Abstract
Background
Distal femoral osteotomies (DFO) can be used to correct deformities around the knee. Although osteotomies can be fixed with either internal or external fixation techniques, the advantages of one over the other are unclear.
Questions/purposes
We asked whether (1) for both techniques, we could accurately correct the deformities based on our preoperative goals for mechanical axis deviation (MAD) and lateral distal femoral angle (LDFA), and (2) intraoperative times, (3) preoperative and postoperative knee ROM, and (4) complications differed.
Patients and Methods
We identified 26 patients (34 limbs) who underwent femoral osteotomies. We compared accuracy of correction (based on correction of the MAD and the LDFA), duration of surgery, preoperative and postoperative knee ROM, and complications. The minimum followup was 20 months (mean, 29 months; range, 20–40 months).
Results
We achieved the desired MAD within 10 mm of the goal in 18 of 21 limbs with the unilateral frame and in 12 of 13 limbs using fixator-assisted plating. Operative time for fixator-assisted plating was longer (122 ± 34 minutes) than when using a unilateral frame (94 ± 65 minutes). Preoperative and postoperative knee ROMs were similar for both techniques and there were no major complications.
Conclusions
We obtained accurate correction of deformities with both fixation techniques. Our experience suggests the method to be used should be left to the discretion of the surgeon and the needs and wishes of the patient after adequate explanation of the advantages and disadvantages.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoral osteotomies are used for correcting deformity and unloading joints with unicompartmental arthritis. Although TKA narrowed the indications for this once-common procedure, the femoral osteotomy remains a reasonable treatment for many patients with limb deformities [7, 25], and is broadly indicated when there is a deformity resulting in malalignment of the hip and lower extremity (nonunion/malunion of a fractured femur neck and rotational deformities, such a severe femoral anteversion or hip osteoarthritis).
Angular deformities of the distal femur can be acquired or developmental, and are seen in patients with fracture malunion [11, 27], adolescent-onset Blount disease [13, 33], metabolic disorders [14], osteoarthritis [5, 6, 17, 18], and idiopathic processes [14, 20]. Limb deformities affect axial alignment of the lower limbs and are especially important regarding mechanical forces sustained across articular cartilage during ambulation. Biomechanical studies [8, 19, 39] describe how varus and valgus alignment of the knee increase medial and lateral load respectively; this theoretically could facilitate the progression of osteoarthritis.
During the past 9 years, we used two minimally invasive approaches to DFOs. The DFO with a unilateral fixator is entirely percutaneous, and the DFO with fixator-assisted plating is a minimal incision technique that does not require patients to wear an external fixator. We are inclined to use external fixation in a patient with a thin thigh, when there is a perceived need to adjust position postoperatively, or when surgical time is an issue (combined femoral/tibial surgery), whereas we are inclined to use a locking plate in patients with large thighs or when there is a particular desire to avoid external fixation, like an adjacent knee replacement or a patient who is immunocompromised. However, the decision to use either technique is largely driven by patient choice.
We asked (1) if we could accurately correct the deformities based on our preoperative goals for the MAD and LDFA with both techniques, and whether (2) the intraoperative times, (3) preoperative and postoperative knee ROM, and (4) complications differed.
Patients and Methods
We retrospectively reviewed 26 patients (34 treated limbs) who underwent DFO for deformity correction at our institution between 2000 and 2009. We included all patients who underwent correction for femoral deformities with either fixator-assisted plating or a unilateral frame and who had at least 1 year followup, and we recorded their demographics (Table 1). We excluded patients younger than 18 years. There were no differences in age, preoperative joint orientation angles, proportion of varus/valgus deformities, or length of followup between the two groups of patients. Four patients had staged tibial osteotomies. The indications for surgery included distal femoral deformity with mild to moderate unicompartmental knee osteoarthritis. For patients with valgus deformity and a lateral MAD, the minimum deviation was 8 mm lateral. For patients with varus deformity with a medial MAD, the minimum deformity accepted was 18 mm medial. Contraindications included patients with advanced, tricompartmental osteoarthritis, and they were treated with total knee replacement. We were more likely to recommend external fixation if the patient’s skin quality was poor, if there was a surgical time constraint (eg, additional tibial deformity correction in the same surgery), if there was a need for additional limb lengthening or if the deformity was very large and acute correction was not considered to be safe. Taking this into account, we chose the fixation technique after discussion with each patient regarding their preference for internal or external fixation. The minimum followup was 20 months (mean, 29 months; range, 20–40 months). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
Table 1.
