Abstract
Background.
Self-neglect is the behavior of an elderly person that threatens his or her own health and safety, and it is associated with increased morbidity and mortality. Although report of self-neglect is more common among black older adults, the racial/ethnic differences in mortality remain unclear.
Methods.
The Chicago Healthy Aging Project is a population-based cohort study conducted from 1993 to 2005. A subset of these participants were suspected to self-neglect and were reported to a social services agency. Mortality was ascertained during follow-up and from the National Death Index. Cox proportional hazards models were used to assess the mortality risk.
Results.
In the total cohort, there were 5,963 black and 3,475 white older adults, and of these, 1,479 were reported for self-neglect (21.7% in black and 5.3% in white older adults). In multivariable analyses with extensive adjustments, the interaction term indicated that impact of self-neglect on mortality was significantly stronger in black than in white older adults (parameter estimate, 0.54, SE, 0.14, p < .001). This difference persisted over time. In race/ethnicity-stratified analyses, at 6 months after report of self-neglect, the hazard ratio for black older adults was 5.00 (95% confidence interval, 4.47–5.59) and for white older adults was 2.75 (95% confidence interval, 2.19–3.44). At 3 years after report, the hazard ratios were 2.61 (95% confidence interval, 2.25–3.04) and 1.47 (95% confidence interval, 1.10–1.96) for black older adults and white older adults, respectively.
Conclusions.
Future studies are needed to qualify the casual mechanisms between self-neglect and mortality in black and white older adults in order to devise targeted prevention and intervention strategies.
Keywords: Self-neglect, Health disparity, Population-based study, Race/ethnicity, Mortality
SELF-NEGLECT is a pervasive public health issue across all racial/ethnic groups. There are an estimated 1.2 million older adults who self-neglect annually in the United States (1), and data from social services agencies suggest that self-neglect report may be rising (2). According to the National Center on Elder Abuse, self-neglect is defined “ … as the behavior of an elderly person that threatens his/her own health and safety. Self-neglect generally manifests itself in an older person as a refusal or failure to provide himself/herself with adequate food, water, clothing, shelter, personal hygiene, medication (when indicated), and safety precautions” (3). After self-neglect cases are reported to social services agencies and upon investigation, some are confirmed, whereas others are not.
Although self-neglect is associated with adverse outcomes, there is little systematic information on racial/ethnic differences. Self-neglect is classified as a geriatric syndrome (4), a term often used to capture heterogeneous clinical conditions in older persons that do not usually fit into discrete categories of disease classifications. Moreover, self-neglect is an important yet vaguely understood public health issue that represents an extremely frail population crossing sociodemographic and socioeconomic strata.
Prior studies indicate that self-neglect reported to social services agencies is associated with increased morbidity and mortality, particularly among the confirmed cases of self-neglect (5–8). In addition, evidence suggests that the reports of self-neglect are more common among black than among white older adults (9), as was found in reports from the National Adult Protective Services Agency and case studies (1,10). Yet, the significance associated with these black and white differences remains unclear. Improved understanding of these issues is critical to inform research, education, practice, and policy to provide targeted prevention, screening, and interventions within specific racial/ethnic groups. We are not aware of any population-based studies that have examined the racial/ethnic differences in both reported and confirmed self-neglect and its adverse health outcomes.
In this report, we build on the existing literature to examine the black and white differences in mortality associated with reported and confirmed self-neglect in a large and sociodemographically diverse biracial cohort. Our hypothesis is that black compared with white older adults with reported and confirmed self-neglect have significantly greater mortality risk.
METHODS
Design and Participants
The study population consists of participants in the Chicago Health and Aging Project (CHAP). CHAP is a prospective population-based study in a geographically defined biracial community population and is designed to identify risk factors for Alzheimer's disease and other common chronic health problems in older age. Details of the CHAP study design have been described previously (11,12).
Briefly, the study enrolled residents aged 65 years and older of three adjacent neighborhoods on the south side of Chicago. In 1993, the study began with a complete census of the community area. The census identified 7,813 age-eligible residents, 6,158 (78.9%) of whom were enrolled between 1993 and 1997. In 2000, CHAP began to enroll successive cohorts of participants from the study community who had turned 65 years since inception of the study. Data collection occurs in 3-year cycles, with each follow-up cycle beginning after the conclusion of the previous cycle. Follow-up participation rate averaged 80%–85% of survivors at each cycle. Each data collection cycle includes an in-person interview conducted in the participants’ homes. The interviews include standardized questionnaires and tests for the assessment of health history, physical function, cognitive function, health behaviors, and social factors.
The CHAP study is in an urban, racially/ethnically, and socioeconomically diverse community and offers relatively greater generalizability of findings than smaller studies in more selected samples. In addition, the CHAP cohort has been well characterized, with up to 15 years of detailed information on many relevant background variables, permitting in-depth examination of potential confounders. As of 2005, a total of 9,438 black and white older adults had participated in the CHAP study. Written informed consent was obtained, and the study was approved by the Institutional Review Board at Rush University Medical Center.
Conceptual Framework
There have been a number of conceptual frameworks postulated for the syndrome of self-neglect (13–16). This study follows the conceptual framework (13) derived from a large cohort of elder self-neglect cases reported to social services agencies. This conceptual framework represents a comprehensive synthesis of self-neglect and is widely used by public health workers, clinicians, and researchers to better understand the issues of self-neglect (9,17–21). The elements in this conceptual framework include medical comorbidities (eg, diabetes, cancer, cerebrovascular disease, cardiovascular disease), depression, cognitive impairment, physical function impairment, and lack of social well-being. The central hypothesis is that increased burden of medical comorbidities compounded by cognitive impairment and depression may in turn worsen physical function. In this model, lower level of health-related factors represent the central event associated with worsening vulnerability to self-neglect. In addition to the health-related factors, greater depressive symptoms, lack of social network, and inadequate support services increases inability for self-protection, leading to the syndrome of self-neglect.
