Abstract
Background
Myofascial pain syndrome (MPS) is a regional musculoskeletal pain disorder that is caused by myofascial trigger points. The objective of this study was to determine the prevalence of MPS among chronic back pain patients, as well as to identify risk factors and the outcome of this disorder.
Methods
This was a prospective observational study involving 126 patients who attended the Pain Management Unit for chronic back pain between 1st January 2009 and 31st December 2009. Data examined included demographic features of patients, duration of back pain, muscle(s) involved, primary diagnosis, treatment modality and response to treatment.
Results
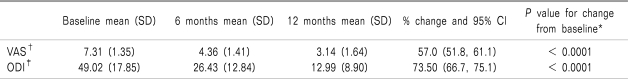
The prevalence of MPS among chronic back pain patients was 63.5% (n = 80). Secondary MPS was more common than primary MPS, making up 81.3% of the total MPS. There was an association between female gender and risk of developing MPS (χ2 = 5.38, P = 0.02, O.R. = 2.4). Occupation, body mass index and duration of back pain were not significantly associated with MPS occurrence. Repeated measures analysis showed significant changes (P < 0.001) in Visual Analogue Score (VAS) and Modified Oswestry Disability Score (MODS) with standard management during three consecutive visits at six-month intervals.
Conclusions
MPS prevalence among chronic back pain patients was significantly high, with female gender being a significant risk factor. With proper diagnosis and expert management, MPS has a favourable outcome.
Keywords: chronic back pain, myofascial pain syndrome, trigger point
INTRODUCTION
Myofascial pain syndrome (MPS) is a trigger point-induced regional musculoskeletal pain disorder affecting one or more muscles or groups of muscles. A myofascial trigger point is defined as a hyperirritable spot, usually within a taut band of skeletal muscle or in the muscle fascia, which is painful on compression and can give rise to characteristic referred pain, motor dysfunction, and autonomic phenomena [1].
MPS is a common cause of pain and dysfunction in the musculoskeletal system. It accounts for 20% to 95% of patients with musculoskeletal pain presenting at general medical clinics and pain management centres [2-6]. Despite the prevalence of MPS, awareness among clinicians is still inadequate, which results in this condition often being misdiagnosed or underdiagnosed and thus under-treated [7-9].
The purpose of this study was to review our experience with MPS in patients with chronic back pain in order to provide local data on prevalence, risk factors and outcome of patients with MPS.
MATERIALS AND METHODS
After approval by the Ethics Committee of University Science Malaysia, a prospective observational study was carried out on 126 consecutive patients who attended the Pain Management Unit at Hospital University Science Malaysia, Kelantan, between 1st January and 31st December 2009 for chronic back pain (i.e. lasting more than 6 months). Data examined included patient demographic features, duration of back pain, muscle(s) involved, primary diagnosis, treatment modality and response to treatment.
MPS diagnosis was based upon the presence of a trigger point, reproducible pain, taut band, referred pain and jump sign. Initially, patients were requested to point to the painful spot with one finger in order to locate a trigger point. A trigger point was identified when a painful nodule on a muscle was felt through either a flat or pincer palpation technique. During palpation or compression of that point, reproduction of recognized pain was taken as one of the criteria for MPS diagnosis. A force of approximately 2 kg was applied in order to palpate the trigger point or to elicit reproducible pain. A taut band can be felt as a rope-like induration that extends from a trigger point nodule to the attachment of the taut muscle fibers at each end of the muscle. The taut band can be snapped or rolled under the finger in accessible muscles. Referred pain was defined as any pain felt away from the area of palpation. The presence of referred pain depends on the amount of pressure applied and thus also depends on subcutaneous thickness; the pressure of compression was adjusted to a constant level by applying digital pressure that caused the finger to blanch. When the nail turned pale, the amount of pressure was measured to be approximately 3 to 4 kg/cm2. Jump sign is a general pain response of the patient who winces, may cry out or may withdraw in response to pressure applied on a trigger point. Subjective complaints of pain were measured using a visual analogue scale (VAS) between 0 and 10. Functional disability was assessed with the Modified Oswestry Disability Score (ODI) between 0 and 100.
All patients with MPS were subjected to standard therapy consisting of physical therapy, oral medication and exercise. Trigger point injection was given when the initial pain score was > 7 or when other modes of therapy failed to alleviate pain during subsequent visits. In the event of more than one muscle involved in MPS, trigger point injection was given to the most painful muscle. Follow-up visits that fell within one month of the specified six monthly intervals were chosen to represent those points in follow-up.
