Abstract
Background:
Residual muscle weakness, cross-innervation (caused by misdirected regenerating axons), and muscular imbalance are the main causes of internal rotation contractures leading to limitation of shoulder joint movement, glenoid dysplasia, and deformity in obstetric brachial plexus palsy. Muscle transfers and release of antagonistic muscles improve range of motion as well as halt or reverse the deterioration in the bony architecture of the shoulder joint. The aim of our study was to evaluate the clinical outcome of shoulder muscle transfer for shoulder abnormalities in obstetric brachial plexus palsy.
Materials and Methods:
One hundred and fifty patients of obstetric brachial plexus palsy with shoulder deformity underwent shoulder muscle transfer along with anterior shoulder release at our institutions from 1999 to 2007. Shoulder function was assessed both preoperatively and postoperatively using aggregate modified Mallet score and active and passive range of motion. The mean duration of follow-up was 4 years (2.5–8 years).
Results:
The mean preoperative abduction was 45° ± 7.12, mean passive external rotation was 10° ± 6.79, the mean active external rotation was 0°, and the mean aggregate modified Mallet score was 11.2 ± 1.41. At a mean follow-up of 4 years (2.5–8 years), the mean active abduction was 120° ± 18.01, the mean passive external rotation was 80° ± 10.26, while the mean active external rotation was 45° ± 3.84. The mean aggregate modified Mallet score was 19.2 ± 1.66.
Conclusions:
This procedure can thus be seen as a very effective tool to treat internal rotation and adduction contractures, achieve functional active abduction and external rotation, as well as possibly prevent glenohumeral dysplasia, though the long-term effects of this procedure may still have to be studied in detail clinico-radiologically to confirm this hypothesis.
Level of evidence:
Therapeutic level IV
Keywords: Brachial plexus palsy, contracture, mallet score
INTRODUCTION
Obstetric brachial plexus palsy occurs due to trauma to the roots of the brachial plexus during difficult delivery,[1] or as suggested by some authors, even during intrauterine life.[2] It has been documented in earlier literature that about 75–90% of all obstetric brachial plexus palsies recover spontaneously and completely during the first year of life. However the patients who do not recover spontaneously usually have some permanent damage and the brunt of the damage is borne by the shoulder.[3] Almost all patients with obstetric palsy have involvement of the fifth and sixth cervical nerves and almost 48% of them have involvement of C5-C6 alone.[1] In fact, in the last few decades, it has been proved by many authors that shoulder abnormalities are a rule in patients with chronic brachial plexopathy.[3] These abnormalities develop very early in infancy and are caused by muscle imbalances due to the developing cross-innervation in a growing child. The imbalance is between the more powerful adductor–internal rotator and the relatively less powerful abductor–external rotator group. The resultant contracture results in assymetrical forces acting on the glenohumeral articulation leading to grossly deformed and posteriorly subluxated humeral head with an excessively retroverted glenoid if allowed to act unchecked over the years.[3]
Surgery for the shoulder in brachial plexus palsy is aimed at treating the internal rotation contracture, increasing the range of abduction and external rotation as well as to prevent secondary structural changes in the glenohumeral articulation.[4] Most of the surgeries are modifications of Sever's original description of release of the subscapularis and the pectoralis major.[5] L'Episcopo described a surgery in which he divided the tendinous origin of the teres major, latissimus dorsi, and repositioned them under the lateral head of the triceps thus converting them into external rotators.[6] Various modifications of this technique have been described over the years, such as those by Zachary and Leeds[7] and Phipps and Hoffer,[8] though the basic principle of all the surgeries has remained the same, that is, either releasing, sectioning, or transferring the overacting internal rotators to convert them into external rotators. A newer modification of this technique was suggested by Chuang et al. in 1998 which has since then been widely used at various centers of the world.[9] More recently, the role of injecting botulinum toxin in the hyperacting muscle has been investigated by some authors (Grosmann et al., 2007). It has been shown that injecting the hyper-agonist muscle with botulinum toxin reduces spastic co-contractions and improves resting posture of the muscles.[10,11]
The present study describes a series of 150 consecutive patients operated at our institutes for secondary shoulder deformities due to obstetric brachial plexus palsy by a combination including anterior shoulder release and tendon transfer. The aims of the present study were to determine the effect of these soft tissue rebalancing procedures on glenohumeral function based on shoulder movements as well as functional grading.
