Abstract
Background
Premature closure of the proximal femoral growth plate results in coxa brevis, which usually is associated with insufficiency of the hip abductors. Distal and lateral transfer of the greater trochanter sometimes is recommended to correct this problem. Most of what is known arises from studies of children and adolescents.
Questions/purposes
We asked whether this procedure in adults with coxa brevis would eliminate hip abductor insufficiency and would improve their hip function based on the Harris hip score (HHS).
Patients and Methods
We prospectively followed 11 patients, aged 19 to 55 years (mean, 40 years) who had distal and lateral trochanteric transfer. All patients had pain and a positive Trendelenburg test before surgery. This test was performed at the latest followup by three observers and the interobserver reliability was determined by the kappa coefficient. The HHS was obtained before surgery and at the latest followup. The minimum followup was 25 months (mean, 52 months; range, 25–77 months).
Results
Insufficiency of the hip abductors was eliminated in seven (according to two observers) and eight (according to one observer) of the 11 patients after surgery; the kappa coefficient ranged from 0.79 to 1.0. The mean HHS improved from 64 points preoperatively to 76 points at the final followup. The two patients with preexisting severe osteoarthritis of the hip had the worst final scores and persisted with a positive Trendelenburg test at the final followup.
Conclusions
Distal and lateral transfer of the greater trochanter can eliminate insufficiency of the hip abductors and improve joint function in adult patients with coxa brevis and we believe should be considered for patients without severe osteoarthritis of the hip.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Partial or complete growth arrest at the proximal femoral physis combined with normal development of the greater trochanter results in femoral neck shortening and elevation of the proximal tip of the greater trochanter relative to the center of rotation of the femoral head. This deformity is termed coxa brevis [5, 25], high-standing greater trochanter [26] or relative trochanteric overgrowth [6, 13, 23], and occurs as a sequela of diseases such as developmental dysplasia of the hip, slipped capital femoral epiphysis, infections of the hip, and Legg-Calvé-Perthes disease. In this situation the hip abductors habitually become functionally insufficient owing to the reduction of their resting length and lever arm [20]. Furthermore, the resultant vector of the forces acting on the hip becomes more vertical, increasing the pressure over a reduced area of the joint and causing chondral damage [1, 17, 30]. In extreme cases, this deformity also may limit hip abduction and produce painful impingement between the greater trochanter and the ilium [16, 30].
Several techniques have been suggested for treating coxa brevis, including epiphysiodesis of the greater trochanter [23], distal and lateral transfer of the greater trochanter [12], and femoral neck lengthening osteotomy [11, 19]. These techniques essentially have the same goals: correct the biomechanical abnormalities of the hip and its resulting clinical effects, such as gait disturbance (gluteus medius lurch), pelvic instability (Trendelenburg sign), and fatigue pain on walking. Some studies [4–7, 12, 15, 16, 21–23, 27] have concluded that distal and lateral transfer of the greater trochanter is an effective technique to improve gait and restore abductor power in patients with coxa brevis. These studies, however, mainly included children and adolescents.
Thus, we asked whether this procedure used for adult patients with coxa brevis would: (1) eliminate insufficiency of the hip abductors; and (2) improve hip function based on the HHS [10].
Patients and Methods
We prospectively followed all 11 adult patients (eight women, three men) with coxa brevis, aged 19 to 55 years (mean, 40 years) who underwent distal and lateral transfer of the greater trochanter between 2003 and 2007. The surgery was indicated in patients with abductor insufficiency, detected by a positive Trendelenburg test [9], associated with any degree of pain in the hip. The surgery was contraindicated in patients older than 60 years, in whom fixation of the osteotomized trochanter can be problematic. The deformity was caused by Legg-Calvé-Perthes disease in seven patients, developmental dysplasia of the hip in two, slipped capital femoral epiphysis in one, and osteomyelitis of the proximal femur in one. The affected side was shorter when compared with the unaffected side in all 11 patients; the shortening ranged from 0.8 to 2.1 cm (mean, 1.2 cm), and patients were given either a heel lift or a full length sole lift before the surgery to compensate for the discrepancy. No patients were lost to followup. The minimum followup was 25 months (mean, 52 months; range, 25–77 months). We recalled all patients specifically for this study. Approval of our hospital’s Institutional Review Board was obtained and all patients gave written informed consent before surgery.
