Abstract
Objectives
To estimate trends in the prevalence of fatigue among elders living in public housing or in the community; to compare health status of elders living in public housing to their community-dwelling counterparts.
Design
Cross-sectional study.
Setting
Community-dwelling elders who reported ever residing in public housing were compared to those living in other community settings.
Participants
Participants of the Health and Retirement Study (seven waves of interviews conducted from 1995 through 2006) interviewed in 2006 with complete data on housing status, self-report measures of health status and measures of functioning (n=16,191).
Measurements
Self-reported fatigue, functioning, and other health conditions. We also evaluated four functional indices: overall mobility, large muscle functioning, gross motor functioning, and fine motor functioning.
Results
Those reporting having lived in public housing were twice as likely to rate their health as fair or poor relative to those with no public housing experience (57.3% vs 26.9%, respectively). Cardiac conditions, stroke, hypertension, diabetes, arthritis and psychiatric problems were all more prevalent in those living in public housing relative to community-dwelling elders not living in public housing. Fatigue was more prevalent in persons residing in public housing (26.7%) as compared to other community-dwelling elders (17.8%).
Conclusion
The health status of persons residing in public housing is poor. Fatigue and comorbid conditions are highly prevalent and more common in those living in public housing. Developing care models that meet the needs of this oft-neglected population is warranted.
Keywords: Elderly, Public Housing, Fatigue
INTRODUCTION
Nearly 2 million older persons reside in publicly subsidized rental housing.1 With average reported income of applicants being $10,000, individuals seeking residence in public housing are among the poorest in the United States.2 Despite this, little is known about individual health factors likely to affect the trajectory of disability of older persons residing in these settings over time.3 In general, the clinical goals for older persons include minimizing symptom burden to improve the daily living experience and quality of life.4 Recognizing symptom burden and its relation to health status factors is one of the missing links to understanding the needs of this population. To our knowledge, no studies have described the prevalence of important symptoms such as fatigue in this population. With up to 50% in outpatient settings presenting with the complaint,5 fatigue has clearly been shown to predict limitations in physical activity, the development and progression of disability, the development of frailty 6 and mortality. 7
Using a nationally representative sample of US adults aged >50 years, we sought: 1) to estimate trends of fatigue among community-dwelling elders stratified by type of residence and ethnicity; and 2) to characterize this population with respect to health status and co-morbid conditions. The operating hypothesis was that elders living in public housing would have poorer health, more chronic illness and greater fatigue than older persons not in public housing. Currently, 3.4 million of the 35 million elders in the United States live in poverty and are eligible for housing assistance programs.8 Thus, the overarching goal of this study was to provide a much-needed description of the health status and symptom burden of the nation’s most poor and at-risk older individuals.
METHODS
The Health and Retirement Study (HRS) was approved by the Institutional Review Board at the University of Michigan and all respondents provided informed consent.
Sample
The HRS is a nationally-representative prospective study of US adults aged >50. Respondents are interviewed on a biennial basis, and the sample is periodically refreshed with younger cohorts to keep the sample representative of the current US population. Details of the sample and study design have been described previously.9,10 The present analysis uses data from seven waves of interviews conducted from 1995 through 2006 and includes respondents who were originally interviewed as part of Study of Assets and Health Dynamics Among the Oldest Old (AHEAD) in 1995 prior to the joining of this survey with the HRS (these respondents are grouped with the HRS respondents from 1996, described below). In the 2006 wave 18,469 adults were interviewed and the sample was 58.9% female, 74.5% White, 13.9% Black and 9.3% Latino with an average age of 68 years. We included HRS respondents interviewed in 2006 who had complete data on housing status, self-report measures of health status and measures of functioning. Respondents interviewed by proxy were excluded (N=1,260). The final sample size was 16,191.
