Abstract
Bow hunter’s stroke is typically due to mechanical compression or stretching of the dominant vertebral artery (VA) during contralateral head rotation against the bony elements of the atlas and axis. We report a case of vertebrobasilar insufficiency due to bilateral vertebral artery occlusion at the left C3–4 and the right C1–2 junction on rightward head rotation. A 64-year-old man experienced ischemic symptoms during 90° head rotation to the right with complete resolution of symptoms after returning his head to the neutral position. Dynamic cervical angiography with rightward head rotation showed severe compression of the right VA at the transverse foramen of C3–4 and mechanical stenosis of the left VA at the C1–2 level. During head rotation, the flow of the right VA was decreased more than the left side. Cervical 3-D computed tomography (CT) on rightward head rotation demonstrated displacement of the uncovertebral C3–4 joint, with excessive rotation of the C3 vertebral body. Based on these findings, instability at C3–4 was suspected to be the main cause of the vertebrobasilar insufficiency. Anterior discectomy and fusion at the C3/4 level were performed. Postoperatively, the patient experienced complete resolution of symptoms, and dynamic cervical angiography showed disappearance of the compression of the right VA. To our knowledge, this is the first reported case of bow hunter’s stroke diagnosed by dynamic cerebral angiography and cervical 3-D CT without angiography, and treated by anterior decompression and fusion without decompression of the VA.
Keywords: Bow hunter’s stroke, Instability, Uncovertebral joint, 3-D CT angiography, Anterior fusion
Introduction
Bow hunter’s syndrome is a rare symptomatic vertebrobasilar insufficiency presenting as dizziness, vertigo, syncope, nausea, or sensorimotor disturbance due to stenosis or occlusion of the vertebral artery (VA) upon head rotation [1–3]. In most cases, the dominant VA is occluded at the atlanto-axial level and coexisted contralateral hypoplastic VA or poor collateral flow supplied by the anterior cerebral circulation via the posterior communicating artery contributes to this vertebrobasilar insufficiency [2, 4–8]. The extrinsic factors identified VA compression by osteophyte, cervical spondylosis, fibrous bands, cervical disc herniation, or VA stretching by intervertebral instability along the craniocervical axis [3, 7–12].
We report a unique case of the dominant VA stretching stenosis caused by C3–4 excess rotation with the contralateral VA occlusion at the atlanto-axial level on rightward head rotation manifesting as bow hunter’s syndrome. The patient was diagnosed by dynamic cerebral angiogram and cervical 3-D CT without angiogram, and was successfully treated by anterior C3–4 intervertebral fusion.
Case report
Presentation
A 64-year-old man with no relevant past history developed dizziness induced by rotation of his head to the right. The symptom did not improve with conservative therapy by a local physician for 9 months. Furthermore, it progressed to recurrent near-syncope, and he was referred to the outpatient clinic of our department. He was non-diabetic and had no contributing history of head or neck injury, although he was taking medications for hypertension and hypercholesterolemia.
Examination
On admission, the general examination was unremarkable. His near-syncopal episodes that occurred on rotating the head to the right had persisted for more than 5 months, which had limited his cervical range of motion and disturbed his daily activities and his occupation as a truck driver. In particular, he had to rotate his head to the right nearly 90° to ensure safe maneuvering when he drove a right-hand drive truck.
The patient suffered from near-syncopal episodes that developed within a few seconds when rotating the head to the right nearly 90°. He could not hold the rotated position for more than a few seconds because of immediate syncope. These symptoms always resolved completely on returning his head to the neutral position. Leftward rotation of his head did not induce ischemic symptoms. He had no other neurological findings.
Cerebral magnetic resonance imaging (MRI) showed multiple lacunar infarctions in bilateral corona radiata, but there were no contributing lesions, and well-developed posterior communicating arteries were present. Standard anterior–posterior and lateral radiographs of the cervical spine showed no abnormalities and spondylitic change. Dynamic cervical radiography with flexion and extension revealed no instability in the cervical spine. Cervical MRI showed no abnormal structures causing severe external compression to the dural sac or the spinal cord.
