Abstract
Background
Surgical synovectomy relieves pain in patients with rheumatoid arthritis (RA). The comparative effect of arthroscopic versus open synovectomy on pain reduction, recurrence of synovitis, radiographic progression, and need for subsequent total joint arthroplasty (TJA) is unclear. Whether synovectomy relieves pain in patients with advanced degenerative joint changes is also controversial.
Questions/purposes
We therefore asked whether arthroscopic synovectomy resulted in equal pain relief, recurrence rates, rates of radiographic progression, likelihood of arthroplasty, and whether surgical synovectomy relieved pain and halted progression in the presence of advanced RA.
Methods
We searched PubMed, Cochrane Database of Systematic Reviews, and BMJ Clinical Evidence. After appropriate selection criteria, 58 studies were identified, including 36 on open synovectomy and 22 on arthroscopic synovectomy, with a total of 2589 patients and a mean followup of 6.1 years. Meta-analysis was performed for knees and elbows, comparing open versus arthroscopic synovectomy. Variables included the percentage of patients with pain reduction, recurrence of synovitis, radiographic progression, and need for subsequent TJA or arthrodesis.
Results
Patients undergoing arthroscopic synovectomy had similar pain reduction, but more frequent recurrences of synovitis and radiographic progression than patients with open synovectomy. Patients undergoing arthroscopic synovectomy had similar and decreased risks of subsequent elbow and knee arthroplasties, respectively. Advanced preoperative radiographic RA did not correlate with worse pain scores nor increased need for subsequent arthroplasty when compared with minimal degenerative joint changes.
Conclusions
Arthroscopic synovectomy, while providing similar pain relief, may place patients at higher risk for recurrence and radiographic progression of RA. Advanced preoperative degenerative joint disease should not be an absolute contraindication to synovectomy.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
With RA, the synovial lining is presumably the primary autoimmune target [17]. Inflammation progresses from synovitis to pannus invasion, with loss of articular cartilage and destruction of subchondral bone architecture [17, 58]. Although medical therapy has advanced considerably, many patients remain unresponsive to pharmacologic treatment. Some authors recommend surgical synovectomy for patients who do not experience substantial pain relief in response to medical therapy for 6 months [9, 42, 58]. This procedure was first proposed at a meeting of the Society of Surgery of Paris in 1900 [41]. By removing all visible synovial lining, synovectomy can alleviate local pain and swelling [19, 26, 47, 51, 56, 65]. Additionally, by removing the inflammatory target, synovectomy could slow progression of RA [1, 5, 11, 35, 52], although this point is contested [31, 45, 51]. Advanced RA (radiographically defined as Larsen Stages III-V [34]) traditionally has been viewed as a contraindication to synovectomy, as the procedure does not address changes in the articular cartilage or subchondral bone [42]. However, some authors have argued that synovectomy relieves pain even for advanced RA [14, 20, 37, 50, 51].
Debate exists regarding the comparative effect of open versus arthroscopic synovectomy on pain relief and recurrence [65]. Arthroscopic synovectomy offers several theoretical advantages, including decreased invasiveness of surgery, potential for faster recovery, and reduced hospital stay. Concerns remain that arthroscopic synovectomy may result in subtotal resection of the synovial lining, and more rapid recurrence of joint pain, progression of disease, and likelihood of arthroplasty. In the sole published comparative trial, Tanaka et al. [65] assigned 54 patients to either arthroscopic or open synovectomy based on ROM so as to minimize baseline differences in ROM between cohorts. These patients were followed for a mean of 13 years, and no differences were found between open or arthroscopic synovectomy groups regarding pain, function, recurrence of synovitis, progression to arthroplasty, or radiographic progression. However, no power analyses were performed, specifically for the end points of recurrence of synovitis or radiographic progression. From these data the authors were unable to recommend one approach over the other [65]. Numerous observational studies exist for the open and the arthroscopic approaches in the knee and the elbow [11, 13, 20, 21, 26, 28, 33, 39, 43, 44, 54, 65], but as each examines a specific approach, it is difficult to use one specific study to justify using one approach over another. Thus, the question regarding whether arthroscopic synovectomy provides similar rates of pain relief, recurrence, progression, and subsequent TJA to open synovectomy remains unanswered.
We therefore asked whether arthroscopic synovectomy resulted in equal pain relief, recurrence rates, rates of radiographic progression, likelihood of arthroplasty, and whether surgical synovectomy in the presence of advanced RA relieved pain and halted progression.
Search Strategy and Criteria
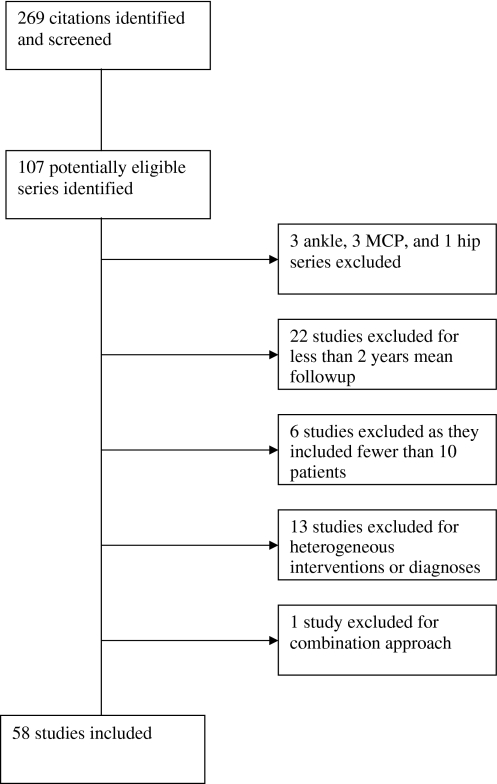
We reviewed the literature using the most common databases of published medical literature, including PubMed, Cochrane Database of Systematic Reviews, and BMJ Clinical Evidence. Our query terms were “synovectomy” and “rheumatoid arthritis” and our search was limited to papers written in English, research on humans, age older than 18 years, and publication date later than 1975. A publication date limitation was decided on because of the vast differences in technique and perioperative management of synovectomy performed in the 1960s and early 1970s compared with those used more recently. This search returned 267 citations, the abstracts of which we reviewed to narrow down to studies examining any of several clinical effects of surgical synovectomy in RA (Fig. 1). Exclusion criteria included: joints for which three or fewer studies could be identified, sample size less than 10, less than 2 years mean followup, lack of either preoperative or postoperative radiographs, inclusion of combination treatments (such as arthrodesis, tendon transfers, etc, with the exception of radial head resection), or heterogeneity of procedures, joints, approaches, or diagnoses without segregation of results. One study was excluded because the use of a miniarthrotomy with arthroscopic assistance for synovectomy of the knee could not be classified as open or arthroscopic [46]. After these criteria, 58 manuscripts remained.