Reporting and Assessment of Self-Neglect
In the CHAP cohort, there are reported and not-reported cases of self-neglect. Reported self-neglect to the Chicago Department on Aging can come from a variety of sources, including health care and legal professionals, law enforcement officers, community organizations, city workers, postal workers, utility workers, family members, or concerned neighbors or friends who have contact with seniors. When an older adult experiencing self-neglect is reported, a home assessment is performed by the Chicago Department on Aging. In this assessment, the concerns for unmet personal health and safety needs are identified and considered as a continuum of severity, which could worsen over time. These unmet needs are then categorized as either confirmed or unconfirmed self-neglect. Confirmed cases refer to any evidence of unmet needs, and unconfirmed cases refer to no evidence of unmet needs. The details of the self-neglect measure have been previously described (9,22–27). Prior studies indicate that inter-rater reliability of the assessment was high (all variables had κ ≥ .70) (28), as was internal consistency (Cronbach's coefficient alpha of .95) (9).
We matched data from CHAP participants to self-neglect cases reported to the social services agency from January 1, 1993 to October 1, 2005. Matching was based on an algorithm that compared date of birth, sex, race, exact home address, zip codes, and the home phone number. This resulted in a total of 1,479 black and white older CHAP participants who matched a social service agency record. If a CHAP participant was reported more than once, we selected the first report. For the present study, we only used self-neglect cases that were reported to social services agencies after the baseline CHAP interview.
Study Variables
Data on vital status were obtained from family members at regular follow-up contact and through newspaper obituaries. Reports of deaths were verified by matching with the National Death Index, which also provided date of death. We used all-cause mortality as primary end point for the present analyses. Demographic variables include age (in years), sex, income categories, and educational attainment (years of education completed). In this manuscript, race/ethnicity is operationalized as black (non-Hispanic black) or white (non-Hispanic white). The race/ethnicity variable was self-reported in accordance with the U.S. census as well as other large-scale epidemiological studies (ie, the Established Populations for Epidemiological Studies of the Elderly project). A cohort indicator was defined according to baseline participation in either the original cohort or the successive cohorts.
Prior studies suggest that health-related variables are associated with increased risk of self-neglect (9,22–27). These variables include cigarette smoking, alcohol use, depressive symptoms, self-reported medical conditions, cognitive function, physical function, body mass index, social network, and social engagement. Cigarette smoking (ever smoked) and alcohol use (more than 12 drinks in the last 12 months) were assessed based on a series of questions derived from the Established Populations for Epidemiological Studies of the Elderly project. Data on self-reported, physician-diagnosed medical conditions were collected for hypertension, diabetes mellitus, stroke, heart disease, hip fracture, and cancer. Body mass index was calculated by dividing the measured weight in kilograms by the square of the measured height in meters assessed during the in-home interview.
A battery of four cognitive function tests was administered: the Mini-Mental State Examination (29), immediate and delayed recall of brief stories in the East Boston Memory Test (30), and the Symbol Digit Modalities Test (31). To assess global cognitive function with minimal floor and ceiling artifacts, we constructed a summary measure by first transforming a person's score on each individual test to a z-score and then averaging z-scores across the four tests.
Physical function was assessed by direct performance testing, which is thought to provide a more objective and detailed assessment (32) than self-report. We used the modified version of the Short Physical Performance Battery, with total score range of 0–15. It assessed walking speed, tandem stand ability, and repeated chair stand ability (range 0–5 each). Associations between measures of reported disability and physical performance tests are usually strong (33), and physical performance tests have been used to confirm self-report measures (32). In addition, self-reported physical function was assessed using the Katz Activities of Daily Living scale. It measures limitations in an individual's ability to perform six basic self-care tasks (34) and is scored by adding the score on the individual items (range 0–6).
Psychosocial well-being are important factors to consider in the cases of self-neglect (25). Psychosocial variables included the assessment of depressive symptoms, social network, and social engagement. Symptoms of depression were measured using a modified version (35) of the Center for the Epidemiological Study of Depression Scale (range 0–10) (36). Social networks were summarized by the total number of children, relatives, and friends seen at least monthly (37). Social engagement was assessed by asking how often participates participate in social activities outside of house: religious activities, museums, library, and senior centers (11,37).
Analytic Approach
Black and white differences in sociodemographic, health-related, and psychosocial variables were examined stratified by self-neglect report status (reported or unreported). In this study, self-neglect report occurred throughout the study period of 1993–2005. Thus, reports of self-neglect were modeled as a time-varying covariate (38) in a series of Cox proportional hazards models (39), which were used to examine the relationship between reported self-neglect and mortality for black and white older adults, adjusting for covariates. The magnitude of the mortality risk varies with time after the report of self-neglect. Hence, we created a variable for log time after the report of elder self-neglect to allow for this change in risk over time. To demonstrate effects, we calculated the mortality risk at specific time points (3, 6 months, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 7, and 8 years).
In the primary model (Model A), we tested the interaction of self-neglect report and race/ethnicity (Self-Neglect × Race/Ethnicity) on mortality risk after inclusion of the effect of self-neglect report and time after self-neglect report as well as adjustment for cohort, age, sex, education, and income. We tested two-way and three-way interactions of these core variables and retained those with statistical significance in the primary model. The interaction of race/ethnicity with time after report of self-neglect was not significant and therefore not retained in subsequent models. In two additional models, we examined whether the interaction of self-neglect report and race/ethnicity with mortality changed after adjustment for other potential confounders in both black and white older adults. In the second model (Model B), we added health-related variables of medical conditions, global cognitive function, physical performance testing, body mass index, alcohol use, and smoking to the primary model. In the third model (Model C), we added symptoms of depression, social network, and social engagement to Model B to examine the extent to which psychosocial variables affected the interaction terms between self-neglect report and race/ethnicity with mortality risk.
In addition to the analyses of reported self-neglect, we considered the interaction terms of confirmed self-neglect (a subset of reported self-neglect) and race/ethnicity and reanalyzed all of the above Models A–C using the same time-varying covariate analyses. In this report, we did not include analyses of unconfirmed cases of self-neglect in the cohort, as this subset was not the primary focus on this report. Lastly, we examined the association of self-neglect (reported and confirmed) and mortality risk stratified by race/ethnicity separately for black and white older adults. We repeated the models as previously described (Model A–C) with mortality as the outcome. Hazard ratio (HR), parameter estimate (PE), SE, and p values were reported accordingly.
Crude mortality stratified by self-neglect and race was calculated as the number of deaths per 100 person-years. Medical conditions, cognitive function, and physical function were modeled as time-dependent variables in our analyses. All analyses used two-sided alternatives with p value less than .05. All analyses were done using the PROC PHREG procedure in SAS (40).
