Abstract
A case of late dislocation of a disc spacer L5/S1 with perforation of the sigmoid colon and transanal passage 4 years after implantation is reported. The objective is to describe an uncommon complication of anterior endoscopic spondylodesis L5/S1. To our knowledge, this is the first report on this rare complication. A 39-year-old patient suffering from a spondylolisthesis L5/S1 (Meyerding grade 2) with bilateral lysis L5 was operated with posterior instrumentation L5/S1 and anterior endoscopic insertion of two disc spacers. 4 years after surgery the patient noticed one of the spacers in the toilet. Radiographic examination of the colon with contrast dye revealed a perforation at the distal sigmoid colon. At the lumbosacral junction there was a bony defect at the site of the absent spacer and an anterior dislocation of the second spacer. A partial resection of the colon at the perforation site with end-to-end anastomosis was performed. The second spacer was removed, and the defect was packed with autologous cancellous bone and local antibiotics. The further course was uneventful. 2 weeks postoperatively the patient was discharged without signs of infection. The radiographic examination after 6 months showed healing of the bone graft with bony fusion L5/S1. In case of incomplete or absent bony fusion the dislocation of intradiscal spacers may arise even years after the primary surgery. In consequence periodical radiographic examinations of spinal instrumentations are recommended until complete bony fusion occurred. Unclear abdominal symptoms following anterior spine surgery require immediate examination.
Keywords: Colon perforation, Anterior spine surgery, Minimal invasive, Spacer dislocation
Introduction
Spinal surgery may adversely affect adjacent visceral structures in the immediate neighbourhood of the anterior spine. Apart from direct trauma during surgery late sequelae have been reported. In the cervical spine esophageal perforation caused by late screw migration after anterior cervical plating has been described [1].
In the lumbosacral region the colon sigmoideum and the rectum are in direct proximity to the spine. Injuries to the colon with perforation have been described in connection with spinal surgery and inflammatory spinal disease [2–5]. However, there is no report on late perforation of the colon caused by migration of a lumbar spinal implant until now.
In this report we present the unusual case of late dislocation of a disc spacer L5/S1 resulting in perforation of the sigmoid colon and its transanal passage 4 years after implantation.
Patient and methods
A 39-year-old patient suffered from chronic low back pain since the age of 16 years. The patient was adipose (166 cm/86 kg) and he was suffered from hypertension and diabetes. Pain increased over years temporarily radiating to both of the legs. Walking distance diminished to less than 2 km. There was an occasional sensory deficit in the left foot. Radiographic examination revealed a spondylolisthesis L5/S1 (Meyerding grade 2) with bilateral isthmic lysis L5 (Fig. 1a).
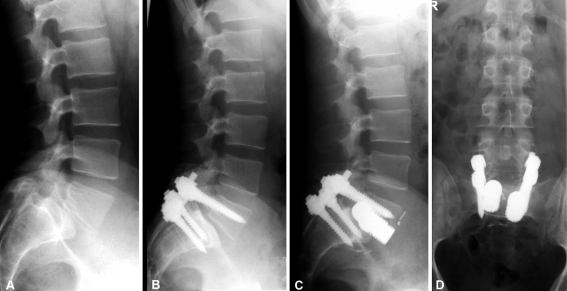
Fig. 1.
39-year-old patient with spondylolisthesis L5/S1 (a). Posterior instrumentation with partial reduction (b), 8 weeks later anterior endoscopic insertion of two disc spacers (c, d)
In January 2002, posterior instrumentation L5/S1 with partial reduction of the spondylolisthesis was performed. 8 weeks later anterior endoscopic spondylodesis L5/S1 was also added (Fig. 1b). Two holes with a diameter of 16 mm were drilled into the disc space and two disc spacers with a diameter of 17 mm (ESKA Disc Dowel) were inserted (Fig. 1c,d). Postoperatively, low back pain improved. There was a slight L5 sensory root lesion on the right side with minimal weakness. Radiographs showed instrumentation and spacers in place; one spacer protruding a few millimetres anteriorly.
At 1 year postoperatively, radiographic examination showed an unchanged position of the spacers. At 2 years postoperatively increasing dislocation of the disc spacers was noticed (Fig. 2a–d). At that time the patient suffered from moderate low back pain. Surgical revision of the dislocated spacers was recommended, however, the patient refused surgery.
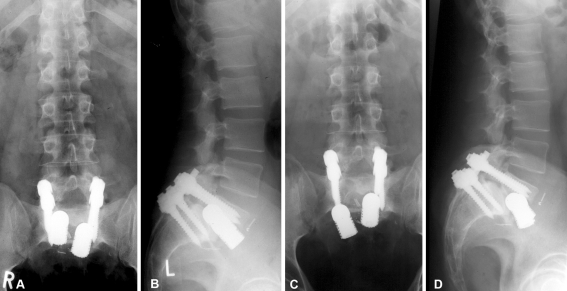
Fig. 2.