Patient demographics of the two groups
| Variables | Unilateral frame | Fixator-assisted plating |
|---|---|---|
| Age (years) | 37 ± 12 | 36 ± 16 |
| Men | 9 | 1 |
| Women | 7 | 9 |
| Valgus deformity (patients) | 15 | 12 |
| Varus deformity (patients) | 4 | 1 |
| Rotational deformity (patients) | 2 | 0 |
| Varus = preoperative LDFA greater than or equal to 90º (degrees) | 94.6 ± 5.6 | 95.6 ± 6.8 |
| Preoperative LDFA less than 90º (degrees) | 85.4 ± 5.6 | 84.4 ± 6.8 |
| Followup (months) | 30 ± 10 | 28 ± 6 |
LDFA = lateral distal femoral angle.
Preoperative evaluation included measurements of frontal plane deformity on a 51-inch erect-leg bipedal radiograph. The second author (RS) made all measurements on the radiographs; the MAD and joint orientation angles, including the LDFA, were measured using the methods described by Paley et al. [23, 26]. A previous study showed high interobserver reliability for long film measurements of joint orientation angles, such as the MAD and LDFA [12]. We defined the magnitude of the deformity by the MAD. Where neutral alignment was the goal, the distal mechanical axis line was drawn through the center of the knee. When overcorrection was the goal, the distal mechanical axis line was drawn to the desired location through the knee. Patients who intentionally had overcorrection either had unicompartmental arthritis or valgus deformity. The center of rotation and angulation (CORA) was located at the intersection of the proximal and distal mechanical axis lines. We planned the level of the proposed osteotomy, and determined the appropriate translation needed at the osteotomy site.
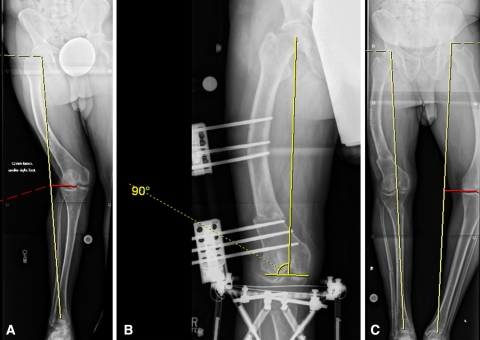
The senior authors (SRR, ATF) performed all surgeries using both techniques. The procedure for the unilateral frame (Fig. 1) was performed with the patient under combined spinal and epidural anesthesia with sedation. All half pins were inserted perpendicular to the anatomic axis of each segment of the femur to provide improved frame fit on the thigh. The femur was predrilled bicortically and 6-mm hydroxyapatite-coated half pins were inserted by hand through stab incisions. Using four half pins, the unilateral rail frame (EBI/ Biomet, Parsippany, NJ, USA) was mounted. This distal clamp of the frame had variable angulation, enabling the frame mount to match the deformity. The frame then was removed and angulation was adjusted to the neutral position. Using a percutaneous multiple drill hole and osteotome technique under fluoroscopic guidance, an osteotomy was performed through a 1-cm incision. An acute correction of the deformity was accomplished and translation as needed was introduced. A neutral frame was applied to stabilize the osteotomy. A few millimeters of compression was applied to ensure optimal contact and stability, and fluoroscopic images were taken to ensure there was no change in bone position after applying compression.
Fig. 1A–C.
The radiographs show the correction of deformity using a unilateral frame. The patient is a 48-year-old man with a marked windswept deformity. (A) A preoperative radiograph with a red line shows the MAD in the right limb. (B) This radiograph shows DFO and correction of the deformity with the unilateral frame. The yellow lines illustrate a normal LDFA of 90°. (C) A postoperative radiograph after removal of the unilateral frame is shown. The patient had a staged tibial osteotomy. MAD has been corrected to 0.