RESULTS
Baseline Characteristics
There were 5,963 (63.2%) black older adults and 3,475 (36.8%) white older adults in the CHAP cohort. Among black older adults, the proportion of self-neglect was 21.7% (n = 1,295). Among white older adults, the proportion of self-neglect was 5.3% (n = 184). The mean age for black older adults with self-neglect report was 73.1 (6.2) and for white older adults with self-neglect report was 77.9 (7.6). Among black older adults with self-neglect report, 35.6% were men. Among white older adults with self-neglect report, 29.4% were men. Characteristics of black and white differences by self-neglect report status are shown in Table 1.
Table 1.
Characteristic of the Study Sample by Self-Neglect Report (SNR) by Race
| Black |
White |
|||
| No-SNR, N = 4,668 | SNR, N = 1,295 | No-SNR, N = 3,291 | SNR, N = 184 | |
| Sociodemographic | ||||
| Age, y, M (SD) | 71.6 (6.2) | 73.1 (6.2) | 75.3 (7.5) | 77.9 (7.6) |
| Men, n (%) | 1,917 (41.1) | 461 (35.6) | 1,326 (40.3) | 54 (29.4) |
| Education, y, M (SD) | 11.4 (3.5) | 10.8 (3.4) | 13.7 (3.3) | 12.7 (3.6) |
| Income categories, M (SD) | 4.7 (2.3) | 3.9 (2.1) | 6.3 (2.6) | 4.4 (2.2) |
| Health-related variables | ||||
| Total number of medical conditions, M (SD) | 1.3 (1.0) | 1.6 (1.1) | 1.2 (0.9) | 1.4 (1.0) |
| Specific medical conditions | ||||
| Heart disease, n (%) | 719 (15.4) | 300 (23.2) | 571 (17.4) | 33 (17.9) |
| Hypertension, n (%) | 3,040 (65.4) | 913 (70.6) | 1,642 (50.1) | 101 (54.9) |
| Cancer, n (%) | 895 (19.2) | 303 (23.4) | 907 (27.6) | 51 (27.7) |
| Stroke, n (%) | 632 (13.6) | 303 (23.4) | 378 (11.5) | 30 (16.3) |
| Diabetes, n (%) | 554 (11.9) | 226 (17.5) | 149 (4.5) | 20 (10.9) |
| Hip fracture, n (%) | 184 (3.9) | 70 (5.4) | 226 (6.9) | 20 (10.9) |
| MMSE, M (SD) | 25.3 (5.5) | 24.9 (5.2) | 27.3 (4.4) | 26.8 (3.7) |
| Global cognition, M (SD) | −0.17 (1.01) | −0.41 (0.99) | 0.22 (0.97) | −0.25 (1.13) |
| Katz disability, M (SD) | 0.4 (1.2) | 0.4 (1.2) | 0.3 (0.9) | 0.4 (1.1) |
| Physical performance, M (SD) | 8.8 (4.4) | 6.4 (4.4) | 9.5 (4.5) | 6.2 (4.9) |
| BMI in kg/m2, M (SD) | 28.4 (6.1) | 28.8 (6.7) | 26.5 (5.3) | 26.4 (5.3) |
| Smoking (ever), n (SD) | 2,588 (55.4) | 718 (55.4) | 1,690 (51.4) | 96 (52.2) |
| Alcohol, n (SD) | 1,144 (24.6) | 255 (19.8) | 1,724 (52.6) | 65 (35.3) |
| Psychosocial variables | ||||
| CESD, M (SD) | 1.7 (2.1) | 2.0 (2.2) | 1.1 (1.7) | 1.8 (2.2) |
| Social network, M (SD) | 6.9 (5.8) | 6.9 (5.6) | 8.4 (7.1) | 7.1 (7.8) |
| Social engagement, M (SD) | 2.3 (1.7) | 2.1 (1.6) | 2.5 (1.7) | 2.3 (1.6) |
| Death per 100 person-years | 4.70 | 25.05 | 6.58 | 26.25 |
Notes: BMI = body mass index; CESD = Center for the Epidemiological Study of Depression Scale; MMSE = Mini-Mental State Examination.
Black participants had follow-up data for a median of 6.7 years (inter-quartile range: 3.6–10.9 years), during which 2,431 deaths occurred. White participants had follow-up data for a median of 6.4 years (inter-quartile range: 2.4–10.9 years), during which 1,545 deaths occurred. The mortality rate for black older adults with reported self-neglect was 25.05 deaths/100 person-years and was 4.70 deaths/100 person-years among black older adults without reported self-neglect. The corresponding mortality rate for white older adults with reported self-neglect was 26.25 deaths/100 person-years and was 6.58 deaths/100 person-years among white older adults without reported self-neglect.
Interaction of Self-neglect, Race/Ethnicity and Mortality
Analyses testing for differences between black and white in the effect of self-neglect on the risk of mortality included an interaction term of Black × Self-neglect. In the initial analysis (Table 2, Model A), black compared with white older adults with reported self-neglect had significantly stronger mortality risk (PE, 0.46; SE, 0.11; HR, 1.58; 95% confidence interval [CI], 1.27–1.97; p < .001). The added risk for black was only slightly lower after additional adjustment for cognitive function, physical function, nutritional status, alcohol, smoking, and the presence of medical conditions (PE, 0.44; SE, 0.12; HR, 1.55; 95% CI, 1.23–1.97; p < .001; Table 2, Model B). With the addition of psychosocial variables of depression, social network, and social engagement (Table 2, Model C), black compared with white older adults with reported self-neglect had significantly stronger mortality risk (PE, 0.50; SE, 0.14; HR, 1.53; 95% CI, 1.20–1.93; p < .001). For confirmed self-neglect, results were similar (fully adjusted, PE, 0.49; SE, 0.13; HR, 1.63; 95% CI; 1.27–2.12; p < .001).
Table 2.
