Abstract
Background
Mechanical bowel preparation prior to colectomy is controversial for several reasons, including a theoretically increased risk of Clostridium difficile infection.
Objective
To compare the incidence of Clostridium difficile infection among patients who underwent mechanical bowel preparation and those who did not. A secondary objective was to assess the association between Clostridium difficile infection and the use of oral antibiotics.
Design
Observational cohort study.
Setting
The Michigan Surgical Quality Collaborative Colectomy Project (n=24 hospitals) participates in the American College of Surgeons- National Surgical Quality Improvement Program with additional targeted data specific to colectomy patients.
Patients
Adult patients (21 years and older) admitted to participating hospitals for elective colectomy between August 2007 and June 2009.
Main Outcome Measure
Laboratory detection of a positive Clostridium difficile toxin assay or stool culture.
Results
2263 patients underwent colectomy and fulfilled inclusion criteria. 54 developed a Clostridium difficile infection, for a hospital median rate of 2.8% (range 0 to 14.7%). Use of mechanical bowel preparation was not associated with increased incidence of Clostridium difficile infection (p=0.95). Among 1685 patients that received mechanical bowel preparation, 684 (41%) received oral antibiotics. The proportion of patients who were diagnosed with Clostridium difficile infection after using preoperative oral antibiotics was smaller than the proportion of patients with Clostridium difficile infection who did not receive oral antibiotics (1.6% vs. 2.9%, p=0.09).
Limitations
Potential underestimation of Clostridium difficile infection due to the study's strict data collection criteria and risk of undetected infection after postoperative day 30.
Conclusions
In contrast to previous single-center data, this multi-center study showed preoperative use of mechanical bowel preparation was not associated with increased risk of Clostridium difficile infection after colectomy. Moreover, the addition of oral antibiotics with mechanical bowel preparation did not confer any additional risk of infection.
Keywords: Colectomy, Clostridium difficile, Clostridium difficile infection (CDI), mechanical bowel preparation, oral antibiotics prophylaxis
INTRODUCTION
Clostridium difficile may soon exceed methicillin-resistant staphylococcus aureus (MRSA) as the primary cause of hospital-associated infections in the United States.1 The virulence of Clostridium difficile infection (CDI) is escalating, with a national increase in mortality from 5.7 per million population in 1999 to 23.7 per million population in 2004.1-3 The increasing incidence of CDI is a particular burden among surgical patients for several reasons.4-5 Patients undergoing surgical resection are subject to the usual host risk factors including immunosuppression, age, and multiple comorbidities.6 Perhaps most importantly, these patients regularly receive prophylactic antibiotic medication. Accordingly, current efforts to curb CDI have focused on decreasing exposure to the organism and minimizing antimicrobial therapy.6-10
Among surgical patients, those who undergo colectomy are at a unique risk of CDI due to the additional physical disruption of the indigenous colonic microflora.5 Traditionally, bowel preparation with oral antibiotics has been considered a cornerstone of preoperative care for colorectal surgical patients.9 This process includes use of cathartics to rid the intestines of bulk stool along with oral antibiotics to kill residual live bacteria. More recently however the use of mechanical bowel preparation has been implicated as a possible antecedent to CDI due to eradication of the normally protective microflora.11 Therefore, the use of a bowel preparation prior to colectomy has become a topic of debate among traditionalists who cite prolonged experience with bowel preparation and empiricists who cite absence of benefit or even potential harm per randomized trial evidence.7, 9, 11-14
High quality clinical data reflecting realistic patterns of use outside of the carefully controlled setting of a randomized trial or single institutions could help to clarify the risks and benefits of using a mechanical preparation among patients undergoing colectomy. The purpose of our study was to examine the association between use of mechanical bowel preparation and CDI among colectomy patients, using a clinical database that incorporates and supplements the American College of Surgeons- National Surgical Quality Improvement Program (ACS-NSQIP) database. A secondary goal was to assess the association between the incidence of CDI among colectomy patients who received bowel preparation with and without oral antibiotics.