1. Data analysis
Data were analyzed using SPSS software version 12.0. Frequency and descriptive statistics were calculated to check all relevant characteristics of the data. χ2 analysis was performed to detect the relationship between MPS occurrence and potential risk factors. Differences in VAS and ODI during three consecutive visits were measured with repeated measure ANOVA.
RESULTS
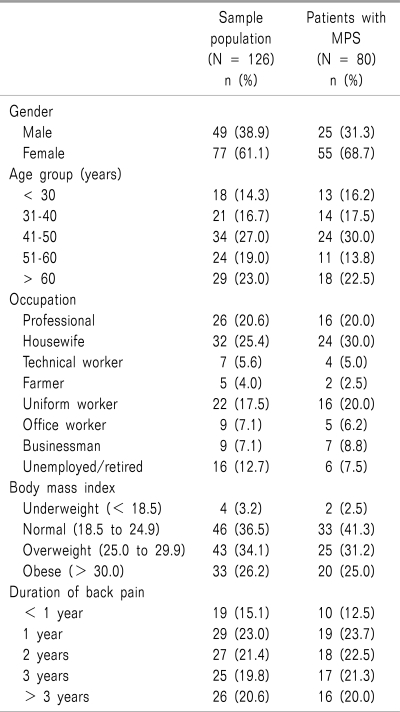
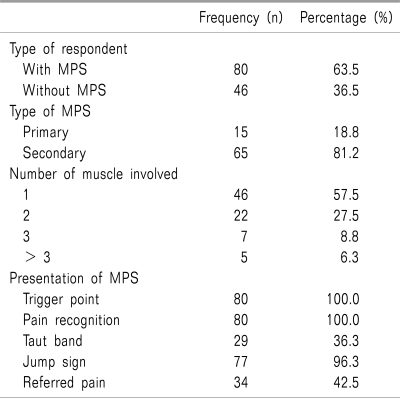
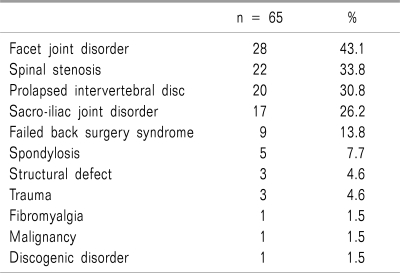
A total of 126 patients were included in this study. The mean age of patients was 48.5 ± 15.0 years, and 61.1% of the patients were women. Distribution of socio-demographic study variables among patients are shown in Table 1. Eighty out of 126 patients fulfilled the MPS criteria, thus giving a prevalence of 63.5%. Secondary MPS was the most common type (81.2%). Characteristics of MPS are summarized in Table 2. Causes of secondary MPS are listed in Table 3.
Table 1.
Demographic Characteristics of all Patients and Patients With MPS
Table 2.
Characteristics of Myofascial Pain Syndrome
Table 3.
Secondary Causes of MPS
Demographic characteristic of patients and causes of secondary MPS were analysed with the χ2 test to find an association with MPS occurrence. Only female gender was found to be significantly associated with occurrence of MPS: χ2 = 5.38, P = 0.02, O.R. = 2.4.
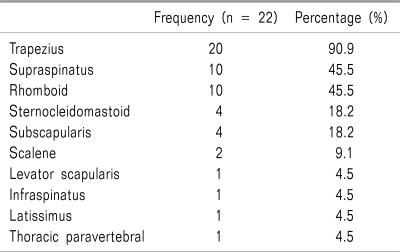
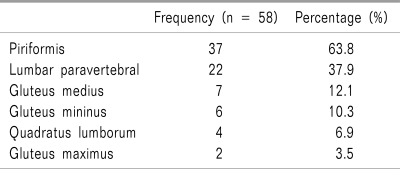
The muscles involved in patients with MPS were categorized according to their location in the upper or lower half of the body (shown in Table 4 and 5, respectively). In the upper half of the body, the trapezius was the commonest muscle involved, while the piriformis was found to be the commonest muscle affected in the lower half of the body.
Table 4.
Muscles of Myofascial Pain Syndrome in Upper Half of the Body
Table 5.