Proportional Hazard Models of Self-Neglect Report and Race/Ethnicity Association With All-Cause Mortality
| Model A | Model B | Model C | |
| Hazard Ratio (95% confidence interval) |
|||
| Sociodemographic | |||
| Cohort | 0.79 (0.69–0.89) | 0.83 (0.72–0.95) | 0.81 (0.71–0.93) |
| Age, centered at 75 y | 1.08 (1.08–1.09) | 1.04 (1.03–1.05) | 1.04 (1.03–1.05) |
| Men | 1.63 (1.52–1.75) | 1.62 (1.49–1.76) | 1.61 (1.48–1.75) |
| Black | 0.79 (0.72–0.86) | 0.59 (0.54–0.66) | 0.59 (0.54–0.66) |
| Income | 0.94 (0.92–1.96) | 0.98 (0.96–0.99) | 0.98 (0.96–0.99) |
| Education, centered at 12 y | 0.97 (0.96–0.99) | 1.01 (0.99–1.02) | 1.01 (0.99–1.03) |
| Age × Education | 1.00 (1.00–1.00) | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) |
| Sex × Education | 1.03 (1.01–1.05) | 1.01 (0.99–1.03) | 1.01 (0.99–1.03) |
| Health-related variables | |||
| Medical conditions | 1.18 (1.14–1.23) | 1.18 (0.14–1.22) | |
| Global cognition | 0.73 (0.70–0.77) | 0.74 (0.71–0.77) | |
| Physical performance | 0.91 (0.90–0.92) | 0.91 (0.91–0.92) | |
| BMI | 0.97 (0.97–0.98) | 0.97 (0.97–0.98) | |
| Smoking | 1.28 (1.19–1.39) | 1.28 (1.18–1.38) | |
| Alcohol | 0.93 (0.85–1.01) | 0.93 (0.85–1.01) | |
| Psychosocial variables | |||
| CESD | 1.02 (1.01–1.04) | ||
| Social network | 0.99 (0.99–1.01) | ||
| Social engagement | 0.95 (0.93–0.98) | ||
| Self-neglect | 2.79 (2.28–3.41) | 2.33 (1.88–2.89) | 2.36 (1.90–2.93) |
| Log time after report | 0.69 (0.66–0.72) | 0.69 (0.66–0.73) | 0.69 (0.66–0.73) |
| Black × Self-Neglect Report | 1.58 (1.27–1.97) | 1.55 (1.22–1.97) | 1.53 (1.20–1.93) |
Note: Medical conditions, global cognition, physical performance, BMI, CESD, social network, and social engagement were run from lower levels to higher levels. BMI = body mass index; CESD = Center for the Epidemiological Study of Depression scale.
Reported Self-Neglect and Mortality Stratified by Race/Ethnicity
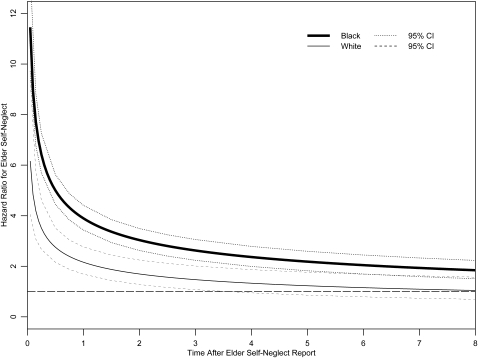
In the stratified analyses of race/ethnicity and mortality, we calculated the mortality risk at specific time points (3, 6 months, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 7, and 8 years). In the fully adjusted analysis for black older adults (Table 3, Model A), reported self-neglect was significantly associated with increased mortality risk at each of the follow-up time points. The mortality risk remained elevated in the early period after the report of self-neglect at 3 months (HR, 6.42; 95% CI, 5.71–7.23), 6 months (HR, 5.00; 95% CI, 4.47–5.59), 1 year (HR, 3.89; 95% CI 3.45–4.39), and 2 years (HR, 3.03; 95% CI 2.64–3.47). After 2 years, the mortality risk for black older adults with reported self-neglect slowly tapered over time but remained significant (Figure 1).
Table 3.
Race-Stratified Proportional Hazard Models of Self-Neglect Report Association With All-Cause Mortality
| Black |
White |
|||||
| Model A | Model B | Model C | Model A | Model B | Model C | |
| Hazard Ratio (95% confidence interval) |
||||||
| Sociodemographic | ||||||
| Cohort | 0.69 (0.59–0.81) | 0.74 (0.62–0.88) | 0.71 (0.61–0.85) | 0.96 (0.76–1.21) | 0.87 (0.77–0.99) | 1.02 (0.79–1.29) |
| Age, centered at 75 y | 1.08 (1.07–1.09) | 1.04 (1.03–1.05) | 1.04 (1.03–1.05) | 1.09 (1.08–1.10) | 1.05 (1.04–1.06) | 1.05 (1.04–1.06) |
| Men | 1.58 (1.43–1.75) | 1.52 (1.36–1.70) | 1.51 (1.35–1.69) | 1.79 (1.58–2.03) | 1.80 (1.57–2.07) | 1.78 (1.55–2.05) |
| Income | 0.94 (0.91–0.96) | 0.99 (0.96–1.01) | 0.99 (0.97–1.02) | 0.94 (0.91–0.96) | 0.96 (0.94–0.99) | 0.97 (0.94–0.99) |
| Education, centered at 12 y | 0.97 (0.95–0.99) | 1.01 (0.99–1.03) | 1.01 (0.99–1.03) | 0.99 (0.96–1.02) | 1.02 (0.99–1.05) | 1.02 (0.99–1.06) |
| Age × Education | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) |
| Sex × Education | 1.03 (1.00–1.05) | 1.00 (0.98–1.03) | 1.00 (0.98–1.03) | 1.01 (0.97–1.04) | 0.99 (0.96–1.03) | 0.99 (0.96–1.03) |
| Log time after report | 0.69 (0.66–0.72) | 0.69 (0.66–0.73) | 0.69 (0.66–0.73) | 0.72 (0.64–0.81) | 0.71 (0.62–0.80) | 0.70 (0.62–0.80) |
| Health-related variables | ||||||
| Medical conditions | 1.19 (1.14–1.25) | 1.19 (1.14–1.24) | 1.16 (1.09–1.23) | 1.16 (1.09–1.23) | ||
| Global cognition | 0.71 (0.67–0.76) | 0.72 (0.68–0.76) | 0.76 (0.71–0.82) | 0.77 (0.72–0.82) | ||
| Physical performance | 0.92 (0.91–0.93) | 0.92 (0.91–0.94) | 0.89 (0.88–0.91) | 0.90 (0.89–0.92) | ||
| BMI | 0.97 (0.96–0.98) | 0.97 (0.96–0.98) | 0.98 (0.96–0.99) | 0.98 (0.96–0.99) | ||
| Smoking | 1.20 (1.08–1.33) | 1.19 (1.07–1.32) | 1.41 (1.24–1.59) | 1.40 (1.24–1.58) | ||
| Alcohol | 0.98 (0.87–1.09) | 0.97 (0.86–1.09) | 0.87 (0.77–0.99) | 0.89 (0.78–1.01) | ||
| Psychosocial variables | ||||||