MATERIALS AND METHODS
Patients and data collection
Data were collected as part of The Michigan Surgical Quality Collaborative (MSQC), a program sponsored in part by Blue Cross and Blue Shield of Michigan/ Blue Care Network to measure and improve the quality of care through regional collaboration.15 A coalition of 34 teaching and community hospitals across the state of Michigan are enrolled in the MSQC. The Colectomy Project, a special 24-hospital subset of the larger MSQC initiative, was started in 2007 to better understand best practices in various areas of colon surgery as identified by four Current Procedural Terminology codes(CPT) (open segmental colectomy [44204], laparoscopic segmental colectomy [44140], ileocolic resection [44205], and laparoscopic ileocolic resection[44160]).15
Adult patients (21 years and older) admitted to participating hospitals for colectomy between August 15, 2007 and June 30, 2009 were eligible for the study. Patients undergoing emergent or urgent colectomy were excluded. The patient clinical data were abstracted from patient charts by dedicated Surgical Clinical Reviewers (SCR) who were trained and responsible for extracting the ACS-NSQIP data and 25 additional data elements pertinent to colectomy patients, in accordance with the policies and procedures prescribed for the ACS- NSQIP database.16 Requisite procedure includes a follow-up for surgical complications (including CDI) for 30 days after surgical procedure date via electronic records, paper charts, phone call and/or follow-up letter.17 Institutional Review Board approval was obtained from the University of Michigan Institutional Review Board- Medical (HUM00033887).
Variables
The primary dependent variable was presence of infection with the Clostridium difficile (C. difficile) organism, identified by laboratory detection of the toxin in the stool or by a positive stool culture. Empirical treatment alone or diagnosis without laboratory evidence did not qualify. The primary independent variable was use of mechanical bowel preparation obtained from electronic records and paper charts. Mechanical bowel preparation was defined to include the use of oral cathartics both with and without enemas. Patients who used enemas alone (1.6%) were not included under the definition of mechanical bowel preparation. In a secondary analysis, we tested the association between use of oral antibiotic prophylaxis and CDI.
Statistical Analysis
Independent and dependent variables were analyzed in association with covariates routinely collected by the ACS-NSQIP database and the Colectomy Project (Table 1). Univariate associations were assessed using chi square for categorical variables and the two sample t-test for the continuous measures of age and BMI. The Fisher's exact test was used when the expected frequency of any cell in the contingency table was < 5. Variables that were significant at the 5% level (alpha < 0.05) in the univariate analysis were sequentially incorporated into the model at the multivariate level to assess the association between mechanical bowel preparation and CDI after adjusting for the relevant factors. Analyses were conducted using SPSS software version 18 (Chicago, IL). A p-value ≤ 0.05 was considered statistically significant.
Table 1.
Data elements abstracted per the National Surgical Quality Improvement Program and Michigan Surgical Quality Consortium Colectomy Project*.
| Preoperative Patient Risk Factors |
|---|
| Age |
| BMI |
| Sex |
| Race/ Ethnicity |
| White |
| Other |
| Functional Status |
| Prior to surgery |
| Independent |
| Partially or Totally Dependent |
| Prior to current illness |
| Independent |
| Partially or Totally Dependent |
| ASA |
| 1= No Disturbance |
| 2= Mild Disturbance |
| 3= Severe Disturbance |
| 4= Life Threatening |
| 5= Moribund |
| Pulmonary |
| Dyspnea |
| COPD |
| Current pneumonia |
| Cardiac |
| History of CHF (within 30 days) |
| MI (within 6 months) |
| Cardiac Surgery (previous) |
| Angina (within 30 days) |
| Hypertension |
| Central Nervous System |
| Impaired sensorium |
| CVA (with neurological deficit) |
| TIA |
| CNS Tumor |
| Hepatobiliary |
| Ascites |
| Renal |
| Acute Renal Failure |
| On Dialysis |
| Nutritional/Immune Other |
| Steroid use for chronic condition |
| Weight loss >10% |
| Disseminated cancer |
| Bleeding disorder |
| Transfusion >4 U PRBCs |
| Chemotherapy |
| Radiotherapy |
| Sepsis |
| Surgical Descriptors |
| Prior Operation |
| Type of resection* |
| Ileocolectomy |
| Segmental colectomy |
| Transfer from Healthcare facility |
| Admitted directly from home |
| Acute Care Hospital |
| Chronic Care Facility |
| Other |
| CPT Code |
| 44140 |
| 44160 |
| 44204 |
| 44205 |
| Open vs. closed |
| Anastomosis vs. partial removal |
| Bowel Preparation* |
| Oral Antibiotics with Bowel Preparation* |
| Outcome |
| Clostridium difficile infection (CDI)* |
RESULTS
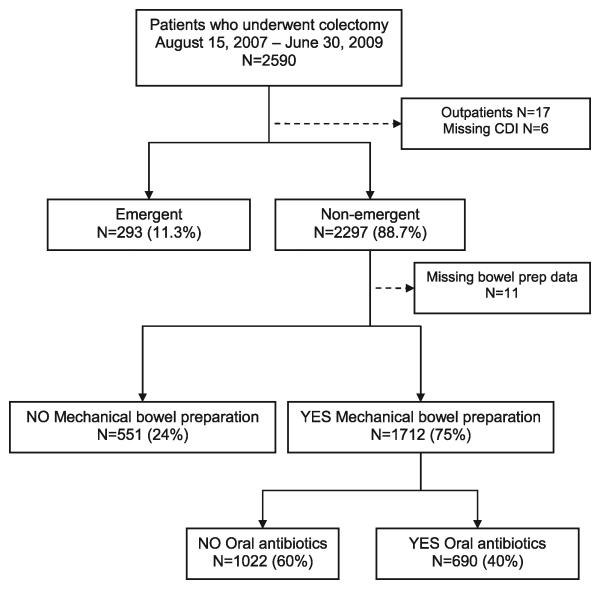
The initial cohort included 2297 colectomy patients who underwent a non-emergent colectomy between August 15, 2007 and June 30, 2009. Seventeen patients were excluded because they did not require postoperative hospitalization and another 17 patients were excluded due to missing data (6 missing CDI and 11 missing mechanical bowel preparation) for a final total of 2263 inpatient colectomy patients (Figure 1).