Muscles of Myofascial Pain Syndrome in Lower Half of the Body
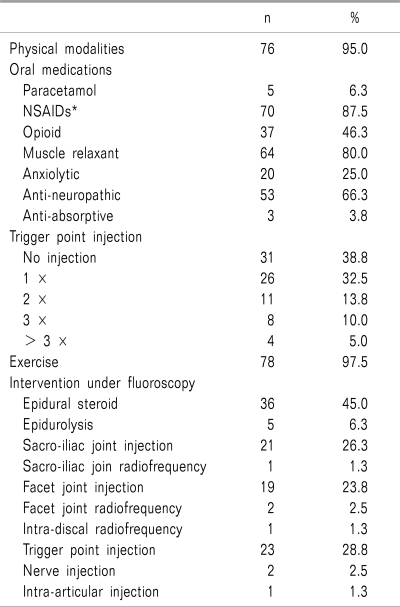
Treatment for MPS in this study is shown in Table 6. Almost all patients were subjected to physical modalities, exercise and a combination of oral medications. NSAIDs were the most frequent oral medication prescribed to patients. Treatment for causes of secondary MPS was done under fluoroscopy guidance. Reduction in both VAS and ODI was found to be significant, as shown in Table 7.
Table 6.
Treatment Modalities of MPS
*NSAIDs: non-steroidal anti-inflammatory drugs.
Table 7.
The Changes of VAS and ODI Over Time
*P value from repeated measurements analysis ANOVA, †VAS: visual analogue score, ‡ODI: Oswestry disability score.
DISCUSSION
In our study, MPS prevalence among our patients was 63.5%, which is consistent with findings reported in many studies and review articles across different populations [2,4-6]. This suggests that MPS is a major health problem among populations. We had no difficulty in making the diagnosis of MPS among our patients as the clinical presentation was classical.
Female gender was found to be a significant risk factor for developing MPS with an odds ratio of 2.4. This is consistent with the findings of Fricton et al. [2] and Drewes and Jennum [10], both of which found that MPS is more prevalent in female than male patients. This was attributed to the hormonal changes in women, whereby pain was reported to increase during the second week of the menstrual cycle [11]. More extensive research into this matter is warranted in order to establish the possible causal relationship between female gender and MPS.
Apart from female gender, other variables were found to be insignificant risk factors for MPS. These findings lead us to believe that MPS can present in any age group, occupation, or weight, as long as precipitating and perpetuating factors are present. Although there are numerous references describing the pathogenesis and treatment of MPS, there are limited studies discussing its risk factors [12]. Comparison with other studies in the area is also limited.
Upper back pain is a common symptom of trapezius and para spinal muscle MPS. Myofascial trigger point development in this area is commonly due to habitual poor posture, emotional stress and overuse or secondary to degenerative cervical joint disease or trauma [6,13]. Flax [14] reported that MPS of the trapezius and scalene muscles can potentially present as a co-morbidity of cervical spondylosis. The finding of piriformis being the most common muscle involved in the lower half of the body is consistent with the statement by Hains [15], 2002 that MPS of the piriformis and the muscles around the posterior superior iliac spine, the iliac crest and posterior sacroiliac line are common sources of lower back pain. In addition, MPS of the piriformis muscle has been recognized as a common cause of Piriformis Syndrome, a clinical symptom of sciatica secondary to compression or irritation of the sciatic nerve by an abnormal piriformis muscle. It has been documented as a primary or contributory cause for sciatica and lower back pain [16].
The primary goal of management for MPS is to break the vicious cycle of pain through elimination of trigger points. A multi-disciplinary approach is required in managing MPS [17]. In this study, once diagnosed with MPS, patients were subjected to proven efficacious treatment, which included physical therapy (heat and ultrasound), oral medication, and exercise (stretching and strengthening) with or without trigger point injection [18,19]. Thirty-one patients were not given trigger point injection as 14 of them claimed to have tolerable pain (VAS ≤ 6), while the remaining 17 refused despite having a VAS ≥ 7. For those who accepted trigger point injection (n = 49), the majority required only one or two injections. Only 4 patients required more than 3 injections. These patients were regarded as having refractory MPS, and were offered Botulinum A injection. Most previously published studies measured the efficacy of various treatment modalities for MPS based on a short-term outcome. In our study, however, we examined the overall outcome over a twelve-month period, which was favourable in terms of reduction in VAS and ODI. These findings emphasised that a multi-disciplinary approach to MPS treatment is required in order to provide long-term benefit in pain relief.