| CESD | 1.02 (0.99–1.04) | 1.03 (0.99–1.07) | ||||
| Social network | 0.99 (0.99–1.01) | 1.00 (0.99–1.01) | ||||
| Social engagement | 0.96 (0.93–0.99) | 0.95 (0.91–0.99) | ||||
| Self-neglect mortality risk | ||||||
| 3 mo | 7.90 (7.12–8.77) | 6.46 (5.75–7.26) | 6.42 (5.71–7.23) | 4.19 (3.29–5.33) | 3.46 (2.67–4.46) | 3.51 (2.72–4.53) |
| 6 mo | 6.11 (5.53–6.75) | 5.02 (4.49–5.62) | 5.00 (4.47–5.59) | 3.32 (2.70–4.09) | 2.72 (2.17–3.39) | 2.75 (2.19–3.44) |
| 1 y | 4.72 (4.24–5.25) | 3.91 (3.47–4.40) | 3.89 (3.45–4.39) | 2.64 (2.15–3.25) | 2.13 (1.70–2.67) | 2.16 (1.72–2.71) |
| 1.5 y | 4.06 (3.62–4.55) | 3.37 (2.96–3.83) | 3.36 (2.96–3.82) | 2.31 (1.85–2.88) | 1.85 (1.46–2.36) | 1.87 (1.47–2.39) |
| 2 y | 3.65 (3.23–4.12) | 3.04 (2.65–3.48) | 3.03 (2.64–3.47) | 2.10 (1.66–2.66) | 1.68 (1.29–2.17) | 1.69 (1.31–2.19) |
| 2.5 y | 3.36 (2.96–3.82) | 2.79 (2.43–3.23) | 2.79 (2.42–3.22) | 1.95 (1.52–2.51) | 1.56 (1.18–2.04) | 1.57 (1.19–2.06) |
| 3 y | 3.14 (2.75–3.59) | 2.62 (2.26–3.04) | 2.61 (2.25–3.04) | 1.84 (1.41–2.39) | 1.46 (1.09–1.95) | 1.47 (1.10–1.96) |
| 4 y | 2.82 (2.45–3.25) | 2.36 (2.01–2.77) | 2.36 (2.01–2.77) | 1.67 (1.25–2.23) | 1.32 (0.96–1.81) | 1.33 (0.97–1.82) |
| 5 y | 2.59 (2.23–3.02) | 2.18 (1.84–2.58) | 2.17 (1.84–2.57) | 1.55 (1.14–2.11) | 1.22 (0.87–1.71) | 1.23 (0.88–1.72) |
| 6 y | 2.43 (2.08–2.84) | 2.04 (1.71–2.43) | 2.03 (1.71–2.43) | 1.46 (1.05–2.02) | 1.14 (0.80–1.63) | 1.15 (0.81–1.64) |
| 7 y | 2.29 (1.95–2.69) | 1.93 (1.60–2.31) | 1.92 (1.60–2.31) | 1.39 (0.99–1.95) | 1.08 (0.75–1.57) | 1.09 (0.76–1.58) |
| 8 y | 2.18 (1.85–2.58) | 1.83 (1.52–2.21) | 1.83 (1.52–2.21) | 1.33 (0.93–1.89) | 1.04 (0.71–1.52) | 1.04 (0.71–1.53) |
Note: Medical conditions, global cognition, physical performance, BMI, CESD, social network, and social engagement were run from lower levels to higher levels. BMI = body mass index; CESD = Center for the Epidemiological Study of Depression Scale.
Figure 1.
Black and white differences in the self-neglect and mortality risk over 8 years of follow-up (hazard ratio [95% confidence intervals]).
In the fully adjusted analysis for white older adults (Table 3, Model A), mortality risk was also high in the early period after the identification of reported self-neglect, although the HRs at each time point appeared substantially lower than for black older adults. The mortality risk remained elevated in the early period after the report of self-neglect at 3 months (HR, 3.51; 95% CI, 2.72–4.53), 6 months (HR, 2.75; 95% CI, 2.19–3.44), 1 year (HR, 2.16; 95% CI, 1.72–2.71), and 2 years (HR, 1.69; 95% CI, 1.31–2.19). However, after 4 years of follow-up, the mortality risk for white older adults with reported self-neglect was no longer statistically significant (Figure 1).
Confirmed Self-Neglect and Mortality Stratified by Race
In the fully adjusted analyses (Table 4), confirmed self-neglect among older black adults was associated with increased mortality risk. There were similar patterns of elevated mortality risk in the earlier period of follow-up, with subsequent slow decline in the magnitude of mortality risk over time that remained statistically significant throughout. For white older adults with confirmed self-neglect, mortality risk was also significantly higher in the earlier period of follow-up but was not statistically significant after the first 2 years of follow-up.
Table 4.
Race-Stratified Hazard Ratio for Confirmed Self-Neglect Associated With All-Cause Mortality
| Black |
White |
|
| Time After Report | Hazard Ratio (95% confidence interval) | |
| 3 mo | 6.36 (5.62–7.19) | 3.41 (2.60–4.46) |
| 6 mo | 4.92 (4.38–5.54) | 2.58 (2.02–3.28) |
| 1 y | 3.82 (3.37–4.33) | 1.95 (1.52–2.51) |
| 1.5 y | 3.29 (2.88–3.77) | 1.66 (1.27–2.17) |
| 2 y | 2.96 (2.56–3.42) | 1.48 (1.11–1.97) |
| 2.5 y | 2.73 (2.34–3.18) | 1.35 (0.99–1.84) |
| 3 y | 2.55 (2.18–2.99) | 1.26 (0.91–1.73) |
| 4 y | 2.29 (1.94–2.72) | 1.12 (0.19–1.59) |
| 5 y | 2.12 (1.77–2.53) | 1.02 (0.70–1.48) |
| 6 y | 1.98 (1.64–2.39) | 0.95 (0.64–1.40) |
| 7 y | 1.87 (1.54–2.27) | 0.89 (0.59–1.34) |
| 8 y | 1.78 (1.45–2.17) | 0.85 (0.55–1.29) |
DISCUSSION
Our study in a biracial community population suggests that reported self-neglect to a social services agency was associated with a large and significant increased mortality risk in both black and white older adults. Moreover, increased mortality risks associated with self-neglect persisted throughout the follow-up period (8 years) for black older adults but not for white older adults. Overall, impact of self-neglect on mortality risk was significantly stronger in black than in white older adults.