Figure 1.
Colectomy patient cohort.
Among the entire cohort, 74% of patients underwent a preoperative mechanical bowel preparation. Patients who did and did not undergo mechanical bowel preparation differed in several ways (Table 2). Most notably, those who underwent a mechanical bowel preparation were more likely to be functionally independent and to have a lower (i.e., healthier) American Society of Anesthesiologists (ASA) score. As a reflection of these variables, patients who underwent bowel preparation were less likely to have comorbid disease including cardiovascular, renal, or bleeding disorders or pre-operative “sepsis”.
Table 2.
Patient characteristics and use of mechanical bowel preparation prior to colectomy.
| Variable | Bowel Preparation N=1685 (74%) |
No Bowel Preparation N=578 (25%) |
p-value |
|---|---|---|---|
| Age | 65.61 +/− 14.54 | 64.84 +/− 17.05 | .33 |
| Body mass index | 28.36 +/− 6.31 | 27.35 +/− 5.83 | .001 |
| Sex | .11 | ||
| Male | 836 (49.6) | 264 (45.7) | |
| Female | 849 (50.4) | 314 (54.3) | |
| Race/ Ethnicity | .13 | ||
| White | 1259 (74.7) | 449 (77.8) | |
| Other | 426 (25.3) | 128 (22.2) | |
| Preoperative functional status | <.001 | ||
| Independent | 1603 (95.1) | 513 (88.8) | |
| Dependent | 82 (4.9) | 65 (11.2) | |
| Type of Resection | <.001 | ||
| segmental | 1157 (68.7) | 324 (56.1) | |
| ileocolic | 528 (31.3) | 254 (43.9) | |
| ASA | <.001 | ||
| 1= No Disturbance | 27 (1.6) | 11 (1.9) | |
| 2= Mild Disturbance | 860 (51.0) | 256 (44.3) | |
| 3= Severe Disturbance | 723 (42.9) | 262 (45.3) | |
| 4= Life Threatening | 74 (4.4) | 45 (7.8) | |
| 5= Moribund | 1 (0.1) | 4 (0.7) | |
| Dyspnea | 1425 (84.6) | 478 (82.7) | .29 |
| Chronic obstructive pulmonary disease | 101 (6.0) | 40 (6.9) | .43 |
| Pneumonia | 6 (0.4) | 2 (0.3) | 1.0a |
| Congestive heart failure | 16 (0.9) | 20 (3.5) | <.001 |
| History of myocardial infarction | 15 (0.9) | 12 (2.1) | .02 |
| Acute Renal Failure | 1 (0.1) | 6 (1.0) | .001a |
| Dialysis | 11 (0.7) | 7 (1.2) | .19a |
| Steroid Use | 57 (3.4) | 36 (6.2) | <.01 |
| Malnourished (>10% Loss of body weight) | 61 (3.6) | 28 (4.8) | .19 |
| Disseminated Cancer | 52 (3.1) | 26 (4.5) | .11 |
| Bleeding Disorder | 72 (4.3) | 47 (8.1) | <.001 |
| Transfusions | 4 (0.2) | 9 (1.6) | .001a |
| Sepsis | 60 (3.6) | 88 (15.2) | <.001 |
| Transfer from another healthcare facility | .01 | ||
| No (Admitted from home) | 1661 (98.6) | 560 (96.9) | |
| Transferred from an acute care hospital | 9 (0.5) | 9 (1.6) | |
| Transferred from a chronic care facility | 14 (0.8) | 6 (1.0) | |
| Other | 1 (0.1) | 3 (0.5) |
Fisher exact test; parentheses denote column percentages
Forty one percent of patients who underwent a mechanical bowel preparation also used preoperative oral antibiotics (Table 3). Patients who used oral antibiotics were more likely to be white, male, report less use of steroids (2.3% vs. 4.1%, p=.05), and preoperative incidence of sepsis (2.2% vs 4.5%, p=.01) than those who did not use oral antibiotics. In both comparisons (Tables 2 and 3), patients with ileocolic resections were less likely than patients who underwent a segmental colectomy to use a mechanical bowel preparation and less likely to use oral antibiotics in conjunction with the prescribed mechanical bowel preparation.
