Abstract
Aim:
The effect of Tualang honey on wound healing in bacterial contaminated full-thickness burn wounds was evaluated in 36 male Sprague Dawley rats.
Materials and Methods:
The rats were randomly divided into three groups (n = 12/group). Three full-thickness burn wounds were created on each rat. Each group of rats was inoculated with a different organism in the burn wounds: Group A was inoculated with Pseudomonas aeruginosa, Group B was inoculated with Klebsiella pneumoniae and Group C was inoculated with Acinetobacter baumannii. One wound on each rat was dressed with either Tualang honey, Chitosan gel or Hydrofibre silver. Each wound size was measured on day 3, 6, 9, 12, 15, 18 and 21 of the study.
Results:
The mean wound size of the Tualang honey-treated wounds was not statistically different than that of the Chitosan gel or Hydrofibre silver-treated wounds when the wounds were compared throughout the entire experiment (P > 0.05). However, comparing the mean wound size on day 21 alone revealed that the Tualang honey-treated wounds were smaller in comparison to that of the Chitosan gel and Hydrofibre silver-treated groups.
Conclusions:
This study shows that topical application of Tualang honey on burn wounds contaminated with P. aeruginosa and A. baumannii gave the fastest rate of healing compared with other treatments.
Keywords: Burn wound, honey, Pseudomonas aeruginosa, Acinetobacter baumannii, wound healing
INTRODUCTION
Honey, an ancient remedy for the treatment of infected wounds, has recently been “rediscovered” by the medical profession, particularly in cases where conventional, modern therapeutic agents have failed. The current prevalence of antibiotic resistant microbial species has led to a re-evaluation of honey.
In light of the enormous potential for application of honey, it is important that research continues to evaluate not only honeys already recognized for their antibacterial properties, but also other locally produced honeys such as Tualang honey. Tualang honey is used commonly as a medicinal product and as food in Malaysia. However, little scientific information about its therapeutic potential, including wound healing properties and antimicrobial activity have been published to date. In this study, we evaluated the wound healing effects of Tualang honey in full-thickness burn wound in a Sprague Dawley rat model.
MATERIALS AND METHODS
Male Sprague Dawley rats were obtained from the Laboratory Animal Research Unit (LARUSM), School of Medical Sciences, Universiti Sains Malaysia (USM), Kota Bharu, Kelantan. All parts of this project were performed in the animal house, School of Medical Sciences, USM. This study complied with the ‘Principles of Laboratory Animal Care’ and ‘Guide for the Care and Use of Laboratory Animals’ and was approved by the university's ethical committee. (No. of Animal Ethics Approval: USM/Animal Ethics Approval/2007/(34) (108).
Study design
Thirty-six male Sprague Dawley rats weighing between 350 and 400 grams were used in the study. The rats were housed individually and were provided free access to water and a standard commercial rat diet throughout the study. The animals were randomly divided into three groups of twelve animals each and subjected to the experimental protocols described below.
Anaesthesia and surgical protocol
Skin preparation
On the day of wounding, rats were immobilized in the ventral position and the dorsum of the rats was shaved. Immediately before procedure, the rats were anaesthetized with an intramuscular injection of ketamine (35.0 mg/kg) and xylazine (5.0 mg/kg) in the gluteal area. When fully anaesthetized, the shaved areas were cleaned with povidone iodine, 70 % alcohol and chlorhexidine. The operation site was isolated with a sterile towel.
Full-Thickness burn wound creation
Burn wounds were created under sterile technique on the dorsum of the rats between the last thoracic vertebra and the first sacrum by placing a piece of hot metal perpendicular to the dorsum of the rat for 30 seconds. The area of the wound was approximately 1.0 cm × 1.0 cm in size. A total of three wounds (2 cm apart) were created on each rat.