Fig. 1.
The flowchart shows the effect of exclusion criteria on the number of included studies. The initial literature searches revealed 267 citations, 58 ultimately were included. MCP = metacarpophalangeal joint.
From each study the following data were collected: first author, year of publication, journal, joint involved, approach (open versus arthroscopic), number of subjects, average age of subjects, number of female subjects, length of average followup, percent of patients with pain reduction at last followup, percent of patients with recurrence of synovitis at last followup (as defined by various authors as either erythema, swelling, heat, and/or the need for repeat synovectomy [19, 39, 51, 65]), percent of patients with radiographic progression at last followup (an increase in numeric grade as defined by Larsen et al. [34], Steinbrocker et al. [63], the modification by Rau and Herborn of the system by Larsen et al. [55], Smiley and Wasilewski [60], or Crossan and Vallance [12]), percent of patients who underwent arthroplasty or arthrodesis of the joint in question by last followup, percent of patients with radiographically advanced disease preoperatively defined by Stage III or greater [34] (Table 1), or Stage III or greater according to Steinbrocker et al. [63], and whether the study concluded their intervention affected ROM. All studies were reviewed and evaluated by one author (PNC). Study quality was judged based on selection criteria, study design, completeness of followup, clarity of description of the intervention, clarity of description of the outcomes measured, and completeness of data provided. In most studies one unblinded orthopaedic surgeon assessed radiographs. Blinded radiographic assessments, multiple reviewers, and/or consensus methods rarely were described. The 58 studies had a mean sample size of 44.6 patients (range, 10–202 patients) and a mean length of followup of 6.1 years (range, 2.0–14.4 years), with a total of 2589 patients (Table 2).
Table 1.
Larsen’s grading system for RA
| Grade | Definition |
|---|---|
| 0 | Normal |
| 1 | Soft tissue swelling, slight joint space narrowing (< 25% of the original joint space), periarticular osteoporosis |
| 2 | Definite early abnormality, one or several small erosions |
| 3 | Medium destructive abnormality, marked erosions |
| 4 | Severe destructive abnormality, large erosions |
| 5 | Gross deformity, the bony outlines of the joint have disappeared |
Table 2.
Studies included in analysis
| First author | Year | Approach | Joint | Number of patients | Average years of followup |
|---|---|---|---|---|---|
| Tanaka [65] | 2006 | Arthroscopic and open cohorts | Elbow | 23 | 13.0 |
| Nemoto [44] | 2004 | Arthroscopic | Elbow | 11 | 3.1 |
| Horiuchi [26] | 2002 | Arthroscopic | Elbow | 21 | 8.1 |
| Lee [36] | 1997 | Arthroscopic | Elbow | 14 | 3.5 |
| Nakagawa [43] | 2007 | Open | Elbow | 15 | 8.7 |
| Fuerst [19] | 2006 | Open | Elbow | 85 | 8.7 |
| Maenpaa [39] | 2003 | Open | Elbow | 103 | 5.2 |
| Woods [72] | 1999 | Open | Elbow | 45 | 10.0 |
| Gendi [20] | 1997 | Open | Elbow | 171 | 6.5 |
| Jensen [29] | 1996 | Open | Elbow | 25 | 4.3 |
| Lonner [38] | 1997 | Open | Elbow | 12 | 6.1 |
| Herold [24] | 1995 | Open | Elbow | 12 | 14.0 |
| Vahvanen [68] | 1991 | Open | Elbow | 70 | 7.5 |
| Alexiades [2] | 1990 | Open | Elbow | 20 | 14.4 |
| Tulp [67] | 1989 | Open | Elbow | 50 | 6.5 |
| Ferlic [15] | 1987 | Open | Elbow | 57 | 7.2 |
| Saito [57] | 1986 | Open | Elbow | 23 | 4.0 |
| Brumfield [8] | 1985 | Open | Elbow | 42 | 6.7 |
| Gschwend [23] | 1985 | Open | Elbow | 35 | |
| Linclau [37] | 1983 | Open | Elbow | 31 | 2.5 |
| Eichenblat [14] | 1982 | Open | Elbow | 25 | 5.5 |
| Copeland [10] | 1979 | Open | Elbow | 25 | 4.3 |
| Brattstrom [7] | 1975 | Open | Elbow | 105 | 3.8 |
| Stein [62] | 1975 | Open | Elbow | 32 | 3.3 |
| Rao [54] | 2006 | Arthroscopic | Knee | 52 | 5.0 |
| Gibbons [21] | 2002 | Arthroscopic | Knee | 25 | 8.0 |
| Tanaka [66] | 2002 | Arthroscopic | Knee | 59 | 5.0 |
| Roch-Bras [56] | 2002 | Arthroscopic | Knee | 41 | 8.9 |
| Takagi [64] | 2001 | Arthroscopic | Knee | 15 | 2.0 |
| Sculco [59] | 2000 | Arthroscopic | Knee | 22 | 4.0 |
| Klug [33] | 2000 | Arthroscopic | Knee | 93 | 2.8 |
| Fiocco [16] | 1996 | Arthroscopic | Knee | 17 | 2.5 |
| Ogilvie-Harris [47] | 1991 | Arthroscopic | Knee | 96 | 3.0 |
| Smiley [60] | 1990 | Arthroscopic | Knee | 25 | 4.0 |
| Klein [32] | 1988 | Arthroscopic | Knee | 59 | 2.7 |
| Wilkes [71] | 1985 | Arthroscopic | Knee | 30 | 4.8 |