Table 3.
Patient characteristics and use of oral antibiotics among patients who underwent mechanical bowel preparation prior to colectomy.
| Variable | Bowel preparation with oral antibiotics, N = 684 (%) |
Bowel preparation without oral antibiotics, N = 1001(%) |
p- value |
|---|---|---|---|
| Age | 65.1 +/− 13.9 | 65.9 +/− 14.9 | .20 |
| Body mass index | 28.7 +/− 6.41 | 28.1 +/−6.2 | .05 |
| Sex | .04 | ||
| Male | 360 (52.6) | 476 (47.6) | |
| Female | 324 (47.4) | 525 (52.4) | |
| Race/ Ethnicity | <.001 | ||
| White | 563 (82.3) | 696 (69.5) | |
| Other | 121 (17.7) | 305 (30.5) | |
| Preoperative functional status | .09 | ||
| Independent | 600 (95.1) | 945 (94.4) | |
| Dependent | 84 (4.9) | 56 (5.6) | |
| Type of Resection | <.001 | ||
| segmental | 534 (78.1) | 623 (62.2) | |
| ileocolic | 150 (21.9) | 378 (37.8) | |
| ASA | .66a | ||
| 1= No Disturbance | 8 (1.2) | 19 (1.8) | |
| 2= Mild Disturbance | 349 (51.0) | 511 (51.0) | |
| 3= Severe Disturbance | 299 (43.7) | 434 (42.4) | |
| 4= Life Threatening | 28 (4.1) | 46 (4.6) | |
| 5= Moribund | 0 (0.0) | 1 (0.1) | |
| Dyspnea (moderate or at rest) | 111 (16.2) | 149 (14.9) | .45 |
| Chronic obstructive pulmonary disease | 41 (6.0) | 60 (6.9) | 1.0 |
| Pneumonia | 5 (0.7) | 1 (0.1) | .04a |
| Congestive heart failure | 4 (0.6) | 12 (1.2) | .22 |
| History of myocardial infarction | 8 (1.2) | 7 (0.7) | .31 |
| Acute renal failure | 0 (0.0) | 1 (0.1) | 1.0a |
| Dialysis | 7 (1.0) | 4 (0.4) | .13a |
| Steroid Use | 16 (2.3) | 41 (4.1) | .05 |
| Malnutrition (>10% l oss of body weight) | 18 (2.6) | 43 (4.3) | .07 |
| Disseminated cancer | 17 (2.5) | 35 (3.5) | .24 |
| Bleeding Disorder | 28 (4.1) | 44 (4.4) | .77 |
| Transfusions | 1 (1.1) | 3 (0.3) | .65a |
| Sepsis | 15 (2.2) | 45 (4.5) | .01 |
| Transfer from another healthcare facility | .36a | ||
| Admitted directly from home | 674 (98.5) | 987 (98.6) | |
| Transferred from an acute care hospital | 2 (0.3) | 7 (0.7) | |
| Transferred from a chronic care facility | 7 (1.0) | 7 (0.7) | |
| Other | 1 (0.1) | 0 (0.0) |
Fisher's exact test; parentheses denote column percentages
The hospital median rate of CDI was 2.8%, ranging from 0 to 14.7%. In the full cohort, 54 patients (2.4%) were diagnosed with CDI based on a positive C. difficile diagnostic laboratory result postoperatively. Among patients who had a bowel preparation, 40/1685 (2.4%) were diagnosed with CDI (Table 4). Among patients who had no bowel preparation, 14/578 (2.4%) were diagnosed with a CDI. In unadjusted analysis, use of a mechanical bowel preparation was not associated with a higher risk of CDI than absence of a mechanical bowel preparation (p=0.95). Among patients who underwent a mechanic bowel preparation, use of preoperative oral antibiotics showed a trend toward lower rates of CDI than omission of oral antibiotics, although this was not statistically significant (1.6% vs. 2.9%, p=.09). We performed a univariate analysis to identify other factors associated with CDI. After adjusting for variables that were statistically significant in the univariate analysis, multiple logistic regression revealed no association between the use of mechanical bowel preparation and CDI and no statistically significant association between the use of prophylactic oral antibiotics and CDI (Table 5).
Table 4.