Treatments
The rats were randomly divided into three groups of twelve animals each. In the first group (Group A), the three burn wounds were inoculated with 104 colony forming unit (CFU) of Pseudomonas aeruginosa, in the second group (Group B) the wounds were inoculated with 104 CFU of Klebsiella pneumoniae and in the third group (Group C) the wounds were inoculated with 104 CFU of Acinetobacter baumannii. Inoculation was performed by pipetting 104 CFU (0.5 ml) of each microorganism directly onto the wound using an automatic pipette. The inoculum was spread evenly across the wound surface.
Each rat received one treatment per wound so that one wound per rat was treated with Tualang honey (0.2 ml), Chitosan gel (0.5 ml) or Hydrofibre silver dressing (measuring 2.5 cm × 2.5 cm). The Tualang honey was provided by Federal Agricultural Marketing Authority (FAMA) Malaysia. The Chitosan gel was provided by Nuclear Malaysia and the Hydrofibre silver dressings were purchased from ConvaTec (Malaysia). The first treatment was applied approximately ten minutes after burn infliction and five minutes after the wound was inoculated with a microorganism. Following treatment, the wound was covered with sterile gauze and a bandage. Every three days the wound was cleaned with 0.9% saline and the dressing was changed. Three rats from each group were euthanized on days 3, 7, 14 and 21.
Evaluation of wounds
On days 3, 6, 9, 12, 15, 18 and 21 post-operation, the condition of each wound was examined. Photographs were taken after the burn wounds were created and during each dressing change. For wound size measurement, the wounds were traced on a transparency paper and the tracings were measured.
Statistics
All results are expressed as the mean ± SD. The results for each group were analyzed with repeated-measures ANOVA using the treatment groups as the independent group and wound size as the dependent variable. Statistical significance was evaluated using independent t test by using a statistical software package (SPSS 12.0). A P value of <0.05 was considered to be significant.
RESULTS
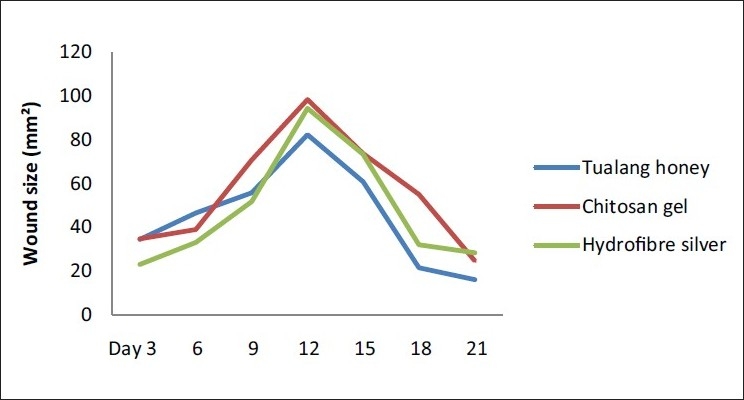
In Group A, there was a 14% reduction in wound size by day 9 (P = 0.585) in the Tualang honey-treated wounds, and 73% by day 15 (P = 0.116). The wounds remained smaller for the Tualang honey-treated wounds than in the Chitosan gel and Hydrofibre silver-treated wounds by day 18 (P = 0.130) and day 21 (P = 0.385). The mean wound size of Tualang honey-treated wounds and other treated wounds gradually decreased with time [Table 1 and Figure 1].
Table 1.
Wound size measurement in rats inoculated with Pseudomonas aeruginosa (Group A)
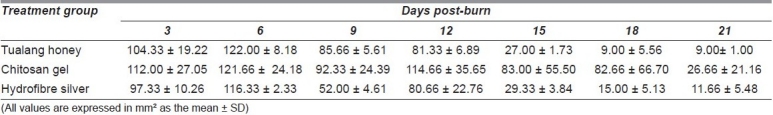
Figure 1.