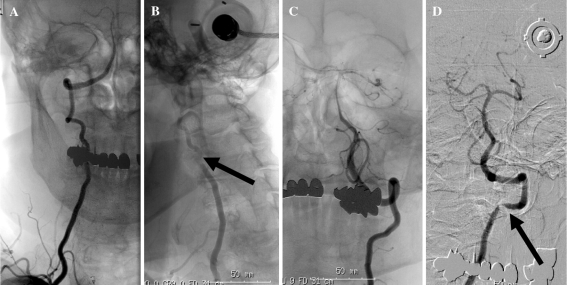
Cerebral angiography showed that the right VA was dominant and the left VA was non-dominant, and both of them had normal flow in the neutral position. Dynamic cervical angiography with rightward head rotation revealed severe stenosis of the dominant right VA at the C3–4 level, with simultaneous severe stenosis of the non-dominant left VA at the atlanto-axial level (Fig. 1). The dominant VA was not compromised at the atlanto-axial level with symptomatic head rightward rotation. Since the patient could tolerate the rotated position for only a few seconds, dynamic examination had to be performed within this time window. No compromise of VA was found either with the head in neutral position or rotation to the left, and the blood supply to the posterior circulation was adequate.
Fig. 1.
Preoperative cerebral angiograms of the right VA show normal flow in the neutral position (a), and severe stenosis between the transverse foramen of C3 and C4 (arrow) and decreased flow on rightward head rotation (b), and angiograms of the left VA show normal flow in the neutral position (c), and severe stenosis at the C1–2 level (arrow) and decreased flow on rightward head rotation (d)
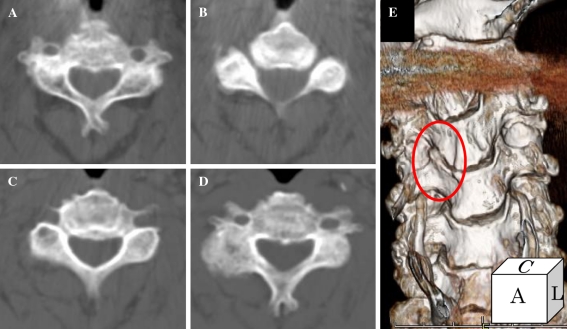
Cervical computed tomography showed no osseous structures protruding into the transverse foramen (Fig. 2a–d). Cervical 3-D CT on rightward head rotation demonstrated displacement of the uncovertebral C3–4 joint, with excessive rotation of the C3 vertebral body, suggestive of C3–4 uncovertebral joint instability (Fig. 2e).
Fig. 2.
Preoperative axial cervical CT scans show no osseous structures in the transverse foramina of C3 (a) and C3/4 (b, c) or C4 (d), and 3-D CT on rightward head rotation shows displacement of the uncovertebral joint at the C3/4 level (e, ellipse)
Based on these findings, his symptoms appeared to be caused by ischemia of bilateral vertebral arteries, mainly due to stretch compression of the right VA at C3–4 during rightward head rotation. The basis for the stretch compression was instability of the right C3/4 uncovertebral joint. Since his symptom failed to improve with conservative therapy, surgical intervention involving C3/4 anterior intervertebral fusion was performed.
Operation
The patient underwent anterior discectomy and fusion at the C3/4 level. He was positioned supine on the operating table with the head slightly extended and rotated to the left. A small roll was placed in the interscapular region. A transverse linear incision along the transverse skin line was made at the C3/4 level under fluoroscopy guidance. The platysma was incised transversely, and the superficial cervical fascia was exposed. The lateral margin of the right omohyoid muscle was dissected to obtain a surgical window formed by the carotid sheath laterally and the esophagus medially. The ventral surfaces of the C3 and the C4 vertebral bodies were exposed, and a discectomy was carried out at the C3–4 level. There were no osteophytic or degenerative changes observed. Anterior discectomy was performed, and a threaded titanium cage, 8 mm in diameter, was inserted into the C3/4 intervertebral space.
Postoperative course
A soft cervical collar was used for 4 weeks postoperatively. Dynamic cervical radiography showed no C3/4 instability. Cerebral angiography was obtained 3 months later. Dynamic angiography on rightward head rotation showed complete disappearance of the right VA stenosis at the C3–4 level and restoration of the blood supply, with slight residual stenosis of the left VA at the C1–2 level (Fig. 3). The patient has not suffered dizziness or near-syncope after the surgery.
Fig. 3.
Postoperative digital subtraction angiograms on rightward head rotation show that stenosis of the right VA has disappeared at the C3–4 level (a), and there is slight residual stenosis of the left VA at C1–2 (arrow) with improved flow after the operation (b)
The patient resumed his previous occupation as a truck driver and has remained asymptomatic.