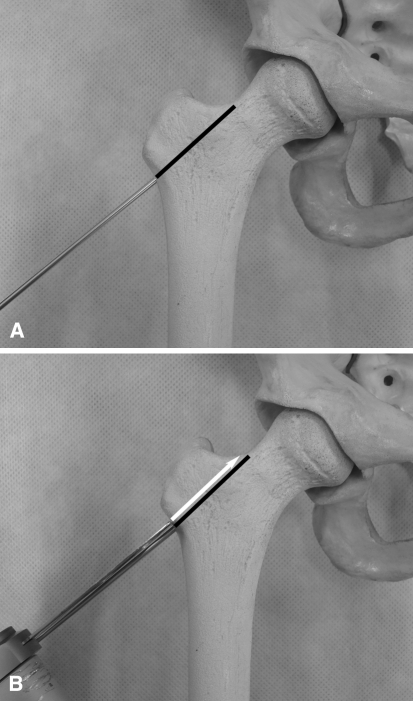
All operations were performed by one surgeon (FLG) using the same technique. A 10-cm incision was made beginning at the level of the proximal tip of the greater trochanter and extending distally along the proximal femoral shaft. The fascia lata was divided, and the upper portion of the vastus lateralis released from its proximal attachment at the base of the greater trochanter. Under image intensifier control, a 2-mm guide wire was introduced laterally at the base of the greater trochanter, forming an angle approximately 45° with the femoral diaphysis, and then driven along a line continuous with the superior border of the femoral neck; the osteotomy is performed with an oscillating saw following the guide wire immediately proximal to it (Fig. 1). The abductor muscles attached to the osteotomized greater trochanter were released from the joint capsule using scissors. The greater trochanter was transferred and provisionally fixed with two or three K-wires to the lateral femoral cortex with the proximal tip of the greater trochanter approximately level to the center of rotation of the femoral head; it was important that the new attachment site at the lateral femoral cortex was bleeding, but no wedge of bone was removed from this area, as this could have prevented or diminished lateral displacement of the greater trochanter. Once an adequate position was confirmed with the aid of an image intensifier, the greater trochanter is definitely fixed with two 6.5-mm cancellous screws and washers; in small patients two 4.5-mm malleolar screws were used. The wound was closed appropriately in layers.
Fig. 1A–B.
(A) The guide wire is positioned at the base of the greater trochanter and then driven to the superior border of the femoral neck, as marked with the black line; and (B) the osteotomy is performed with an oscillating saw following the guide wire immediately proximal to it, as indicated by the white arrow.
The rehabilitation protocol included early mobilization and toe-touch weightbearing with a walker for 6 weeks, followed by 50% weightbearing for another 6 weeks. Subsequently, under radiographic confirmation of bone healing, the walker was discontinued and patients were allowed to perform full weightbearing and active abduction exercises. Routine followups after surgery were scheduled at 6 weeks; 3, 6 and 12 months; and yearly thereafter. At each visit, the patients’ activities of daily living, pain, gait, deformity, and ROM of the hip were assessed according to the HHS, and AP radiographs of the pelvis were obtained with the hips in neutral position and source-to-film distance of 1 m.
The clinical data analyzed in this study were obtained preoperatively and at the latest followup by one of us (LPC, observer A) not participating in the treatment. The clinical data included the HHS, which is a validated measurement tool of the hip function [24, 32], and assessment of the competence of the hip abductors using the Trendelenburg test [9]. This test also was performed at the latest followup by two independent orthopaedic consultants (observers B [LGGM] and C [ATS]) not participating in the treatment, one at a time and blinded to each other’s results. The kappa coefficient [2] was calculated using the SAS/STAT® version 9.0 software (SAS Institute Inc, Cary, NC, USA) for gauging the interobserver reliability.