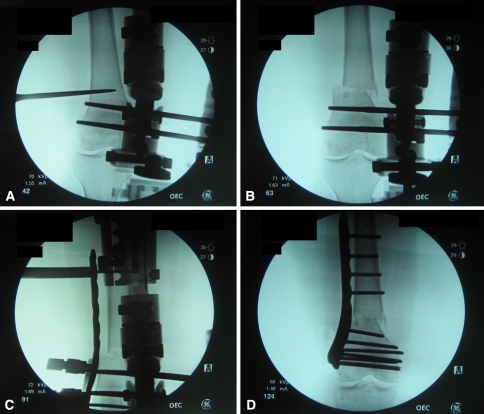
Fixator-assisted plating was performed with the patient under combined spinal and epidural anesthesia with sedation. The multiaxial correction (MAC) frame (EBI) was applied on the anterior and medial aspects of the femur to match the deformity. The CORA was localized on the patient’s thigh using c-arm fluoroscopy, and the hinge of the fixator was centered over it. The frame then was fixed using two to three proximal and two to three distal 6-mm half pins. The proximal pins were placed anteriorly and distal pins were introduced from the medial side, off an arch. Pin position was chosen so the lateral aspect of the femur was free for plating. The frame was detached and the osteotomy was performed using a percutaneous multiple drill hole and osteotome technique under fluoroscopic guidance, before the frame was reattached (Fig. 2A). Using the external fixator, the bone fragments were realigned, intraoperatively, to correct the deformity, and alignment was confirmed using fluoroscopy (Fig. 2B). A 5-cm lateral skin incision was made over the lateral distal femur. The fascia of the iliotibial band was incised, and a path was created along the distal femur and under the vastus lateralis to apply the locking pate. Internal fixation was performed using a Smith & Nephew (Memphis, TN, USA) locked distal femur plate. Proximal screws were placed percutaneously using the targeting device (Fig. 2C). The proximal plate typically was separated from the bone to accommodate the appropriate translation at the osteotomy site. After placing the first two proximal and distal locking screws through the plate, the frame and half pins were removed. The remaining plate screws then were inserted. The last intraoperative fluoroscopic images showed no change from the desired position (Fig. 2D).
Fig. 2A–D.
The fluoroscopy images show the operative technique for fixator-assisted plating. (A) This image shows application of temporary frame and osteotomy, followed by (B) correction of deformity, (C) application of the lateral locking plate, and (D) plate fixation and frame removal.
In both techniques, alignment was optimized by using a fixator that allowed precise measurement of angular correction. The position was checked with intraoperative radiographs using the Bovie cord alignment technique [16, 23, 34]; placing the cord from the center of the hip to the ankle center, and then checking the position of the cord at the knee.
Patients wearing a unilateral frame were allowed to weightbear as tolerated and had supervised physical therapy three times a week. Most patients in this group were walking without the need for two crutches at 6 to 8 weeks postoperatively. Patients requiring surgery to both limbs had staged procedures, with correction to the second limb 6 to 8 weeks after the first. Patients performed daily pin care with half-strength hydrogen peroxide solution and coverage of pin sites with a dry sterile gauze wrap. The frame was removed when the patient was able to weightbear without pain and when bridging bone on three of four cortices were seen on radiographs.
Patients who had fixator-assisted plating were kept at 30-lb partial weightbearing for 6 weeks, and then allowed to progress weightbearing at the surgeon’s discretion.
Postoperative followup was at 2 weeks, monthly for 6 months, and 1 and 2 years postoperatively. Patients also returned as needed between these scheduled visits. At each visit, we measured knee ROM and took radiographs to assess bone healing and check alignment. We determined osseous union by the presence of bridging bone on three of four cortices, as seen on the AP and lateral radiographs. For both treatment arms, the following information was obtained from the medical records: duration of surgery, complications, LDFA, MAD, and knee ROM. We also recorded the time patients wore the unilateral frame. We defined major complications as those warranting additional surgery, such as nonunion, refracture, hardware failure, deep pin infection requiring premature pin removal, infection requiring intravenous antibiotics, permanent knee stiffness, neurovascular injury, and stress fracture through a pin or screw hole. We defined a minor complication as a common postoperative problem, such as superficial skin infections and hardware-associated discomfort.
We divided each group into two subgroups, depending on whether the treatment goal was a MAD of 0 mm (center) or overcorrection. The outcomes included MAD data points medial and lateral to midline. To report this accurately, we averaged the medial and lateral data points separately. This generates separate medial and lateral values. We also recorded this as an absolute value. This way, the reader can understand the absolute distance between the postoperative MAD and the intended goal, and the direction of displacement.
We performed an independent sample t-test to calculate the absolute difference between the intended and achieved joint angle and the a priori intended correction (0 MAD for patients without arthritis, overcorrection for patients with arthritis). To assess the precision of the reported reliability estimates, we calculated 95% confidence intervals (95% CI). We performed all analyses using SPSS Version 14.0 (SPSS Inc, Chicago, IL, USA).