Possible Mechanisms
The mechanisms between black and white older adults with self-neglect and mortality require further investigation. We considered differences in education and income between black and white older adults, but the adjustment for these factors did not substantially change the associations. In addition, we considered a comprehensive series of health-related characteristics that are commonly associated with increased mortality risk among black and white older adults, including time-dependent variables of medical conditions, physical function, and cognitive function, but adjustment for these factors did not substantially alter the association. We also considered several psychosocial characteristics such as depressive symptoms, limited social networks, and social engagement, but again, adjustment for these factors did not change the results.
Black and white differences in reporting of suspected cases of self-neglect require further examination. In our prior study of self-neglect (6), we found no statistically significant differences in threshold of self-neglect reporting in black and white older adults. However, we could not investigate the specific indicators or phenotypes of self-neglect. The construct of self-neglect severity comprised 15 indicators of different self-neglect behaviors. It is possible that there are significant differences in the specific behaviors that predispose black older adults to have higher mortality risk. In addition, there could be black/white differences in the rate of long-term care health services utilization or proposed and/or accepted interventions by social services agencies, which may in part account for the mortality differences. There could also be differences in the onset of medical conditions, types of medical conditions, higher rate of medical comorbidities, and greater changes in the severity of medical conditions between black and white older adults over time, which could contribute toward the sustained mortality risk among black older adults (41–44). Lastly, there could be a black/white differential of health and metabolic consequences of self-neglect, which could account for the differential mortality risk.
A wide range of health disparities could also significantly contribute toward these differences in adverse health outcomes (45–47). Black and white differences in access to health and health care professionals may contribute toward the differential mortality risks. Other important disparities include racial discordance between health care professionals and older adults with self-neglect, patient's lack of trust in health care professionals, patient's lower perception of patient-centered care and cultural competency in their communication with health care professionals, and decreased involvement by patients in their medical decision making (48–51). Furthermore, there could be experiences prior to age 65 that could have influenced the self-neglect behaviors with respect to mortality risks, as posited by the theory of cumulative disadvantage (47). This theory suggests that individuals with higher education have more health resources including improved ability to avoid stressors and unhealthy lifestyles and thus have beneficial cumulative effects on health with increasing age. These issues rooted in health disparities are important and should be subject to further investigation.
We found that mortality risk for black and white older adults with self-neglect decreases over the 8 years of follow-up. It is possible that the identification of elder self-neglect triggered interventions from social services, family members, neighbors, community organizations, and/or health care professionals. Some of the existing interventions include home maker services, meal services, nutritional counseling, home health services, referrals to health care professionals, benefit check-up, and other benefits provided by the social services agencies. These interventions could lead to potential reduction in the severity of self-neglecting behaviors could in turn lower the mortality risk over time. This finding supports comprehensive efforts to promote early reporting and identification of self-neglecting older adults in order to reduce morbidity and mortality and improve health and well-being. Future studies are needed to elucidate the effectiveness of existing interventions and prevention strategies for self-neglect cases.
Contribution to Existing Literature
Our study extends the existing literature in three ways. This study is of a large sample of racially/ethnically diverse population-based study of older adults in a geographically defined community that is socioeconomically diverse, expanding the generalizability of the study findings. Second, this is the first study to demonstrate the effect of self-neglect on mortality risk among black and white older adults, showing the substantial increased mortality, especially during the first 2 years. This has direct practice and policy implications for devising prompt and efficient interventions to deal with the black and white older adults with self-neglect. Given the higher HR of mortality risk in black older adults than white older adults, targeted and timely interventions are needed to address these disparities in health outcomes.
Third, the study is the first to demonstrate that increased mortality risk persisted throughout the study period only for black older adults with self-neglect but not for white older adults with self-neglect. However, it is also possible that the relatively smaller sample size of white older adults who experience self-neglect could lead to unstable estimates in the rate in whites. The causal mechanisms for this finding remain unclear, and further study is needed to elucidate the differential characteristics for these black and white older adults who self-neglect with respect to adverse health outcomes. Moreover, future studies are needed to evaluate the effectiveness of existing interventions by social services agencies and health care professionals in ameliorating the racial/ethnic differences in mortality risk associated with self-neglect.
Limitations
Our study has limitations. First, we relied on reports of self-neglect from social services agencies rather than having a uniform measure of self-neglect for the entire CHAP cohort, and we were unable to elucidate the racial/ethnic differences in specific behaviors or phenotypes of self-neglect associated with mortality risk. However, this study provides a base for the future study of racial/ethnic differences in self-neglect through uniform data collection in CHAP and in other cohorts. Second, we did not have information on the onset of medical conditions, severity of medical conditions, trajectory of decline of medical conditions, recent infections, detailed measures of executive function, metabolic abnormalities, illicit drug use, and psychiatric diagnosis, which could be potential confounders not considered in the association between self-neglect and mortality in black and white older adults.
Third, the study did not have any information on the social services agencies’ or health care professional's intervention as the result of self-neglect or the effectiveness of these interventions in modifying the mortality risk in black and white older adults. Fourth, we did not have information on the potential self-neglecting experiences prior to age 65, which could have contributed toward the racial/ethnic differences in mortality risk between black and white older adults. Fifth, we did not have comprehensive measures of socioeconomic status (ie, occupation prestige, savings, quality of education, etc.), which could have operated differently by race and contributed toward the black and white differences in self-neglect and mortality risk.