| Aritomi [3] | 1981 | Arthroscopic | Knee | 33 | 3.7 |
| Jensen [28] | 1991 | Open | Knee | 55 | 6.1 |
| Cozzolino [11] | 1991 | Open | Knee | 38 | 4.0 |
| Doets [13] | 1989 | Open | Knee | 83 | 7.0 |
| Ishikawa [27] | 1986 | Open | Knee | 78 | 14.1 |
| Meijers [40] | 1983 | Open | Knee | 10 | 5.0 |
| Goldie [22] | 1981 | Open | Knee | 44 | 14 |
| Fowler [18] | 1977 | Open | Knee | 19 | 4.3 |
| Jones [30] | 1976 | Open | Knee | 43 | 4.0 |
| Patiala [52] | 1976 | Open | Knee | 202 | 9.5 |
| Pahle [48] | 1975 | Open | Knee | 20 | 3.0 |
| A&RC [4] | 1976 | Open | Knee | 33 | 3.0 |
| Laurin [35] | 1974 | Open | Knee | 66 | 7.5 |
| Smith [61] | 2006 | Arthroscopic | Shoulder | 16 | 5.5 |
| Wakitani [70] | 1999 | Arthroscopic | Shoulder | 18 | 7.8 |
| Petersson [53] | 1986 | Open | Shoulder | 15 | 4.0 |
| Pahle [50] | 1985 | Open | Shoulder | 54 | 5.3 |
| Pahle [49] | 1981 | Open | Shoulder | 29 | 2.9 |
| Kim [31] | 2006 | Arthroscopic | Wrist | 19 | 5.8 |
| Park [51] | 2003 | Arthroscopic | Wrist | 19 | 2.4 |
| Adolfsson [1] | 1997 | Arthroscopic | Wrist | 24 | 3.8 |
| Vahvanen [69] | 1984 | Open | Wrist | 97 | 8.5 |
| Ochi [45] | 1991 | Open | Wrist/ knee | 79 | 5.0 |
| Mean | 44.6 | 6.1 | |||
| Median | 30.5 | 5.1 | |||
| Minimum | 10 | 2.0 | |||
| Maximum | 202 | 14.4 |
Arithmetic mean, median, minimum, and maximum are reported for number of subjects and average years of followup; A&RC = Arthritis and Rheumatism Council.
Descriptive statistics, including standard deviations, were weighted for sample size [6]. Unless otherwise noted, all analyses were segregated by joint and approach (Table 3). Only two studies examining shoulder synovectomy by the arthroscopic approach [61, 70] and one study of synovectomy of the wrist by the open approach [69] could be identified. Although descriptive statistics were calculated for these joints, they were excluded from further analyses. As each variable was reported by a distinct pool of studies, heterogeneity analyses [25] were performed on each variable separately, revealing meta-analysis to be valid (p > 0.05) on all variables except ROM (p < 0.001) (Table 4). No further analyses of ROM were performed. Unweighted data were pooled. Pooling corrects for sample size and weighting is unnecessary for these analyses. Chi square tests were performed to compare open and arthroscopic approaches for knees and elbows with respect to number of patients with (1) pain reduction, (2) recurrent synovitis, (3) radiographic progression, and (4) progression to TJA or arthrodesis. As most reported data did not segregate results based on radiographic stage, no pooling could be performed to evaluate the effect of advanced preoperative RA on pain reduction or subsequent TJA. Instead, linear regression was performed with individual studies as data points. Studies with greater than 50% of patients with preoperative radiographically advanced RA also were subgrouped for calculation of weighted means. All analyses were performed using Excel X© (Microsoft©, Redmond, WA, USA) and SPSS 16.0© (SPSS©, Chicago, IL, USA).
Table 3.
Descriptive statistics of demographic data by joint and approach, weighted for sample size
| Joint | Approach | Year of publication | Age (years) | Years of followup | % Female | % of patients with advanced RA preoperatively |
|---|---|---|---|---|---|---|
| Elbow | Arthroscopic | 2003 | 51.7 | 8.0 | 80 | 71.9 |
| Open | 1992 | 52.8 | 6.5 | 60 | 56.7 | |
| Knee | Arthroscopic | 1996 | 43.1 | 4.1 | 80 | 27.5 |
| Open | 1981 | 56.8 | 8.2 | 60 | 38.5 |
Advanced RA is defined radiographically by greater than Larsen Stage II.
Table 4.
Heterogeneity statistics.
| Variable | I2 | p Value |
|---|---|---|
| Percent of patients with pain relief | 16% | 0.28 |
| Percent of patients with synovitic recurrence | 0% | 0.52 |
| Percent of patients with radiographic progression | 61% | 0.11 |
| Percent of patients who underwent TJA | 0% | 0.49 |
| Synovectomy improved range of motion | 91% | 0.001 |
I2 = statistic that describes portion of variation between studies that can be attributed to heterogeneity of data; TJA = total joint arthroplasty.
Results
Most patients experienced a reduction in pain at last followup, and a minority had recurrent synovitis or required TJA or arthrodesis (Table 5). Radiographic progression was common regardless of the joint or approach (Table 5). Preoperative advanced radiographic RA was common, accounting for 43% of the patients in trials that reported preoperative radiographic classification. All studies were Level of Evidence IV.
Table 5.