Results
We achieved an MAD within 10 mm of the goal in 18 of 21 limbs with the unilateral frame (Table 2) and in 12 of 13 limbs using fixator-assisted plating (Table 3). We achieved restoration of LDFA to within the normal range (87º–90º) in 14 of 21 limbs using the unilateral frame and nine of 13 limbs with fixator-assisted plating. In the unilateral frame group, we achieved an absolute average of 8.5-mm off-neutral alignment in patients with a varus deformity (Table 4); whereas in the fixator-assisted plating group, we achieved an average of 8-mm off-neutral alignment. One patient had varus correction with a fixator-assisted locking plate and a preoperative MAD of 64 mm medial. Postoperative MAD achieved was neutral (also had a staged tibial osteotomy). The results of patients who underwent intentional overcorrection were recorded (Table 5). We also were able to correct the LDFA based on the presenting deformity (Table 6). The mean LDFA was similar in the two treatment groups preoperatively (p = 0.7627) and postoperatively (p = 0.491).
Table 2.
Preoperative and postoperative measurements of patients treated using the unilateral frame
| Patient | Age at surgery (years) | Preoperative MAD (mm) | Postoperative MAD (mm) | Goal (mm) | Preoperative LDFA (degrees) | Postoperative LDFA (degrees) |
|---|---|---|---|---|---|---|
| 1 | 47 | 34 lateral | 8 lateral | 0 | 81 | 93 |
| 2 | 36 | 39 lateral | 20 medial | 15 medial | 80 | 90 |
| 3 (L) | 20 | 8 lateral | 7 medial | 10 medial | 83 | 88 |
| 3 (R) | 20 | 12 lateral | 13 medial | 10 medial | 84 | 89 |
| 4 (L) | 32 | 20 lateral | 14 medial | 10 medial | 83 | 90 |
| 4 (R) | 32 | 13 lateral | 10 medial | 10 medial | 86 | 92 |
| 5 | 56 | 20 lateral | 3 lateral | 0 | 84 | 93 |
| 6 | 54 | 21 lateral | 9 medial | 10 medial | 85 | 95 |
| 7 (L) | 31 | 16 lateral | 12 medial | 15 medial | 85 | 90 |
| 7 (R) | 31 | 38 lateral | 9 medial | 15 medial | 83 | 90 |
| 8 | 50 | 50 lateral | 16 lateral | 0 | 78 | 83 |
| 9 | 48 | 83 lateral | 4 medial | 0 | 86 | 94 |
| 10 | 30 | 24 lateral | 6 medial | 10 medial | 83 | 92 |
| 11 (R) | 33 | 47 lateral | 5 lateral | 0 | 81 | 90 |
| 11 (L) | 33 | 75 lateral | 19 lateral | 0 | 79 | 89 |
| 12 | 22 | 18 medial | 4 lateral | 0 | 92 | 87 |
| 13 | 35 | 100 medial | 19 medial | 0 | 96 | 89 |
| 14 | 44 | 47 medial | 5 lateral | 6 lateral | 96 | 84 |
| 15 | 21 | 65 medial | 4 medial | 0 | 98 | 89 |
| 16 (L) | 14 | 15 lateral | 0 | 0 | 84 | 89 |
| 16 (R) | 15 | 15 lateral | 7 lateral | 0 | 85 | 91 |
MAD = mechanical axis deviation; LDFA = lateral distal femoral angle.
Table 3.
Preoperative and postoperative measurements of patients treated with fixator-assisted plating
| Patient | Age at surgery (years) | Preoperative MAD (mm) | Postoperative MAD (mm) | Goal (mm) | Preoperative LDFA (degrees) | Postoperative LDFA (degrees) |
|---|---|---|---|---|---|---|
| 17 (L) | 21 | 20 lateral | 19 medial | 10 medial | 82 | 91 |
| 17 (R) | 21 | 9 lateral | 6 medial | 10 medial | 87 | 92 |
| 18 | 24 | 20 lateral | 11 medial | 10 medial | 83 | 91 |
| 19 | 45 | 21 lateral | 5 lateral | 0 | 84 | 91 |
| 20 (L) | 32 | 3 lateral | 10 medial | 10 medial | 87 | 91 |
| 20 (R) | 32 | 23 lateral | 5 medial | 10 medial | 85 | 90 |
| 21 | 48 | 54 lateral | 13 medial | 10 medial | 72 | 91 |
| 22 | 34 | 55 lateral | 2 lateral | 0 | 83 | 90 |
| 23 | 64 | 55 lateral | 35 lateral | 0 | 80 | 85 |
| 24 | 19 | 32 lateral | 0 | 0 | 85 | 91 |
| 25 | 60 | 64 medial | 0 | 0 | 103 | 95 |
| 26 (L) | 32 | Rotational deformity | 6 medial | 85 | 86 | |
| 26 (R) | 32 | 6 medial | 86 | 95 |
MAD = mechanical axis deviation; LDFA = lateral distal femoral angle.