Unchanged position of the spacers 1 year postoperatively (a, b), increasing dislocation of the right disc spacer 2 years postoperatively (c, d)
In June 2006, after defecation, the patient noticed one of the spacers in the toilet. Last week he had suffered from abdominal pain and diarrhoea. A white blood count (WBC) was 7,000 and C-reactive protein (CRP) was 6.3 (norm up to 5.0).
Radiographs of the colon with contrast dye revealed a perforation of the distal sigmoid colon with contrast dye extrusion onto the promontory. Computed tomography and conventional radiographic examination of the lumbosacral junction demonstrated a bony defect at the site of the absent spacer and an anterior dislocation of the second spacer. The posterior instrumentation was still in place, but there was no evidence of bony fusion (Fig. 3a–f).
Fig. 3.
Four years postoperatively transanal passage of one spacer (a, b), contrast dye flow from sigma to the defect site (c, d), absent bony fusion L5/S1 (e, f)
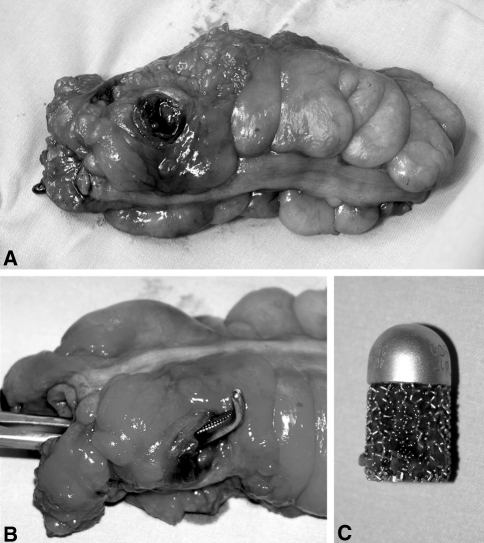
Surgery with partial resection of the colon was performed at the defect site with end-to-end anastomosis (Fig. 4a–c). The lumbosacral junction was approached anteriorly and debridement of the defect site of the absent spacer was carried out. The second spacer was removed, and the defect was packed with autologous cancellous bone and antibiotic gel foam.
Fig. 4.
Perforation of the resected sigmoid colon (a, b), spacer (c)
Result
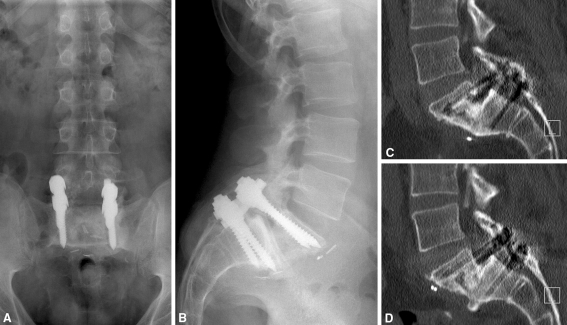
The further course was uneventful. WBC and CRP were normalised and there were no clinical signs of infection. 2 weeks postoperatively the patient was discharged. The radiographic examination after 6 months showed incorporation of the bone graft and bony fusion L5/S1 (Fig. 5a–d).
Fig. 5.
Six months postoperatively solid bony fusion, no signs of infection
At 1 year postoperatively the patient reported occasional minimal pain; he showed a slight sensory L5 root lesion on the right side with minimal dorsal flexion weakness of the foot. He suffered, however, from retrograde ejaculation.
Discussion
Anterior implantation of spacer with posterior instrumentation is a reliable technique for lumbar interbody fusion. In the last decade laparoscopic techniques for anterior fusion have evolved. They are intended to decrease postoperative morbidity and reduce hospitalisation. However, the complication rate of laparoscopic techniques is quite considerable, including vessel injuries, retrograde ejaculation, new radicular pain, and ileus [6–10].
To our knowledge there are no previous reports of a sigmoid colon perforation consequent to late migration of a spacer neither in laparoscopic nor in open anterior lumbar interbody fusion. In the case described, perforation occurred 4 years after implantation of the spacer.
The crucial risk factor for dislocation of an intervertebral spacer is the delayed or absent bony fusion of the segment. Bony bridging of the segment with ingrowth of bone into the surface of the spacer is a safe protection against dislocation. On the other hand, migration of an intradiscal spacer may be induced by repetitive micromotion in the segment consequent to incomplete or the lack of bony fusion. Furthermore, the tendency for dislocation may be influenced by
the shape of the spacer,
the surface of the spacer,
the contact area to the adjacent bone,
the amount of reduction of the spondylolisthesis in relation to the shape of the spacer,
the quality of the bone (cortical, sclerotic, cancellous) and
protrusion forces especially in lordotic segments.