Discussion
The main cause of this patient’s symptoms can be attributed to stretch compression of the VA at the C3–4 level induced by rightward head rotation. We hypothesize that the stretch compression of the right VA is caused by hyperrotation of the transverse process, due to rotational instability at the C3–4 level. Preoperative cervical 3-D CT in the rotated position showed subluxation of the facet joint at the C3–4 level, which indicates that the facet joint at that level was malfunctioning to some extent.
In several case reports, 3-D CT angiography was used for the diagnosis of bow hunter’s stroke [9, 13]. In the present case, dynamic cerebral angiography demonstrated high-grade stenosis in the left VA at the C3–4 level, and 3-D CT of the cervical spine showed subluxation of the facet joint at the same level. Therefore, 3-D CT angiography was not necessary, because these two findings were enough to make the diagnosis of stretch compression of the VA at the C3–4 level.
Kotani et al. [14, 15] reported that the biomechanical role of uncovertebral joints in cervical segmental stability differs significantly at each intervertebral level because of the distinct anatomic variations. For axial rotational stability of the cervical spine, the uncovertebral joint has a more important role at C3–4 than at lower cervical levels. This theory seems applicable in the present case, in which dynamic cervical 3-D CT showed displacement of the uncovertebral joint only at the C3–4 level, indicating that the C3–4 uncovertebral joint experienced the most loaded condition of the cervical levels. Furthermore, this patient had performed frequent rightward head rotation maneuvers as part of his work as a truck driver for more than 30 years. Such overuse activity may have triggered axial rotational instability of the uncovertebral joint at C3–4 in this patient. This mechanistic defect potentially explains why the stretch compression of the VA occurred at the C3–4 level.
There are several treatments reported for bow hunter’s stroke, including conservative treatment with a neck collar to avoid neck rotation [16]. Anticoagulation may alleviate symptoms [5, 7], but it is only palliative and does not directly treat the underlying pathology [4, 5, 11, 17, 18]. Surgery is an option for patients who fail to respond to conservative therapy [18]. Surgical modalities include decompression of the vertebral artery, C1–2 posterior fusion, and decompression of the VA with anterior cervical fusion. Of course, the choice of treatment for each patient must be individualized and depends on the underlying pathology [2, 5, 6, 17–20]. In the present case, stretch compression of the VA at C3–4 with neck rotation was considered to be the main cause of rotational vertebrobasilar insufficiency. Therefore, to address this problem, anterior discectomy and fusion were performed. There were several reports in which anterior discectomy and fusion with decompression of the VA were performed for bow hunter’s stroke [10, 11, 19]. However, in the present case, because there was no evidence of osteophytic change or cervical disc herniation, compression of the VA by this mechanism seems less likely. Anterior fusion without decompression of the VA was considered sufficient to relieve this patient’s symptoms and resulted in complete resolution of the preoperative symptoms.
Conclusion
Axial rotational instability of the uncovertebral joint can be a cause of bow hunter’s stroke. In such cases, stretching of the VA is the major pathological mechanism. Dynamic cerebral angiography and cervical 3-D CT without angiography were sufficient to confirm the diagnosis. Anterior fusion of this level, without decompression of the VA, can be used as the sole treatment modality. An understanding of the underlying pathological mechanisms in bow hunter’s stroke helps in choosing the most effective treatment strategy.
Acknowledgments
Conflict of interest None of the authors has any potential conflict of interest.