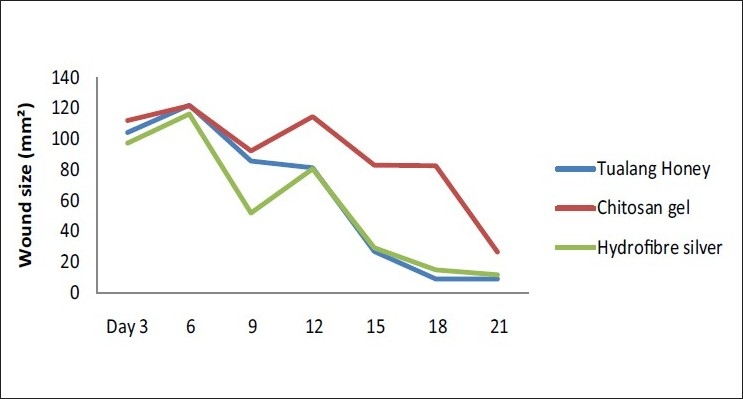
Wound size measurement in rats inoculated with Pseudomonas aeruginosa (Group A)
In Group B, there was a 47% reduction in wound size by day 9 (P = 0.019) in the Tualang honey-treated wounds, and however increased by 106% by day 12 (P = 0.056) and 24% by day 15 (P = 0.997). The wounds remained larger for the Tualang honey-treated wounds than in the Chitosan gel and Hydrofibre silver-treated wounds by day 18 (P = 0.852) and day 21 (P = 0.874). There was no significant difference among the three treatments at day 6, 12, 15, 18 or 21 except day 3 and 9. The mean wound size of Tualang honey-treated wounds and other treated wounds increased at day 12 because of significant inflammation from K. pneumoniae infection and then gradually decreased after day 15 [Table 2 and Figure 2].
Table 2.
Wound size measurement in rats inoculated with Klebsiella pneumoniae (Group B)
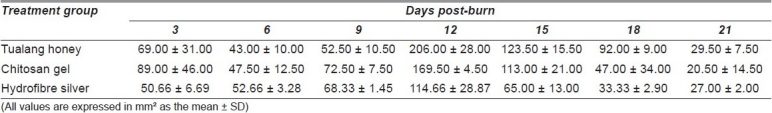
Figure 2.
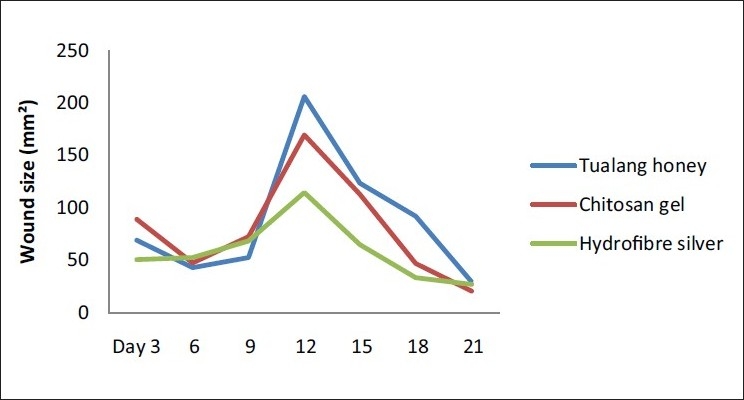
Wound size measurement in rats inoculated with Klebsiella pneumoniae (Group B)
In Group C, there was a 44% reduction in wound size by day 9 (P = 0.659) in the Tualang honey-treated wounds, and 39% by day 15 (P = 0.810). The wounds remained smaller for the Tualang honey-treated wounds than in the Chitosan gel and Hydrofibre silver-treated wounds by day 18 (P = 0.524) and day 21 (P = 0.808). The mean wound size of Tualang honey-treated wounds and other treated wounds increased at day 12 and then gradually decreased after day 15, which is similar to Group B [Table 3 and Figure 3].
Table 3.