Weighted averages and standard deviations
| Approach | Joint | Percent of patients with less pain than preoperatively (± SD) | Percent of patients with recurrent synovitis (± SD) | Percent of patients with radiographic progression (± SD) | Percent of patients who had undergone TJA (± SD) | Percent of patients with advanced RA preoperatively (± SD) |
|---|---|---|---|---|---|---|
| Arthroscopic | Elbow | 79.4 ± 31.1% | 21.9 ± 7.9% | 65.6 ± 29.9% | 15.0 ± 12.2% | 71.9 ± 10.2% |
| Open | Elbow | 80.0 ± 9.7% | 9.3 ± 8.9% | 27.7 ± 22.7% | 19.2 ± 16.5% | 56.7 ± 36.4% |
| Arthroscopic | Knee | 73.1 ± 9.0% | 34.9 ± 30.4% | 75.4 ± 30.1% | 10.7 ± 14.3% | 23.1 ± 23.4% |
| Open | Knee | 65.5 ± 9.0% | 13.2 ± 7.7% | 55.2 ± 23.0% | 19.0 ± 14.8% | 38.5 ± 16.1% |
| Arthroscopic | Wrist | 79.1 ± 13.1% | 10.5 ± NA% | 34.9 ± 17.4% | 0.0 ± 0.0% | 34.2 ± 33.5% |
| Open | Wrist | 88.0 ± NA% | 24.0 ± NA% | 88.7 ± NA% | 8.2 ± NA% | 6.2 ± NA% |
| Arthroscopic | Shoulder | 81.3 ± NA% | NA | 87.5 ± NA% | 6.3 ± NA% | 50.0 ± NA% |
| Open | Shoulder | 83.7 ± 4.8% | 0.0 ± 0.0% | 26.6 ± NA% | 11.6 ± 1.3% | 61.4 ± 25.7% |
| Mean | 75.2 ± 12.0% | 17.4 ± 18.8% | 47.5 ± 30.7% | 15.9 ± 14.6% | 43.1 ± 29.6% | |
TJA = total joint arthroplasty; NA = not applicable owing to insufficient data; SD = standard deviation.
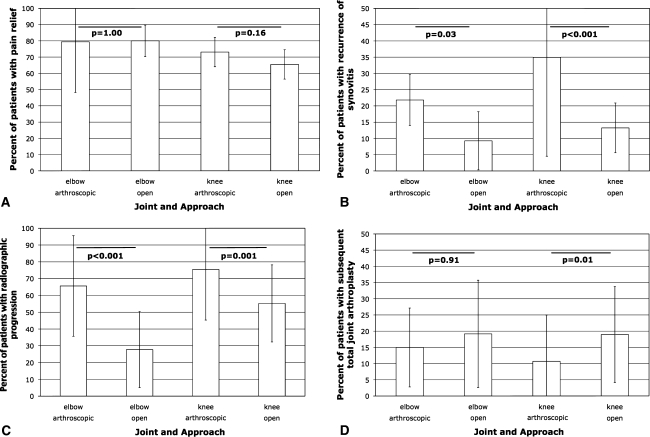
Thirty-three of the 58 studies reported the percentage of patients with pain reduction at last followup. Combining approaches and joints, 75.2% of patients reported pain reduction at last followup (Table 4). Arthroscopic and open synovectomy provided similar pain relief at last followup for elbows (p = 1.00) and knees (p = 0.16) (Fig. 2A).
Fig. 2A–D.
The graphs show the weighted mean results at last followup segregated by joint and approach, with weighted standard deviation error bars. The lines connecting the bars show the results of chi square tests. They show (A) percent of patients with pain reduction as compared with preoperatively, (B) percent of patients with recurrence of synovitis, (C) percent of patients with radiographic progression, and (D) percent of patients who subsequently underwent TJA or arthrodesis.
Thirty-one of the 58 studies reported the percentage of patients with recurrent synovitis at last followup. Combining joints and approaches, 17.4% of patients had recurrence of synovitis (Table 2). Arthroscopic synovectomy was more likely than open synovectomy to lead to recurrence of synovitis for elbows (p = 0.03) and knees (p < 0.001) (Fig. 2B).
Twenty-seven of the 58 studies reported the percentage of patients with radiographic progression at last followup. Combining joints and approaches, 47.5% of patients showed radiographic progression (Table 2). Arthroscopic synovectomy was more likely than open synovectomy to lead to radiographic progression for elbows (p < 0.001) and knees (p = 0.001) (Fig. 2C).
Thirty-five of the 58 studies reported the percentage of patients who underwent TJA or arthrodesis at last followup. Combining joints and approaches, 15.9% of patients underwent subsequent TJA at followups ranging from 2 to 14 years (Table 2). Arthroscopic and open synovectomy were equally likely to require subsequent arthroplasty in elbows (p = 0.91), but for knees, open synovectomies were more likely to require TJA or arthrodesis (p = 0.01) at last followup (Fig. 2D).
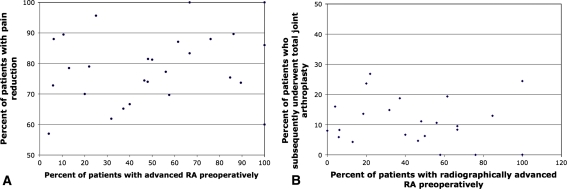
Thirty-two of the 58 studies reported the percentage of patients with preoperative radiographically advanced RA, 27 of which also reported percent of patients with pain reduction at last followup, and 23 which reported percent of patients who had undergone TJA or arthrodesis at last followup. We observed no association between percent of patients with preoperative radiographically advanced RA and either percent of patients with pain reduction at last followup (r2 = 0.054; p = 0.245) (Fig. 3A) or percent of patients who underwent subsequent TJA (r2 = 0.016; p = 0.564) (Fig. 3B). Of the 10 studies with greater than 50% of patients with preoperative radiographically advanced RA and also reporting percent of patients who underwent subsequent TJA, 10.7% underwent subsequent TJA, compared with 15.9% of all patients.
Fig. 3A–B.
