reducing the rate of the primary efficacy outcome was similar in patients who were heterozygous or homozygous for loss-of-function alleles, and in those who were not carriers of the alleles[31]. Although the role of CYP2C19 genetic polymorphisms is still controversial, several cohort studies have shown that patients with prior MI, ACS, or percutaneous coronary intervention (PCI) who are prescribed clopidogrel have significantly increased RR of CV events, which includes death from CV causes, MI, stroke, or stent thrombosis (1.5-4), with CYP2C19 reduced-function genetic variants[19,32,33]. This increased risk is apparent even among patients who are heterozygous for reduced-function allelic variants[19,32,33]. Mega and his colleagues have found that carriers of a reduced-function CYP2C19 allele have significantly lower levels of the active metabolite of clopidogrel, diminished platelet inhibition, and a higher rate of major adverse CV events. Specifically, common polymorphisms in the CYP2C19 gene, seen in approximately 30% of caucasians, 40% of blacks, and > 55% of East Asians[34], significantly diminish the pharmacokinetic and pharmacodynamic responses to clopidogrel by approximately one quarter to one third. Genetic polymorphisms of CYP2C19 modulate clopidogrel pharmacokinetics and pharmacodynamics in healthy volunteers[12,35], as well as in patients[14,36,37]. As compared with subjects with no CYP2C19 variant allele, subjects with one or two CYP2C19 loss-of-function alleles have been shown to have lower plasma concentrations of the active metabolite of clopidogrel and a decrease in the ADP-induced platelet aggregation of clopidogrel[12]. In addition, investigators have demonstrated that, among individuals treated with clopidogrel, patients with a reduced-function CYP2C19 allele tend to have significantly lower levels of the active clopidogrel metabolite, diminished platelet inhibition, and a higher rate of major adverse CV events[32], including stent thrombosis[37].
PPI METABOLISM
PPIs are prodrugs that are transformed nonenzymatically in the acid environment of gastric parietal cells to active derivatives, which bind covalently to H+ K+ -ATPase (proton pump)[38,39]. This irreversible inhibition of the proton pump leads to long-term acid suppression for up to 36 h[38].
Li et al[40] have compared the degree of CYP2C19 inhibition by the currently used PPIs (e.g. omeprazole, esomeprazole, lansoprazole, rabeprazole, and pantoprazole), and the inhibition of CYP2C19 by the PPIs was measured in vitro using S-mephenytoin 4-hydroxylation as a marker reaction. They have found that lansoprazole is the most potent inhibitor of CYP2C19, whereas pantoprazole and rabeprazole are the least potent. The currently available PPIs include omeprazole, esomeprazole, lansoprazole, pantoprazole and rabeprazole. All PPIs are hepatically metabolized to an extent via the cytochrome P450 mixed oxidase system. The isoenzymes CYP3A4 and particularly, CYP2C19, are the major isoforms that cause PPI biotransformation. The relative contribution of this latter pathway in general metabolism differs among drugs and has been reported to be omeprazole = esomeprazole > pantoprazole > lansoprazole > rabeprazole[41]. In contrast to the situation with clopidogrel, reduced CYP2C19 function results in less inactivation of PPI and an increase in pharmacodynamic effect (greater acid inhibition). Poor CYP2C19 metabolism has been associated with improved clinical outcomes such as healing of esophagitis or eradication of Helicobacter pylori (H. pylori)[10].
Gilard et al[19], using a novel surrogate marker (vasodilator-stimulated phosphoprotein phosphorylation platelet reactivity index, or PRI) for CV events, have reported that there is a higher PRI in patients taking clopidogrel plus PPI than in those taking clopidogrel without PPI. In another double-blind, placebo-controlled trial, patients undergoing coronary artery stent implantation received dual antiplatelet treatment, and were randomized to receive omeprazole or placebo for 7 d to compare the PRI value between the two groups. The authors found significantly more poor responders, as measured by PRI, in the omeprazole group than in the placebo group[10]. In the PRINCIPLE-TIMI 44 trial, mean inhibition of platelet aggregation was significantly lower for patients on a PPI than for those not on a PPI after a 600 mg clopidogrel loading dose (P = 0.02). This indicates that PPI users have significantly less inhibition of ADP-induced platelet aggregation than non-users[26]. Metabolism of PPIs and clopidogrel involves CYP2C19, therefore, the CYP2C19 isoform is the key enzyme in the metabolism of many PPIs, which are also inhibitors of the CYP2C19 and CYP3A4 isoenzymes to varying degrees. This has led to the assumption that some PPIs have the ability to inhibit metabolic activation of clopidogrel[41,42]. The ability of a PPI to inhibit CYP2C19 activity could reduce R-130964 generation and cause a diminished clopidogrel response. Thus, concomitant PPI therapy can further reduce clopidogrel metabolism, which predisposes patients to such adverse CV events and death[43-45].
SEARCH STRATEGY TO IDENTIFY ARTICLES RELEVANT TO THE POTENTIAL INTERACTION BETWEEN CLOPIDOGREL AND PPIs
The PubMed and Medline searches were conducted using the keywords “clopidogrel” and “proton pump inhibitors” to identify studies that evaluated a potential interaction between clopidogrel and PPIs. Reference lists of recent publications on these topics were also evaluated for relevant publications. An initial screen to identify relevant papers by reading the abstracts or titles was performed. The original studies but not the review articles were included. The second screening was based on full-text review. Studies were selected if they reported on the incidence of major cardiac adverse events or mortality. Studies were excluded if the primary end point was only biological or GI safety driven, or if there was inappropriate group comparison. These articles are subsequently separated into two different categories depending upon that support or against the drug-drug interaction between clopidogrel and PPIs.
CLINICAL EVIDENCES SUPPORT DRUG INTERACTION
Recent studies of the influence of PPIs on clinical outcomes with clopidogrel therapy are summarized in Table 1. We have conducted a nationwide, population-based study in 3278 patients with coronary artery disease who had taken clopidogrel after PCI, using the Taiwan National Health Insurance database[20]. According to the Kaplan-Meier analysis, the incidence of rehospitalization due to acute MI (AMI) or angina (P = 0.001) and mortality (P < 0.001) was significantly greater for patients with concomitant PPI use (n = 572) than for those without (n = 2706). Multivariate analyses showed that concomitant PPI use was associated with an increased risk of rehospitalization (HR: 1.23, 95% CI: 1.07-1.41, P = 0.003) and mortality (HR: 1.65, 95% CI: 1.35-2.01, P < 0.001)[20]. Due to the fact that the prevalence of CYP2C19 loss-of-function alleles is much greater among East Asians than among other populations, we believe that concomitant use of clopidogrel and PPIs may have the possibility of low response to clopidogrel in East Asians patients who have undergone PCI. Pezalla et al[21] have assigned their patients into three groups: no PPI exposure group (control), low PPI exposure group, or high PPI exposure group based on the adherence rates to PPIs. They have found that the 1-year AMI rate was 1.38% (66 of 4800 patients) in the control group, 3.08% (22 of 712 patients) in the low PPI exposure group, and 5.03% in the high PPI exposure group. Using the control group MI incidence as the expected MI rate, the difference in MI rates between the control and high exposure groups (1.38% vs 5.03%) was significant (P < 0.05).
Table 1.
