Abstract
Background
Lidocaine patch (L5P) has demonstrated short-term efficacy in treating both acute surgical pain and chronic neuropathic pain with tolerable side effects. Percutaneous endoscopic lumbar discectomy (PELD) is the mainstay of minimally invasive spine surgery (MISS). Sufficient analgesia during PELD surgery makes the patient consider it real MISS. This study was performed to evaluate the efficacy and adverse effects of lidocaine patch in patients who underwent PELD under local anesthesia.
Methods
L5P (L group) or placebo (P group) was randomly applied on the skin of the back covering the anticipated path of the working channel before 1 hour of surgery in 100 patients who underwent a single level PELD at L4-L5. Efficacy of the lidocaine patch was assessed by patient's numeric rating scale (NRS) of pain at each stage during the surgery and by a 5-scale grading of the satisfaction with the anesthesia of the operator and patients after surgery.
Results
Mean NRS scores at the stages of needle insertion, skin incision, serial dilation and insertion of working channel, and subcutaneous suture were significantly lower in the L group than the P group. Postoperative operator's and patients' satisfaction scores were also significantly higher in L group than in the P group. There were subtle adverse effects in both groups.
Conclusions
L5P provided better pain relief during PELD, especially at the stage of needle insertion, skin incision, serial dilation and insertion of working channel, and subcutaneous suture. It also provided higher patient and operator postoperative satisfaction, with only subtle adverse effects.
Keywords: analgesia, endoscopy, lidocaine, percutaneous discectomy, transdermal patch
INTRODUCTION
In the treatment of chronic neuropathic pain such as postherpetic neuralgia, lidocaine 5% patch (L5P) has demonstrated short-term efficacy with tolerable side effects including erythema, rash, and minimal systemic absorption [1,2]. Trials on its use for the treatment of acute somatic pain in procedures such as local anesthesia for vascular access procedures and minor dermatological procedures have been conducted [3,4].
Percutaneous endoscopic lumbar discectomy (PELD) is a mainstay of minimally invasive spine surgery (MISS) [5]. Sufficient analgesia during the surgery, however, makes the patient feel as if it is real MISS. Therefore, it is important for the operator to recognize potential nerve damage during MISS, the preferred route of performing PELD is under local anesthesia with intravenous analgesia rather than under general anesthesia accompanied with complicated neural monitoring systems. In addition, it is also difficult to ignore the risks involved in general anesthesia such as accidental extubation or disposition of endotracheal tube during operation with the patient in prone position.
This study was designed and performed to evaluate the efficacy and adverse effects of the lidocaine patch in patients who underwent PELD.
MATERIALS AND METHODS
This study was conducted at the pain clinics at Pusan National University Hospital and Pusan National University Yangsan Hospital in Korea from March 2008 to February 2010. The study was approved by the Policy of the Ethical Committee at Pusan National University Hospital Institutional Review Board. All eligible patients were informed about the study, and written consent was obtained from all participants.
The 100 included in the study were scheduled to receive single-level PELD at the L4-L5. They were scheduled for PELD due to refractory pain experienced following repeated epidural steroid injection, motor deficit, or cauda equina syndrome. The operator marked the anticipated approach site on the skin, usually 10 cm from the midline before 1 day of the surgery. They were randomly allocated to be given either 700 mg of L5P (Lidotop patch; Teikoku Pharma-, Sanbonmatsu, Japan) or a placebo patch, 10 × 14 cm in size; the 2 groups were referred to as the L and P groups, prospectively. The placebo patch could not be obtained from the manufacturer of L5P; therefore, the patch from the manufacturer was peeled off, and the opposite inactive side was applied on the patients' skin in the P group. Using a random-number table, the nurses randomly applied a patch with its active or inactive side down on the skin surface marked previously by the operator before 1 hour of the surgery. To ensure tight adhesion of the patch to the skin, adhesive plaster was applied on top to cover the patch and adjacent skin in both groups. Another nurse removed the patch immediately after the patient entered the operating room. The operator and patient were blind to whether the patch was applied on its active or inactive side.
The PELD procedure was divided into 8 stages according to the perceived painful events associated with it: (a) needle insertion; (b) discography; (c) skin incision; (d) serial dilation and insertion of working channel; (e) anulotomy; (f) discectomy; (g) radiofrequency or laser ablation of the ingrown nerves into the nucleus pulposus and inner anulus; and (h) subcutaneous suturing [6]. The pain was assessed using a patient's numeric rating scale (NRS), from 0 to 10, with 0 being no pain at all and 10 being the worst pain imaginable among all 8 stages during surgery. Operator and patient satisfaction with the anesthesia was assessed by 5 grades, namely, "excellent (-100%), very good (-75%), good (-50%), fair (-25%), and poor (-0%)," after PELD surgery. Adverse effects were also recorded.