The graphs show, for each study (plotted as data points), (A) percent of patients with advanced radiographic RA preoperatively versus the percent of patients with pain relief at last followup, and (B) percent of patients who had undergone TJA or arthrodesis at last followup. Linear regression revealed no correlation in either data series.
Discussion
In RA refractory to medical therapy for 6 months, surgical synovectomy has been recommended [9, 42, 58]. This procedure may alleviate local pain and swelling [19, 26, 47, 51, 56, 65] and potentially slow progression of RA [1, 5, 11, 31, 35, 45, 51, 52] by removing the synovial lining, the inflammatory target [17]. Whether this procedure can benefit patients with radiographically advanced RA is unknown [14, 20, 37, 42, 50, 51]. Whether the arthroscopic versus the open approach to the procedure affects pain relief, recurrence, radiographic progression, or need for subsequent TJA is unknown [65]. We sought to answer the question regarding whether approach or advanced preoperative disease affects these outcomes.
This study has several limitations. First, the quality of our findings is only as good as the quality of the original data. All studies included in our analysis were designated Level IV, which introduces bias and limits interpretation. Randomized clinical trials are lacking, and thus these studies are the highest level of evidence available. Second, our study design compares observational studies performed by different authors. Heterogeneity of studies limits the interpretation that can be drawn from our results. In particular the advent of disease-modifying, antirheumatic drugs has altered the clinical course of RA and could affect the above variables in more current clinical series. However, heterogeneity analyses were performed and I2 values were sufficiently high to allow meta-analytic comparison [25], suggesting comparison of studies is appropriate. Third, we did not attempt to contact authors to obtain original data. Given the large number of studies, the diversity of countries of origin, and relatively distant years of publication, this effort would have been leviathan and likely futile. Fourth, limitation to studies in the English language in just three clinical databases may bias toward research performed in the United States and Europe. Fifth, our review was limited to published data. Sixth, most studies determined radiographic progression by grade as determined by one unblinded orthopaedic surgeon, which limits the validity of these grades. As limitations three through six affect arthroscopic and open approaches equally, our results are unlikely to have been affected. Seventh, studies were reviewed by only one author (PNC). Given the numeric nature of the data collection from which conclusions have been drawn, the addition of multiple authors would be unlikely to alter our results. A randomized clinical trial could more adequately answer the questions put forward by this study. However, because of the relative rarity of this procedure, such a trial may never be performed. Thus this meta-analysis is warranted to provide some guidance in selection of approach and patients for synovectomy.
Our review of the literature suggests that synovectomy provides pain relief for 75.2% of patients at an average of 6 years postoperatively; the literature supports surgical synovectomy to provide pain relief. Arthroscopic and open synovectomy provided similar pain relief for the elbow (p = 1.00) and the knee (p = 0.16).
Only a minority (17.4%) of patients experienced recurrence of synovitis after synovectomy. Arthroscopic synovectomy was more likely than open synovectomy to lead to recurrence of synovitis for elbows (p = 0.03) and knees (p < 0.001). Whether this difference is mediated by improved observation or improved access of the synovial lining with the open approach is unclear. Future studies will be needed to explore this effect.
Many patients (47.5%) experienced progression despite synovectomy, suggesting that synovectomy does not prevent progression. Without a matched control group, we cannot draw conclusions regarding whether synovectomy alters natural history. Arthroscopic synovectomy was more likely than open synovectomy to lead to radiographic progression for elbows (p < 0.001) and knees p = 0.001). Again, the precise source of this effect is unclear.
The minority of patients (15.9%) underwent subsequent TJA, paralleling the beneficial effect of synovectomy on pain relief and synovitis recurrence. Arthroscopic and open synovectomy were equally likely to require subsequent arthroplasty in elbows (p = 0.91), but for knees, open synovectomies were more likely to require TJA or arthrodesis (p = 0.01). This finding, which contrasts with our findings in pain relief and recurrence, could be attributable to changing trends in approach in combination with changing diagnostic criteria. As arthroscopic synovectomy has become more common and diagnostic criteria no longer include tissue samples [17], synovectomy may be performed earlier in the disease course and thus be less likely to lead to TJA within 6 years.
The literature suggests synovectomy is commonly performed for patients with advanced radiographic stages of RA. Advanced disease was found in 43% of patients who underwent synovectomy in trials that used a preoperative radiographic classification. We found no correlation between radiographic stage and postoperative pain reduction or need for subsequent arthroplasty. Among the subgroup of studies performed in which a majority (> 50%) of patients showed radiographically advanced RA preoperatively, similar outcomes were seen. Previous studies have agreed with this conclusion. Gendi et al. [20] examined 171 patients and tried to predict which would respond well to synovectomy. They found no correlation between worse radiographic scores preoperatively and progression to arthroplasty. Other authors also noted that patients with advanced RA had better results than anticipated [14, 18, 20, 30, 35, 37, 50, 51]. Overall, our review suggests advanced preoperative radiographic stage of disease should not be an absolute contraindication for synovectomy.
Synovectomy provides lasting pain relief in the majority of patients at an average of 6 years followup. Only a minority (17.4%) of patients experience recurrent synovitis or progression to arthroplasty or arthrodesis (15.9%). Open and arthroscopic synovectomy appear to provide similar pain relief. Arthroscopic synovectomy of the elbow and knee might have higher rates of recurrent synovitis and radiographic progression of disease when compared with open synovectomy. Additionally, advanced preoperative radiographic stage of disease may not be an absolute contraindication to synovectomy, as these patients have similar pain reduction and no elevated risk of subsequent arthroplasty when compared with patients with less degenerative joint changes. Well-designed randomized clinical trials will be necessary to confirm these findings.
Acknowledgments
We thank Joseph Nguyen and Dr. Stephen Lyman for assistance in selecting appropriate statistical analyses.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
This work was performed at the College of Physicians and Surgeons at Columbia University in New York, NY and at the Hospital for Special Surgery in New York, NY.
