Abstract
Meralgia paresthetica is a rarely encountered sensory mononeuropathy characterized by paresthesia, pain or sensory impairment along the distribution of the lateral femoral cutaneous nerve (LFCN) caused by entrapment or compression of the nerve as it crossed the anterior superior iliac spine and runs beneath the inguinal ligament. There is great variability regarding the area where the nerve pierces the inguinal ligament, which makes it difficult to perform blind anesthetic blocks. Ultrasound has developed into a powerful tool for the visualization of peripheral nerves including very small nerves such as accessory and sural nerves. The LFCN can be located successfully, and local anesthetic solution distribution around the nerve can be observed with ultrasound guidance. Our successfully performed ultrasound-guided blockade of the LFCN in meralgia paresthetica suggests that this technique is a safe way to increase the success rate.
Keywords: lateral femoral cutaneous nerve, meralgia paresthetica, ultrasound
Meralgia paresthetica is characterized by pain or paresthetica along the lateral femoral cutaneous nerve (LFCN) and is caused when this nerve is entrapped by fibrosis of the nerve or other various reasons. The LFCN is a small pure sensory nerve that emerges from the lumbar plexus, runs along the iliacus and reaches the femoral region through the inguinal ligament.
Currently, for the diagnosis and treatment of meralgia paresthetica, blocking of the LFCN is performed. This is performed using the anatomical landmarks of this nerve, but there are many difficulties in performing a blind block due to the anatomical diversity of the nerve; consequently, the failure rate has been reported as high as 60% [1].
Ultrasound nowadays is being developed into a powerful tool that can observe very small peripheral nerves, such as accessory nerves or sural nerves, so its usage in periphery nerve block is increasing [2]. Ultrasound can confirm the target nerve and surrounding structures so diagnosis is more accurate, additional damage is reduced during administration of medication and injection of steroids and local anesthetic agent can be done at the exact location. Compared to blind blocks, the amount of local anesthetic agent can be reduced, lessening systemic toxicity from the local anesthetic agent [3].
We report a successfully performed ultrasound-guided blockade of the LFCN in a patient with meralgia paresthetica.
CASE REPORT
A 46-year-old female patient was admitted with complaints of severe pain and paresthetica in the right anterolateral femoral region, which started a month ago. At the time of admittance, the visual analog scale (VAS) of the patient was 8, and she complained of excruciating pain in the right femoral region when she started to walk, causing her to rest more than 5 minutes before walking again. Recently, she had even woken once or twice in the night from the pain in the right femoral region. There was no pain in the lumbar region. To treat these symptoms, the patient had visited a private orthopedics hospital, but there were no abnormalities in the lumbar x-ray, and despite continual physical modalities, there were no improvements in symptoms. After careful history taking, it was found that she had a total thyroidectomy 8 months previous because of a thyroid mass, and after the procedure her weight increased 27 kg, from 67 kg to 94 kg. In the standing position the lower abdominal fat of the patient hung over the inguinal area (Fig. 1). There were no other metabolic diseases such as diabetes mellitus. In the physical exam, the straight leg raising test was normal, there was numbness in the right lateral femoral region, and there were trigger points along the inguinal ligament that generated symptomatic pain when pressured.
Fig. 1.
Standing position. A picture which shows inguinal area is covered with fat tissues of lower abdominal area.