In conclusion, MPS is common and poses a major health problem in the Malaysian population. Furthermore, female gender is a significant risk factor for MPS. The outcome of this syndrome is favourable if proper diagnosis and prompt management is undertaken.
References
- 1.Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: The trigger point manual. Baltimore: Williams & Wilkins; 1999. pp. 21–34. [Google Scholar]
- 2.Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60:615–623. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- 3.Fishbain DA, Goldberg M, Meagher BR, Steele R, Rosomoff H. Male and female chronic pain patients categorized by DSM-III psychiatric diagnostic criteria. Pain. 1986;26:181–197. doi: 10.1016/0304-3959(86)90074-6. [DOI] [PubMed] [Google Scholar]
- 4.Skootsky SA, Jaeger B, Oye RK. Prevalence of myofascial pain in general internal medicine practice. West J Med. 1989;151:157–160. [PMC free article] [PubMed] [Google Scholar]
- 5.Cakit BD, Taskin S, Nacir B, Unlu I, Genc H, Erdem HR. Comorbidity of fibromyalgia and cervical myofascial pain syndrome. Clin Rheumatol. 2010;29:405–411. doi: 10.1007/s10067-009-1342-5. [DOI] [PubMed] [Google Scholar]
- 6.Moon CW. Myofascial pain syndrome. Korean J Pain. 2004;17(Suppl):36–44. [Google Scholar]
- 7.Marcus NJ. Failure to diagnose pain of muscular origin leads to unnecessary surgery. Pain Med. 2002;3:161–166. doi: 10.1046/j.1526-4637.2002.02020.x. [DOI] [PubMed] [Google Scholar]
- 8.Ceneviz C, Maloney G, Mehta N. Myofascial pain may mimic trigeminal neuralgia. Cephalalgia. 2006;26:899–901. doi: 10.1111/j.1468-2982.2006.01123.x. [DOI] [PubMed] [Google Scholar]
- 9.Facco E, Ceccherelli F. Myofascial pain mimicking radicular syndromes. Acta Neurochir Suppl. 2005;92:147–150. doi: 10.1007/3-211-27458-8_32. [DOI] [PubMed] [Google Scholar]
- 10.Basford JR, An KN. New techniques for the quantification of fibromyalgia and myofascial pain. Curr Pain Headache Rep. 2009;13:376–378. doi: 10.1007/s11916-009-0061-6. [DOI] [PubMed] [Google Scholar]
- 11.Severino SK, Moline ML. Premenstrual syndrome. Obstet Gynecol Clin North Am. 1990;17:889–903. [PubMed] [Google Scholar]
- 12.Simons DG, Dommerholt J. Myofascial trigger points and myofascial pain syndrome: a critical review of recent literature. J Man Manip Ther. 2006;14:E124–E171. [Google Scholar]
- 13.Yap EC. Myofascial pain--an overview. Ann Acad Med Singapore. 2007;36:43–48. [PubMed] [Google Scholar]
- 14.Flax HJ. Myofascial pain syndromes: the great mimicker. Bol Asoc Med P R. 1995;87:167–170. [PubMed] [Google Scholar]
- 15.Coaccioli S, Varrassi G, Sabatini C, Marinangeli F, Giuliani M, Puxeddu A. Fibromyalgia: nosography and therapeutic perspectives. Pain Pract. 2008;8:190–201. doi: 10.1111/j.1533-2500.2008.00188.x. [DOI] [PubMed] [Google Scholar]
- 16.Durrani Z, Winnie AP. Piriformis muscle syndrome: an underdiagnosed cause of sciatica. J Pain Symptom Manage. 1991;6:374–379. doi: 10.1016/0885-3924(91)90029-4. [DOI] [PubMed] [Google Scholar]
- 17.Kamanli A, Kaya A, Ardicoglu O, Ozgocmen S, Zengin FO, Bayik Y. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25:604–611. doi: 10.1007/s00296-004-0485-6. [DOI] [PubMed] [Google Scholar]
- 18.Han SC, Harrison P. Myofascial pain syndrome and trigger-point management. Reg Anesth. 1997;22:89–101. doi: 10.1016/s1098-7339(06)80062-3. [DOI] [PubMed] [Google Scholar]
- 19.Lavelle ED, Lavelle W, Smith HS. Myofascial trigger points. Anesthesiol Clin. 2007;25:841–851. doi: 10.1016/j.anclin.2007.07.003. [DOI] [PubMed] [Google Scholar]