Conventional analgesics: (a) preoperative intravenous 50 microgram of fentanyl and 30 mg of ketorolac, (b) preoperative skin and subcutaneous infiltration of 10 ml of 1% lidocaine, and (c) intraoperative additional intravenous injection 50 µg of fentanyl with anular infiltration of 2 ml of 1% lidocaine before anulotomy were also administrated in both patient groups.
Statistical analysis was performed using the SPSS ver. 12.0 for Windows software (SPSS Inc., Chicago, IL). All values were calculated as mean ± SD. Demographic characteristics, such as age and sex of patients, were analyzed using the Student t-test and the chi-square test for the inter-group comparison, respectively. The mean NRS score at each stage of PELD procedure was compared between groups using a Student t-test. The scaling percentages given by the operator and patient on postoperative satisfaction with the anesthesia were analyzed between groups using a chi-squared test.
RESULTS
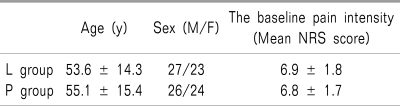
The mean age (L: 53.6 ± 14.3 years; P: 55.1 ± 15.4 years) and sex distribution (L: M/F = 27/23; P: M/F = 26/24) were not significantly different between the L and P groups. The baseline pain intensity before PELD procedure was also not significantly different between the 2 groups, (L: 6.9 ± 1.8; P: 6.8 ± 1.7) (Table 1).
Table 1.
Demographic Characteristics
There was no difference of mean age, sex distribution, and the baseline pain intensity between 2 groups. L group: lidocaine 5% patch applied with active side down, P group: lidocaine 5% patch applied with inactive side down, NRS: numeric rating scale.
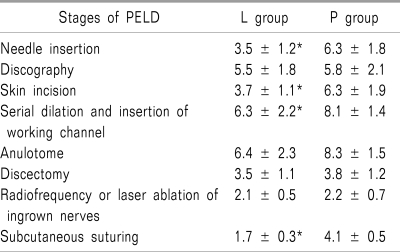
The mean NRS score at the stage of needle insertion, skin incision, serial dilation and insertion of working channel, and subcutaneous suturing was significantly lower in the L group in the P group (Table 2).
Table 2.
The mean Numeric Rating Scale (NRS) Scores During Percutaneous Endoscopic Lumbar Discectomy (PELD) at the L4-L5
L group: lidocaine 5% patch applied with active side down, P group: lidocaine 5% patch applied with inactive side down. *P < 0.05, The mean NRS scores at the stage of needle insertion, skin incision, serial dilation and insertion of working channel, and subcutaneous suturing were significantly lower in the L group than in P group.
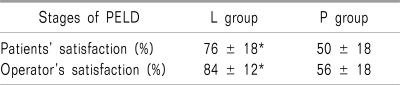
The postoperative patient and operator satisfaction scores were significantly higher in L group (76 ± 18% and 84 ± 12% respectively) than in the P group (50 ± 18% and 56 ± 18% respectively) (Table 3).
Table 3.
Postoperative Patients' and Operator's Satisfaction
Five-grade sale of rating patient and operator postoperative satisfaction: excellent (-100%), very good (-80%), good (-60%), fair (-40%), and poor (-20%). L group: lidocaine 5% patch applied with active side down, P group: lidocaine 5% patch applied with inactive side down. *P < 0.05, Postoperative patients' and operator's satisfaction scores were significantly higher in the L group than in the P group.
There were subtle adverse effects such as skin rashes in 2 cases and 1 case in the L and P groups, respectively.
DISCUSSION
PELD is known to be a representative method of MISS. The operators usually consider it MISS because it involves a small incision, low-degree damage to the normal tissue, the use of local anesthesia, an early ambulation immediately after surgery, and a short hospital stay. Moreover, patients who have undergone PELD also consider that they underwent MISS until the end of the operation. Most of these patients have suffered from severe radicular pain for a considerable period, and they require treatment to alleviate this intractable pain. Patients may have the same impression as the operators from because of tolerable pain experienced during the operation that PELD is truly MISS. Using local anesthesia for performing PELD has a great merit about potential nerve damage compared to general anesthesia. It can also minimize the risk of accidental extubation or displacement of endotracheal tube. However, if the pain during the operation is too difficult to endure, patients will not perceive PELD under local anesthesia MISS.