Table 4.
Preoperative versus postoperative MAD (correction to neutral)
| Deformity/number of patients | Preoperative MAD (mm) | Postoperative MAD (mm)* |
|---|---|---|
| Unilateral frame | ||
| Preoperative MAD lateral (valgus) n = 7 | 48 lateral (20–83 lateral) | 7.5 (3–19) |
| Preoperative MAD medial (varus) n = 3 | 61 medial (18–100 medial) | 8.5 (4–12) |
| Fixator-assisted plating | ||
| Preoperative MAD lateral (valgus) n = 6 | 32 lateral (15–55 lateral) | 8 (0–35) |
| Preoperative MAD medial (varus) n = 1 | 64 medial | 0 |
* Postoperative MAD values are expressed as absolute mm away from the center of the knee.
Table 5.
Preoperative versus postoperative MAD (overcorrection)
| Deformity/number of patients | Preoperative mean MAD (mm) | Postoperative mean MAD (mm)* |
|---|---|---|
| Unilateral frame | ||
| Preoperative MAD lateral (valgus) n = 8 | 21 lateral (8–39 lateral) | 12 (7–20 medial) |
| Preoperative MAD medial (varus) n = 1 | 47 medial | 5 lateral |
| Fixator-assisted plating | ||
| Preoperative MAD lateral (valgus) n = 6 | 22 lateral (3–54 lateral) | 11 (5–19 medial) |
* Postoperative MAD values are expressed as absolute mm away from the center of the knee.
Table 6.
Preoperative versus postoperative LDFA
| Deformity | Preoperative LDFA (degrees) | Postoperative LDFA (degrees) |
|---|---|---|
| Unilateral frame | ||
| Preoperative LDFA less than 90° (valgus) | 85 ± 6 | 90 ± 3 |
| Preoperative LDFA greater than or equal to 90° (varus) | 95 ± 6 | 90 ± 3 |
| Fixator-assisted plating | ||
| Preoperative LDFA less than 90° (valgus) | 84 ± 7 | 91 ± 2 |
| Preoperative LDFA greater than or equal to 90° (varus) | 96 ± 7 | 91 ± 2 |
LDFA = lateral distal femoral angle.
The operative time for fixator-assisted plating (mean, 122 minutes) was longer (p = 0.001) than application of a unilateral frame (mean, 94 minutes). The average time patients wore the unilateral frame was 111 ± 24 days.
At last followup, knee ROM was similar to the preoperative ROM in both groups (p = 0.501).
We observed no nonunions, deep infections, or complications in our study population. Good postoperative pin care by patients resulted in no pin site infections. One patient (with a unilateral frame) presented with new-onset thigh pain on the day of frame removal. A radiograph showed a fracture proximal to the osteotomy site through a pin site. We removed the pin and left the frame in place for an additional 6 weeks. None of the patients with unilateral frames required additional alignment changes postoperatively.
Patients who underwent fixator-assisted plating tended to require postoperative transfusions more than those with a unilateral frame. Seven extremities treated with a locking plate experienced hardware-related discomfort and underwent hardware removal at an average of 10 months (range, 6–13 months) postoperatively.
Discussion
The literature suggests that progressive osteoarthritis is associated with malalignment of the joints [8, 9, 25, 35, 38]. The benefits of early femoral osteotomy to correct the deformity are twofold: biomechanical studies and studies containing short-term data suggest that realignment often reduces symptoms [8, 9] and may prevent joint degeneration before arthritic changes [8, 9, 38], and restoration of normal alignment in the patients with arthritis often can decrease pain, improve function, and slow further degeneration [9, 38]. Moreover, if the relief of symptoms is incomplete, and the patient later requires joint replacement, the arthroplasty may be simplified by restoration of the anatomy. There is little to suggest choosing one technique over the other for fixation after a DFO. Regarding this, we asked the following: (1) how accurately were we able to correct the deformities, based on our preoperative goals for the MAD and LDFA; were there any differences in (2) the intraoperative time and (3) preoperative and postoperative knee ROM; and (4) what complications are associated with either technique?