Clinical evidences support the interaction between clopidogrel and proton pump inhibitors
| Study design | Follow-up | Number of patients on clopidogrel with/without PPI | End point | Results | Ref. |
| Population-based study | 6 yr | PPI: 572; no PPI: 2706 | Rehospitalization (due to AMI or angina); mortality | Rehospitalization in PPI vs no PPI groups: HR: 1.23 (95% CI: 1.07-1.41, P = 0.003); mortality: HR: 1.65 (95% CI: 1.35-2.01, P < 0.001) | Huang et al[20] |
| Retrospective cohort study | 1 yr | Low PPI: 712; high PPI: 5.03%(?); without PPI: 4800 | MI | Acute MI rate: non-PPI: 1.38% (66/4800); low PPI exposure: 3.08% (22/712); high PPI exposure: 5.03% (?) (P < 0.05 for high vs no PPI use) | Pezalla et al[21] |
| Retrospective nested case-control | 3 mo | Cases: 734 (PPI: 194); controls: 2057 (PPI: 424) | Death or readmitted for MI | Readmission for acute MI, adjusted OR 1.27 (95% CI: 1.03-1.57); pantoprazole OR: 1.02 (95% CI: 0.70-1.47); other PPIs (omeprazole, lansoprazole and rabeprazole) OR: 1.40 (95% CI: 1.10-1.77) | Juurlink et al[23] |
| Retrospective cohort study | October 2003 and January 2006 | PPI: 5244; without PPI: 2961 | Death or rehospitalization for MI or unstable angina | Death or rehospitalization: non-PPI vs PPI groups: 20.8% vs 29.8% OR: 1.25 (95% CI: 1.11-1.41); omeprazole OR: 1.24 (95% CI: 1.08-1.41); rabeprazole OR: 2.83 (95% CI: 1.96-4.09) | Ho et al[24] |
| Retrospective cohort study using the National Medco Integrated Database | 1 yr | PPI: 6828; without PPI: 9862 | Stroke or TIA, ACS, CV death, coronary revascularization | MACE rate in the PPI vs non-PPI groups: 25.1% vs 17.8% (adjusted HR of 1.57, 95% CI: 1.39-1.64); Omeprazole: 25.1% HR: 1.39 (95% CI: 1.22-1.57), esomeprazole: 24.9% HR: 1.57 (95% CI: 1.40-1.76), lansoprazole: 24.3% HR: 1.39 (95% CI: 1.16-1.67) and pantoprazole: 29.2% HR: 1.61 (95% CI: 1.44-1.81) | Kreutz et al[25] |
| Retrospective cohort within RCT | 28 d and 1 yr | PPI: 366; without PPI: 1750 | Death, MI, stroke at 1 yr; Death, MI, UTVR at 28 d | Death, MI, stroke at 1 yr: HR: 1.55, 95% CI: 1.031-2.341, P = 0.035; Death, MI, UTVR at 28 d, HR: 1.63, 95% CI: 1.015-2.627, P = 0.043 | Dunn et al[46] |
| Retrospective cohort study | 1 yr | PPI: 318; without PPI: 502 | CV death, Q-wave MI, coronary revascularization and stent thrombosis | Major MACE event rate in the PPI vs non-PPI groups: 13.8% vs 8% (P = 0.008); HR of MACE: 1.8 (95% CI: 1.1-2.7, P = 0.01); overall mortality: 4.7% vs 1.8% (P = 0.02) | Gaglia et al[48] |
| Retrospective observational study (FRENA registry) | 15 mo | PPI: 519; no PPI: 703 | MI, stroke, critical limb ischemia, death | Incidence of events of PPI vs no PPI groups: MI: 4.4% vs 2.1%, HR: 2.5 (95% CI: 1.3-4.8, P = 0.003); stroke: 3.7% vs 2.3%, HR: 1.9 (95% CI: 1.03-3.7, P = 0.039); critical limb ischemia: 4.7% vs 3.4%; HR: 1.6 (95% CI: 0.95-2.8, P = 0.077); death: 7.5% vs 3.3%, HR: 2.2 (95% CI: 1.3-3.7, P = 0.003) | Muñoz-Torrero et al[49] |
PPI: Proton pump inhibitor; TIA: Transient ischemic attack; MI: Myocardial infarction; AMI: Acute MI; ACS: Acute coronary syndrome; CV: Cardiovascular.
A large epidemiological study has investigated the medical records of the Ontario Public Drug Program[23]; the investigators isolated 13 636 patients with prescriptions for clopidogrel within 3 d of AMI. This study found that there was a significant association between occurrence of AMI and concurrent use of PPI (adjusted OR: 1.27, 95% CI: 1.03-1.57). A stratified analysis based on the specific PPI user revealed that pantoprazole was not associated with an increased risk of MI in patients taking clopidogrel. In contrast, the other PPIs were associated with a 40% increase in the risk of recurrent MI (OR: 1.40, 95% CI: 1.10-1.77). Therefore, the pantoprazole may be safer than other PPIs in terms of the subsequent risk due to recurrent MI in patients taking clopidogrel.
Ho et al[24] have performed a retrospective cohort study of 8205 patients with ACS who were taking clopidogrel after discharge from hospital. Using pharmacy refill data, the investigators found that 64% (n = 5244) of the patients were prescribed a PPI at discharge or during follow-up, while 36% (n = 2961) were not. There was a significantly higher rate of death or rehospitalization for ACS in patients prescribed clopidogrel plus a PPI (adjusted OR: 1.25, 95% CI: 1.11-1.41). This finding supports the theory of an interaction between PPI and clopidogrel. In the Clopidogrel Medco Outcomes Study[25], researchers analyzed integrated data on pharmacy and medical records claims from > 10 million patients, including 16 690 patients taking clopidogrel for a full year following coronary stenting. This retrospective cohort study found that the risk of major adverse CV events [including stroke or transient ischemic attack (TIA), ACS, coronary revascularization, or CV death] was raised from 17.9% to 25.1% in patients also taking PPIs (HR: 1.51, 95% CI: 1.39-1.64, P < 0.0001). The overall risk of major cardiac events was 51% higher among patients taking any PPIs. These included a 70% increase in the risk of MI or unstable angina, a 48% increase in the risk of stroke or TIA, and a 35% increase in the need for urgent target vessel revascularization[25].
The Clopidogrel for Reduction of Events during Observation trial was a large, randomized, double-blind study[46]. The investigators evaluated both the 28-d incidence of death, MI, or urgent target vessel revascularization and 1 year rate of death, MI, or stroke for patients on clopidogrel with or without a PPI, and placebo with or without a PPI. The results showed that baseline PPI use was independently associated with adverse CV events at 28 d and 1 year in the overall population (OR: 1.633, 95% CI: 1.02-2.63 at 28 d; OR: 1.55, 95% CI: 1.03-2.34 at 1 year)[46]. The phenomenon that concomitant use of PPIs and clopidogrel was associated with an increased risk of recurrent MI is not only observed for omeprazole, but may also be seen for most PPIs[23-25]. A recent has also found that there was a slightly increased risk (< 20%) of MI hospitalization or death in older patients who started both clopidogrel and a PPI compared with those without a PPI[47].
Gaglia et al[48] have examined the effect of a PPI at discharge after PCI with DESs on the incidence of major adverse cardiac events (MACE) in patients with (318 cases) or without (502 cases) a PPI. The MACE included death, Q-wave MI, target vessel revascularization, and stent thrombosis. All patients were taking clopidogrel. Using the univariate survival analysis, there was a greater rate of MACE (13.8% vs 8.0%, P = 0.008) and overall mortality (4.7% vs 1.8%, P = 0.02) in the PPI group. After multivariate analysis, the adjusted MACE HR for PPI at discharge was 1.8 (95% CI: 1.1-2.7, P = 0.01). Another multicenter, observational (FRENA) registry was conducted in Spanish hospitals to evaluate the influence of concomitant use of PPI on outcome in 1222 patients receiving clopidogrel[49]. PPI users had a higher incidence of MI (rate ratio: 2.5, 95% CI: 1.3-4.8), ischemic stroke (rate ratio: 1.9, 95% CI: 1.03-3.7), and a nonsignificantly higher rate of critical limb ischemia (rate ratio: 1.6, 95% CI: 0.95-2.8) than nonusers. On multivariate analysis, concomitant use of clopidogrel and PPIs was independently associated with an increased risk for subsequent ischemic events; both in the whole series of patients (HR: 1.8, 95% CI: 1.1-2.7) and in those with cerebrovascular disease or peripheral artery disease (HR: 1.5, 95% CI: 1.01-2.4)[49]. The authors have concluded that concomitant use of PPIs and clopidogrel is associated with a nearly doubling of the incidence of subsequent MI or ischemic stroke in patients with established arterial disease.