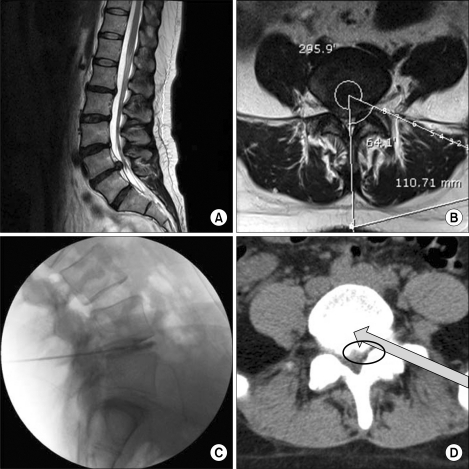
In this study, applying L5P with conventional analgesic methods gained both operator and patient satisfactions with subtle adverse effects after PELD and lower pain scores during PELD. A considerable pain relief was shown at the stages of needle insertion, skin incision, serial dilation and insertion of working channel, and subcutaneous suturing. These 4 stages are directly related to skin and subcutaneous tissue injuries. The needle and working channel is supposed to bridge the anatomic structures from the skin to the targeted anulus at the L4-L5 intervertebral disc space. The intervening structures in the following order are the latissimus dorsi muscle, external and internal oblique muscle, superficial thoracolumbar fascia, erector spinae muscle (lateral tract: iliocostalis lumborum muscle), deep thoracolumbar fascia, quadratus lumborum muscle, erector spinae muscle (lateral tract: intertransversarii mediales muscle), and psoas major muscle (Fig. 1) [7,8].
Fig. 1.
The anticipated passage of the needle and working channel while performing percutaneous endoscopic lumbar discectomy at the L4-L5. The anatomic structures from the skin to the targeted anulus at the L4-L5 intervertebral disc space are seen in the following order from the skin surface to the disc: (1) the latissimus dorsi muscle, (2) external and internal oblique muscle, (3) superficial thoracolumbar fascia, (4) erector spinae muscle (lateral tract: iliocostalis lumborum muscle), (5) deep thoracolumbar fascia, (6) quadratus lumborum muscle, (7) erector spinae muscle (lateral tract: intertransversarii mediales muscle), and (8) psoas major muscle. This is a case of a 37-year-old patient who underwent single-level PELD at the L4-L5. (A) Preoperative T2-weighted sagittal magnetic resonance image (MRI); the approaching angle and distance from the midline were measured for the proper placement of the needle and working channel before PELD (B); preoperative T2-weighted axial MRI; (C) intraoperative discogram, lateral view; and (D) postoperative computed tomography. Air shadows are seen in the passage of the working channel in the muscles (arrow) and in the anterior epidural space after the removal of herniated nucleus pulposus using right-angled forceps (circle).
However, pain was not alleviated at the stages of discography, anulotomy, discectomy, and radiofrequency or laser ablation despite the application of L5P; this evoked pain may have been possibly experienced as a result of burning anulus and its tight adhesion with the exiting nerve root and irritation of the ingrown nerves into the inner anulus and nucleus pulposus. However, the outcome according to the operator was better as no interferences occurred while determining pain concordance and provocation, measuring the intradiscal pressure, and determining the shape of the discogram during discography. In addition, it was easy for the operator to recognize whether the tip of the radiofrequency or laser was located too near to ablate the corda equina or the nerve root during radiofrequency or laser ablation for the ingrown nerves into the inner anulus and nucleus pulposus.
L5P is considered more effective in alleviating pain that is superficial than in alleviating pain that arises from deep somatic painful procedure. In cases of the percutaneous vertebroplasty or kyphoplasty, which are some other MISS procedures in clinical practice, the pain mainly originates deep from bone penetration of the needle and cement augmentation, and not superficially from the skin or subcutaneous tissue penetration of the needle. The longer the duration of the specific procedure and the depth of the passage through the superficial soft tissue during this procedure is, the more the pain that is experienced. Comparative studies taking into account the ratio of the depth and duration of the procedure in soft superficial tissue versus in deep somatic tissue will be required to compare the efficacy of L5P.
The most painful 2 stages during PELD in both groups were the serial dilation and insertion of working channel and the anulotomy stages. If the pain was too severe, and scored more than 6 in the NRS score, a small dose of propofol intravenously administered so that the patient can endure the remaining procedure including identification of the intervening the nerves. However, it is vital for the operator to recognize whether the exiting nerve or the traversing nerve has been intervened in a working channel or anulotome from the patients' response. If the nerve has been intervened, it is strongly recommended to observe the relation between the nerve and the burning anulus through the endoscope. The best anesthesia during PELD is one that can be administered under careful monitoring, leaving the patient conscious, but without any discomfort pain that can be misconceived by the patient s as intervening nerve.