MATERIALS AND METHODS
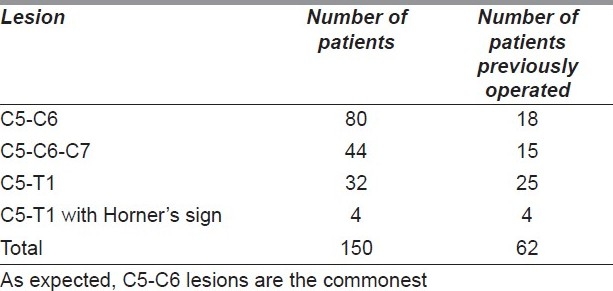
Between January 1999 to June 2007, 305 patients were evaluated and treated for obstetric brachial plexus palsy at our institute. Of these, 35 had a complete recovery and were treated conservatively, and 169 patients were operated primarily at around 3 months for a primary nerve surgery. One hundred and sixty-three children with obstetric brachial plexus palsy with shoulder deformities and contractures were treated with soft tissue rebalancing surgeries of which 62 had been operated previously for primary nerve surgeries. Thirteen were lost to follow-up, making a total of 150 patients who were included in the study. Most patients were operated on by the senior surgeon (MRT) and about 15 by the other senior author (RM). There were 81 boys and 69 girls. The average age at the time of presentation to our institute was 3 months and the average age for shoulder muscle transfer was 40 ± 20.06 months (range 15 months to 8 years). Of the 150 children, 80 were C5-C6 lesions, 34 were C5-C7 lesions, 32 were C5-T1 lesions, and 4 were C5-T1 lesions with Horner's sign. Exploration, neurotisation, and nerve grafting were performed around the age of 3 months in 62 patients; these included 18 patients with C5-C6 lesions, 15 C5-C7 lesions, 25 C5-T1 lesions, and all 4 patients with global plexus palsy with Horner's sign [Table 1]. The right shoulder was affected in 78 of these patients while the left was affected in 72 patients.
Table 1.
Distribution of the lesions of brachial plexus palsy
All patients were evaluated preoperatively according to a fixed protocol designed by the senior author (MRT), which included active and passive shoulder range of motion, presence or absence of Putti's sign, presence or absence of contractures, and an aggregate modified Mallet score (total 25). The aggregate Mallet[4] score is calculated by finding the individual Mallet score for the five components (global abduction, global external rotation, hand-to-spine, hand-to-mouth, and hand-to-neck) and then summing up the individual components. For each component, grade I is given for no motion while grade V denotes normal motion (Equal to contralateral side). The patients were also examined preoperatively for co-contractions between the muscles.
The surgeries were aimed at releasing the contracted muscle and augmenting the weaker but more useful muscle. The surgical technique was therefore a combination of existing historical techniques tailored to the situation in the individual child based on three factors – muscle strength, co-contractions, and concomitant contractures. All patients had shoulder abduction and external rotation weakness with a concomitant internal rotation contracture.
Surgical technique
During the surgical procedure, lateral position was given with the affected arm draped free and able to move in all directions. The surgical incision was infiltrated with 1:1,00,00,00 (one million) concentration of saline adrenaline for a bloodless operative field. This concentration allows much larger volumes to be injected without reducing the quality of vasoconstriction. The first incision was taken on the lateral margin of the scapula in the axilla going across the axillary skin fold to expose and detach the tendons of the conjoined muscles, teres major, and latissimus dorsi from their insertion on the humerus. These conjoined tendons were then elevated upto their neurovascular pedicle found proximally along the lateral border of the scapula. Through a second incision posteriorly over the spine of the scapula, the tendon of the infraspinatus was exposed below the scapular spine after retracting the posterior fibers of the deltoid away. A wide subcutaneous tunnel between the first and second incision was created through which the detached tendon of the teres major was tunneled, and woven on to the tendon of the infraspinatus using 2-0 nylon, keeping the upper limb abducted and externally rotated after the anterior shoulder release was completed as described in the next paragraph.