A recent systematic review and meta-analysis of 25 articles has also described that administration of PPIs together with clopidogrel corresponded to a 29% increased risk of combined MACE (RR: 1.29, 95% CI: 1.15-1.45) and a 31% increased risk of MI (RR: 1.31, 95% CI: 1.12-1.53), but does not influence the risk of death[50]. In summary, these reports indicated that concomitant use of PPI and clopidogrel might be associated with an increased risk of CV events.
CLINICAL EVIDENCE AGAINST DRUG INTERACTION
In a retrospective analysis of the National Medco Integrated Database, the authors identified 1641 patients who had undergone a PCI/stent procedure[25]. These patients were divided into two cohorts: one with patients taking PPIs (n = 234) and one not taking PPIs (n = 1407). Over the 12-mo study period, the incidence of CV events was 24.8% for patients taking a PPI, and 20.8% for those who were not. There was no significant difference in the risk of any event between the two groups. In the National Heart Lung and Blood Institute dynamic registry, a univariate analysis of a cohort study found that patients prescribed both PPI and clopidogrel were not associated with adverse clinical outcomes after PCI[51]. In the nationwide French registry of 2208 patients presenting with AMI who received clopidogrel therapy, the authors found that the use of any PPI had no effect on the clinical response to clopidogrel[52]. Further evidence against drug interactions was from the randomized Clopidogrel and the Optimization of Gastrointestinal Events Trial (COGENT), in which 3627 patients taking aspirin after ACS or stent implantation were randomized to clopidogrel alone or with low-dose omeprazole[53]. The primary GI end point was a composite of overt or occult bleeding, symptomatic gastroduodenal ulcers or erosions, obstruction, or perforation. The primary CV end point was a composite of death from CV causes, nonfatal MI, revascularization, or stroke. The trial was terminated prematurely when the sponsor lost financing. However, the results of COGENT revealed that omeprazole was associated with a 45% reduction in the risk of GI events and no increase in the risk of CV events, including secondary analysis of AMI or revascularization. The authors concluded that among patients receiving aspirin and clopidogrel, prophylactic use of a PPI reduced the rate of upper GI bleeding. However, there was no apparent CV interaction between clopidogrel and omeprazole.
O’Donoghue et al[26] have used a multivariable Cox model with propensity score to assess the association of concomitant use of clopidogrel (n = 6795; 300 mg loading dose, 75 mg daily maintenance dose) and PPI with clinical outcomes. The primary endpoint was a composite of CV death, nonfatal MI, or stroke. Results revealed that in the clopidogrel group, the Kaplan-Meier rate of the primary endpoint throughout long-term follow-up was 11.8% for individuals on a PPI and 12.2% for those not on a PPI. After adjustment for potential confounders and the propensity to treat with a PPI, no significant association remained between use of a PPI and risk of the primary endpoint (adjusted HR: 0.94, 95% CI: 0.80-1.11, P = 0.46). Recently, the French Registry of Acute-ST-Elevation and Non-ST Elevation Myocardial Infarction has reported their experience in assessing the clinical impact of PPI treatment on the efficacy of clopidogrel therapy[54]. This study found that PPI use was not associated with an increased risk for any of the main in-hospital events (in-hospital survival, reinfarction, stroke, bleeding, and transfusion). Besides, PPI treatment was not an independent predictor of 1-year MI, stroke, or death (HR: 0.98, 95% CI: 0.90-1.08, P = 0.72) in patients administered clopidogrel for recent MI (Table 2).
Table 2.
Clinical evidences against interaction between clopidogrel and proton pump inhibitors
| Study design | Follow-up | Number of patients on clopidogrel with/without PPI | End point | Results | Ref. |
| Cohort study | 12 yr | PPI: 83; no PPI: 176 | MI, CV death, urgent revascularization | No significant effect of use of PPIs | Collet et al[43] |
| Retrospective cohort study | 180 d | PPI: 3996; no PPI: 14 569 | MI, death or coronary revascularization | Adjusted RR for MI or death: 1.22 (95% CI: 0.99-1.51); for revascularization, 0.97 (95% CI: 0.79-1.21) | Rassen et al[47] |
| Retrospective cohort study | 1-yr | PPI: 397; no PPI: 138 | MI, death, CABG or repeat PCI | Death, MI events with PPI vs non-PPI groups: 6.7% vs 9.6% (P = 0.32); CABG with PPI vs non-PPI groups: 3.1% vs 4.1% (P = 0.53); revascularization with PPI vs non-PPI groups: 15.8% vs 14.2% (P = 0.65) | Ramirez et al[51] |
| Prospective, double-blind placebo- controlled multicentre RCT | Median of 133 d | PPI: 1801; no PPI: 1826 | Cardiovascular events (death, non-fatal MI, CABG or PCI, or ischemic stroke) | Cardiovascular events: HR: 1.02, 95% CI: 0.70-1.51 | Bhatt et al[53] |
| Double-blind randomized trial | 6 mo | PPI: 2257; no PPI: 4538 | MACE (CV death, MI, stroke) | MACE in PPI vs no PPI groups after adjustment for potential confounders: 11.8% vs 12.2%, adjusted HR: 0.94 (95% CI: 0.80-1.11, P = 0.46) | O’Donoghue et al[26] |
| Retrospective cohort study (FAST-MI Registry) | 1 yr | PPI: 1453; no PPI: 900 | Death, MI, or stroke | No in-hospital difference in death, reinfarction, or major bleeding in PPI vs no PPI groups; Death, MI, or stroke at 1 yr in PPI. no PPI groups: 12% vs 14% (P = 0.72), adjusted OR: 0.98 (95% CI: 0.90-1.08) | Simon et al[54] |
PPI: Proton pump inhibitor; PCI: Percutaneous coronary intervention; MI: Myocardial infarction; RR: Relative risk; CV: Cardiovascular.
In summary, these articles did not show drug interactions between PPIs and clopidogrel in terms of increasing the risk of CV death, nonfatal MI, or stroke in patients with ACS.