L5P is composed of an adhesive material containing 5% lidocaine, which is applied to a non-woven polyester felt backing and covered with a polyethylene terephthalate (PET) film release liner. The size of the patch is 10 × 14 cm. Each adhesive patch contains 700 mg of lidocaine (50 mg/g adhesive) in an aqueous base. It also contains the following inactive ingredients: dihydroxyaluminum amino-acetate, disodium edetate, gelatin, glycerin, kaolin, methylparaben, polyacrylic acid, polyvinyl alcohol, propylene glycol, propylparaben, sodium carboxymethylcellulose, sodium polyacrylate, D-sorbitol, tartaric acid, and urea. The amount of lidocaine systemically absorbed from L5P is directly related to both the duration and the surface area of application. Lidocaine is metabolized rapidly by the liver into a number of metabolites, including monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have pharmacologic activities similar to, but less potent than that of lidocaine. The blood concentrations of these metabolites are negligible after L5P application. After intravenous administration of lidocaine, the serum MEGX and GX concentrations range from 11% to 36% and from 5% to 11% of the original lidocaine concentrations, respectively. Lidocaine and its metabolites are excreted via the kidneys. Less than 10% of lidocaine is excreted without being metabolized. The half-life of lidocaine elimination from plasma following intravenous administration is 81 to 149 minutes (mean 107 ± 22, n = 15). The systemic clearance is 0.33 to 0.90 L/min [9].
L5P is considered more effective in neuropathic pain presented as allodynia rather than somatic pain [10]. Probably, the target symptom is tactile allodynia on basis of the experience of L5P application in patients with postherpetic neuralgia. Such touch and pressure sensations are conducted in large myelinated nerve fibers, such as Aβ fibers. It takes longer time to experience the loss of these sensations than pain and warm temperature, which are charged in small unmyelinated never C-fibers, after applying L5P or local infiltration of lidocaine. The 8% lidocaine pump spray produces cutaneous topical anesthesia after 30 minutes, which is faster than L5P in the current perception threshold [11]. In cases of L5P was not applied prior to PELD, the alternate route might be to use the spray for accelerating the analgesic effect after patient's arrival into the operating room.
The biggest limitation of this study was the unavailability of a vehicle patch without lidocaine (placebo patch) similar to the actual patch itself. The tactile texture of the inactive side of the patch is much more different from the lidocaine-active side. This limitation may have confounded the results. However, none of patients had ever applied an L5P before this operation, so none of them were able to identify which side is active or inactive when the patch was applied. The other limitation was the difference in pain intensity according to the degree and direction of herniation of the nucleus pulposus among the eligible patients; however, each patient has his/her own pain threshold that would be different to another. The baseline pain intensity of the patients before the operation did not significantly differ between the 2 groups or appear to affect the results when assessing pain intensity categorized into different painful stages. In this study, the PELD patients were ones who were experiencing refractory pain following repeated epidural steroid injection, motor deficit, or cauda equina syndrome. It would be more helpful if a future study examines the efficacy of L5P application after considering the cause of PELD as well, even if the causes would overlap in some of the patient cases. The other limitation of using the L5P in clinical application is insurance coverage. The use of L5P is only permitted for the postherpetic neuralgia. However, the cost of applying 1 L5P is only 1 US dollar; 1 patch is enough to cover the anticipated passage of the working channel. L5P application before PELD appears to be a cost-effective analgesic method from the results of pain amelioration during PELD from the perspective of both patients and operator as assessed by the satisfaction score they gave after PELD in this study.
The postoperative pain will affect the way patients will view and rate their satisfaction with PELD. However, because in most cases in this study, the patients suffered from radicular pain originating from herniated nucleus pulposus, their perception of pain was lowered postoperatively. Surgical injury causes flare formation around the wound, and results in 2 different types of hyperalgesia. Primary hyperalgesia occurs when both thermal and mechanical stimuli are applied to damaged tissue close to the site of injury. The underlying mechanism for this pain involves peripheral sensitization of primary afferent nociceptors by locally released algogenic mediators. In contrast, ischemia may play an important role in postoperative pain behavior and hyperalgesia and local acidosis parallels them. Low pH activates several ion channels susceptible pain transduction, i.e., acid-sensing ion channels, vanilloid receptors, purinergic receptors, and potassium channels. Surgical injury also induces hypersensitivity in adjacent tissues, referred to as secondary hyperalgesia, and is observed only when mechanical stimuli are applied to uninjured tissues surrounding the wound. Secondary mechanical hyperalgesia is considered to be a consequence of central sensitization and results from enhanced response of the dorsal horn neurons to peripheral inputs; with magnitude and duration of pain corresponding to the degree of tissue injury [12]. The pain from a small incision of less than 1 cm and soft tissue injury are too small to be compared with pain experienced from compressed dorsal root ganglion and cauda equina in PELD. The dysesthesia may persist in some cases, but it will have originated only from a detached site in the dorsal root ganglion from the herniated nucleus pulposus, and it can be treated with neuropathic pain medications such as anticonvulsants administration for 3 months after PELD.