CONCLUSIONS
In sum, self-neglect is a common but under-recognized and poorly understood geriatric syndrome. Like other geriatric syndromes that are the result of the complex interactions among a variety of medical, psychological, and social risk factors, self-neglect is likely to develop and progress slowly over time (52). Our findings contribute to an improved understanding of the differences in self-neglect between black and white older adults with respect to adverse health outcomes in a defined biracial population, showing that black older adults compared with white older adults with self-neglect had higher mortality risk. As the baby boomer population increases rapidly, self-neglect will likely increase over time and come to the attention of the health care, social services, and legal systems. This could have important implications as it will likely place significantly higher burdens on the existing system dealing with older adults who self-neglect.
Future studies are needed to elucidate the back and white differences in the specific self-neglect behaviors and mortality risk. Studies are also needed to examine the role of racial disparities in influencing the relationship of self-neglect with other adverse health outcomes. We need to examine the relations between caregiving and community support with the risk for self-neglect cases among black and white older adults. Moreover, we need to identify risk factors associated with self-neglect by race and to explore the contextual factors that lead to the significantly higher prevalence of self-neglect in black older adults. These findings may be useful not only in informing future research efforts of self-neglect across racially/ethnically diverse populations but also in developing racially/ethnically relevant clinical, social, and policy guidelines for the treatment and prevention of self-neglect. Together, these efforts could reduce health disparities and improve health and aging in our increasing racially/ethnically diverse society.
FUNDING
This work was supported by National Institute on Aging (R01 AG11101), Paul B. Beeson Career Development Award in Aging (K23 AG030944), American Federation for Aging Research, The Starr Foundation, John A. Hartford Foundation, and The Atlantic Philanthropies.
CONFLICT OF INTEREST
All authors have no conflict of interest and declare no financial interest.
Acknowledgments
The authors wish to thank Ms. Ann Marie Lane for community development and oversight of project coordination and Ms. Michelle Bos, Ms. Holly Hadden, Mr. Flavio LaMorticella, and Ms. Jennifer Tarpey for coordination of the study. We thank George Dombrowski, MS, for data management support. We are also grateful for the men and women of the social services agencies for their dedication and tireless effort in protecting the vulnerable aging populations.
X.Q.D. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.National Center on Elder Abuse. The National Elder Abuse Incidence Study. Washington, DC: American Public Human Services Association; 1998. [Google Scholar]
- 2.Teaster PB. A Response to Abuse of Vulnerable Adults: The 2000 Survey of State Adult Protective Service. http://www.ncea.aoa.gov/ncearoot/Main_Site/pdf/research/apsreport030703.pdf. 2002. Accessed January 16, 2006. [Google Scholar]
- 3.National Center on Elder Abuse. Website. NCEA: the Basics. http://elderabusecenter.org/pdf/research/apsreport030703.pdf. 2006. Accessed June 20, 2006. [Google Scholar]
- 4.Dyer CB, Pickens S, Burnett J. Vulnerable elders: when it is no longer safe to live alone. JAMA. 2007;298(12):1448–1450. doi: 10.1001/jama.298.12.1448. [DOI] [PubMed] [Google Scholar]
- 5.Lachs MS, Williams CS, O’Brien S, Pillemer KA, Charlson ME. The mortality of elder mistreatment. JAMA. 1998;280(5):428–432. doi: 10.1001/jama.280.5.428. [DOI] [PubMed] [Google Scholar]
- 6.Dong X, Simon M, Mendes de Leon C, et al. Elder self-neglect and abuse and mortality risk in a community-dwelling population. JAMA. 2009;302(5):517–526. doi: 10.1001/jama.2009.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lachs MS, Williams CS, O’Brien S, Pillemer KA. Adult protective service use and nursing home placement. Gerontologist. 2002;42(6):734–739. doi: 10.1093/geront/42.6.734. [DOI] [PubMed] [Google Scholar]
- 8.Dong X, Simon MA, Evans DA. Prospective study of the elder self-neglect and emergency department use in a community population. Am J Emerg Med. 2011 doi: 10.1016/j.ajem.2011.02.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong X, Simon MA, Evans DA. Characteristics of elder self-neglect in a biracial population: findings from a population-based cohort. Gerontology. 2010;56(3):325–334. doi: 10.1159/000243164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Brien J, Thibault J, Turner L, Laird-Fick H. Self-neglect: an overview. J Elder Abuse Negl. 1999;11(2):1–19. [Google Scholar]
- 11.Bienias JL, Beckett LA, Bennett DA, Wilson RS, Evans DA. Design of the Chicago Health and Aging Project (CHAP) J Alzheimers Dis. 2003;5(5):349–355. doi: 10.3233/jad-2003-5501. [DOI] [PubMed] [Google Scholar]
- 12.Evans DA, Bennett DA, Wilson RS, et al. Incidence of Alzheimer disease in a biracial urban community: relation to apolipoprotein E allele status. Arch Neurol. 2003;60(2):185–189. doi: 10.1001/archneur.60.2.185. [DOI] [PubMed] [Google Scholar]
- 13.Dyer CB, Goodwin JS, Pickens-Pace S, Burnett J, Kelly PA. Self-neglect among the elderly: a model based on more than 500 patients seen by a geriatric medicine team. Am J Public Health. 2007;97(9):1671–1676. doi: 10.2105/AJPH.2006.097113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orem DE. Nursing: Concepts of Practice. 4th ed. St Louis, MO: Mosby; 1991. [Google Scholar]
- 15.Choi NG, Kim J, Asseff J. Self-neglect and neglect of vulnerable older adults: reexamination of etiology. J Gerontol Soc Work. 2009;52(2):171–187. doi: 10.1080/01634370802609239. [DOI] [PubMed] [Google Scholar]
- 16.Iris M, Ridings JW, Conrad KJ. The development of a conceptual model for understanding elder self-neglect. Gerontologist. 2010;50(3):303–315. doi: 10.1093/geront/gnp125. [DOI] [PubMed] [Google Scholar]
- 17.Dyer CB, Franzini L, Watson M, et al. Future research: a prospective longitudinal study of elder self-neglect. J Am Geriatr Soc. 2008;56(suppl 2):S261–S265. doi: 10.1111/j.1532-5415.2008.01978.x. [DOI] [PubMed] [Google Scholar]