Keeping the arm abducted, an anterior incision is taken in the delto-pectoral groove to release the shoulder joint. Through this incision, the coraco humeral ligament and if necessary the capsule of the shoulder joint was cut to obtain full external rotation and reduction of the subluxated head in those cases where it was fully subluxated. In some cases, partial excision of the hypertrophied tip of the coraocoid process was done if found to be impinging on the humerus in rotation or abduction. At this stage, botulinum toxin was injected into the subscapularis and the pectoralis major in selected cases depending on the degree of co-contraction felt pre-operatively and a presence of a strong Putti's sign.
After achieving hemostasis, the wound was closed in layers. A plaster spica was applied keeping the arm in abduction above 90° and external rotation with the elbow slightly flexed to hold the rotation more easily and the forearm supinated. This spica was worn for 4–6 weeks after which a controlled rehabilitation program was started by a well-trained physiotherapist which included active and passive range of motion exercises along with strengthening exercises. An extension elbow-guard was used to prevent flexion of the elbow during active shoulder abduction. This brace was removed while doing physiotherapy for external rotation.
After the surgery, the patients were asked to follow-up every 6 weeks for the first 3 months followed by 3 monthly for the first year and half yearly thereafter. During every follow-up visit, the patients were assessed as to their active and passive range of motion, Putti's sign, as well as their aggregate modified Mallet score.
Statistical analysis
Data were entered using Microsoft Excel 2007 and analyzed using SPSS version 16. Since the data were not distributed normally (Kolmogorov–Smirnov test for normality), Wilcoxon signed rank test was used for before and after comparison of different variables. P value of less than 0.05 was taken as significant.
RESULTS
All patients showed improvement in shoulder joint function and movement after the surgical procedure as measured by the aggregate modified Mallet score after a mean follow-up of 4 years (range 2.5–8 years) [Figures 1a–e and Figures 2a–e]. The pre-operative Mallet score ranged from 8 to 13 with a mean of 11.2 ± 1.41. This score improved to a mean aggregate Mallet score of 19.2 ± 1.66 (range 15–20). No patient had worsening of shoulder function. All factors of the Mallet score (global abduction, global external rotation, hand-to-mouth, hand-to-spine, and hand-to-neck) improved with the maximum improvement being seen in the global abduction and global external rotation (pre-operative mean of 2.0 to a post-operative mean of 4.1 for abduction and pre-operative mean of 2.0 to a post-operative mean of 4.0 for external rotation). The active abduction improved from a pre-operative value of 45° ± 7.12 to a post-operative value of 120° ± 18.01, while the passive external rotation improved from 10° ± 6.79 pre-operatively to 80° ± 10.26 post-operatively . The active external rotation also showed a similar increase from a pre-operative value of 0° to 45° ± 7.12 post-operatively. The details of the pre-operative and post-operative range-of-motion and Mallet scores are provided in Table 2. A total of 10 patients had botulinum toxin A injected into their subscapularis and sternal head of pectoralis major. The post-operative Mallet scores of these 10 patients was marginally better than the other patients (19.5 ± 0.52) (P>0.05). However this is not statistically significant at this time.
Figure 1.

(a) Seven years post-operative clinical photograph of a girl operated with anterior shoulder release and latissimus dorsi and teres major transfer. Active external rotation was 80° (Mallet score-IV). Note the healed scar of the anterior shoulder release (blue arrow). (b) Active abduction of around 130° (Mallet score IV). (c) Hand-to-neck Mallet score V. (d) Hand-to-mouth Mallet score V. (e) Hand-to-spine Mallet score IV.
Figure 2.

(a) Preoperative clinical photograph of a 14-month-old child with untreated right-sided obstetric brachial plexus palsy (C5-6 lesion) showing inability to abduct the right shoulder with a concomitant internal rotation contracture, (b) Three years post-operative clinical photograph of the same patient depicting excellent clinical function showing abduction (2b), external rotation (2c), hand-to-head (2d), and hand-to-mouth (2e) activities, (c) Three years postoperative clinical photograph of the same patient depicting excellent clinical function showing abduction (2b), external rotation (2c), hand-to-head (2d), and hand-to-mouth (2e) activities, (d) Three years post-operative clinical photograph of the same patient depicting excellent clinical function showing abduction (2b), external rotation (2c), hand-to-head (2d), and hand-to-mouth (2e) activities, (e) Three years postoperative clinical photograph of the same patient depicting excellent clinical function showing abduction (2b), external rotation (2c), hand-to-head (2d), and hand-to-mouth (2e) activities.