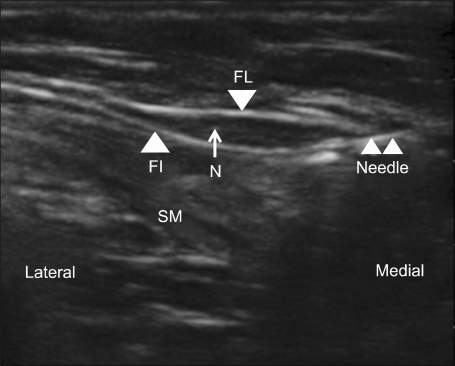
Based on the past history and physical exam, meralgia paresthetica was suspected, so a lateral femoral cutaneous nerve block using ultrasound (S-nerve™, Sonosite Inc., Bothell WA., USA) was planned for the purpose of diagnosis and treatment. First, the block area was sterilized with 102% povidine and surgically draped. Jelly was applied to the linear probe (13-6 Hz) and disinfected transparent plastic was draped. The end of the linear probe was positioned at the anterior superior iliac spine (ASIS), and in line with the inguinal ligament it was moved down and confirmed the LFCN located above the Sartorius and below the tensor fasciae latae (Fig. 2). A 23 gauge, 60 mm needle was inserted facing the lateral from the medial side of the patient and positioned near the LFCN by monitoring the current position using ultrasound. A mixture of 1:10,000 epinephrine 0.15 ml, 0.2% bupivacaine 9 ml, and triamcinolone acetonide 40 mg was injected around the nerve while monitoring medication diffusion with ultrasound. After injection, the patient was bed rested for 30 minutes and returned home without complications. In a visit a week later, the patient's VAS had been reduced to 3. Using the same method as the first procedure, the procedure was performed once more but with half the amount of bupivacaine and triamcinolone acetonide, that is 1:10,000 epinephrine 0.15 ml, 0.2% bupivacaine 5 ml, and triamcinolone acetonide 20 mg. A week after the second procedure, a medical examination was conducted over the telephone and the VAS had decreased to 0. Currently, 4 months after the procedure the condition has improved without complications.
Fig. 2.
Ultrasound image of the lateral femoral cutaneous nerve in the short axis. FL: fascia lata, FI: fascia iliaca, N: lateral femoral cutaneous nerve, SM: Sartorius muscle.
DISCUSSION
Lateral femoral cutaneous nerve block for the treatment of meralgia paresthetica is a commonly known treatment method, but there were no reports of procedures using ultrasound in South Korea.
Hafer first presented meralgia paresthetica in 1885, reporting pressure on the lateral femoral cutaneous nerve as cause for the pain. From the Greek words meros (thigh) and algos (pain), Roth named it "meralgia paresthetica" in 1895, which has been used up to the present time [4].
Meralgia paresthetica is characterized by pain and paresthica along the LFCN and is caused by compression of the nerves from conditions that increase intra-abdominal pressure such as obesity, pregnancy, tight belts or pants, metabolic disorders (diabetes), alcohol and lead poisoning, or damage from surgeries near the inguinal region because of anatomical variability of the LFCN. Obesity is considered to be the reason in our case since there was a recent 27 kg increase in body weight.
The LFCN is a pure sensory nerve that originates from the 2, 3 lumbar nerves emerges from the side of the psoas major and passes the iliacus diagonally towards the ASIS. It then passes above, below or between the inguinal ligament, above the Sartorius and into the subcutaneous tissue of the femoral region. Then it is divided into anterior and posterior division: the front controls the frontal femoral region and up to the knee area, the rear controls the lateral femoral region up to the greater trochanter area.
The anatomical variability of the LFCN is about 30% [5], and according to reports of Bjurlin et al. [6], the distance from the ASIS to the LFCN can vary from 0.3-6.5 cm. For these reasons, there have been many methods suggested for LFCN block. However, blind blocks have had a failure rate of more than 60% and there could be blockages of the femoral or obturator nerve or intra-abdominal insertion [1]. Nerve stimulators can reportedly increase the success rate up to 85%, but their use doubles the time needed and results can vary depending on the patient's subjective complaints of paresthetica [1].
Recently, ultrasound usage has increased dramatically in the area of pain medicine since it can confirm the target nerve and surrounding structures to allow accurate diagnosis, reduce additional damage when injecting medication, and allow injection of steroids or local anesthetic agents in the exact location.
Ng et al. [7] investigated whether ultrasound was an accurate tool to find the location of the LFCN in 20 cadavers and 10 volunteers. The location of the LFCN found through anatomical landmarks of 2.5 cm interior and 2.5 cm below the ASIS was compared with the location of the LFCN found using ultrasound. Accuracy was confirmed by dissection of the cadavers, and location of the actual nerve was confirmed by using the transdermal nerve stimulators in the volunteers. Location accuracy using anatomical landmarks was 5.3% in cadavers and 0% in volunteers, while accuracy of the ultrasound was 84.2% in cadavers and 80% in volunteers. This study demonstrated how inaccurate blind block according to anatomical landmarks can be due to anatomical variance of the LFCN, while highlighting the accuracy of ultrasound-guided procedures.