Our study has several limitations. First, the patients were reviewed retrospectively and most data were retrieved from charts. We occasionally needed to retrospectively measure radiographs, but these measurements were made by one author (RS) using a uniform method. Second, we included all patients treated using either fixation technique, which resulted in different proportions of men to women in both groups. However, other variables, such as age, preoperative joint orientation angles, and proportion of varus/valgus deformities, are comparable. Third, our study is a small series and therefore we were not able to look at subjective variables such as pain control, patient satisfaction, and their experiences with the rehabilitation process. Therefore, we chose the objective variables of joint orientation angle correction, joint ROM, operative times, and complication profile. Fourth, we found inconsistent recording of pain, narcotic use, cost, preoperative and postoperative SF-36 scores, and superficial pin infection. Although our results show that the techniques are equivalent in terms of accuracy of correction of joint orientation angles, a future larger prospective study would better define the full experience of undergoing these two different surgical techniques and help patients and doctors make a more informed decision.
We found that both methods reliably and accurately corrected the deformity. This corroborates with other studies [1, 21, 22, 29, 37, 42, 43]. However, we would like to highlight one patient (age 64 years) who presented with a MAD of 55 mm lateral and a dynamic deformity with joint line obliquity and lax collateral ligaments. After plating, the knee lapsed back into valgus, and the MAD at last followup was 35 mm lateral. We suggest fixator-assisted plating is not ideal for patients with a very dynamic deformity, as it is difficult to predict how the joint line obliquity will affect the final position. External fixation may be a better approach for these patients.
Various studies of fractures [3, 15, 40, 41] report operative times, but it is difficult to draw parallels with these. However, we agree with Boghdady and Shalaby [3] that familiarity with the operative technique plays a major role in reducing the mean operative time.
The postoperative ROM of the knee was preserved in our series of patients. This concurs with other series, such as the series of Oh et al. [21] that included 19 limbs that were corrected using a locking plate and there was no loss of adjacent joint ROM when measured at last followup. Higher rates of adjacent joint stiffness were reported in other studies [3, 15, 40, 41].
Although our study broadly fits into the framework of previous studies examining deformity correction [28, 30, 31], there have not been any studies comparing these methods of fixation in adult distal femur osteotomies. We found both methods of femoral fixation are associated with low complication rates. Although locking plates provide more mechanical rigidity at the osteotomy site, common disadvantages include the risk of hardware failure or painful hardware, inability for residual correction after surgery, and potential bone loss under the plate [27]. The most common postoperative problem encountered was painful hardware, and seven patients treated with a locking plate experienced pain, which led to hardware removal at an average of 10 months after surgery. Despite this, several studies show rigid internal fixation is used extensively in patients after DFOs [1, 18, 21, 22, 42]. Our results are corroborated by Keast-Butler and Schemitsch’s review of fixation techniques, where they found no evidence supporting internal fixation with plates over external fixation after distal radial fractures [10]. We report a smaller complication profile compared with fracture studies [2, 29, 32] which suggest definitive treatment of femoral fractures with external fixation is associated with nonunion in 9% to 20% of patients, deep pin track infections in 6% to 20%, and knee stiffness in 0% to 45%, whereas a systematic literature review by Zlowodzki et al. [43] (n = 327) found that average nonunion, fixation failure, deep infection, and secondary surgery rates were 5.5%, 4.9%, 2.1%, and 16.2%, respectively. Fixation failure has been attributed to waiting too long to bone graft defects, premature weightbearing, and placing the plate too anterior on the femoral shaft [4, 36, 37].
We found both surgical techniques provided similarly accurate deformity correction, and have unique disadvantages intraoperatively and postoperatively, which should be evaluated for every patient to achieve the greatest concordance and optimal surgical outcome. This reiterates the statement by Paley et al. [24, 26] that the CORA method and principles of planning deformity correction can be applied with most hardware systems, and any complications tend to be associated with inappropriate application rather than the choice of hardware. Both techniques of DFO can be used effectively. The choice of technique is based on the clinical scenario as well as the surgeon’s experience and preference.
Acknowledgment
We thank Lindsey Schacter for assistance with data collection in this project.