Wound size measurement in rats inoculated with Acinetobacter baumannii (Group C)
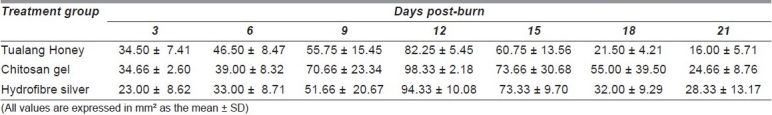
Figure 3.
Wound size measurement in rats inoculated with Acinetobacter baumannii (Group C)
Overall, the mean wound size of the Tualang honey-treated wounds was not statistically different than that of the Chitosan gel or Hydrofibre silver-treated wounds when the wounds were compared throughout the entire experiment. However, comparing the mean wound size on day 21 alone revealed that the Tualang honey-treated wounds were smaller in comparison to that of the Chitosan gel and Hydrofibre silver-treated groups.
During the period of study, there was colonization of burn wound with Staphylococcus species. The colonization occurred in all the three groups and therefore did not differentially affect the result.
DISCUSSION
Previous reports have attributed the effectiveness of honey as a dressing to antibacterial properties related to four properties of honey. First, honey is a supersaturated sugar solution that facilitates a strong interaction between the sugar molecules and water molecules. This ‘osmotic effect’ leaves very few water molecules free to support microorganismal growth. Second, honey has a pH between 3.2 and 4.5, which is acidic enough to inhibit the growth of most microorganisms. Third, hydrogen peroxide produced by glucose oxidation is perhaps the most important antibacterial component, although not all researchers agree with its importance. The hydrogen peroxide concentration produced in honey activated by dilution is typically around 1 mmol/l and it is about 1000 times less than in the 3% solution commonly used as an antiseptic. A study with Escherichia coli exposed to a constantly replenished stream of hydrogen peroxide, showed that bacterial growth was inhibited by 0.02–0.05 mmol/l hydrogen peroxide, a concentration that was not damaging to fibroblast cells from human skin.[1] Lastly, several phytochemical factors with antibacterial activity have been identified in honey as honey stimulates healing in dormant wounds and speeds the healing process by stimulating cell growth.[2]
Our results revealed that the in vivo wound contraction of the Tualang honey-treated full-thickness burn wounds was not statistically different than that of the Chitosan gel or Hydrofibre silver-treated wounds when the wounds were compared throughout the entire study (P > 0.05). However, comparing the mean wound size on day 21 alone revealed that the Tualang honey-treated wounds were smaller in comparison to that of the Chitosan gel and Hydrofibre silver-treated groups in Groups A and C. This shows that Tualang honey has the effect of promoting wound contraction in full-thickness burn wounds. These findings are in agreement with earlier study by Efem, Postmes et al. and Subrahmanyam, as observed in both animal studies and clinical trials.[3–5]
Efem conducted one of the first clinical trials of honey (floral source not specified) as a wound dressing. Honey dressings were used to treat 59 patients with recalcitrant wounds and ulcers, 47 of which had been treated for what clinicians deemed a “sufficiently long time” (1 month to 2 years) with conventional treatments of commercial wound dressings or systemic and topical antibiotics. The wounds were of varied etiology, such as Fourniers gangrene, burns, cancrum oris, diabetic ulcers, traumatic ulcers, decubitus ulcers, sickle cell ulcers, and tropical ulcers, showed no signs of healing, and were increasing in size. Following topical application of honey, 58 of the 59 cases showed remarkable improvement. He observed that honey debrided wounds rapidly, replacing sloughed, gangrenous, and necrotic tissue with granulation tissue and advancing epithelialization.[3]
In one experimental study by Postmes et al., comparisons were made between honey and silver sulfadiazine, and between honey and sugar, on standard deep dermal burns, 7 cm × 7 cm, made on Yorkshire pigs. Epithelialization was achieved within 21 days with honey and sugar whereas it took 28–35 days with silver sulfadiazine. Granulation was clearly seen to be suppressed initially by treatment with silver sulfadiazine. In all honey-treated wounds the histological appearance of biopsy samples showed less inflammation than in those treated with sugar and silver sulfadiazine.[4]