The use of mechanical bowel preparation and Clostridium difficile infection at the patient level*.
| C. difficile infection | No C. difficile infection | p-value | |
|---|---|---|---|
| No Bowel Preparation, n=578 | 14 (2.4%) | 564 (97.6%) | 0.95 |
| Yes Bowel Preparation, n=1685 | 40 (2.4%) | 1645 (97.6%) | |
| Without Oral antibiotics, n=1001 | 29 (2.9%) | 972 (97.1%) | 0.09 |
| With Oral antibiotics, n=684 | 11 (1.6%) | 673 (98.4%) |
Hospital median rate of mechanical bowel infection=2.8%, range = 0-14.7%.
Table 5.
The use of mechanical bowel preparation and Clostridium difficile infection after colectomy.
| Variable | Unadjusted Odds Ratio, (95% confidence interval [CI]) |
Adjusted** Odds Ratio (95% CI) |
|---|---|---|
| No mechanical bowel preparation | Reference | --- |
| Yes mechanical bowel preparation | OR=0.98 (0.53-1.81) | OR=0.96 (0.50- 1.83) |
| Without oral antibiotics* | Reference | --- |
| With oral antibiotics* | OR=0.55 (0.27-1.10) | OR=0.60 (0.29-1.23) |
Cohort that used mechanical bowel preparation
Adjusted for characteristics that achieved p<0.05 association in univariate analyses.
Among full cohort: body mass index, preoperative functional status, type of resection, ASA status, congestive heart failure, history of myocardial infarction, acute renal failure, steroid use, bleeding disorder, transfusions, sepsis and transfer from healthcare facility.
Among those who used a mechanical bowel preparation: body mass index, sex, race, type of resection, pneumonia, steroid use and sepsis.
DISCUSSION
This study of 2263 colectomy patients from 24 hospitals does not show an association between the use of mechanical bowel preparation and postoperative CDI. Overall, a hospital median rate of 2.8% of patients (range= 0-14.7%) were diagnosed with CDI based on a positive C. difficile diagnostic laboratory result postoperatively. We did identify a trend toward fewer CDIs among patients who used oral antibiotics with their bowel preparations compared with those who did not.
The findings of this multicenter study contradict an earlier single-center study,11 and add to the controversy about mechanical bowel preparation and CDI risk.11, 18-21 Therefore, it is important to note the differences between patients in our cohort who received a bowel preparation and those who did not. We found that healthier patients (lower ASA score, functionally independent and fewer comorbidities) were more likely to undergo mechanical bowel preparation. We conducted additional post-hoc analyses adjusting for previously described risk factors for CDI, including renal disease and sepsis,22 Both renal disease (0.1% vs. 1%; p=0.001) and sepsis (3.6% vs. 15.2%; p< 0.001) were reported at a higher rate among patients that did not undergo bowel preparation. Binary logistic regression revealed no significant association between the CDI and renal disease (p=.08, [95% CI, 0.81- 61.67]) or sepsis (p=0.38, [95% CI, 0.12 -2.23]) among patients that used or did not use a bowel preparation. It is possible that future research will further clarify these potential associations. However, our dataset covers most of the state of Michigan and was built on and designed to be even more comprehensive (eg, oversampling colectomy cases, capturing use of bowel preparation, capturing laboratory designated CDI) than the ACS NSQIP, which is widely regarded as the highest quality large-scale (non-cancer) clinical dataset available. It is unlikely that an adequate number of cases could be captured in a future effort, except by a well-funded randomized controlled trial specifically designed to evaluate the use of mechanical bowel preparation.
Investigation of the association between bowel preparation and CDI is particularly timely because the national incidence of CDI has more than doubled in the past decade.1, 3 Currently, the CDI-associated mortality rate has increased by approximately 4-fold in the United States, primarily associated with the hypervirulent strain identified as NAP1/BI/027 toxinotype III.2, 23-25 Moreover, the financial burden of CDI is estimated to exceed $3 billion dollars a year,26 not including the indirect costs of infection such as complications of treatment and time away from work and family.
The new NAP 1 strain of C. difficile is unlikely to have caused this epidemic based on virulence alone.27 Antibiotic therapy, antimicrobial resistance, and the increased use of gastric acid suppression have also been cited as potential contributing factors.27 In addition, recent data suggest that the risk of CDI is increasing at a particularly rapid rate among surgical patients—an increase that has been most pronounced among those who undergo colectomy compared to other common inpatient procedures.5 These findings may be a consequence of host risk factors such as immunosuppression, age and multiple comorbidities,6 or alternatively the result of exposure to prophylactic perioperative antibiotics,4, 28 or finally due to the physical disruption of indigenous colonic microflora.5
In a single center study,11 investigators demonstrated a higher rate of Clostridium difficile colitis when oral antibiotics were added to a mechanical bowel preparation regimen. It is plausible that the combined physical and chemical disruption of colonic microflora during the use of mechanical bowel preparation with oral antibiotics results in additive risk. However, the findings of our current multi-center study refute this hypothesis; patients who underwent bowel preparation before a colectomy had exactly the same rates of post-operative CDI as those who did not. While the median hospital rate of CDI was lower in our cohort than the hospital rate in the single center study (2.8% vs. 4.2%), the total number of patients was seven-fold greater (2274 vs. 304 patients) and included 24 hospitals, which supports the greater generalizability of our findings.