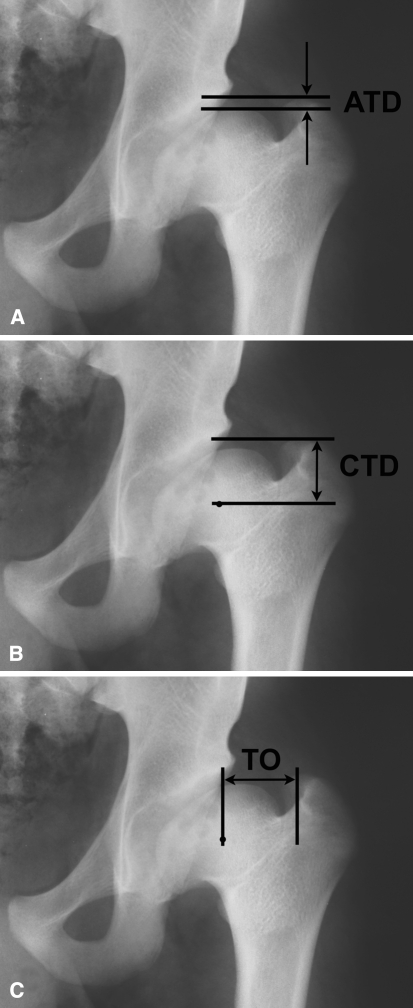
Additionally, one of us not participating in the treatment (LPC) evaluated all AP pelvic radiographs obtained preoperatively and at the latest followup. The measured parameters, all of which have high interobserver and intraobserver reliability [18, 31], included (Fig. 2): articulotrochanteric distance (ATD), defined as the vertical distance between two horizontal parallel lines, one passing through the tip of the greater trochanter and the other through the most cephalic portion of the femoral head; centrotrochanteric distance (CTD), defined as the vertical distance between two horizontal parallel lines, one passing through the tip of the greater trochanter and the other through the center of rotation of the femoral head; and trochanteric offset (TO), defined as the horizontal distance between two vertical parallel lines, one passing through the tip of the greater trochanter and the other through the center of rotation of the femoral head; the values of ATD and CTD are defined as negative when the tip of the greater trochanter is above the most cephalic portion of the femoral head and above the center of rotation of the femoral head, respectively, and defined as positive when the tip of the greater trochanter is below these same landmarks. Using the method described by Tönnis [29], the severity of osteoarthritis was classified on the basis of the same radiographs as follows: Grade 0 = no radiographic changes; Grade 1 = increased sclerosis of femoral head and acetabulum, slight decrease in the height of the cartilage, and slight osteophytes; Grade 2 = small cysts in the femoral head or acetabulum, marked decrease in the height of cartilage, and slight deviation from the round shape of the femoral head; and Grade 3 = large cysts in the femoral head and acetabulum, severe decrease in cartilage up to complete absence of the joint cleft, severe deviation of the round form of the femoral head, and avascular necrosis.
Fig. 2A–C.
The radiographic parameters, (A) articulotrochanteric distance (ATD), (B) centrotrochanteric distance (CTD) and (C) trochanteric offset (TO) are shown; the values of ATD and CTD are defined as negative when the tip of the greater trochanter is above the most cephalic portion of the femoral head and above the center of rotation of the femoral head, respectively.
Results
The insufficiency of the abductor musculature, as determined by the Trendelenburg test, was eliminated in seven of the 11 patients according to observers A and B and in eight of the 11 patients according to observer C (Table 1). Agreement between observers A and C and between observers B and C had a kappa coefficient of 0.79; agreement between observers A and B had a kappa coefficient of 1. Independently of the observer, two of the patients who continued to have abductor insufficiency were those with severe osteoarthritis of the hip (Tönnis Grade 3) before surgery.
Table 1.