DISCUSSION/RECOMMENDATIONS
ADP-induced platelet aggregation of clopidogrel has been shown to be reduced in patients receiving omeprazole or other PPIs[19,29,43,55,56], previous retrospective cohort studies[21,23-25,46,48] and a meta-analysis[50] have indicated that concomitant use of PPIs and clopidogrel may be associated with an increased risk of CV events. However, a systematic review and meta-analysis have claimed that these previous studies had significant heterogeneity, which indicates that the evidence is biased, confounded or inconsistent. They have proposed that prospective randomized trials are required to investigate whether a cause-and-effect relationship truly exists regarding PPI-clopidogrel drug interactions[50]. Other articles have opposite opinions; many studies have reported that the use of PPIs had no effect on the clinical response to clopidogrel[26,38,39,51,53]. It is possible that biological differences detected by platelet function tests are not large enough to have clinical relevance. It is very common that clopidogrel and statins are used together in patients with coronary artery disease. There is some evidence to support a possible pharmacokinetic interaction between statins and clopidogrel. However, real-life interactions including hard end point studies seem to lack an association between the two drugs[57]. The United States FDA, on November 17, 2009, updated the public and health care professions about new safety information concerning a drug interaction between omeprazole and clopidogrel. The FDA recommends that co-administration of omeprazole and clopidogrel should be avoided because omeprazole reduces the effectiveness of clopidogrel[58]. This concern also extends to the use of esomeprazole when taken with clopidogrel. The results of new studies performed by the manufacturers of clopidogrel and submitted to FDA have indicated that co-administration of omeprazole and clopidogrel reduces plasma concentrations of the active metabolite of clopidogrel by about 45%, and the effect on platelet inhibition is reduced by as much as 47%. Other potent inhibitors of CYP2C19 including esomeprazole, cimetidine, fluconazole, ketoconazole, voriconazole, etravirine, felbamate, fluoxetine, fluvoxamine and ticlopidine are expected to have a similar effect as omeprazole and should also be avoided[58]. The European Medicines Agency, has also indicated that concomitant use of PPI and clopidogrel-containing medicines should be avoided unless absolutely necessary[59]. Nevertheless, the current totality of evidence does not justify a conclusion that PPIs are associated with CV events among clopidogrel users. How to respond to the PPI-clopidogrel interaction remains a matter of debate. Some have suggested that PPIs should simply be avoided in patients taking clopidogrel. This is not good advice and reflects oversimplification of an exceedingly complex topic. Others have argued that the PPI-clopidogrel interaction is of no consequence. Although it is probably true for many patients, the interactions do occur in a considerable number of cases. Health-care providers must make decisions for their patients in the present situation of conflicting evidence, and we therefore propose the following recommendations.
Patients who require clopidogrel should start and continue their therapy
The occurrence of stent thrombosis in patients with DESs may be associated with a poor outcome such as AMI or sudden cardiac death. In the Swedish Coronary Angiography and Angioplasty Registry, where 13 738 bare-metal stents (BMSs) and 6033 DES patients were followed up for 3 years[60], the authors found that late stent thrombosis in the DES group was associated with an increased rate of death. Patients with DESs had an 18% increase in the relative long-term risk of death, compared with patients with BMSs. The FDA and advisory reports from the American Heart Association (AHA), American College of Cardiology, Society for Cardiovascular Angiography and Interventions, and American College of Surgeons have recommended that antiplatelet agents such as aspirin or clopidogrel should be used for at least 1 year following the use of a DES[58,61]. Similar reports have also stressed the importance of 12 mo dual antiplatelet therapy after placement of a DES in patients with a low risk for bleeding[62,63]. Thus, continued clopidogrel therapy is recommended because it is beneficial for decreasing the adverse outcome in patients who require the drug.
Identify the risk of GI ulcer and bleeding; high-risk patients should receive PPI therapy
A meta-analysis of 22 trials of daily low-dose aspirin vs placebo in > 57 000 patients revealed an RR of 1.7 for major bleeding and 2.07 for significant GI bleeding, without any difference between a daily dose of 75-162.5 mg and 162.5-325 mg[64]. Upper GI events, such as symptomatic or complicated ulcers, occur in 1 in 20 NSAID users and in 1 in 7 older adults using NSAIDs[65], which accounts for 30% of related hospitalization and death[66,67]. Endoscopic trials suggest that the GI toxicity of a coxib plus aspirin is additive, which results in an overall risk of endoscopic ulcer formation[68,69]. In the Clopidogrel in Unstable angina to prevent Recurrent Events study, 1.3% of patients who received clopidogrel on top of aspirin had major GI hemorrhage as compared to 0.7% of patients treated with aspirin alone. This indicates that the risk of major bleeding is increased among patients treated with clopidogrel in addition to aspirin[70]. A consensus document approved by the American College of Cardiology Foundation (ACCF), American College of Gastroenterology and AHA in 2008 strongly recommends the administration of PPIs to decrease peptic ulcer or GI bleeding in high-risk patients[71]. Patients that receive aspirin or dual antiplatelet therapy may have a high risk of peptic ulcer or GI bleeding if they present with symptoms of dyspepsia or persistent epigastric pain, or have a history of previous GI bleeding, and concomitant use of NSAID or oral anticoagulants. These patients should receive PPIs to decrease peptic ulcer or GI bleeding in high-risk patients[71].
Consider using pantoprazole when a PPI is indicated
This recommendation is based on the observation that pantoprazole is less potent than omeprazole to inhibit CYP2C19[40] and does not appear to attenuate the pharmacodynamic response to clopidogrel[72,73]. Co-administration of pantoprazole may enhance the antiplatelet effect of enteric-coated aspirin in patients with ACS, who are undergoing PCI and dual antiplatelet therapy[74]. Furthermore, it has been reported that pantoprazole had no association with recurrent MI in a large population-based, case-control study of patients receiving clopidogrel[23].
Histamine-2-receptor antagonist can be used as an alternative to PPIs for GI protection
Concomitant use of clopidogrel and an NSAID (including low-dose aspirin) has been associated with impaired healing of asymptomatic ulcers[75] and disruption of platelet aggregation[76], with a consequent increase in serious upper GI events (OR: 7.4, 95% CI: 3.5-15)[77]. Histamine-2-receptor antagonists are able to decrease peptic ulcer or esophagitis in low-dose aspirin users[78]. Famotidine is a histamine H2-receptor antagonist that is well tolerated and able to prevent and heal peptic ulcers in patients who are receiving conventional NSAIDs[79,80]. The FAMOUS trial (Famotidine for the Prevention of Peptic Ulcers in Users of Low-dose Aspirin) was a randomized, double-blind, placebo-controlled trial, which demonstrated that famotidine prevented gastric and duodenal ulcers, and erosive esophagitis in patients taking low-dose aspirin (i.e. 75-325 mg)[81]. Concerning the long-term use of PPIs, an alternative management strategy has been proposed, including the use of H2-receptor antagonists[81,82]. In other words, H2-receptor antagonists such as famotidine might be considered as a useful alternative in patients with drug interactions between clopidogrel and PPIs.
Think about other alternative antiplatelet therapy to avoid interaction between clopidogrel and PPIs
Prasugrel is a third-generation thienopyridine with more consistent and efficient metabolism than clopidogrel. Prasugrel appears less susceptible to genetic variation and drug interactions, which is the limitation of clopidogrel in antiplatelet activity[83-85]. Previous studies have reported that the prasugrel has greater potency and more rapid platelet inhibition than clopidogrel, and has a comparable safety profile[86,87]. In a retrospective analysis of the TRITON-TIMI 38 study, a randomized controlled trial that compared prasugrel and clopidogrel in > 13 000 patients with ACS, there was a 19% RR reduction in the composite CV endpoint with prasugrel vs clopidogrel, but with increased major bleeding[88].
Another direct-acting inhibitor of the ADP receptor P2Y12 is ticagrelor, which has a more rapid onset and more pronounced platelet inhibition than clopidogrel[89]. Gurbel et al[90] has recently reported that ticagrelor therapy may overcome the nonresponsiveness to clopidogrel, and in their study, almost all clopidogrel nonresponders and responders treated with ticagrelor had platelet reactivity below the cut-off points associated with ischemic risk. An important randomized, double-blind, multicenter, clinical study, the PLATO trial has recently been conducted to compare the efficacy of ticagrelor and clopidogrel in 18 624 patients with ACS. Treatment with ticagrelor compared with clopidogrel significantly reduced the rate of death from vascular causes, MI, or stroke (HR: 0.84, 95% CI: 0.77-0.92, P < 0.001), without an increase in the rate of overall major bleeding, but with an increase in the rate of non-procedure-related bleeding[27]. In view of the above evidence and the drug interaction between clopidogrel and PPIs, newer drugs such as prasugrel or ticagrelor may have the potential to overcome the limitations of clopidogrel.