Table 2.
Preoperative and postoperative mallet scores and values of abduction and external rotation
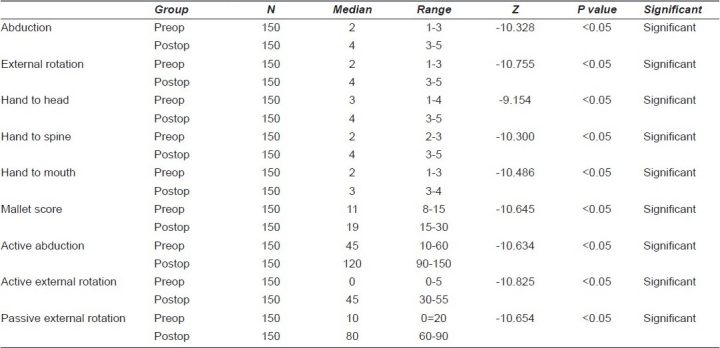
All the increases in the Mallet scores of the respective components were statistically significant at P<0.05. No patient had a decrease or weakness in internal rotation with the hand-to-spine score improving from a mean of 2.4 to a post-operative of 3.8. No post-operative complications like wound infection, axillary nerve, or radial nerve palsy were noted.
Statistical analysis performed using the Wilcoxon Signed rank test with P<0.05.
DISCUSSION
It has been well documented in literature[1] that almost 90% of all patients of obstetric brachial plexus palsy recover completely and thus can be treated conservatively. However, this figure is different in this study group with only 35 of the 305 patients recovering completely. The reason for this discrepancy may be the fact that ours is a tertiary referral center and only those patients who do not recover sufficiently are sent to us for further management.
Shoulder deformities in obstetric brachial plexus palsies have been an object of study and debate over a number of years. The cross-innervations of the regenerating nerve fibers lead to significant internal rotation and adduction contractures with profound effect on the glenohumeral development and functional ability of the child. The range of soft tissue and bony implications of this condition is so vast that a “cafeteria” approach has to be adopted for the management of a particular deformity. Current treatment options include anterior shoulder release, tendon transfers, and soft tissue balancing procedures,[3,4,12] concomitant use of botulinum toxin A[11] and humeral and glenoid osteotomies.[13] However, there are no clear guidelines for the selection of any of these procedures as well as the ideal timing at which they should be used.
The average age of our patients at the time of surgery was 44 months (range 18 months to 7 years). This was slightly more as compared to that quoted in western literature. In a series by Waters et al.,[4] the average age at the time of tendon transfers was 27 months while that in a series by Hoffer et al.,[8] it was 28 months. This finding may be due to lack of awareness among other specialties and the fact that there are no nationally or regionally circulated guidelines for the management as well as referral of patients of obstetric plexus palsy to a specialist clinic such as ours.
In our series, the aggregate modified Mallet score was used to evaluate the patients pre- and post-operatively. The intra- and interobserver reliability of the Mallet classification system have been adequately established.[14,15] All our patients showed satisfactory improvement in the Mallet scores with the score improving from a pre-operative mean of 11 to a post-operative mean of 19.2. This compares well with other similar series which have been previously reported. Waters et al.[4] reported on 23 patients of obstetric palsy treated with tendon transfers and musculotendinous lengthening, in which the average Mallet score improved from 10 to 18.
In recent times, there has been a general trend toward performing bony surgeries in the form of humeral[13,14] and glenoid[16] osteotomies as salvage procedures for late obstetric palsies with secondary glenohumeral dysplasia. This inference has been put forth due to the assumption that soft tissue procedures may not be able to stop or reverse bony changes in the glenohumeral joint. However this statement may not be true as we have been able to match the results of glenoid as well as humeral osteotomies irrespective of the amount of glenohumeral dysplasia in the form of clinical outcome (Details of some of the important studies mentioned in literature are given in Table 3). Pre-operative and post-operative magnetic resonance imaging scanning was possible in only a few of our patients due to financial constraints. However the few in which this was possible showed good improvement in parameters of glenohumeral dysplasia like glenoid version and percentage of humeral head anterior to the transverse scapular line [Figures 3a and b].