Clinical details of the patients
| Patient | Age at operation (years) | Etiology | Length of followup (months) | Trendelenburg test | Harris hip score | ||
|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative (observer) | Preoperative | Postoperative | ||||
| 1 | 50 | LCPD | 77 | Positive | Positive (A, B, C) | 54 | 34 |
| 2 | 41 | LCPD | 74 | Positive | Positive (A, B); Negative (C) | 85 | 90 |
| 3 | 47 | LCPD | 68 | Positive | Negative (A, B, C) | 50 | 78 |
| 4 | 44 | DDH | 63 | Positive | Negative (A, B, C) | 54 | 77 |
| 5 | 55 | LCPD | 61 | Positive | Positive (A, B, C) | 49 | 35 |
| 6 | 49 | SCFE | 54 | Positive | Negative (A, B, C) | 70 | 87 |
| 7 | 36 | DDH | 52 | Positive | Negative (A, B, C) | 90 | 100 |
| 8 | 35 | LCPD | 41 | Positive | Negative (A, B, C) | 65 | 59 |
| 9 | 19 | LCPD | 33 | Positive | Negative (A, B, C) | 76 | 100 |
| 10 | 38 | OM | 28 | Positive | Positive (A, B, C) | 39 | 78 |
| 11 | 30 | LCPD | 25 | Positive | Negative (A, B, C) | 75 | 97 |
| Mean | 40 | 52 | 64 | 76 | |||
LCPD = Legg-Calvé-Perthes disease; DDH = developmental dysplasia of the hip; SCFE = slipped capital femoral epiphysis; OM = osteomyelitis of the proximal femur; Observer A = one of the authors, not participating in the treatment (LPC); Observer B = not an author, not participating in the treatment; Observer C = not an author, not participating in the treatment.
Overall, the mean HHS improved from 64 points (range, 39–90) to 76 points (range, 34–100) after surgery. Eight of the 11 patients had improvement of their HHS, with four of them achieving 90 or more points. Three patients had a decrease in their HHS, obtaining values between 34 and 59 points (Table 1). According to the HHS questionnaire, pain was reduced or eliminated in seven of the 11 patients, remained the same in two patients, one of whom graded it as slight and the other as moderate, and increased in two other patients, both with severe osteoarthritis of the hip (Tönnis Grade 3). No changes in hip ROM were detected after surgery. Limp was reduced or eliminated in nine of the 11 patients. In one patient limp worsened from moderate to severe and another patient continued to have a severe limp; these two patients had preexisting Tönnis Grade 3 osteoarthritis.
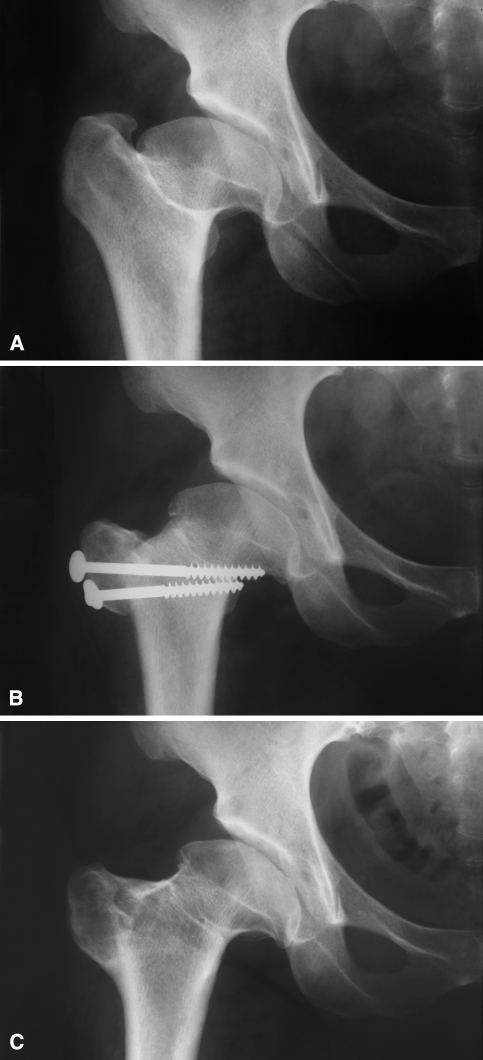
The radiographic assessment showed that all patients had improved ATD, CTD, and TO (Fig. 3), but a neutral or positive CTD was achieved in only three of the 11 patients. The majority of patients (six of 11) had a negative CTD between 1 and 5 mm (Table 2). The mean distal and lateral trochanteric advancement was 19 mm (range, 5–35 mm) and 13 mm (range, 6–20 mm), respectively. During the followup, no changes in the severity of osteoarthritis were observed (Table 2), and none of the patients showed radiographic evidence of osteonecrosis of the femoral head.