There were subtle adverse effects of L5P application, such as skin erythema in 2 cases and 1 case in the L and P groups, respectively. There were no other potential allergic or anaphylactic, and dose-related systemic reactions such as excitatory central nerve system and cardiovascular manifestation reported in this study. The manufacture recommends applying up to 3 patches, only once for up to 12 hours within a 24-hour period; only on intact skin due to anticipated variability in absorption.
In conclusion, L5P application 1 hour before PELD produced considerable relief from superficial somatic pain during the needle insertion, skin incision, serial dilation and insertion of working channel, and subcutaneous suturing. The use of patch also resulted in a higher postoperative satisfaction of the patients and operator. Providing additional analgesia to patients undergoing PELD under local anesthesia helped them to overcome subtle adverse effect as well as to recognize PELD procedure as true MISS. From an operator's perspective, it helped the operator recognize potential nerve damage during the procedure in cooperative patients.
ACKNOWLEDGEMENTS
This study was supported by The Medical Research Center, Pusan National University Hospital and Yangsan Hospital in 2008.
References
- 1.Rowbotham MC, Davies PS, Verkempinck C, Galer BS. Lidocaine patch: double-blind controlled study of a new treatment method for post-herpetic neuralgia. Pain. 1996;65:39–44. doi: 10.1016/0304-3959(95)00146-8. [DOI] [PubMed] [Google Scholar]
- 2.Moon JY, Choi JB, Lee PB, Son HM, Nam FS, Kim YC, et al. An open-label trial of the 5% lidocaine patches for the treatment of chronic pain. Korean J Pain. 2009;22:216–223. [Google Scholar]
- 3.Curry SE, Finkel JC. Use of the Synera patch for local anesthesia before vascular access procedures: a randomized, double-blind, placebo-controlled study. Pain Med. 2007;8:497–502. doi: 10.1111/j.1526-4637.2006.00204.x. [DOI] [PubMed] [Google Scholar]
- 4.Schecter AK, Pariser DM, Pariser RJ, Ling MR, Stewart D, Sadick NS. Randomized, double-blind, placebo-controlled study evaluating the lidocaine/tetracaine patch for induction of local anesthesia prior to minor dermatologic procedures in geriatric patients. Dermatol Surg. 2005;31:287–291. doi: 10.1111/j.1524-4725.2005.31075. [DOI] [PubMed] [Google Scholar]
- 5.Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J. 2004;4:564–573. doi: 10.1016/j.spinee.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 6.Kim KH. Posterolateral percutaneous endoscopic lumbar discectomy. Korean J Pain. 2004;17(Suppl):5–12. [Google Scholar]
- 7.Moeller TB, Reif E. Pocket atlas of sectional anatomy. Volume 3 spine, extremities, joints. Stuttgart: Thieme; 2007. pp. 310–311. [Google Scholar]
- 8.Ross LM, Lamperti ED. Atlas of anatomy. General anatomy and musculoskeletal system. Stuttgart: Thieme; 2006. pp. 138–141. [Google Scholar]
- 9.Freeman R. The treatment of neuropathic pain. CNS Spectr. 2005;10:698–706. doi: 10.1017/s1092852900019696. [DOI] [PubMed] [Google Scholar]
- 10.Kern KU, Kohl M, Kiefer RT. Lidocaine patch for therapy of neuropathic and non-neuropathic pain. A clinical case series of 87 patients. Nervenarzt. 2010;81:1490–1497. doi: 10.1007/s00115-010-3060-2. [DOI] [PubMed] [Google Scholar]
- 11.Kanai A, Suzuki A, Okamoto H. Comparison of cutaneous anesthetic effect of 8% lidocaine spray with lidocaine patch using current perception threshold test. Pain Med. 2010;11:472–475. doi: 10.1111/j.1526-4637.2009.00790.x. [DOI] [PubMed] [Google Scholar]
- 12.Lavand'homme P. Perioperative pain. Curr Opin Anaesthesiol. 2006;19:556–561. doi: 10.1097/01.aco.0000245284.53152.1f. [DOI] [PubMed] [Google Scholar]