In the clinical trials on partial-thickness burns, honey was found to promote the healing of burn wounds. Subrahmanyam has conducted clinical trials comparing the effectiveness of pure honey (obtained directly from hives, with no processing or dilution) and other traditional remedies (such as boiled potato peelings or amniotic membrane) to current pharmacologic and surgical methods (silver sulfadiazine (SSD) and tangential excision with skin grafts). Eighty-four percent of patients treated with honey showed satisfactory epithelialization after 7 days, with 100% of patients showed epithelialization by 21 days. Of the patients treated with SSD, 72% and 84% showed satisfactory healing by days 7 and 21, respectively. In these studies, histological analysis of honey-dressed wounds showed early decrease in inflammation, better infection control and faster healing. Honey was as effective as or more effective than SSD, one of the most common topical burn treatments in use. However, Subrahmanyam also concluded that whereas honey was superior for the treatment of superficial burns, full-thickness burns responded better to tangential excision and skin grafting.[5–7]
They have concluded that honey induces a fast rate of tissue regeneration and suppresses inflammation, edema, exudation and malodor in wounds.
In another study, Bergman et al. has observed clinically that healing in open wounds is faster with honey. An experimental study carried out using mice also compared honey with saline dressings, on wounds made by excising skin (10 mm × 10 mm) down to muscle. Histological examination showed that the thickness of granulation tissue and the distance of epithelialization from the edge of the wound were significantly greater, and the area of the wound significantly smaller in those treated with honey.[8]
Honey provides a moist healing environment and prevents bacterial growth even when wounds are heavily infected. The benefits of a moist wound environment are well established; It protects the wound, reduces infection rates, reduces pain, debrides necrotic tissue, and promotes granulation tissue formation. Moist wound dressings enable epithelialization to occur along the top surface of the wound, rather than underneath the scab, as occurs in dry wounds, resulting in a pitted scar. The physical properties of honey make it an ideal moist wound dressing. The high viscosity of honey (which varies from floral source to floral sources) provides a protective barrier to prevent wounds from becoming infected, effectively sealing the wound.[9] It is a very effective means of quickly rendering heavily infected wounds sterile without the side effects of antibiotics, and it is effective against antibiotic-resistant strains of bacteria, with no adverse effects on wound tissues.
Bacterial susceptibility to honey varies by species. Honey may have either bactericidal or bacteriostatic effects and may require a period of exposure before the bacteria is killed. However, whether the effects are bacteriostatic or bactericidal is not a major issue in terms of therapeutic use, because some of the antibiotics in common use in medical practice have only bacteriostatic effects. Complete bacteriostasis, maintained by regular application of honey, would be sufficient to allow the healing process to proceed normally.[10]
Cooper et al. tested the sensitivity of 17 strains of P. aeruginosa isolated from infected burns to two honeys with different types of antibacterial activity, a pasture honey and a manuka honey, both with median levels of activity. All strains showed similar sensitivity to honey with minimum inhibitory concentrations below 10% (vol/vol); both honeys maintained bactericidal activity when diluted more than 10-fold. In their study, honey with proven antibacterial activity has the potential to be an effective treatment option for burns infected or at risk of infection with P. aeruginosa.[11] In our study, we have demonstrated that Tualang honey promotes the healing of wounds innoculated with P. aeruginosa which is most likely attributed by honey's antibacterial activity.