References
- 1.Adolfsson L, Frisen M. Arthroscopic synovectomy of the rheumatoid wrist: a 3.8 year follow-up. J Hand Surg Br. 1997;22:711–713. doi: 10.1016/S0266-7681(97)80430-5. [DOI] [PubMed] [Google Scholar]
- 2.Alexiades M, Scott TS, Figgie MP, Inglis AE. Minimum ten year follow-up for elbow synovectomy for rheumatoid arthritis. Trans Orthop Res Soc. 1990;14:255. [Google Scholar]
- 3.Aritomi H, Yamamoto M. A clinical evaluation of arthroscopic synovectomy of the knee joint with the electric resectoscope. Ryumachi. 1981;21(Suppl):11–20. [PubMed] [Google Scholar]
- 4.Arthritis and Rheumatism Council, British Orthopaedic Association. Controlled trial of synovectomy of knee and metacarpophalangeal joints in rheumatoid arthritis. Ann Rheum Dis. 1975;35:437–442. [PMC free article] [PubMed]
- 5.Aschan W, Moberg E. A long-term study of the effect of early synovectomy in rheumatoid arthritis. Bull Hosp Jt Dis Orthop Inst. 1984;44:106–121. [PubMed] [Google Scholar]
- 6.Bland JM, Kerry SM. Statistics notes: weighted comparison of means. BMJ. 1998;316:129. doi: 10.1136/bmj.316.7125.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brattstrom H, Al Khudairy H. Synovectomy of the elbow in rheumatoid arthritis. Acta Orthop Scand. 1975;46:744–750. doi: 10.3109/17453677508989260. [DOI] [PubMed] [Google Scholar]
- 8.Brumfield RH, Jr, Resnick CT. Synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 1985;67:16–20. [PubMed] [Google Scholar]
- 9.Canale ST, Beaty JH. Campbell’s Operative Orthopaedics. New York, NY: Mosby; 2007. [Google Scholar]
- 10.Copeland SA, Taylor JG. Synovectomy of the elbow in rheumatoid arthritis: the place of excision of the head of the radius. J Bone Joint Surg Br. 1979;61:69–73. doi: 10.1302/0301-620X.61B1.422636. [DOI] [PubMed] [Google Scholar]
- 11.Cozzolino F, Gigliotti S, Giuzio E, Angrisani C. Surgical synovectomy in the treatment of rheumatoid arthritis: the results obtained in a controlled study. Chir Organi Mov. 1991;76:341–346. [PubMed] [Google Scholar]
- 12.Crossan JF, Vallance R. The shoulder joint in rheumatoid arthritis. In: Bayley I, Keddel L, editors. Shoulder Surgery. New York, NY: Springer, Verlag; 1982. pp. 131–139. [Google Scholar]
- 13.Doets HC, Bierman BT, Soesbergen RM. Synovectomy of the rheumatoid knee does not prevent deterioration: 7-year follow-up of 83 cases. Acta Orthop Scand. 1989;60:523–525. doi: 10.3109/17453678909150115. [DOI] [PubMed] [Google Scholar]
- 14.Eichenblat M, Hass A, Kessler I. Synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 1982;64:1074–1078. [PubMed] [Google Scholar]
- 15.Ferlic DC, Patchett CE, Clayton ML, Freeman AC. Elbow synovectomy in rheumatoid arthritis: long-term results. Clin Orthop Relat Res. 1987:119–125. [PubMed]
- 16.Fiocco U, Cozzi L, Rigon C, Chieco-Bianchi F, Baldovin M, Cassisi GA, Gallo C, Doria A, Favaro MA, Piccoli A, Candia A, Rubaltelli L, Todesco S. Arthroscopic synovectomy in rheumatoid and psoriatic knee joint synovitis: long-term outcome. Br J Rheumatol. 1996;35:463–470. doi: 10.1093/rheumatology/35.5.463. [DOI] [PubMed] [Google Scholar]
- 17.Firestein G, Budd RC, Harris ED. Jr, McInnes IB, Ruddy S, eds. Kelley’s Textbook of Rheumatology. New York, NY: Saunders; 2008. [Google Scholar]
- 18.Fowler RL, Berg E. Synovectomies in moderately to severely involved rheumatoid knees: an alternative to implant arthroplasty. South Med J. 1977;70:181–183, 188. [DOI] [PubMed]
- 19.Fuerst M, Fink B, Ruther W. Survival analysis and longterm results of elbow synovectomy in rheumatoid arthritis. J Rheumatol. 2006;33:892–896. [PubMed] [Google Scholar]
- 20.Gendi NS, Axon JM, Carr AJ, Pile KD, Burge PD, Mowat AG. Synovectomy of the elbow and radial head excision in rheumatoid arthritis: predictive factors and long-term outcome. J Bone Joint Surg Br. 1997;79:918–923. doi: 10.1302/0301-620X.79B6.7408. [DOI] [PubMed] [Google Scholar]
- 21.Gibbons CE, Gosal HS, Bartlett J. Long-term results of arthroscopic synovectomy for seropositive rheumatoid arthritis: 6–16 year review. Int Orthop. 2002;26:98–100. doi: 10.1007/s00264-001-0309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldie IF. Synovectomy in rheumatoid arthritis: theoretical aspects and a 14-year follow-up in the knee joint. Reconstr Surg Traumatol. 1981;18:2–7. [PubMed] [Google Scholar]
- 23.Gschwend N, Steiger U. Elbow synovectomy. Ann Chir Gynaecol Suppl. 1985;198:31–36. [PubMed] [Google Scholar]