Lee et al. [8] performed an LFCN block using blind technique in patients with meralgia paresthetica. From the three cases, two showed successful results, and the procedure was performed 4 and 3 times, respectively, for the 2 cases. Although the type of local anesthesia used was different, since our case obtained effective treatment results with less local anesthesia in two procedures, it can be suggested that ultrasound-guided blockage of the LFCN is more effective than results from blind technique.
It is commonly known that the amount of local anesthetic agent used is reduced in ultrasound-guided nerve blocks [8]. When blocking the LFCN, the amount of local anesthetic agent used in blind blocks is no less than 30 ml [9], while in ultrasound-guided LFCN blocks, usually 10 to 15 ml is recommended [10]. Hurdle et al. [11] also reported a 100% success rate in ultrasound-guided blockage of the LFCN in 10 patients with small anesthetic dosages of 1 ml to 8 ml. Reducing the amount of local anesthetic agent used can reduce systemic toxicity as well as the risk of unintended blockage of the femoral or obturator nerves [9].
One week after the second procedure was performed, there were improvements in the VAS and no complaints of sensory impairment or motor weakness in unintended areas, despite using half the amount of local anesthetic agent compared to the first procedure. This effective result without unintended blocks was from accurate injection using ultrasound despite the small amount of local anesthetic agent used compared to blind blockage. Future research regarding minimum dosage of local anesthetic agent required when performing ultrasound-guided blockage of LFCN will be necessary.
References
- 1.Shannon J, Lang SA, Yip RW, Gerard M. Lateral femoral cutaneous nerve block revisited. A nerve stimulator technique. Reg Anesth. 1995;20:100–104. [PubMed] [Google Scholar]
- 2.Bodner G, Harpf C, Gardetto A, Kovacs P, Gruber H, Peer S, et al. Ultrasonography of the accessory nerve: normal and pathologic findings in cadavers and patients with iatrogenic accessory nerve palsy. J Ultrasound Med. 2002;21:1159–1163. doi: 10.7863/jum.2002.21.10.1159. [DOI] [PubMed] [Google Scholar]
- 3.Eichenberger U, Stöckli S, Marhofer P, Huber G, Willimann P, Kettner SC, et al. Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided, nerve dimension-based method. Reg Anesth Pain Med. 2009;34:242–246. doi: 10.1097/AAP.0b013e31819a7225. [DOI] [PubMed] [Google Scholar]
- 4.Grossman MG, Ducey SA, Nadler SS, Levy AS. Meralgia paresthetica: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:336–344. doi: 10.5435/00124635-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Keegan JJ, Holyoke EA. Meralgia paresthetica: an anatomical and surgical study. J Neurosurg. 1962;19:341–345. doi: 10.3171/jns.1962.19.4.0341. [DOI] [PubMed] [Google Scholar]
- 6.Bjurlin MA, Davis KE, Allin EF, Ibrahim DT. Anatomic variations in the lateral femoral cutaneous nerve with respect to pediatric hip surgery. Am J Orthop. 2007;36:143–146. [PubMed] [Google Scholar]
- 7.Ng I, Vaghadia H, Choi PT, Helmy N. Ultrasound imaging accurately identifies the lateral femoral cutaneous nerve. Anesth Analg. 2008;107:1070–1074. doi: 10.1213/ane.0b013e31817ef1e5. [DOI] [PubMed] [Google Scholar]
- 8.Lee HK, Chung SY, Lee SY, Suh YS, Kim C. Management of meralgia paresthetica by lateral femoral cutaneous nerve block: case reports. J Korean Pain Soc. 1995;8:152–155. [Google Scholar]
- 9.Sharrock NE. Inadvertent "3-in-1 block" following injection of the lateral cutaneous nerve of the thigh. Anesth Analg. 1980;59:887–888. [PubMed] [Google Scholar]
- 10.Brown DL. Atlas of regional anesthesia. 2nd ed. Philadelphia: WB Saunders; 1999. p. 114. [Google Scholar]
- 11.Hurdle MF, Weingarten TN, Crisostomo RA, Psimos C, Smith J. Ultrasound-guided blockade of the lateral femoral cutaneous nerve: technical description and review of 10 cases. Arch Phys Med Rehabil. 2007;88:1362–1364. doi: 10.1016/j.apmr.2007.07.013. [DOI] [PubMed] [Google Scholar]