Footnotes
The institution of the authors has received support from EBI/Biomet and Smith and Nephew Inc, but not directly for this study.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research
References
- 1.Aglietti P, Menchetti PP. Distal femoral varus osteotomy in the valgus osteoarthritic knee. Am J Knee Surg. 2000;13:89–95. [PubMed] [Google Scholar]
- 2.Alonso J, Geissler W, Hughes JL. External fixation of femoral fractures: indications and limitations. Clin Orthop Relat Res. 1989;241:83–88. [PubMed] [Google Scholar]
- 3.Boghdady GW, Shalaby M. Safety and reliability of external fixation for basicervical and intertrochanteric fractures in high-risk elderly patients. Strategies Trauma Limb Reconstr. 2007;2:83–89. doi: 10.1007/s11751-007-0025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur: a report of four cases. J Orthop Trauma. 2004;18:565–570. doi: 10.1097/00005131-200409000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Cooke TD, Pichora D, Siu D, Scudamore RA, Bryant JT. Surgical implications of varus deformity of the knee with obliquity of joint surfaces. J Bone Joint Surg Br. 1989;71:560–565. doi: 10.1302/0301-620X.71B4.2768297. [DOI] [PubMed] [Google Scholar]
- 6.Edgerton BC, Mariani EM, Morrey BF. Distal femoral varus osteotomy for painful genu valgum: a five-to-11-year follow-up study. Clin Orthop Relat Res. 1993;288:263–269. [PubMed] [Google Scholar]
- 7.Fragomen AT, Rozbruch SR. Proximal femoral osteotomy. In: Rozbruch SR, Ilizarov S, editors. Limb Lengthening and Reconstruction Surgery. New York, NY: Informa Healthcare USA Inc; 2006. pp. 369–384. [Google Scholar]
- 8.Guettler J, Glisson R, Stubbs A, Jurist K, Higgins L. The triad of varus malalignment, meniscectomy, and chondral damage: a biomechanical explanation for joint degeneration. Orthopedics. 2007;30:558–566. doi: 10.3928/01477447-20070701-18. [DOI] [PubMed] [Google Scholar]
- 9.Gugenheim JJ, Jr, Brinker MR. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J Bone Joint Surg Am. 2003;85:1229–1237. doi: 10.2106/00004623-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Keast-Butler O, Schemitsch EH. Biology versus mechanics in the treatment of distal radial fractures. J Orthop Trauma. 2008;22(8 suppl):S91–S95. doi: 10.1097/BOT.0b013e3181839655. [DOI] [PubMed] [Google Scholar]
- 11.Kettelkamp DB, Hillberry BM, Murrish DE, Heck DA. Degenerative arthritis of the knee secondary to fracture malunion. Clin Orthop Relat Res. 1988;234:159–169. [PubMed] [Google Scholar]
- 12.Khakharia S, Bigman D, Fragomen AT, Pavlov H, Rozbruch SR. Comparison of PACS and hard-copy 51-inch radiographs for measuring leg length and deformity. Clin Orthop Relat Res. 2010 Jul 13. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 13.Kline SC, Bostrum M, Griffin PP. Femoral varus: an important component in late-onset Blount’s disease. J Pediatr Orthop. 1992;12:197–206. doi: 10.1097/01241398-199203000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Knapp DR, Jr, Price CT. Correction of distal femoral deformity. Clin Orthop Relat Res. 1990;255:75–80. [PubMed] [Google Scholar]
- 15.Kourtzis N, Pafilas D, Kasimatis G. Management of pertrochanteric fractures in the elderly patients with an external fixator. Injury. 2001;32(suppl 4):SD115–SD128. doi: 10.1016/s0020-1383(01)00158-9. [DOI] [PubMed] [Google Scholar]
- 16.Krettek C, Miclau T, Grun O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures: technical note. Injury. 1998;29(suppl 3):C29–C39. doi: 10.1016/S0020-1383(98)95006-9. [DOI] [PubMed] [Google Scholar]
- 17.Maquet P. The treatment of choice in osteoarthritis of the knee. Clin Orthop Relat Res. 1985;192:108–112. [PubMed] [Google Scholar]
- 18.McDermott AG, Finklestein JA, Farine I, Boynton EL, MacIntosh DL, Gross A. Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am. 1988;70:110–116. [PubMed] [Google Scholar]
- 19.McKellop HA, Llinas A, Sarmiento A. Effects of tibial malalignment on the knee and ankle. Orthop Clin North Am. 1994;25:415–423. [PubMed] [Google Scholar]
- 20.Morsy A, Tsuchiya H, Matsubara H, Kabata T, Tomita K. Ilizarov deformity correction of the lower limbs in Ellis-van Creveld syndrome. J Orthop Sci. 2007;12:505–509. doi: 10.1007/s00776-007-1157-7. [DOI] [PubMed] [Google Scholar]
- 21.Oh CW, Song HR, Kim JW, Kyung HS, Lee HJ, Min WK, Park BC. Deformity correction with submuscular plating technique in children. J Pediatr Orthop B. 2010;19:47–54. doi: 10.1097/BPB.0b013e32832f5b06. [DOI] [PubMed] [Google Scholar]
- 22.Omidi-Kashani F, Hasankhani IG, Mazlumi M, Ebrahimzadeh MH. Varus distal femoral osteotomy in young adults with valgus knee. J Orthop Surg Res. 2009;4:15. doi: 10.1186/1749-799X-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 24.Paley D. Chapter 11, Hardware and osteotomy considerations. In: Principles of Deformity Correction. Heidelberg, Germany: Springer-Verlag; 2002:291–410.