- 24.Herold N, Schroder HA. Synovectomy and radial head excision in rheumatoid arthritis: 11 patients followed for 14 years. Acta Orthop Scand. 1995;66:252–254. doi: 10.3109/17453679508995535. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 26.Horiuchi K, Momohara S, Tomatsu T, Inoue K, Toyama Y. Arthroscopic synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2002;84:342–347. doi: 10.2106/00004623-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Ishikawa H, Ohno O, Hirohata K. Long-term results of synovectomy in rheumatoid patients. J Bone Joint Surg Am. 1986;68:198–205. [PubMed] [Google Scholar]
- 28.Jensen CM, Poulsen S, Ostergren M, Hansen KH. Early and late synovectomy of the knee in rheumatoid arthritis. Scand J Rheumatol. 1991;20:127–131. doi: 10.3109/03009749109165288. [DOI] [PubMed] [Google Scholar]
- 29.Jensen CM, Rasmussen SW, Haugegaard M, Melchior TM, Hansen H. Elbow synovectomy in rheumatoid arthritis. Acta Orthop Belg. 1996;62:144–147. [PubMed] [Google Scholar]
- 30.Jones D, Taylor JG. Experience with knee synovectomy in Norwich, 1964–1973. Acta Orthop Scand. 1976;47:423–431. doi: 10.3109/17453677608988714. [DOI] [PubMed] [Google Scholar]
- 31.Kim SJ, Jung KA, Kim JM, Kwun JD, Kang HJ. Arthroscopic synovectomy in wrists with advanced rheumatoid arthritis. Clin Orthop Relat Res. 2006;449:262–266. doi: 10.1097/01.blo.0000218732.44591.c9. [DOI] [PubMed] [Google Scholar]
- 32.Klein W, Jensen KU. Arthroscopic synovectomy of the knee joint: indication, technique, and follow-up results. Arthroscopy. 1988;4:63–71. doi: 10.1016/S0749-8063(88)80066-5. [DOI] [PubMed] [Google Scholar]
- 33.Klug S, Wittmann G, Weseloh G. Arthroscopic synovectomy of the knee joint in early cases of rheumatoid arthritis: follow-up results of a multicenter study. Arthroscopy. 2000;16:262–267. doi: 10.1016/S0749-8063(00)90050-1. [DOI] [PubMed] [Google Scholar]
- 34.Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 1977;18:481–491. doi: 10.1177/028418517701800415. [DOI] [PubMed] [Google Scholar]
- 35.Laurin CA, Desmarchais J, Daziano L, Gariepy R, Derome A. Long-term results of synovectomy of the knee in rheumatoid patients. J Bone Joint Surg Am. 1974;56:521–531. [PubMed] [Google Scholar]
- 36.Lee BP, Morrey BF. Arthroscopic synovectomy of the elbow for rheumatoid arthritis: a prospective study. J Bone Joint Surg Br. 1997;79:770–772. doi: 10.1302/0301-620X.79B5.7466. [DOI] [PubMed] [Google Scholar]
- 37.Linclau LA, Winia WP, Korst JK. Synovectomy of the elbow in rheumatoid arthritis. Acta Orthop Scand. 1983;54:935–937. doi: 10.3109/17453678308992937. [DOI] [PubMed] [Google Scholar]
- 38.Lonner JH, Stuchin SA. Synovectomy, radial head excision, and anterior capsular release in stage III inflammatory arthritis of the elbow. J Hand Surg Am. 1997;22:279–285. doi: 10.1016/S0363-5023(97)80164-5. [DOI] [PubMed] [Google Scholar]
- 39.Maenpaa HM, Kuusela PP, Kaarela K, Kautiainen HJ, Lehtinen JT, Belt EA. Reoperation rate after elbow synovectomy in rheumatoid arthritis. J Shoulder Elbow Surg. 2003;12:480–483. doi: 10.1016/S1058-2746(03)00167-8. [DOI] [PubMed] [Google Scholar]
- 40.Meijers KA, Valkenburg HA, Cats A. A synovectomy trial and the history of early knee synovitis in rheumatoid arthritis: a multicentre study. Rheumatol Int. 1983;3:161–166. doi: 10.1007/BF00541595. [DOI] [PubMed] [Google Scholar]
- 41.Mignon A. Synovectomie du genou. Bull Soc Chir Paris. 1900;26:1113–1115. [Google Scholar]
- 42.Morrey BF. The Elbow and its Disorders. New York, NY: Saunders; 2008. [Google Scholar]
- 43.Nakagawa N, Abe S, Saegusa Y, Imura S, Kubo H, Nishibayashi Y, Yoshiya S. Long-term results of open elbow synovectomy for rheumatoid arthritis. Mod Rheumatol. 2007;17:106–109. doi: 10.1007/s10165-006-0547-6. [DOI] [PubMed] [Google Scholar]
- 44.Nemoto K, Arino H, Yoshihara Y, Fujikawa K. Arthroscopic synovectomy for the rheumatoid elbow: a short-term outcome. J Shoulder Elbow Surg. 2004;13:652–655. doi: 10.1016/j.jse.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 45.Ochi T, Iwase R, Kimura T, Hirooka A, Masada K, Owaki H, Wakitani S, Murata N, Ono K. Effect of early synovectomy on the course of rheumatoid arthritis. J Rheumatol. 1991;18:1794–1798. [PubMed] [Google Scholar]
- 46.Ogawa H, Itokazu M, Ito Y, Fukuta M, Shimizu K. The therapeutic outcome of minimally invasive synovectomy assisted with arthroscopy in the rheumatoid knee. Mod Rheumatol. 2006;16:360–363. doi: 10.1007/s10165-006-0526-y. [DOI] [PubMed] [Google Scholar]
- 47.Ogilvie-Harris DJ, Basinski A. Arthroscopic synovectomy of the knee for rheumatoid arthritis. Arthroscopy. 1991;7:91–97. doi: 10.1016/0749-8063(91)90085-C. [DOI] [PubMed] [Google Scholar]
- 48.Pahle J, Raunio P, Hamalainen M. Synovectomy of rheumatoid joints. Scand J Rheumatol Suppl. 1975;153–154. [PubMed]