Fig. 3A–C.
These radiographs illustrate the case of a 47 year-old woman with coxa brevis. (A) The articulotrochanteric distance and centrotrochanteric distance are negative on the preoperative radiograph, and a small trochanteric offset can be seen. (B) A radiograph taken 1 month after distal and lateral transfer of the greater trochanter shows marked improvement of the cited parameters. (C) A radiograph taken 4 years postoperatively shows solid bone union and maintenance of the joint space. The screws were removed 1.5 years after the transfer owing to persistent trochanteric bursitis.
Table 2.
Radiologic assessment
| Patient | ATD (mm) | CTD (mm) | TO (mm) | Tönnis grade | ||||
|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | |
| 1 | 6 | 25 | −13 | 6 | 25 | 32 | 3 | 3 |
| 2 | 3 | 13 | −12 | −2 | 44 | 57 | 1 | 1 |
| 3 | −4 | 18 | −24 | −2 | 31 | 50 | 1 | 1 |
| 4 | 4 | 9 | −10 | −5 | 30 | 36 | 2 | 2 |
| 5 | −10 | 17 | −26 | 1 | 21 | 35 | 3 | 3 |
| 6 | −4 | 14 | −23 | −5 | 34 | 40 | 1 | 1 |
| 7 | −15 | 12 | −34 | −7 | 27 | 37 | 0 | 0 |
| 8 | −18 | 17 | −40 | −5 | 32 | 52 | 1 | 1 |
| 9 | −4 | 23 | −27 | 0 | 30 | 48 | 0 | 0 |
| 10 | 5 | 10 | −13 | −8 | 34 | 44 | 2 | 2 |
| 11 | −6 | 10 | −20 | −4 | 27 | 43 | 0 | 0 |
| Mean | −4 | 15 | −22 | −3 | 30 | 43 | ||
ATD = articulotrochanteric distance; CTD = centrotrochanteric distance; TO = trochanteric offset.
No patients had a surgical site infection, and the greater trochanter healed in all patients within 12 weeks after surgery. Two patients had trochanteric bursitis and were treated successfully by hardware removal; there were no other complaints related to the transferred trochanter.
Discussion
The work of Pauwels [20] enabled better understanding of the biomechanics of the hip. Since then, effort has been applied to the development of surgical techniques to restore adequate function in patients with coxa brevis, promoting more physiologic joint contact forces, reducing pain, increasing the efficiency of the abductors, and possibly delaying the occurrence of osteoarthritis [1, 17, 30]. Treatment by distal and lateral advancement of the trochanter was first described by Jani [12], and many subsequent reports have confirmed its value in improving gait and abductor function [4–7, 12, 15, 16, 21–23, 27]. However, these studies mainly included children and adolescents. This fact motivated us to investigate whether this technique is also effective in adults to eliminate insufficiency of the hip abductors and improve hip function.
Our study has some limitations. First is the small number of subjects. Ideally, a larger number of patients would allow for a more detailed analysis, with the possibility of matched subgroups compared by etiology and age. However, having an adult patient with coxa brevis that was not corrected during childhood or adolescence is unusual, and we believe it would be difficult to have a much larger group operated on at one institution. Second is the relatively short followup, which prevented us from reaching any conclusion regarding the theoretical protective effect of this procedure on the development and progression of hip osteoarthritis. Finally, we had no comparison with other reconstruction techniques.