When dual therapy is necessary, separation of PPI and clopidogrel for > 12 h
PPIs and clopidogrel are each given once daily and both have relatively short half lives of 1-2 h and 4-6 h, respectively[39,91]. The clopidogrel concentrations should be very low or unmeasurable at 4-6 h after ingestion[91]. Besides, clopidogrel is most effective when taken before a meal. Thus, separation of 12-15 h between these two drugs should theoretically prevent any competitive inhibition of CYP2C19 metabolism and avoid any adverse clinical effects. We therefore suggest taking PPI before breakfast and clopidogrel at bedtime.
CONCLUSION
To date, there remains significant ongoing controversy regarding the clinical outcomes of patients taking clopidogrel and PPIs. From the ACCF Task Force on Clinical Expert Consensus Documents, clinicians should pay attention to gastroprotection strategies that involve PPIs in patients with a high risk of GI bleeding, and eradication of H. pylori in patients with peptic ulcer history who receive dual-antiplatelet therapy[71]. In situations when both clopidogrel and a PPI are indicated, pantoprazole should be used because it is the PPI that is least likely to interact with clopidogrel. Famotidine may be an appropriate alternative for patients who require acid-lowering therapy[78,81]. Until further reliable data become available, wide separation of PPIs and clopidogrel could minimize the potential clinical drug interactions.
Footnotes
Peer reviewers: Gergely Feher MD, PhD, Department of Neurology, Medical School, University of Pecs, 2 Ret str., Pecs, Baranya, H-7623, Hungary; Armen Yuri Gasparyan, MD, PhD, FESC, Associate Professor of Medicine, Postdoctoral Research Fellow, Clinical Research Unit, Dudley Group of Hospitals NHS Foundation Trust, Russell’s Hall Hospital, Pensnett Road, Dudley, West Midlands, DY1 2HQ, United Kingdom; Arshad Ali, MD, FACC, FSCAI, MRCP, Associate Medical director, Kentucky Heart Foundation, Kings Dauhters Medical Center, Suite 10, Ashland, KY 41101, United States; Tien MH Ng, PhD, BCPS, Associate Professor of Clinical Pharmacy Director, PGY2 Residency in Cardiology, University of Southern California, School of Pharmacy 1985 Zonal Ave, Los Angeles, CA 90033, United States
Supported by (in part) The Kaohsiung Veterans General Hospital, Grant No. VGHKS98-034
S- Editor Cheng JX L- Editor Kerr C E- Editor Zheng XM
References
- 1.Easthope SE, Jarvis B. Clopidogrel: potential in the prevention of cardiovascular events in patients with acute coronary syndromes. Am J Cardiovasc Drugs. 2001;1:467–74; discussion 475-6. doi: 10.2165/00129784-200101060-00006. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 3.Chen ZM, Jiang LX, Chen YP, Xie JX, Pan HC, Peto R, Collins R, Liu LS. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366:1607–1621. doi: 10.1016/S0140-6736(05)67660-X. [DOI] [PubMed] [Google Scholar]
- 4.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Chavey WE, Fesmire FM, Hochman JS, Levin TN, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50:e1–e157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 5.King SB, Smith SC, Hirshfeld JW, Jacobs AK, Morrison DA, Williams DO, Feldman TE, Kern MJ, O'Neill WW, Schaff HV, et al. 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee. Circulation. 2008;117:261–295. doi: 10.1161/CIRCULATIONAHA.107.188208. [DOI] [PubMed] [Google Scholar]
- 6.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, et al. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. [DOI] [PubMed] [Google Scholar]
- 7.Grines CL, Bonow RO, Casey DE, Gardner TJ, Lockhart PB, Moliterno DJ, O'Gara P, Whitlow P. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007;49:734–739. doi: 10.1016/j.jacc.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Bavry AA, Bhatt DL. Appropriate use of drug-eluting stents: balancing the reduction in restenosis with the concern of late thrombosis. Lancet. 2008;371:2134–2143. doi: 10.1016/S0140-6736(08)60922-8. [DOI] [PubMed] [Google Scholar]
- 9.Gilard M, Arnaud B, Le Gal G, Abgrall JF, Boschat J. Influence of omeprazol on the antiplatelet action of clopidogrel associated to aspirin. J Thromb Haemost. 2006;4:2508–2509. doi: 10.1111/j.1538-7836.2006.02162.x. [DOI] [PubMed] [Google Scholar]
- 10.Bonvini RF, Reny JL, Mach F, Zeller T, Fontana P. Acute coronary syndrome and its antithrombotic treatment: focus on aspirin and clopidogrel resistance. Curr Vasc Pharmacol. 2009;7:198–208. doi: 10.2174/157016109787455662. [DOI] [PubMed] [Google Scholar]
- 11.Sharma RK, Reddy HK, Singh VN, Sharma R, Voelker DJ, Bhatt G. Aspirin and clopidogrel hyporesponsiveness and nonresponsiveness in patients with coronary artery stenting. Vasc Health Risk Manag. 2009;5:965–972. doi: 10.2147/vhrm.s6787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gasparyan AY, Watson T, Lip GY. The role of aspirin in cardiovascular prevention: implications of aspirin resistance. J Am Coll Cardiol. 2008;51:1829–1843. doi: 10.1016/j.jacc.2007.11.080. [DOI] [PubMed] [Google Scholar]
- 13.Vila PM, Zafar MU, Badimon JJ. Platelet reactivity and nonresponse to dual antiplatelet therapy: a review. Platelets. 2009;20:531–538. doi: 10.3109/09537100903261379. [DOI] [PubMed] [Google Scholar]
- 14.Feher G, Feher A, Pusch G, Koltai K, Tibold A, Gasztonyi B, Papp E, Szapary L, Kesmarky G, Toth K. Clinical importance of aspirin and clopidogrel resistance. World J Cardiol. 2010;2:171–186. doi: 10.4330/wjc.v2.i7.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonello L, Camoin-Jau L, Arques S, Boyer C, Panagides D, Wittenberg O, Simeoni MC, Barragan P, Dignat-George F, Paganelli F. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol. 2008;51:1404–1411. doi: 10.1016/j.jacc.2007.12.044. [DOI] [PubMed] [Google Scholar]
- 16.Wenaweser P, Dörffler-Melly J, Imboden K, Windecker S, Togni M, Meier B, Haeberli A, Hess OM. Stent thrombosis is associated with an impaired response to antiplatelet therapy. J Am Coll Cardiol. 2005;45:1748–1752. doi: 10.1016/j.jacc.2005.01.058. [DOI] [PubMed] [Google Scholar]
- 17.Feher G, Koltai K, Alkonyi B, Papp E, Keszthelyi Z, Kesmarky G, Toth K. Clopidogrel resistance: role of body mass and concomitant medications. Int J Cardiol. 2007;120:188–192. doi: 10.1016/j.ijcard.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 18.Foussas SG, Zairis MN, Patsourakos NG, Makrygiannis SS, Adamopoulou EN, Handanis SM, Prekates AA, Fakiolas CN, Pissimissis EG, Olympios CD, et al. The impact of oral antiplatelet responsiveness on the long-term prognosis after coronary stenting. Am Heart J. 2007;154:676–681. doi: 10.1016/j.ahj.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 19.Gilard M, Arnaud B, Cornily JC, Le Gal G, Lacut K, Le Calvez G, Mansourati J, Mottier D, Abgrall JF, Boschat J. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double-blind OCLA (Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol. 2008;51:256–260. doi: 10.1016/j.jacc.2007.06.064. [DOI] [PubMed] [Google Scholar]