The data associating mechanical bowel preparation with adverse outcomes including CDI11, 18-21 have not been sufficient to transform clinical practice. As recently as 2003, the American Society of Colon and Rectal Surgeons(ASCRS) estimated that 99% of members prescribed some type of mechanical bowel preparation and 75% used oral antibiotic prophylaxis as part of their standard preoperative protocol for elective colorectal surgery.9 Advocates of bowel preparation cite intra-operative benefits such as improved handling of the bowel, better ability to palpate lesions, and reduced operative time 29 and reduced postoperative surgical site infections.7, 12, 30
By contrast, proponents of abandoning preoperative bowel preparation cite a higher rates of anastomotic dehiscence18, 21 and infectious complications (sepsis, surgical site infections, peritonitis).13, 18, 20, 31 An updated meta-analysis concluded that the practice should be stopped altogether.19 Further fueling the debate around the compulsory practice is the additional patient discomfort,6, 18 potential for dehydration,20 and an undercurrent of a concern about an increasingly product-driven practice.32 Several have suggested that a poorly executed bowel preparation regimen can actually place patients at greater risk since liquefied stool remaining in the bowel can more easily be introduced into the peritoneal cavity during surgery.6-7, 30 Most recently, a high-quality randomized controlled trial of mechanical bowel preparation showed equivalency in terms of surgical site infection (SSI) and anastomotic leakage, but more intra-abdominal abscesses amongst patients without mechanical bowel preparation.21 While investigators concluded that it was safe to abandon mechanical bowel preparation, proponents of mechanical bowel preparation felt that this study justified its continued use. Thus, the debate about mechanical bowel preparation in the United States persists. Given that this practice is still the standard of care in the U.S., studies that strive to define and delineate the risks of mechanical bowel preparation are increasingly important.
Our study is subject to several limitations many of which are inherent to the limitations of conducting a retrospective analysis and the constraints of the MSQC/ACS NSQIP dataset. First, we used a rigorous criterion for CDI diagnosis and it is likely that some patients were treated empirically without testing a C. difficile toxin assay or culture. However, this represents normal practice, during which a certain proportion of CDI will be empirically treated and a certain proportion will be under-diagnosed. Second, although the sampling protocol of the ACS-NSQIP is designed to minimize selection bias, it is still possible that some selection bias may have been introduced by not including every case from every hospital. In an effort to mitigate this limitation, the Colectomy Project is designed to oversample colectomy cases specifically. In addition, all cases were elective and we have no reason to believe that any missed elective cases differed from recorded cases in the likelihood of use of a bowel preparation. Third, some patients may have been lost to follow-up or seen subsequently outside of the collaborative hospitals. However, the size of our collaborative (24 hospitals within the region) and reliance on chart ascertainment and 30-day follow-up with chart review, letters, and telephone calls by trained and dedicated SCR's, rather than discharge diagnoses, reduces the risk of missed post-operative CDIs. Lastly, our dataset did not include the use of prophylactic antibiotics at the time of surgery and through the postoperative course. While it is likely that providers engaged in the usual practice of prophylactic antibiotic use before an elective colectomy (all cases in this cohort were elective) and post-operative cessation of antibiotics in compliance with Surgical Care Improvement Project (SCIP) measures, it is not possible to confirm that in this multi-institutional study.
In summary, our multi-center study of colectomy patients showed that use of a mechanical bowel preparation was irrelevant to post-operative CDI. While abandoning the time-honored practice of bowel preparation prior to colectomy could reduce cost, workload, the distress and discomfort of the patient, it is unlikely to reduce the rate of CDI. Our data indicate abandoning mechanical bowel preparation (both with and without oral antibiotics) in order to reduce the risk of CDI is premature and will require additional empiric evidence before clinical practice changes can be implemented.
Acknowledgments
Sources of Support:
This research is supported by an F31NR011548 grant from the National Institute of Nursing Research. The Michigan Surgical Quality Collaborative (ww.msqc.org) is supported through funding from Blue Cross and Blue Shield of Michigan/ Blue Care Network. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute Of Nursing Research, the National Institutes of Health, the Michigan Surgical Quality Collaborative, or Blue Care Network.