Elimination of insufficiency of the hip abductors in our series occurred in seven or eight of the 11 patients, depending on the observer, and this finding is within the wide range reported in the literature (Table 3). This wide range is probably attributable to the variability of indications for surgery, etiology of the deformity, postoperative rehabilitation protocols, and length of followup in the different studies; therefore, comparisons should be regarded with some reservation. The standardized method we used to evaluate competence of the hip abductors (ie, the Trendelenburg test) proved to be reliable, with high kappa values confirming findings in a previous report [28].
Table 3.
Comparison of data from current and previous studies
| Study | Number of hips | Mean age (range) in years | Mean followup (range) in months | Elimination of Trendelenburg sign | Gait improvement | Mean hip score (preoperative, postoperative) |
|---|---|---|---|---|---|---|
| Jani [12] | 44 | NA (6–25) | NA | 29 of 44 hips | All patients | NA |
| Tauber et al. [27] | 9 | 13 (4–25) | 39 (3–72) | 8 of 9 hips | All patients | NA |
| Fernbach et al. [6] | 33 | NA (8–20) | NA (2–21) | 25 of 30 hips | NA | NA |
| Lloyd-Roberts et al. [15] | 17 | 12 (9–17) | 48 (24–72) | 14 of 17 hips | NA | NA |
| Doudoulakis [4] | 30 | 10 (6–13) | 72 (36–96) | 20 of 24 hips | NA | NA |
| Macnicol and Makris [16] | 27 | 14 (8–39) | 96 (24–264) | 20 of 27 hips | All patients | NA |
| Porat et al. [21] | 15 | 12 (11–17) | 60 (33–84) | 15 of 15 hips | All patients | NA |
| Pucher et al. [22] | 55 | 13 (7–16) | 105 (20–318) | 30 of 52 hips | 30 of 48 patients | NA |
| Garrido et al. [7] | 11 | NA (4–13) | 42 (12–96) | 7 of 9 hips | All patients | NA |
| Eilert et al. [5] | 28 | 15 (7–36) | 40 (6–252) | 22 of 26 hips | 26 of 28 patients | NA |
| Schneidmueller et al. [23] | 26 | 13 (6–17) | 120 (12–204) | 8 of 16 hips | NA | MHS (14, 17) |
| Joo et al. [13] | 15 | 16 (13–26) | 42 (28–54) | 3 of 15 hips | NA | IHS (85, 89) |
| Current study | 11 | 40 (19–55) | 52 (25–77) | 7 or 8* of 11 hips | 9 of 11 patients | HHS (64, 76) |
NA = not available; MHS = Merle d’Aubigné-Postel hip score; IHS = Iowa hip score; HHS = Harris hip score.
* elimination of the Trendelenburg sign occurred in seven patients according to two observers, and in eight patients according to a third observer.
Improvement of hip function, based on the values of the HHS, occurred in eight of our 11 patients; many of the previous studies [4–7, 12, 15, 16, 21, 22, 27] did not use a validated tool, such as a hip score, to objectively measure this variable, describing it only in terms of improvement of gait. Although this last parameter is part of the frequently used hip scores [3, 10, 14], it is highly subjective and thus we consider it should not be used alone as the only parameter to describe hip function. Some studies (Table 3) have shown improvement of hip function in the majority of patients treated by distal and lateral transfer of the greater trochanter, either based on a validated hip score or only on gait improvement.
Lateral displacement of the greater trochanter has been described as the most important component of the trochanteric transfer [17, 26, 30], as distal displacement alone does not increase the lever arm of the abductors. Further, distal transfer alone changes the resultant vector of the forces acting on the hip to a more vertical position, increasing the pressure over a reduced area of the joint and possibly accelerating the development of osteoarthritis [17, 30]. Such an effect was reported in one study [8]. In contrast, other authors [15, 16, 27] reported improvement of gait and pain reduction with distal transfer alone. The relative importance of each of these individual components of the distal and lateral transfer of the greater trochanter has yet to be determined. Additionally, as reported by others [6, 7], we found that the degree of clinical improvement did not parallel the distance the trochanter was advanced; a patient with only a few millimeters of distal and lateral displacement showed improvement in the HHS and a negative Trendelenburg sign after surgery, whereas other patients with several millimeters of trochanteric displacement had a decrease in the HHS and continued insufficiency of the hip abductors.