- 18.Paveza G, Vandeweerd C, Laumann E. Elder self-neglect: a discussion of a social typology. J Am Geriatr Soc. 2008;56(suppl 2):S271–S275. doi: 10.1111/j.1532-5415.2008.01980.x. [DOI] [PubMed] [Google Scholar]
- 19.McDermott S. The devil is in the details: self-neglect in Australia. J Elder Abuse Negl. 2008;20(3):231–250. doi: 10.1080/08946560801973077. [DOI] [PubMed] [Google Scholar]
- 20.Naik AD, Burnett J, Pickens-Pace S, Dyer CB. Impairment in instrumental activities of daily living and the geriatric syndrome of self-neglect. Gerontologist. 2008;48(3):388–393. doi: 10.1093/geront/48.3.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pickens S, Naik AD, Burnett J, Kelly PA, Gleason M, Dyer CB. The utility of the Kohlman evaluation of living skills test is associated with substantiated cases of elder self-neglect. J Am Acad Nurse Pract. 2007;19(3):137–142. doi: 10.1111/j.1745-7599.2007.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dong X, Wilson RS, Simon MA, Rajan B, Evans DA. Cognitive decline and risk of elder self-neglect: the findings from the Chicago health and aging project. J Am Geriatr Soc. 2010;58(12):2292–2299. doi: 10.1111/j.1532-5415.2010.03156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong X, Simon MA, Wilson RS, Beck TT, McKinnell K, Evans DA. Association of personality traits with elder self-neglect in a community-dwelling population. Am J Geriatr Psychiatry. 2010 doi: 10.1097/JGP.0b013e3182006a53. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dong X, Wilson RS, Mendes de Leon CF, Evans DA. Self-neglect and cognitive function among community-dwelling older persons. Int J Geriatr Psychiatry. 2010;25(8):798–806. doi: 10.1002/gps.2420. [DOI] [PubMed] [Google Scholar]
- 25.Dong X, Beck TT, Evans DA. A cross-sectional population-based study of self-neglect and psychosocial factors in a biracial community. Aging Ment Health. 2010;14(1):74–84. doi: 10.1080/13607860903421037. [DOI] [PubMed] [Google Scholar]
- 26.Dong X, Mendes de Leon CF, Evans DA. Is greater self-neglect severity associated with lower levels of physical function? J Aging Health. 2009;21(4):596–610. doi: 10.1177/0898264309333323. [DOI] [PubMed] [Google Scholar]
- 27.Dong X, Simon M, Fulmer T, Mendes de Leon CF, Rajan B, Evans DA. Physical function decline and the risk of elder self-neglect in a community-dwelling population. Gerontologist. 2010;50(3):316–326. doi: 10.1093/geront/gnp164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Illinois Department on Aging. Determination of Need Revision Final Report. Vol. I. Ilinois Department on Aging; 1989. [Google Scholar]
- 29.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 30.Albert M, Smith LA, Scherr PA, Taylor JO, Evans DA, Funkenstein HH. Use of brief cognitive tests to identify individuals in the community with clinically diagnosed Alzheimer's disease. Int J Neurosci. 1991;57(3–4):167–178. doi: 10.3109/00207459109150691. [DOI] [PubMed] [Google Scholar]
- 31.Smith A. Symbol Digit Modalities Test Manual-Revised. Los Angeles, CA: Western Psychological; 1984. [Google Scholar]
- 32.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 33.Gill TM, Williams CS, Tinetti ME. Assessing risk for the onset of functional dependence among older adults: the role of physical performance. J Am Geriatr Soc. 1995;43(6):603–609. doi: 10.1111/j.1532-5415.1995.tb07192.x. [DOI] [PubMed] [Google Scholar]
- 34.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6(3):493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 35.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 36.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 37.Cornoni-Huntley J, Brock DB, Ostfeld A, Taylor JO, Wallace RB. Established Populations for Epidemiological Studies of the Elderly Resource Data Book (Rep. No. NIH Publication No. 86-2443) Washington, DC: U.S. Department of Health and Human Services; 1986. [Google Scholar]
- 38.Andersen PK, Gill RD. Cox's regression model counting process: a large sample study. Ann Stat. 1982;10:1100–1120. [Google Scholar]
- 39.Cox DR. Regression models and life tables. J Roy Statis Soc B. 1972;34:187–220. [Google Scholar]
- 40.SAS Institute Inc. SAS Online Doc, Version 9.1.3. Cary, NC: SAS Institute Inc.; 2004. [Google Scholar]
- 41.Ostchega Y, Harris TB, Hirsch R, Parsons VL, Kington R. The prevalence of functional limitations and disability in older persons in the US: data from the National Health and Nutrition Examination Survey III. J Am Geriatr Soc. 2000;48(9):1132–1135. doi: 10.1111/j.1532-5415.2000.tb04791.x. [DOI] [PubMed] [Google Scholar]
- 42.Kelley-Moore JA, Ferraro KF. The black/white disability gap: persistent inequality in later life? J Gerontol Soc Sci. 2004;59(1):S34–S43. doi: 10.1093/geronb/59.1.s34. [DOI] [PubMed] [Google Scholar]
- 43.Ferraro KF, Farmer MM. Double jeopardy, aging as leveler, or persistent health inequality? A longitudinal analysis of white and black Americans. J Gerontol Soc Sci. 1996;51(6):S319–S328. doi: 10.1093/geronb/51b.6.s319. [DOI] [PubMed] [Google Scholar]
- 44.Bulatao RA, Anderson NB. Understanding Racial and Ethnic Differences in Health in Late Life. National Research Council; 2004. [PubMed] [Google Scholar]
- 45.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health Rep. 2002;117(5):426–434. doi: 10.1093/phr/117.5.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bengston VL, Schaie KW. Handbook of Theories of Aging. New York: Springer; 2010. [Google Scholar]
- 48.O’Malley AS, Sheppard VB, Schwartz M, Mandelblatt J. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004;38(6):777–785. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 49.Martin SS, Trask J, Peterson T, Martin BC, Baldwin J, Knapp M. Influence of culture and discrimination on care-seeking behavior of elderly African Americans: a qualitative study. Soc Work Public Health. 2010;25(3):311–326. doi: 10.1080/19371910903240753. [DOI] [PubMed] [Google Scholar]
- 50.Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296–306. [PubMed] [Google Scholar]
- 51.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004;53(9):721–730. [PubMed] [Google Scholar]
- 52.Dong X. Medical implications of elder abuse and neglect. Clin Geriatr Med. 2005;21(2):293–313. doi: 10.1016/j.cger.2004.10.006. [DOI] [PubMed] [Google Scholar]