Footnotes
Disclosures: None
Author contributions:
Krapohl: conception and design; data acquisition; data analysis and interpretation; primary author of manuscript; final approval of manuscript.
Phillips: conception and design, data acquisition; critical revision of manuscript content; final approval of manuscript.
Campbell: data acquisition; critical revision of manuscript content; final approval of manuscript.
Hendren: data analysis and interpretation; critical revision of manuscript content; final approval of manuscript.
Banerjee: data analysis and interpretation; critical revision of manuscript content; final approval of manuscript.
Metzger: conception and design, data analysis and interpretation; critical revision of manuscript content; final approval of manuscript.
Morris: conception and design, data analysis and interpretation; critical revision of manuscript content; final approval of manuscript
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.McDonald LC, Owings M, Jernigan D. Clostridium difficile infection in patients discharged from U.S. short stay hospitals, 1996-2003. Emerging Infectious Diseases. 2006;34:346–353. doi: 10.3201/eid1203.051064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Redelings MD, Sorvillo F, Mascola L. Increase in Clostridium difficile-related mortality rates, United States, 1999-2004. Emerging Infectious Diseases. 2007;13(9):1419–1417. doi: 10.3201/eid1309.061116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ricciardi R, Rothenberger DA, Madoff RD, Baxter NN. Increasing prevalence and severity of Clostridium difficile colitis in hospitalized patients in the United States. Arch Surg. 2007 Jul;142(7):624–631. doi: 10.1001/archsurg.142.7.624. discussion 631. [DOI] [PubMed] [Google Scholar]
- 4.Morris AM, Jobe BA, Stoney M, Sheppard BC, Deveney CW, Deveney KE. Clostridium difficile colitis: an increasingly aggressive iatrogenic disease? Arch Surg. 2002 Oct;137(10):1096–1100. doi: 10.1001/archsurg.137.10.1096. [DOI] [PubMed] [Google Scholar]
- 5.Zerey M, Paton B, Lincourt A, et al. The Burden of Clostridium difficile in Surgical Patients in the United States. Surgical Infections. 2007;8(6):57–566. doi: 10.1089/sur.2006.062. [DOI] [PubMed] [Google Scholar]
- 6.Wilkins K. Perioperative Management. 2005 http://www.fascrs.org/physicians/education/core_subjects/2005/perioperative_management/. Accessed December 7, 2009, 2009.
- 7.Fry DE. Preventive Systemic Antibiotics in Colorectal Surgery. Surgical Infections. 2008;9(6):547–552. doi: 10.1089/sur.2008.9956. [DOI] [PubMed] [Google Scholar]
- 8.Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Am J Surg. 2005;189(4):395–404. doi: 10.1016/j.amjsurg.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 9.Zmora O, Wexner SD, Hajjar L, et al. Trends in preparation for colorectal surgery: survey of the members of the American Society of Colon and Rectal Surgeons. Am Surg. 2003;69(2):150–154. [PubMed] [Google Scholar]
- 10.Song F, Glenny AM. Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomized controlled trials. Br J Surg. 1998;85(9):1232–1241. doi: 10.1046/j.1365-2168.1998.00883.x. [DOI] [PubMed] [Google Scholar]
- 11.Wren SM, Ahmed N, Jamal A, Safadi BY. Preoperative Oral Antibiotics in Colorectal Surgery Increase the Rate of Clostridium difficile Colitis. Archives of Surgery. 2005;140(8):752–756. doi: 10.1001/archsurg.140.8.752. [DOI] [PubMed] [Google Scholar]
- 12.Lewis RT. Oral versus systemic antibiotic prophylaxis in elective colon surgery: a randomized study and meta-analysis send a message from the 1990s. Can J Surg. 2002;45(3):173–180. [PMC free article] [PubMed] [Google Scholar]
- 13.Espin-Basany E, Sanchez-Garcia JL, Lopez-Cano M, et al. Prospective, randomised study on antibiotic prophylaxis in colorectal surgery. Is it really necessary to use oral antibiotics? Int J Colorectal Dis. 2005;20(6):542–546. doi: 10.1007/s00384-004-0736-8. [DOI] [PubMed] [Google Scholar]
- 14.Walz JM, Paterson CA, Seligowski JM, Heard SO. Surgical Site Infection Following Bowel Surgery: A Retrospective Analysis of 1446 Patients. 2006 October 1;141(10):1014–1018. doi: 10.1001/archsurg.141.10.1014. 2006. [DOI] [PubMed] [Google Scholar]
- 15.Michigan Surgical Quality Collaborative Michigan Surgical Quality Collaborative: Building Realtionships… Improving Outcomes…. Future Solutions Now. 2009 https://www.msqc.org/Public/index.aspx. Accessed March 10, 2009, 2009.