Not surprisingly, patients with preexisting severe osteoarthritis had the worst hip scores at the latest followup. If these patients were excluded from the study, improvement of the HHS would have been achieved by eight of nine instead of eight of eleven patients, and the mean HHS after surgery would improve to 85 points instead of 76 points; likewise, insufficiency of the hip abductors would be eliminated in seven (according to two observers) or eight (according to one observer) of nine patients instead of seven or eight of 11 patients and limp would be eliminated or reduced in all patients (nine of nine) instead of nine of 11 patients. Such findings are in accordance with previous reports [5, 16, 22], and we now consider that severe hip osteoarthritis may constitute a contraindication to distal and lateral transfer of the greater trochanter.
Although the number of patients treated is limited and the followup is short, distal and lateral transfer of the greater trochanter can eliminate insufficiency of the hip abductors and improve hip function in adult patients with coxa brevis, as has been observed in children and adolescents. Based on our findings, this procedure should be considered for patients without severe osteoarthritis of the hip.
Acknowledgments
We thank Luis Gustavo G. Martins and Arthur T. Sugo (observers B and C) for their independent evaluations of the patients.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, all investigations were conducted in conformity with ethical principles of research, and informed consent for participation in the study was obtained.
References
- 1.Bombelli R. Osteotomies. In: Structure and Function in Normal and Abnormal Hips. Ed 3. New York, NY: Springer; 1993:119–167.
- 2.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. doi: 10.1177/001316446002000104. [DOI] [Google Scholar]
- 3.d’Aubigné RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 4.Doudoulakis JK. Trochanteric advancement for premature arrest of the femoral-head growth plate: 6-year review of 30 hips. Acta Orthop Scand. 1991;62:92–94. doi: 10.3109/17453679108999229. [DOI] [PubMed] [Google Scholar]
- 5.Eilert RE, Hill K, Bach J. Greater trochanteric transfer for the treatment of coxa brevis. Clin Orthop Relat Res. 2005;434:92–101. doi: 10.1097/01.blo.0000163474.74168.6f. [DOI] [PubMed] [Google Scholar]
- 6.Fernbach SK, Poznanski AK, Kelikian AS, Tachjdian MO, Marzano MJ. Greater trochanteric overgrowth: development and surgical correction. Radiology. 1985;154:661–664. doi: 10.1148/radiology.154.3.3969469. [DOI] [PubMed] [Google Scholar]
- 7.Garrido IM, Moltó FJ, Lluch DB. Distal transfer of the greater trochanter in acquired coxa vara: clinical and radiographic results. J Pediatr Orthop B. 2003;12:38–43. doi: 10.1097/00009957-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Givon U, Schindler A, Ganel A, Levy O. Distal transfer of the greater trochanter revisited: long-term follow-up of nine hips. J Pediatr Orthop. 1995;15:346–348. doi: 10.1097/01241398-199505000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Hardcastle P, Nade S. The significance of the Trendelenburg test. J Bone Joint Surg Br. 1985;67:741–746. doi: 10.1302/0301-620X.67B5.4055873. [DOI] [PubMed] [Google Scholar]
- 10.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 11.Hasler CC, Morscher EW. Femoral neck lengthening osteotomy after growth disturbance of the proximal femur. J Pediatr Orthop B. 1999;8:271–275. doi: 10.1097/00009957-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Jani L. [The development of the femur neck after transposition of the trochanter] [in German. Arch Orthop Unfallchir. 1969;66:127–132. doi: 10.1007/BF00417245. [DOI] [PubMed] [Google Scholar]
- 13.Joo SY, Lee KS, Koh IH, Park HW, Kim HW. Trochanteric advancement in patients with Legg-Calvé-Perthes disease does not improve pain or limp. Clin Orthop Relat Res. 2008;466:927–934. doi: 10.1007/s11999-008-0128-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larson CB. Rating scale for hip disabilities. Clin Orthop Relat Res. 1963;31:85–93. doi: 10.1097/00003086-196300310-00011. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd-Roberts GC, Wetherill MH, Fraser M. Trochanteric advancement for premature arrest of the femoral capital growth plate. J Bone Joint Surg Br. 1985;67:21–24. doi: 10.1302/0301-620X.67B1.3968136. [DOI] [PubMed] [Google Scholar]
- 16.Macnicol MF, Makris D. Distal transfer of the greater trochanter. J Bone Joint Surg Br. 1991;73:838–841. doi: 10.1302/0301-620X.73B5.1894678. [DOI] [PubMed] [Google Scholar]
- 17.Maquet PGJ. Lateral displacement of the greater trochanter. In: Biomechanics of the Hip: As Applied to Osteoarthritis and Related Conditions. New York, NY: Springer; 1985:134–149.