- 20.Huang CC, Chen YC, Leu HB, Chen TJ, Lin SJ, Chan WL, Chen JW. Risk of adverse outcomes in Taiwan associated with concomitant use of clopidogrel and proton pump inhibitors in patients who received percutaneous coronary intervention. Am J Cardiol. 2010;105:1705–1709. doi: 10.1016/j.amjcard.2010.01.348. [DOI] [PubMed] [Google Scholar]
- 21.Pezalla E, Day D, Pulliadath I. Initial assessment of clinical impact of a drug interaction between clopidogrel and proton pump inhibitors. J Am Coll Cardiol. 2008;52:1038–109; author reply 1039. doi: 10.1016/j.jacc.2008.05.053. [DOI] [PubMed] [Google Scholar]
- 22.Gupta E, Bansal D, Sotos J, Olden K. Risk of adverse clinical outcomes with concomitant use of clopidogrel and proton pump inhibitors following percutaneous coronary intervention. Dig Dis Sci. 2010;55:1964–1968. doi: 10.1007/s10620-009-0960-8. [DOI] [PubMed] [Google Scholar]
- 23.Juurlink DN, Gomes T, Ko DT, Szmitko PE, Austin PC, Tu JV, Henry DA, Kopp A, Mamdani MM. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009;180:713–718. doi: 10.1503/cmaj.082001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ho PM, Maddox TM, Wang L, Fihn SD, Jesse RL, Peterson ED, Rumsfeld JS. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301:937–944. doi: 10.1001/jama.2009.261. [DOI] [PubMed] [Google Scholar]
- 25.Kreutz RP, Stanek EJ, Aubert R, Yao J, Breall JA, Desta Z, Skaar TC, Teagarden JR, Frueh FW, Epstein RS, et al. Impact of proton pump inhibitors on the effectiveness of clopidogrel after coronary stent placement: the clopidogrel Medco outcomes study. Pharmacotherapy. 2010;30:787–796. doi: 10.1592/phco.30.8.787. [DOI] [PubMed] [Google Scholar]
- 26.O'Donoghue ML, Braunwald E, Antman EM, Murphy SA, Bates ER, Rozenman Y, Michelson AD, Hautvast RW, Ver Lee PN, Close SL, et al. Pharmacodynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials. Lancet. 2009;374:989–997. doi: 10.1016/S0140-6736(09)61525-7. [DOI] [PubMed] [Google Scholar]
- 27.Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 28.Mehta SR, Tanguay JF, Eikelboom JW, Jolly SS, Joyner CD, Granger CB, Faxon DP, Rupprecht HJ, Budaj A, Avezum A, et al. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet. 2010;376:1233–1243. doi: 10.1016/S0140-6736(10)61088-4. [DOI] [PubMed] [Google Scholar]
- 29.Norgard NB, Mathews KD, Wall GC. Drug-drug interaction between clopidogrel and the proton pump inhibitors. Ann Pharmacother. 2009;43:1266–1274. doi: 10.1345/aph.1M051. [DOI] [PubMed] [Google Scholar]
- 30.Kurihara A, Hagihara K, Kazui M, Ozeki T, Farid NA, Ikeda T. In vitro metabolism of antiplatelet agent clopidogrel: cytochrome P450 isoforms responsible for two oxidation steps involved in the active metabolite formation. Drug Metab Rev. 2005;37(Suppl 2):99. [Google Scholar]
- 31.Paré G, Mehta SR, Yusuf S, Anand SS, Connolly SJ, Hirsh J, Simonsen K, Bhatt DL, Fox KA, Eikelboom JW. Effects of CYP2C19 genotype on outcomes of clopidogrel treatment. N Engl J Med. 2010;363:1704–1714. doi: 10.1056/NEJMoa1008410. [DOI] [PubMed] [Google Scholar]
- 32.Farid NA, Payne CD, Small DS, Winters KJ, Ernest CS, Brandt JT, Darstein C, Jakubowski JA, Salazar DE. Cytochrome P450 3A inhibition by ketoconazole affects prasugrel and clopidogrel pharmacokinetics and pharmacodynamics differently. Clin Pharmacol Ther. 2007;81:735–741. doi: 10.1038/sj.clpt.6100139. [DOI] [PubMed] [Google Scholar]
- 33.Farid NA, Small DS, Payne CD, Jakubowski JA, Brandt JT, Li YG, Ernest CS, Salazar DE, Konkoy CS, Winters KJ. Effect of atorvastatin on the pharmacokinetics and pharmacodynamics of prasugrel and clopidogrel in healthy subjects. Pharmacotherapy. 2008;28:1483–1494. doi: 10.1592/phco.28.12.1483. [DOI] [PubMed] [Google Scholar]
- 34.Chen BL, Zhang W, Li Q, Li YL, He YJ, Fan L, Wang LS, Liu ZQ, Zhou HH. Inhibition of ADP-induced platelet aggregation by clopidogrel is related to CYP2C19 genetic polymorphisms. Clin Exp Pharmacol Physiol. 2008;35:904–908. doi: 10.1111/j.1440-1681.2008.04915.x. [DOI] [PubMed] [Google Scholar]
- 35.Cerletti C, Dell'Elba G, Manarini S, Pecce R, Di Castelnuovo A, Scorpiglione N, Feliziani V, de Gaetano G. Pharmacokinetic and pharmacodynamic differences between two low dosages of aspirin may affect therapeutic outcomes. Clin Pharmacokinet. 2003;42:1059–1070. doi: 10.2165/00003088-200342120-00004. [DOI] [PubMed] [Google Scholar]
- 36.Oliphant CS, Doby JB, Blade CL, Das K, Mukherjee D, Das P. Emerging P2Y12 receptor antagonists: role in coronary artery disease. Curr Vasc Pharmacol. 2010;8:93–101. doi: 10.2174/157016110790226615. [DOI] [PubMed] [Google Scholar]
- 37.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 38.Desta Z, Zhao X, Shin JG, Flockhart DA. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin Pharmacokinet. 2002;41:913–958. doi: 10.2165/00003088-200241120-00002. [DOI] [PubMed] [Google Scholar]
- 39.Shi S, Klotz U. Proton pump inhibitors: an update of their clinical use and pharmacokinetics. Eur J Clin Pharmacol. 2008;64:935–951. doi: 10.1007/s00228-008-0538-y. [DOI] [PubMed] [Google Scholar]
- 40.Li XQ, Andersson TB, Ahlström M, Weidolf L. Comparison of inhibitory effects of the proton pump-inhibiting drugs omeprazole, esomeprazole, lansoprazole, pantoprazole, and rabeprazole on human cytochrome P450 activities. Drug Metab Dispos. 2004;32:821–827. doi: 10.1124/dmd.32.8.821. [DOI] [PubMed] [Google Scholar]
- 41.Fock KM, Ang TL, Bee LC, Lee EJ. Proton pump inhibitors: do differences in pharmacokinetics translate into differences in clinical outcomes? Clin Pharmacokinet. 2008;47:1–6. doi: 10.2165/00003088-200847010-00001. [DOI] [PubMed] [Google Scholar]
- 42.Stedman CA, Barclay ML. Review article: comparison of the pharmacokinetics, acid suppression and efficacy of proton pump inhibitors. Aliment Pharmacol Ther. 2000;14:963–978. doi: 10.1046/j.1365-2036.2000.00788.x. [DOI] [PubMed] [Google Scholar]
- 43.Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, Silvain J, Payot L, Brugier D, Cayla G, Beygui F, et al. Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet. 2009;373:309–317. doi: 10.1016/S0140-6736(08)61845-0. [DOI] [PubMed] [Google Scholar]