Dislocation may occur posteriorly into the spinal canal [11]. In case of anterior dislocation, the vessels, visceral structures, or nerves may be involved [12, 13]. In the case described above, the anterior dislocation of the spacer caused arrosion of the sigmoid colon with perforation and transanal passage of the spacer. Partial resection of the colon was performed; cancellous bone and local antibiotics were applied at the disc space. Bony fusion was achieved within 6 months.
Conclusion
Routine radiographic examinations of spinal instrumentations are recommended until a reliable bony fusion has occurred. Unclear abdominal symptoms following lumber spinal fusion require immediate and detailed radiographic examination.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Pompili A, Canitano S, Caroli F, Caterino M, Crecco M, Raus L, Occhipinti E. Asymptomatic esophageal perforation caused by late screw migration after anterior cervical plating: report of a case and review of relevant literature. Spine. 2002;27(23):E499–E502. doi: 10.1097/00007632-200212010-00016. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen H, Tomita S, Gillingham B. Small bowel perforation from unit rod posterior spinal fusion. J Pediatr Surg. 2005;40(6):e7–e8. doi: 10.1016/j.jpedsurg.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 3.Peacock JE., Jr Colonic perforation with thigh abscess: an unusual presentation of tuberculous spondylitis. South Med J. 1982;75(5):623–625. doi: 10.1097/00007611-198205000-00035. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz AM, Brodkey JS. Bowel perforation following microsurgical lumbar discectomy. A case report. Spine. 1989;14(1):104–106. doi: 10.1097/00007632-198901000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Shindle MK, Khanna AJ, Hoehner JC, O’Neill PJ, Sponseller PD. Colonic perforation complicating posteroanterior fusion using fibular strut autograft for a high-grade spondylolisthesis. J Spinal Disord Tech. 2002;15(6):546–549. doi: 10.1097/00024720-200212000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Chung SK, Lee SH, Lim SR, Kim DY, Jang JS, Nam KS, Lee HY. Comparative study of laparoscopic L5–S1 fusion versus open mini-ALIF, with a minimum 2-year follow-up. Eur Spine J. 2003;12(6):613–617. doi: 10.1007/s00586-003-0526-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Escobar E, Transfeldt E, Garvey T, Ogilvie J, Graber J, Schultz L. Video-assisted versus open anterior lumbar spine fusion surgery: a comparison of four techniques and complications in 135 patients. Spine. 2003;28(7):729–732. doi: 10.1097/01.BRS.0000051912.04345.96. [DOI] [PubMed] [Google Scholar]
- 8.Frantzides CT, Zeni TM, Phillips FM, Mathur S, Zografakis JG, Moore RM, Laguna LE. L5–S1 laparoscopic anterior interbody fusion. JSLS. 2006;10(4):488–492. [PMC free article] [PubMed] [Google Scholar]
- 9.Inamasu J, Guiot BH. Laparoscopic anterior lumbar interbody fusion: a review of outcome studies. Minim Invasive Neurosurg. 2005;48(6):340–347. doi: 10.1055/s-2005-915634. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser MG, Haid RW, Jr, Subach BR, Miller JS, Smith CD, Rodts GE., Jr Comparison of the mini-open versus laparoscopic approach for anterior lumbar interbody fusion: a retrospective review. Neurosurgery. 2002;51(1):97–103. doi: 10.1097/00006123-200207000-00015. [DOI] [PubMed] [Google Scholar]
- 11.McAfee PC, Cunningham BW, Lee GA, Orbegoso CM, Fedder IL, Griffith SL. Revision strategies for salvaging or improving failed cylindrical cages. Spine9. 1999;24(20):2147–2153. doi: 10.1097/00007632-199910150-00015. [DOI] [PubMed] [Google Scholar]
- 12.Cakmak A, Gyedu A, Kepenekçi I, Ozcan C, Unal AE. Colon perforation caused by migration of a bone graft following a posterior lumbosacral interbody fusion operation: case report. Spine. 2010;35(3):E84–E85. doi: 10.1097/BRS.0b013e3181bb1bf2. [DOI] [PubMed] [Google Scholar]
- 13.Yoshimoto H, Sato S, Nakagawa I, Hyakumachi T, Yanagibashi Y, Nitta F, Masuda T. Deep vein thrombosis due to migrated graft bone after posterior lumbosacral interbody fusion. Case report. J Neurosurg Spine. 2007;6(1):47–51. doi: 10.3171/spi.2007.6.1.47. [DOI] [PubMed] [Google Scholar]