In another study, Lusby et al. used an agar dilution method to assess the activity of 6 types of honey against 13 bacteria (Alcaligenes faecalis, Citrobacter freundii, E. coli, Enterobacter aerogenes, K. pneumoniae, Mycobacterium phlei, Salmonella california, Salmonella enteritidis, Salmonella typhimurium, Serratia marcescens, Shigella sonnei, Staphylococcus aureus and Staphylococcus epidermidis) and one yeast (Candida albicans). The study showed that all bacteria except Serratia marcescens were inhibited by all honeys used in this study. The yeast Candida albicans was not inhibited by the honeys. The bacteria that were most sensitive to Medihoney and Manuka were A. faecalis, E. aerogenes and S. aureus. This result demonstrated selectivity of honey against certain bacteria. However, the low level inhibition of K. pneumoniae suggests that honey would not be a practical means of controlling the growth of this microorganism.[12]
Our study confirmed this finding: Tualang honey-treated wounds on rats innoculated with K. pneumoniae (Group B) showed delayed wound healing when compared to wounds treated with Chitosan gel or Hydrofibre silver dressing. The abundant polysaccharidic capsule that typically surrounds K. pneumoniae that may be regarded as the most important virulence determinant could have protected it against the bactericidal action of the treatment.[13]
Two local studies by Nasir et al. and Khoo et al. support the effectiveness of Tualang honey as a dressing in a bacterial contaminated burn wound. Nasir et al. compared antibacterial activity of Aquacel-tualang honey, Aquacel-Manuka honey, Aquacel-Ag and Aquacel- plain dressings against bacteria isolated from patients with partial thickness burn wound. In the in vitro antibacterial study looking at zone of inhibition assays, Aquacel-Ag and Aquacel-Manuka honey dressings gave better zone of inhibition for Gram positive bacteria such as Staphylococcus aureus, coagulase-negative S. aureus (CONS) and Streptococcus spp compared to Aquacel--Tualang honey dressing. However, comparable results were obtained with Aquacel-Manuka honey and Aquacel-Tualang honey dressing against Gram negative bacteria (Enterobacter cloacae, K. pneumoniae, Pseudomonas spp. and Acinetobacter spp).[14] In a study performed by Khoo et al in rats, the effectiveness of Tualang honey, hydrofibre and hydrofibre silver dressing was tested and compared against a full-thickness burn wound that was contaminated either with P. aeruginosa, K. pneumonia or A. baumannii. Wound size assessments showed that wound contraction of burn wounds dressed with Tualang honey was markedly greater than with the hydrofibre silver and hydrofibre dressing. The quantitative and semi-quantitative analyses revealed that Tualang honey-treated rats demonstrated a reduction in bacterial growth compared to hydrofibre silver- and hydrofibre-treated wounds in P. aeruginosa inoculated wounds (P = 0.005), with marked bacterial growth reductions.[15]
In conclusion, we have demonstrated that Tualang honey promotes the healing of wounds innoculated with P. aeruginosa and A. baumannii. Therefore, it has an obvious potential for use in managing burn wounds infected with P. aeruginosa and A. baumannii. Further evaluation of contaminated burn wounds treated with honey must be conducted to determine honey's angiogenic and antibacterial properties. As with any wound care treatment, prospective randomized controlled studies are needed to provide a more robust and informative evidence base concerning its use in wound care in clinical setting and its cost benefit.
Acknowledgments
This research was supported by the Ministry of Higher Education Malaysia, Universiti Sains Malaysia Research University (RU) Grant, (1001/PPSP/8120206). Our appreciation to Federal Agricultural Marketing Authority (FAMA), Kedah and Laboratory Animal Research Unit for the assistance provided. We would like to acknowledge Dr. Kamarul Imran from Department of Community Medicine, School of Medical Sciences, USM and Professor Dr. Jamal from Clinical Research Center, Hospital Kuala Lumpur, for their assistance in statistical analysis.
Footnotes
Source of Support: Ministry of Higher Education Malaysia, Universiti Sains Malaysia Research University (RU) Grant, (1001/PPSP/8120206)
Conflict of Interest: None declared.