- 44.Miao J, Liu R, Li Z. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:2250–2251. [PubMed] [Google Scholar]
- 45.Taubert D, Bouman HJ, van Werkum JW. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:2249–250; author reply 2251. doi: 10.1056/NEJMc090391. [DOI] [PubMed] [Google Scholar]
- 46.Dunn SP, Macaulay TE, Brennan DM, Campbell CL, Charnigo RJ, Smyth SS, Berger PB, Steinhubl SR, Topol EJ. Baseline proton pump inhibitor use is associated with increased cardiovascular events with and without the use of clopidogrel in the CREDO Trial. Circulation. 2008;118:S815. [Google Scholar]
- 47.Rassen JA, Choudhry NK, Avorn J, Schneeweiss S. Cardiovascular outcomes and mortality in patients using clopidogrel with proton pump inhibitors after percutaneous coronary intervention or acute coronary syndrome. Circulation. 2009;120:2322–2329. doi: 10.1161/CIRCULATIONAHA.109.873497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gaglia MA, Torguson R, Hanna N, Gonzalez MA, Collins SD, Syed AI, Ben-Dor I, Maluenda G, Delhaye C, Wakabayashi K, et al. Relation of proton pump inhibitor use after percutaneous coronary intervention with drug-eluting stents to outcomes. Am J Cardiol. 2010;105:833–838. doi: 10.1016/j.amjcard.2009.10.063. [DOI] [PubMed] [Google Scholar]
- 49.Muñoz-Torrero JF, Escudero D, Suárez C, Sanclemente C, Pascual MT, Zamorano J, Trujillo-Santos J, Monreal M. Concomitant use of proton pump inhibitors and clopidogrel in patients with coronary, cerebrovascular, or peripheral artery disease in the factores de riesgo y enfermedad arterial (FRENA) registry. J Cardiovasc Pharmacol. 2011;57:13–19. doi: 10.1097/FJC.0b013e3181fc65e5. [DOI] [PubMed] [Google Scholar]
- 50.Siller-Matula JM, Jilma B, Schrör K, Christ G, Huber K. Effect of proton pump inhibitors on clinical outcome in patients treated with clopidogrel: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:2624–2641. doi: 10.1111/j.1538-7836.2010.04049.x. [DOI] [PubMed] [Google Scholar]
- 51.Siller-Matula JM, Jilma B, Schrör K, Christ G, Huber K. Effect of proton pump inhibitors on clinical outcome in patients treated with clopidogrel: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:2624–2641. doi: 10.1111/j.1538-7836.2010.04049.x. [DOI] [PubMed] [Google Scholar]
- 52.Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Méneveau N, Steg PG, Ferrières J, Danchin N, Becquemont L. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009;360:363–375. doi: 10.1056/NEJMoa0808227. [DOI] [PubMed] [Google Scholar]
- 53.Bhatt DL, Cryer BL, Contant CF, Cohen M, Lanas A, Schnitzer TJ, Shook TL, Lapuerta P, Goldsmith MA, Laine L, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010;363:1909–1917. doi: 10.1056/NEJMoa1007964. [DOI] [PubMed] [Google Scholar]
- 54.Simon T, Steg PG, Gilard M, Blanchard D, Bonello L, Hanssen M, Lardoux H, Coste P, Lefèvre T, Drouet E, et al. Clinical events as a function of proton pump inhibitor use, clopidogrel use, and cytochrome P450 2C19 genotype in a large nationwide cohort of acute myocardial infarction: results from the French Registry of Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) registry. Circulation. 2011;123:474–482. doi: 10.1161/CIRCULATIONAHA.110.965640. [DOI] [PubMed] [Google Scholar]
- 55.VandenBranden M, Ring BJ, Binkley SN, Wrighton SA. Interaction of human liver cytochromes P450 in vitro with LY307640, a gastric proton pump inhibitor. Pharmacogenetics. 1996;6:81–91. doi: 10.1097/00008571-199602000-00007. [DOI] [PubMed] [Google Scholar]
- 56.Howden CW. Clinical pharmacology of omeprazole. Clin Pharmacokinet. 1991;20:38–49. doi: 10.2165/00003088-199120010-00003. [DOI] [PubMed] [Google Scholar]
- 57.Bhindi R, Ormerod O, Newton J, Banning AP, Testa L. Interaction between statins and clopidogrel: is there anything clinically relevant? QJM. 2008;101:915–925. doi: 10.1093/qjmed/hcn089. [DOI] [PubMed] [Google Scholar]
- 58.Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC) November 17, 2009. Available from: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm190784.htm.
- 59.European Medicines Agency. Public statement on possible interaction between clopidogrel and proton pump inhibitors. Available from: http://www.emea.europa.eu/humandocs/PDFs/EPAR/Plavix/32895609en.pdf.
- 60.Lagerqvist B, James SK, Stenestrand U, Lindbäck J, Nilsson T, Wallentin L. Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med. 2007;356:1009–1019. doi: 10.1056/NEJMoa067722. [DOI] [PubMed] [Google Scholar]
- 61.Grines CL, Bonow RO, Casey DE, Gardner TJ, Lockhart PB, Moliterno DJ, O'Gara P, Whitlow P. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Catheter Cardiovasc Interv. 2007;69:334–340. doi: 10.1002/ccd.21124. [DOI] [PubMed] [Google Scholar]
- 62.Smith SC, Feldman TE, Hirshfeld JW, Jacobs AK, Kern MJ, King SB, Morrison DA, O'Neill WW, Schaff HV, Whitlow PL, et al. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention--summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention) Circulation. 2006;113:156–175. doi: 10.1161/CIRCULATIONAHA.105.170815. [DOI] [PubMed] [Google Scholar]
- 63.Maisel WH. Unanswered questions--drug-eluting stents and the risk of late thrombosis. N Engl J Med. 2007;356:981–984. doi: 10.1056/NEJMp068305. [DOI] [PubMed] [Google Scholar]
- 64.McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006;119:624–638. doi: 10.1016/j.amjmed.2005.10.039. [DOI] [PubMed] [Google Scholar]
- 65.Bombardier C, Laine L, Reicin A, Shapiro D, Burgos-Vargas R, Davis B, Day R, Ferraz MB, Hawkey CJ, Hochberg MC, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343:1520–158, 2 p following 1528. doi: 10.1056/NEJM200011233432103. [DOI] [PubMed] [Google Scholar]
- 66.Griffin MR, Piper JM, Daugherty JR, Snowden M, Ray WA. Nonsteroidal anti-inflammatory drug use and increased risk for peptic ulcer disease in elderly persons. Ann Intern Med. 1991;114:257–263. doi: 10.7326/0003-4819-114-4-257. [DOI] [PubMed] [Google Scholar]
- 67.Smalley WE, Ray WA, Daugherty JR, Griffin MR. Nonsteroidal anti-inflammatory drugs and the incidence of hospitalizations for peptic ulcer disease in elderly persons. Am J Epidemiol. 1995;141:539–545. doi: 10.1093/oxfordjournals.aje.a117469. [DOI] [PubMed] [Google Scholar]
- 68.Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastrointestinal complications. J Rheumatol Suppl. 1999;56:18–24. [PubMed] [Google Scholar]
- 69.Lanas A, Bajador E, Serrano P, Fuentes J, Carreño S, Guardia J, Sanz M, Montoro M, Sáinz R. Nitrovasodilators, low-dose aspirin, other nonsteroidal antiinflammatory drugs, and the risk of upper gastrointestinal bleeding. N Engl J Med. 2000;343:834–839. doi: 10.1056/NEJM200009213431202. [DOI] [PubMed] [Google Scholar]