Table 3.
Summary of various articles showing results of various modifications of tendon transfers and bony procedures for obstetric palsy
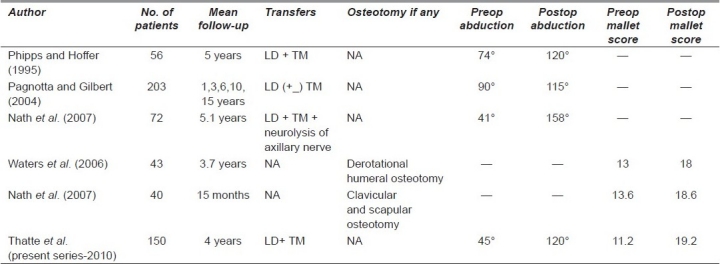
Figure 3.
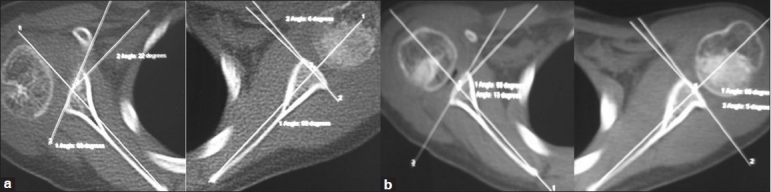
(a) Preoperative MRI of a patient with left brachial plexus palsy showing a subluxed humeral head with a glenoid version of 22° on the affected side as compared to a version of 6° on the normal side, (b) MRI of the same patient 3 years after shoulder muscle transfer showing relocated humeral head with a normalized glenoid version
Also there has been a fear that anterior shoulder release as well as transfer of the powerful internal rotators without a compensatory bony procedure would weaken internal rotation. No patient in our series developed weakness in internal rotation. On the contrary, the average hand-to-spine Mallet score improved from 2.4 to 3.8 postoperatively. This improvement may be attributed to better compliance of the patient to physiotherapy and rehabilitative care[4] as well as to meticulous surgical technique to prevent overzealous anterior release and over-lengthening of the subscapularis.
In a few of our patients, we have used injection of botulinum toxin type A into the pectoralis major and subscapularis as an adjunct to the formal surgical release. The clinical results of this technique were better in these patients though the difference was not statistically significant. It has been suggested by some authors that benefits of botulinum toxin are sustained even beyond the period for which the toxin is recognized to be active.[11] This observation was found to be true in our study also as the results were sustained even 3 years after surgery. This is supposed to be due to improved cortical recruitment of the injured nerves caused by the toxin.[16] It thus appears that botulinum toxin may be effective in improving long-term results though its exact indications, dosage, as well as efficacy may require randomized trials for confirmation.
The points in favor of this study include a large number of patients with a varied age of presentation and surgery, who have been followed up for a significant amount of time with a low attrition rate (less than 10%). All surgeries were performed by a single senior surgeon with a similar technique and a constant treatment protocol was followed. A classification with intra- and interobserver reliability (the Mallet score)[11] was used for evaluation and a well-defined physiotherapy regimen and rehabilitative care was given to all patients.
However the limitations of the present study include the unblinded and noncomparative nature of its treatment modality as well as certain other limitations which are common to other previously described methods. Clinical examination of infants and children is difficult and children's fear of examination, inability to comprehend instructions, and in-coordination due to poorly developed motor function are all hindrances toward accurate clinical examination. Thus clinical examination alone can only be considered as an approximation of the true motor deficit. As a result, any study based solely on clinical findings without any radiological correlation is bound to have some shortcomings. The authors are currently undertaking a study taking into account the clinicoradiological status of the glenohumeral joint as a whole using CT and MRI scans. This study is however limited by the fact that CT and MRI scans preoperatively and postoperatively prove to be a significant financial burden to our patients, many of whom belong to low socioeconomic strata.
In summary, this study indicates that latissimus dorsi and teres major tendon transfers are useful in improving function in chronic brachial plexopathy. Injection of botulinum toxin type A has proved to be an effective adjunct to surgery, though its exact indications still need to be defined. Though bony procedures have found support in recent times, it can be said that glenohumeral changes would still be best treated early with muscle-rebalancing procedures before irreversible changes develop. A CT/MRI based study would be an ideal tool to check the efficacy of such procedures in treating these complex problems of glenohumeral articulation.