- 16.American College of Surgeons National Surgical Quality Improvement Program Program Specifics: ACS NSQIP Data Collection Overview. 2006 http://www.acsnsqip.org/main/programspecs/program_data_collection.jsp. Accessed December 10 2010.
- 17.American College of Surgeons National Surgical Quality Improvement Program The Data Collection Process. ACS NSQIP Operations Manual. 2009 April 1;:ed2009. [Google Scholar]
- 18.Slim K, Vicaut E, Launay-Savary MV, Contant C, Chipponi J. Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery. Ann Surg. 2009;249(2):203–209. doi: 10.1097/SLA.0b013e318193425a. [DOI] [PubMed] [Google Scholar]
- 19.Guenaga KF, Matos D, Castro AA, Atallah AN, Wille-Jorgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev. 2005;(1):CD001544. doi: 10.1002/14651858.CD001544.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Howard DD, White CQ, Harden TR, Ellis CN. Incidence of surgical site infections postcolorectal resections without preoperative mechanical or antibiotic bowel preparation. Am Surg. 2009;75(8):659–663. discussion 663-654. [PubMed] [Google Scholar]
- 21.Contant CM, Hop WC, van't Sant HP, et al. Mechanical bowel preparation for elective colorectal surgery: a multicentre randomised trial. Lancet. 2007;370(9605):2112–2117. doi: 10.1016/S0140-6736(07)61905-9. [DOI] [PubMed] [Google Scholar]
- 22.Eddi R, Malik MN, Shakov R, Baddoura WJ, Chandran C, Debari VA. Chronic kidney disease as a risk factor for Clostridium difficile infection. Nephrology. 2010;15(4):471–475. doi: 10.1111/j.1440-1797.2009.01274.x. [DOI] [PubMed] [Google Scholar]
- 23.Kelly CP. A 76-year-old man with recurrent Clostridium difficile-associated diarrhea: review of C. difficile infection. Journal of the American Medical Association. 2009;301(1):954–962. doi: 10.1001/jama.2009.171. [DOI] [PubMed] [Google Scholar]
- 24.McDonald LC, Killgore GE, Thompson A, et al. An Epidemic, Toxin Gene-Variant Strain of Clostridium difficile. The New England Journal of Medicine. 2005;353(23):2433–2441. doi: 10.1056/NEJMoa051590. [DOI] [PubMed] [Google Scholar]
- 25.McDonald LC. The changing epidemiology of Clostridium difficile; Clostridium difficile: Changing daignosis, epidemiology and treatment (satellite Symposium during the 18th Annual SHEA Scientific Meeting); Orlando, Florida: Robert Michael Educational Institute LLC and Postgraduate Institute for Medicine; 2008. [Google Scholar]
- 26.Dubberke ER, Gerding DN, Classen D, et al. Strategies to Prevent Clostridium difficile Infections in Acute Care Hospitals. Infection Control and Hospital Epidemiology. 2008;29(s1):S81–S92. doi: 10.1086/591065. [DOI] [PubMed] [Google Scholar]
- 27.Blossom DB, McDonald LC. Emerging Infections: The Challenges Posed by Reemerging Clostridium difficile Infection. Clin Infect Dis. 2007;45(2):222–227. doi: 10.1086/518874. [DOI] [PubMed] [Google Scholar]
- 28.Itani KM, Wilson SE, Awad SS, Jensen EH, Finn TS, Abramson MA. Ertapenem versus cefotetan prophylaxis in elective colorectal surgery. N Engl J Med. 2006;355(25):2640–2651. doi: 10.1056/NEJMoa054408. [DOI] [PubMed] [Google Scholar]
- 29.Rovera F, Dionigi G, Boni L, et al. Mechanical bowel preparation for colorectal surgery. Surg Infect (Larchmt) 2006;7(Suppl 2):S61–63. doi: 10.1089/sur.2006.7.s2-61. [DOI] [PubMed] [Google Scholar]
- 30.Hayashi MS, Wilson SE. Is there a current role for preoperative non-absorbable oral antimicrobial agents for prophylaxis of infection after colorectal surgery? Surg Infect (Larchmt) 2009;10(3):285–288. doi: 10.1089/sur.2008.9958. [DOI] [PubMed] [Google Scholar]
- 31.Englesbe M, Brooks L, Kubus J, et al. A statewide assessment of surgical site infection following colectomy: The role of oral antibiotics. Annals of Surgery. 2010;252(3):514–520. doi: 10.1097/SLA.0b013e3181f244f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cosman B. Perioperative Management. 2000 http://www.fascrs.org/physicians/education/core_subjects/2000/perioperative_management/. Accessed December 7, 2009.