References
- 1.Sorensen BF. Bow hunter’s stroke. Neurosurgery. 1978;2:259–261. doi: 10.1227/00006123-197805000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Matsuyama T, Morimoto T, Sakaki T. Bow Hunter’s stroke caused by a nondominant vertebral artery occlusion: case report. Neurosurgery. 1997;41:1393–1395. doi: 10.1097/00006123-199712000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Kimura T, Sako K, Tohyama Y, Hodozuka A. Bow Hunter’s stroke caused by simultaneous occlusion of both vertebral arteries. Acta Neurochir (Wien) 1999;141:895–896. doi: 10.1007/s007010050394. [DOI] [PubMed] [Google Scholar]
- 4.Gomi M, Hattori I, Horikawa F, Iwasaki K. A case of bow hunter’s stroke treated with endovascular surgery. No Shinkei Geka. 2006;34:189–192. [PubMed] [Google Scholar]
- 5.Horowitz M, Jovin T, Balzar J, Welch W, Kassam A. Bow hunter’s syndrome in the setting of contralateral vertebral artery stenosis: evaluation and treatment options. Spine. 2002;27:E495–498. doi: 10.1097/00007632-200212010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Seki T, Hida K, Akino M, Iwasaki Y. Anterior decompression of the atlantoaxial vertebral artery to treat bow hunter’s stroke: technical case report. Neurosurgery. 2001;49:1474–1476. doi: 10.1097/00006123-200112000-00037. [DOI] [PubMed] [Google Scholar]
- 7.Wakayama K, Murakami M, Suzuki M, Ono S, Shimizu N. Ischemic symptoms induced by occlusion of the unilateral vertebral artery with head rotation together with contralateral vertebral artery dissection–case report. J Neurol Sci. 2005;236:87–90. doi: 10.1016/j.jns.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Bulsara KR, Velez DA, Villavicencio A. Rotational vertebral artery insufficiency resulting from cervical spondylosis: case report and review of the literature. Surg Neurol. 2006;65:625–627. doi: 10.1016/j.surneu.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Kawaguchi T, Fujita S, Hosoda K, Shibata Y, Iwakura M, Tamaki N. Rotational occlusion of the vertebral artery caused by transverse process hyperrotation and unilateral apophyseal joint subluxation: case report. J Neurosurg. 1997;86:1031–1035. doi: 10.3171/jns.1997.86.6.1031. [DOI] [PubMed] [Google Scholar]
- 10.Shinohara N, Kohno K, Takeda S, Ohta S, Sakaki S. A case of bow hunter’s stroke caused by bilateral vertebral artery occlusive change on head rotation to the right. No Shinkei Geka. 1998;26:417–422. [PubMed] [Google Scholar]
- 11.Tsutsumi S, Ito M, Yasumoto Y. Simultaneous bilateral vertebral artery occlusion in the lower cervical spine manifesting as bow hunter’s syndrome. Neurol Med Chir (Tokyo) 2008;48:90–94. doi: 10.2176/nmc.48.90. [DOI] [PubMed] [Google Scholar]
- 12.Vates GE, Wang KC, Bonovich D, Dowd CF, Lawton MT. Bow hunter stroke caused by cervical disc herniation. Case report. J Neurosurg. 2002;96(1 Suppl):90–93. doi: 10.3171/spi.2002.96.1.0090. [DOI] [PubMed] [Google Scholar]
- 13.Matsuyama T, Morimoto T, Sakaki T. Usefulness of three-dimensional CT for bow hunter stroke. Acta Neurochir (Wien) 1997;139:265–266. doi: 10.1007/BF01844765. [DOI] [PubMed] [Google Scholar]
- 14.Kotani Y, McNulty PS, Abumi K, Cunningham BW, Kaneda K, McAfee PC. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study. Spine. 1998;23:1559–1565. doi: 10.1097/00007632-199807150-00011. [DOI] [PubMed] [Google Scholar]
- 15.Oh SH, Perin NI, Cooper PR. Quantitative three-dimensional anatomy of the subaxial cervical spine: implication for anterior spinal surgery. Neurosurgery. 1996;38:1139–1144. doi: 10.1097/00006123-199606000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Hayashi K, Matsuo T, Kurihara M, Shibata S. A case of juvenile bow hunter’s stroke. No To Shinkei. 2000;52:431–434. [PubMed] [Google Scholar]
- 17.Shimizu T, Waga S, Kojima T, Niwa S. Decompression of the vertebral artery for bow-hunter’s stroke. Case report. J Neurosurg. 1988;69:127–131. doi: 10.3171/jns.1988.69.1.0127. [DOI] [PubMed] [Google Scholar]
- 18.Hanakita J, Miyake H, Nagayasu S, Nishi S, Suzuki T. Angiographic examination and surgical treatment of bow hunter’s stroke. Neurosurgery. 1988;23:228–232. doi: 10.1227/00006123-198808000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Velat GJ, Reavey-Cantwell JF, Ulm AJ, Lewis SB. Intraoperative dynamic angiography to detect resolution of Bow Hunter’s syndrome: technical case report. Surg Neurol. 2006;66:420–423. doi: 10.1016/j.surneu.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 20.Netuka D, Benes V, Mikulik R, Kuba R. Symptomatic rotational occlusion of the vertebral artery–case report and review of the literature. Zentralbl Neurochir. 2005;66:217–222. doi: 10.1055/s-2005-836600. [DOI] [PubMed] [Google Scholar]