- 18.Omeroğlu H, Uçar DH, Tümer Y. [A new measurement method for the radiographic assessment of the proximal femur: the center-trochanter distance] [in Turkish] Acta Orthop Traumatol Turc. 2004;38:261–264. [PubMed] [Google Scholar]
- 19.Papavasiliou VA, Kirkos JM. Reconstruction of residual deformities of the hip: a new surgical option. Clin Orthop Relat Res. 1997;341:123–127. doi: 10.1097/00003086-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Pauwels F. Osteoarthritis. In: Biomechanics of the Normal and Diseased Hip: Theoretical Foundation, Technique and Results of Treatment: An Atlas. New York, NY: Springer; 1976:129–271.
- 21.Porat S, Robin GC, Howard CB. Cure of the limp in children with congenital dislocation of the hip and ischaemic necrosis: fifteen cases treated by trochanteric transfer and contralateral epiphysiodesis. J Bone Joint Surg Br. 1994;76:463–467. [PubMed] [Google Scholar]
- 22.Pucher A, Ruszkowski K, Bernardczyk K, Nowicki J. The value of distal greater trochanter transfer in the treatment of deformity of the proximal femur owing to avascular necrosis. J Pediatr Orthop. 2000;20:311–316. doi: 10.1097/00004694-200005000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Schneidmueller D, Carstens C, Thomsen M. Surgical treatment of overgrowth of the greater trochanter in children and adolescents. J Pediatr Orthop. 2006;26:486–490. doi: 10.1097/01.bpo.0000226281.01202.94. [DOI] [PubMed] [Google Scholar]
- 24.Söderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–197. doi: 10.1097/00003086-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 25.Stevens PM, Coleman SS. Coxa breva: its pathogenesis and a rationale for its management. J Pediatr Orthop. 1985;5:515–521. doi: 10.1097/01241398-198509000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Takata K, Maniwa S, Ochi M. Surgical treatment of high-standing greater trochanter. Arch Orthop Trauma Surg. 1999;119:461–463. doi: 10.1007/s004020050021. [DOI] [PubMed] [Google Scholar]
- 27.Tauber C, Ganel A, Horoszowski H, Farine I. Distal transfer of the greater trochanter in cox vara. Acta Orthop Scand. 1980;51:661–666. doi: 10.3109/17453678008990858. [DOI] [PubMed] [Google Scholar]
- 28.Tidstrand J, Horneij E. Inter-rater reliability of three standardized functional tests in patients with low back pain. BMC Musculoskelet Disord. 2009;10:58. doi: 10.1186/1471-2474-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]
- 30.Wagner H. Transplantation of the greater trochanter. In: Weil UH ed. Acetabular Dysplasia: Skeletal Dysplasias in Childhood. Berlin, Germany: Springer; 1978:99–102.
- 31.Wiig O, Terjesen T, Svenningsen S. Inter-observer reliability of radiographic classifications and measurements in the assessment of Perthes’ disease. Acta Orthop Scand. 2002;73:523–530. doi: 10.1080/000164702321022794. [DOI] [PubMed] [Google Scholar]
- 32.Wright JG, Young NL. A comparison of different indices of responsiveness. J Clin Epidemiol. 1997;50:239–246. doi: 10.1016/S0895-4356(96)00373-3. [DOI] [PubMed] [Google Scholar]