- 70.Peters RJ, Mehta SR, Fox KA, Zhao F, Lewis BS, Kopecky SL, Diaz R, Commerford PJ, Valentin V, Yusuf S. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003;108:1682–1687. doi: 10.1161/01.CIR.0000091201.39590.CB. [DOI] [PubMed] [Google Scholar]
- 71.Bhatt DL, Scheiman J, Abraham NS, Antman EM, Chan FK, Furberg CD, Johnson DA, Mahaffey KW, Quigley EM. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2008;118:1894–1909. doi: 10.1161/CIRCULATIONAHA.108.191087. [DOI] [PubMed] [Google Scholar]
- 72.Cuisset T, Frere C, Quilici J, Poyet R, Gaborit B, Bali L, Brissy O, Morange PE, Alessi MC, Bonnet JL. Comparison of omeprazole and pantoprazole influence on a high 150-mg clopidogrel maintenance dose the PACA (Proton Pump Inhibitors And Clopidogrel Association) prospective randomized study. J Am Coll Cardiol. 2009;54:1149–1153. doi: 10.1016/j.jacc.2009.05.050. [DOI] [PubMed] [Google Scholar]
- 73.Siller-Matula JM, Spiel AO, Lang IM, Kreiner G, Christ G, Jilma B. Effects of pantoprazole and esomeprazole on platelet inhibition by clopidogrel. Am Heart J. 2009;157:148.e1–148.e5. doi: 10.1016/j.ahj.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 74.Kasprzak M, Koziński M, Bielis L, Boinska J, Plazuk W, Marciniak A, Budzyński J, Siller-Matula J, Rość D, Kubica J. Pantoprazole may enhance antiplatelet effect of enteric-coated aspirin in patients with acute coronary syndrome. Cardiol J. 2009;16:535–544. [PubMed] [Google Scholar]
- 75.Ma L, Elliott SN, Cirino G, Buret A, Ignarro LJ, Wallace JL. Platelets modulate gastric ulcer healing: role of endostatin and vascular endothelial growth factor release. Proc Natl Acad Sci U S A. 2001;98:6470–6475. doi: 10.1073/pnas.111150798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sheikh RA, Romano PS, Prindiville TP, Yasmeen S, Trudeau W. Endoscopic evidence of mucosal injury in patients taking ticlopidine compared with patients taking aspirin/nonsteroidal antiinflammatory drugs and controls. J Clin Gastroenterol. 2002;34:529–532. doi: 10.1097/00004836-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 77.Hallas J, Dall M, Andries A, Andersen BS, Aalykke C, Hansen JM, Andersen M, Lassen AT. Use of single and combined antithrombotic therapy and risk of serious upper gastrointestinal bleeding: population based case-control study. BMJ. 2006;333:726. doi: 10.1136/bmj.38947.697558.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Feldman M, Burton ME. Histamine2-receptor antagonists. Standard therapy for acid-peptic diseases (2) N Engl J Med. 1990;323:1749–1755. doi: 10.1056/NEJM199012203232507. [DOI] [PubMed] [Google Scholar]
- 79.Taha AS, Hudson N, Hawkey CJ, Swannell AJ, Trye PN, Cottrell J, Mann SG, Simon TJ, Sturrock RD, Russell RI. Famotidine for the prevention of gastric and duodenal ulcers caused by nonsteroidal antiinflammatory drugs. N Engl J Med. 1996;334:1435–1439. doi: 10.1056/NEJM199605303342204. [DOI] [PubMed] [Google Scholar]
- 80.Hudson N, Taha AS, Russell RI, Trye P, Cottrell J, Mann SG, Swanell AJ, Sturrock RD, Hawkey CJ. Famotidine for healing and maintenance in nonsteroidal anti-inflammatory drug-associated gastroduodenal ulceration. Gastroenterology. 1997;112:1817–1822. doi: 10.1053/gast.1997.v112.pm9178671. [DOI] [PubMed] [Google Scholar]
- 81.Taha AS, McCloskey C, Prasad R, Bezlyak V. Famotidine for the prevention of peptic ulcers and oesophagitis in patients taking low-dose aspirin (FAMOUS): a phase III, randomised, double-blind, placebo-controlled trial. Lancet. 2009;374:119–125. doi: 10.1016/S0140-6736(09)61246-0. [DOI] [PubMed] [Google Scholar]
- 82.Chan FK. Proton-pump inhibitors in peptic ulcer disease. Lancet. 2008;372:1198–1200. doi: 10.1016/S0140-6736(08)61497-X. [DOI] [PubMed] [Google Scholar]
- 83.Hagihara K, Kazui M, Kurihara A, Yoshiike M, Honda K, Okazaki O, Farid NA, Ikeda T. A possible mechanism for the differences in efficiency and variability of active metabolite formation from thienopyridine antiplatelet agents, prasugrel and clopidogrel. Drug Metab Dispos. 2009;37:2145–2152. doi: 10.1124/dmd.109.028498. [DOI] [PubMed] [Google Scholar]
- 84.Wiviott SD, Trenk D, Frelinger AL, O'Donoghue M, Neumann FJ, Michelson AD, Angiolillo DJ, Hod H, Montalescot G, Miller DL, et al. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: the Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007;116:2923–2932. doi: 10.1161/CIRCULATIONAHA.107.740324. [DOI] [PubMed] [Google Scholar]
- 85.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias WL, Braunwald E, et al. Cytochrome P450 genetic polymorphisms and the response to prasugrel: relationship to pharmacokinetic, pharmacodynamic, and clinical outcomes. Circulation. 2009;119:2553–2560. doi: 10.1161/CIRCULATIONAHA.109.851949. [DOI] [PubMed] [Google Scholar]
- 86.Michelson AD, Frelinger AL, Braunwald E, Downey WE, Angiolillo DJ, Xenopoulos NP, Jakubowski JA, Li Y, Murphy SA, Qin J, et al. Pharmacodynamic assessment of platelet inhibition by prasugrel vs. clopidogrel in the TRITON-TIMI 38 trial. Eur Heart J. 2009;30:1753–1763. doi: 10.1093/eurheartj/ehp159. [DOI] [PubMed] [Google Scholar]
- 87.Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 88.Montalescot G, Wiviott SD, Braunwald E, Murphy SA, Gibson CM, McCabe CH, Antman EM. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction (TRITON-TIMI 38): double-blind, randomised controlled trial. Lancet. 2009;373:723–731. doi: 10.1016/S0140-6736(09)60441-4. [DOI] [PubMed] [Google Scholar]
- 89.Gurbel PA, Bliden KP, Butler K, Tantry US, Gesheff T, Wei C, Teng R, Antonino MJ, Patil SB, Karunakaran A, Kereiakes DJ, Parris C, Purdy D, Wilson V, Ledley GS, Storey RF. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study. Circulation. 2009;120:2577–2585. doi: 10.1161/CIRCULATIONAHA.109.912550. [DOI] [PubMed] [Google Scholar]
- 90.Gurbel PA, Bliden KP, Butler K, Antonino MJ, Wei C, Teng R, Rasmussen L, Storey RF, Nielsen T, Eikelboom JW, Sabe-Affaki G, Husted S, Kereiakes DJ, Henderson D, Patel DV, Tantry US. Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: the RESPOND study. Circulation. 2010;121:1188–1199. doi: 10.1161/CIRCULATIONAHA.109.919456. [DOI] [PubMed] [Google Scholar]
- 91.Kim KA, Park PW, Hong SJ, Park JY. The effect of CYP2C19 polymorphism on the pharmacokinetics and pharmacodynamics of clopidogrel: a possible mechanism for clopidogrel resistance. Clin Pharmacol Ther. 2008;84:236–242. doi: 10.1038/clpt.2008.20. [DOI] [PubMed] [Google Scholar]