See video on www.ijps.org
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kirkos JM, Kyrkos MJ, Kapetanos GA, Haritidis JH. Brachial Plexus Palsy secondary to birth injuries: Long term results of anterior release and tendon transfers around the shoulder. J Bone Joint Surg Br. 2005;87:231–5. doi: 10.1302/0301-620x.87b2.14739. [DOI] [PubMed] [Google Scholar]
- 2.Alfonso I, Papazian O, Shuhaiber H, Yaylali I, Grossman JA. Intrauterine shoulder weakness and obstetric brachial plexus palsy. Pediatr Neurol. 2004;31:225–7. doi: 10.1016/j.pediatrneurol.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Waters PM. Management of shoulder deformities in brachial plexus birth injuries. J Pediatr Orthop. 2010;30:S53–6. [Google Scholar]
- 4.Waters PM, Bae DS. The early effects of tendon transfers and open capsulorrhaphy on Glenohumeral deformity in Brachial plexus Birth palsy. J Bone Joint Surg Am. 2008;90:2171–9. doi: 10.2106/JBJS.G.01517. [DOI] [PubMed] [Google Scholar]
- 5.Sever JW. Obstetric paralysis, its etiology, pathology, clinical aspects and treatment with a report of four hundred and seventy cases. Am J Dis Child. 1916;12:541–78. [Google Scholar]
- 6.L'Episcopo J. Tendon transplantation in Obstetric paralysis. Am J Surgery. 1934;25:122–5. [Google Scholar]
- 7.Zachary RB. Transplantation of teres major and latissimus dorsi for loss of external rotation at shoulder. Lancet. 1947;2:757. doi: 10.1016/s0140-6736(47)90763-0. [DOI] [PubMed] [Google Scholar]
- 8.Hoffer MM, Phipps GJ. Closed reduction and tendon transfers for transfer for treatment of dislocation of the glenohumeral joint secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 1998;80:997–1001. doi: 10.2106/00004623-199807000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Chuang DC, Hae-Shya M, Wei F. A new strategy of muscle transposition for shoulder deformity caused by Obstetric brachial plexus palsy. Plast Recontr Surg. 1998;101:686–94. doi: 10.1097/00006534-199803000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Gracies JM. Physiological effects of Botulinum toxin on spasticity. Mov Disord. 2004;19:120–8. doi: 10.1002/mds.20065. [DOI] [PubMed] [Google Scholar]
- 11.Price AE, DiTaranto P, Yaylali I, Tidwell MA, Grossmann JA. Botulinum toxin type A as an adjunct to the surgical treatment of the medial rotation deformity of the shoulder in birth injuries of the brachial plexus. J Bone Joint Surg Br. 2007;89:327–9. doi: 10.1302/0301-620X.89B3.17797. [DOI] [PubMed] [Google Scholar]
- 12.Nath RK, Paizi M. Improvement in abduction of the shoulder after reconstructive soft-tissue procedures in obstetric brachial plexus palsy. J Bone Joint Surg Br. 2007;89:620–6. doi: 10.1302/0301-620X.89B5.18403. [DOI] [PubMed] [Google Scholar]
- 13.Waters PM, Peljovich AE. Shoulder reconstruction in patients with chronic brachial plexus birth palsy. Clin Orthop Relat Res. 1999;364:144–52. doi: 10.1097/00003086-199907000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Waters PM, Bae DS. The effect of derotational humeral osteotomy on global shoulder function in brachial plexus birth palsy. J Bone Joint Surg Am. 2006;88:1035–42. doi: 10.2106/JBJS.E.00680. [DOI] [PubMed] [Google Scholar]
- 15.Nath RK, Lyons AB, Melcher BA, Paizi M. Surgical correction of medial rotation contracture in obstetric brachial plexus palsy. J Bone Joint Surg Br. 2007;89:1638–44. doi: 10.1302/0301-620X.89B12.18757. [DOI] [PubMed] [Google Scholar]
- 16.Bae DS, Waters PM, Zurakowski D. Reliability of three classification systems measuring active motion in brachial plexus birth palsy. J Bone Joint Surg Am. 2003;85:1733–8. doi: 10.2106/00004623-200309000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