- 25.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 27.Perren SM. Evolution of the internal fixation of long bone fractures: the scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093–1110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 28.Pugh K, Rozbruch SR. Nonunions and malunions. In: Baumgaertner MR, Tornetta P, editors. Orthopaedic Knowledge Update Trauma 3. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005. pp. 115–130. [Google Scholar]
- 29.Ramseier LE, Janicki JA, Weir S, Narayanan UG. Femoral fractures in adolescents: a comparison of four methods of fixation. J Bone Joint Surg Am. 2010;92:1122–1129. doi: 10.2106/JBJS.H.01735. [DOI] [PubMed] [Google Scholar]
- 30.Rozbruch SR, Fragomen AT, Ilizarov S. Correction of tibial deformity with use of the Ilizarov-Taylor spatial frame. J Bone Joint Surg Am. 2006;88(suppl 4):156–174. doi: 10.2106/JBJS.F.00745. [DOI] [PubMed] [Google Scholar]
- 31.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT, Ilizarov G. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Relat Res. 2010;468:1352–1361. doi: 10.1007/s11999-009-1161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rooser B, Bengtson S, Herrlin K, Onnerfalt R. External fixation of femoral fractures: experience with 15 cases. J Orthop Trauma. 1990;4:70–74. doi: 10.1097/00005131-199003000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Sabharwal S. Blount disease. J Bone Joint Surg Am. 2009;91:1758–1776. doi: 10.2106/JBJS.H.01348. [DOI] [PubMed] [Google Scholar]
- 34.Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg Am. 2008;90:43–51. doi: 10.2106/JBJS.F.01514. [DOI] [PubMed] [Google Scholar]
- 35.Saldanha KA, Saleh M, Bell MJ, Fernandes JA. Limb lengthening and correction of deformity in the lower limbs of children with osteogenesis imperfecta. J Bone Joint Surg Br. 2004;86:259–265. doi: 10.1302/0301-620X.86B2.14393. [DOI] [PubMed] [Google Scholar]
- 36.Schandelmaier P, Partenheimer A, Koenemann B, Grun OA, Krettek C. Distal femoral fractures and LISS stabilization. Injury. 2001;32(3):SC55–SC63. doi: 10.1016/s0020-1383(01)00184-x. [DOI] [PubMed] [Google Scholar]
- 37.Schütz M, Müller M, Krettek C, Höntzsch D, Regazzoni P, Ganz R, Haas N. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001;32(suppl 3):SC48–SC54. doi: 10.1016/s0020-1383(01)00183-8. [DOI] [PubMed] [Google Scholar]
- 38.Sharma L, Eckstein F, Song J, Guermazi A, Prasad P, Kapoor D, Cahue S, Marshall M, Hudelmaier M, Dunlop D. Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum. 2008;58:1716–1726. doi: 10.1002/art.23462. [DOI] [PubMed] [Google Scholar]
- 39.Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25:367–377. [PubMed] [Google Scholar]
- 40.Tomak Y, Kocaoglu M, Piskin A, Yildiz C, Gulman B, Tomak L. Treatment of intertrochanteric fractures in geriatric patients with a modified external fixator. Injury. 2005;36:635–643. doi: 10.1016/j.injury.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 41.Vossinakis IC, Badras LS. The external fixator compared with the sliding hip screw for pertrochanteric fractures of the femur. J Bone Joint Surg Br. 2002;84:23–29. doi: 10.1302/0301-620X.84B1.12034. [DOI] [PubMed] [Google Scholar]
- 42.Wang JW, Hsu CC. Distal femoral varus osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am. 2005;87:127–133. doi: 10.2106/JBJS.C.01559. [DOI] [PubMed] [Google Scholar]
- 43.Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005) J Orthop Trauma. 2006;20:366–371. doi: 10.1097/00005131-200605000-00013. [DOI] [PubMed] [Google Scholar]