REFERENCES
- 1.Hyslop PA, Hinshaw DB, Scraufstatter IU, Cochrane CG, Kunz S. Hydrogen peroxide as a potent bacteriostatic antibiotic: Implications for host defense. Free Radic Biol Med. 1995;19:31–7. doi: 10.1016/0891-5849(95)00005-i. [DOI] [PubMed] [Google Scholar]
- 2.Molan PC. The Evidence Supporting the Use of Honey as a Wound Dressing. Int J Low Extrem Wounds. 2006;5:40–54. doi: 10.1177/1534734605286014. [DOI] [PubMed] [Google Scholar]
- 3.Efem SE. Clinical observations on the wound healing properties of honey. Br J Surg. 1988;75:679–81. doi: 10.1002/bjs.1800750718. [DOI] [PubMed] [Google Scholar]
- 4.Postmes TJ, Bosch MM, Dutrieux R, Van Baare J, Hoeksta MJ. Speeding up the healing of burns with honey. An experimental study with histological assessment of wound biopsies. In: Mizrahi A, Lensky Y, editors. Bee Products: Properties, Applications and Apitherapy. New York: Plenum Press; 1997. pp. 27–37. [Google Scholar]
- 5.Subrahmanyam M. Honey dressing versus boiled potato peel in the treatment of burns: A prospective randomized study. Burns. 1996;22:491–3. doi: 10.1016/0305-4179(96)00007-1. [DOI] [PubMed] [Google Scholar]
- 6.Subrahmanyam M. A prospective randomised clinical and histological study of superficial burn wound healing with honey and silver sulfadiazine. Burns. 1998;24:157–61. doi: 10.1016/s0305-4179(97)00113-7. [DOI] [PubMed] [Google Scholar]
- 7.Subrahmanyam M. Early tangential excision and skin grafting of moderate burns is superior to honey dressing: A prospective randomised trial. Burns. 1999;25:729–31. doi: 10.1016/s0305-4179(99)00063-7. [DOI] [PubMed] [Google Scholar]
- 8.Bergman A, Yanai J, Weiss J, Bell D, David MP. Acceleration of wound healing by topical application of honey.An animal model. Am J Surg. 1983;145:374–6. doi: 10.1016/0002-9610(83)90204-0. [DOI] [PubMed] [Google Scholar]
- 9.Bello Y, Phillips TJ. Recent advances in wound healing. JAMA. 2000;283:716–8. doi: 10.1001/jama.283.6.716. [DOI] [PubMed] [Google Scholar]
- 10.Lusby PE, Coombes AL, Wilkinson JM. Honey: A Potent Agent for Wound Healing.? J Wound Ostomy Continence Nurs. 2002;29:295–300. doi: 10.1067/mjw.2002.129073. [DOI] [PubMed] [Google Scholar]
- 11.Cooper RA, Halas E, Molan PC. The Efficacy of Honey in Inhibiting Strains of Pseudomonas Aeruginosa From Infected Burns. J Burn Care Rehabil. 2002;23:366–70. doi: 10.1097/00004630-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Lusby PE, Coombes AL, Wilkinson JM. Bactericidal activity of different honeys against Pathogenic Bacteria. Arch Med Res. 2005;36:464–7. doi: 10.1016/j.arcmed.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 13.Brissel S, Fevre C, Passet V, Issenhuth-Jeanjean S, Tournebize R, Diancourt L. Virulent clones of Klebsiella pneumoniae: Identification and evolutionary scenario based on genomic and phenotypic characterization. PLoS One. 2009;4:1–13. doi: 10.1371/journal.pone.0004982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nasir NA, Halim AS, Singh KK, Dorai AA, Haneef MN. Antibacterial properties of tualang honey and its effect in burn wound management: A comparative study. BMC Complement Altern Med. 2010;10:1–7. doi: 10.1186/1472-6882-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khoo YT, Halim AS, Singh KK, Mohamad NA. Wound contraction effects and antibacterial properties of Tualang honey on full-thickness burn wounds in rats in comparison to hydrofibre. BMC Complement Altern Med. 2010;10:1–8. doi: 10.1186/1472-6882-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]