- 49.Pahle JA. The shoulder joint in rheumatoid arthritis: synovectomy. Reconstr Surg Traumatol. 1981;18:33–47. [PubMed] [Google Scholar]
- 50.Pahle JA, Kvarnes L. Shoulder synovectomy. Ann Chir Gynaecol Suppl. 1985;198:37–39. [PubMed] [Google Scholar]
- 51.Park MJ, Ahn JH, Kang JS. Arthroscopic synovectomy of the wrist in rheumatoid arthritis. J Bone Joint Surg Br. 2003;85:1011–1015. doi: 10.1302/0301-620X.85B7.14195. [DOI] [PubMed] [Google Scholar]
- 52.Patiala H. Follow-up study of synovectomies of the knee joint in patients suffering from rheumatoid arthritis. Scand J Rheumatol. 1976;5:167–173. doi: 10.3109/03009747609165457. [DOI] [PubMed] [Google Scholar]
- 53.Petersson CJ. Shoulder surgery in rheumatoid arthritis. Acta Orthop Scand. 1986;57:222–226. doi: 10.3109/17453678608994381. [DOI] [PubMed] [Google Scholar]
- 54.Rao SK, Rao S, Naik AM. A descriptive clinical evaluation of arthroscopic synovectomy in rheumatoid knees: a prospective study. Ceylon Med J. 2006;51:7–9. doi: 10.4038/cmj.v51i1.1368. [DOI] [PubMed] [Google Scholar]
- 55.Rau R, Herborn G. A modified version of Larsen’s scoring method to assess radiologic changes in rheumatoid arthritis. J Rheumatol. 1995;22:1976–1982. [PubMed] [Google Scholar]
- 56.Roch-Bras F, Daures JP, Legouffe MC, Sany J, Combe B. Treatment of chronic knee synovitis with arthroscopic synovectomy: longterm results. J Rheumatol. 2002;29:1171–1175. [PubMed] [Google Scholar]
- 57.Saito T, Koshino T, Okamoto R, Horiuchi S. Radical synovectomy with muscle release for the rheumatoid elbow. Acta Orthop Scand. 1986;57:71–73. doi: 10.3109/17453678608993220. [DOI] [PubMed] [Google Scholar]
- 58.Scott W. Insall and Scott’s Surgery of the Knee. New York, NY: Churchill Livingstone; 2005. [Google Scholar]
- 59.Sculco TP, Lombardi P, Miric A. The knee joint in rheumatoid arthritis. Compr Ther. 2000;26:127–133. doi: 10.1007/s12019-000-0023-8. [DOI] [PubMed] [Google Scholar]
- 60.Smiley P, Wasilewski SA. Arthroscopic synovectomy. Arthroscopy. 1990;6:18–23. doi: 10.1016/0749-8063(90)90091-Q. [DOI] [PubMed] [Google Scholar]
- 61.Smith AM, Sperling JW, O’Driscoll SW, Cofield RH. Arthroscopic shoulder synovectomy in patients with rheumatoid arthritis. Arthroscopy. 2006;22:50–56. doi: 10.1016/j.arthro.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 62.Stein H, Dickson RA, Bentley G. Rheumatoid arthritis of the elbow: pattern of joint involvement, and results of synovectomy with excision of the radial head. Ann Rheum Dis. 1975;34:403–408. doi: 10.1136/ard.34.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Steinbrocker O, Traeger CH, Batterman RC. Therapeutic criteria in rheumatoid arthritis. J Am Med Assoc. 1949;140:659–662. doi: 10.1001/jama.1949.02900430001001. [DOI] [PubMed] [Google Scholar]
- 64.Takagi T, Koshino T, Okamoto R. Arthroscopic synovectomy for rheumatoid arthritis using a holmium:YAG laser. J Rheumatol. 2001;28:1518–1522. [PubMed] [Google Scholar]
- 65.Tanaka N, Sakahashi H, Hirose K, Ishima T, Ishii S. Arthroscopic and open synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2006;88:521–525. doi: 10.2106/JBJS.E.00472. [DOI] [PubMed] [Google Scholar]
- 66.Tanaka N, Sakahashi H, Sato E, Ishii S. Immunohistological indication for arthroscopic synovectomy in rheumatoid knees: analysis of synovial samples obtained by needle arthroscopy. Clin Rheumatol. 2002;21:46–51. doi: 10.1007/s100670200011. [DOI] [PubMed] [Google Scholar]
- 67.Tulp NJ, Winia WP. Synovectomy of the elbow in rheumatoid arthritis: long-term results. J Bone Joint Surg Br. 1989;71:664–666. doi: 10.1302/0301-620X.71B4.2768318. [DOI] [PubMed] [Google Scholar]
- 68.Vahvanen V, Eskola A, Peltonen J. Results of elbow synovectomy in rheumatoid arthritis. Arch Orthop Trauma Surg. 1991;110:151–154. doi: 10.1007/BF00395798. [DOI] [PubMed] [Google Scholar]
- 69.Vahvanen V, Patiala H. Synovectomy of the wrist in rheumatoid arthritis and related diseases: a follow-up study of 97 consecutive cases. Arch Orthop Trauma Surg. 1984;102:230–237. doi: 10.1007/BF00436135. [DOI] [PubMed] [Google Scholar]
- 70.Wakitani S, Imoto K, Saito M, Murata N, Hirooka A, Yoneda M, Ochi T. Evaluation of surgeries for rheumatoid shoulder based on the destruction pattern. J Rheumatol. 1999;26:41–46. [PubMed] [Google Scholar]
- 71.Wilkes LL. Arthroscopic synovectomy in the rheumatoid knee. J Med Assoc Ga. 1985;74:582–583. [PubMed] [Google Scholar]
- 72.Woods DA, Williams JR, Gendi NS, Mowat AG, Burge PD, Carr AJ. Surgery for rheumatoid arthritis of the elbow: a comparison of radial-head excision and synovectomy with total elbow replacement. J Shoulder Elbow Surg. 1999;8:291–295. doi: 10.1016/S1058-2746(99)90147-7. [DOI] [PubMed] [Google Scholar]