Measures
Fatigue, functioning, and other health conditions were measured by self-report. Respondents were asked about several health problems under a common stem item: “Since we last talked to you, have you had any of the following persistent or troublesome problems…severe fatigue or exhaustion?” Other health conditions respondents under the common stem “Has a doctor ever told you that you have [condition].” History of hypertension, diabetes, cancer, heart disease, stroke, arthritis, psychiatric conditions, and incontinence were assessed in this manner. Functional impairment was assessed by 14 items that assessed activities of daily living and mobility, including difficulty getting out of bed, bathing, eating, walking short and long distances, sitting, getting up from a seated position, climbing stairs, stooping, and lifting and moving objects. Each item was categorized on a two point scale, has no difficulty (coded 0) or has some difficult or cannot do (coded 1). These individual items were summed to generate four functional indices: overall mobility (range: 0–5), large muscle functioning (range: 0–4), gross motor functioning (range: 0–5), and fine motor functioning (range: 0–3).11
Respondents were asked about their housing status at each wave from 1995 to 2006, however, if respondents did not move residences between waves this information was carried forward to the next wave and they were not asked details about their housing. As a result, it was necessary to use all housing data from 1995 to 2006 (seven interview waves) to determine whether a respondent had ever lived in subsidized housing. Subsidized housing residence was determined by the item “Is your (house or apartment) part of a public or subsidized housing complex?” Although the exact wording of this item varied somewhat over the waves, it always included the term “subsidized housing.” A dichotomous variable was created to indicate whether a respondent had ever lived in subsidized housing in any wave, 1995 through 2006. Sociodemographic characteristics including age, sex, ethnicity, educational attainment and net worth were also assessed.
Analysis
The demographic, health, and functioning characteristics of adults who had ever lived in subsidized housing were compared to those who had never lived in subsidized housing using chi-squared tests for categorical variables and Students t tests for continuous variables. We estimated the point prevalence of severe fatigue at three times over the study period: 1995/6, 2000 and 2004. For the majority of respondents, the item on severe fatigue was only assessed during these three waves: 1995 (for the AHEAD sample) or 1996 (for the initial HRS sample), 2000 (full, combined sample) and 2004 (full, combined sample). However, respondents were asked the fatigue item during their initial interview even if it was not during one of these four years (eg, a respondent entered the sample in 2002 [an off-year for the fatigue measure] due to marrying a current HRS participant). These instances represented a minority of the fatigue measures. However, to account for these responses in the prevalence estimates, we combined the data from the off-years with the most recent year that it was asked in the general sample (responses from 1998 [26.9% of responses] were combined with 1995 [16.1%] and 1996 [57.0%]; responses from 2002 [1.3%] were combined with 2000 [98.7%]; and responses from 2006 [1.1%] were combined with 2004 [98.1%]. The denominator for each of the three point prevalence estimates was the number of unique observations for the years combined for that point (that is, no respondent was counted twice in the denominator). We estimated the point prevalence of severe fatigue at these three times stratified by whether respondents had ever lived in subsidized housing or not, and also separately for Whites, Blacks and Hispanics within each of the two housing strata. As described above, we restricted the sample to respondents who were interviewed in 2006, and subsequently we used the 2006 survey weights to adjust these point prevalence estimates for attrition and the sampling design.
RESULTS
Table 1 shows the distribution of sociodemographic and self-reported health conditions by the public housing indicator. On average, participants reporting ever living in public housing were 6 years older than those who never lived in public housing. About 3/4 of the public housing group were women, compared to 59% in those who had never living in public housing. The distribution of ethnicity varied dramatically by public housing history with the majority of persons reporting living in public housing being minorities (public housing: 38.4% Black; 16.2% Hispanic vs no history of living in public housing: 13.0% Black; 8.9% Hispanic). Vast differences in net worth and educational attainment by public housing history are evident. Those reporting having lived in public housing between 1995 and 2006 were twice as likely to rate their health as fair or poor relative to those with no public housing experience (57.3% vs 26.9%, respectively). While prevalence of cancer, fall history, and incontinence were somewhat similar across the housing categories, the prevalence of psychiatric problems and stroke were double in the public housing group compared to those who did not report living in public housing. Cardiac conditions, hypertension, diabetes, and arthritis were all more prevalent in those living in public housing relative to community-dwelling elders not living in public housing. Reports of pain were more common in persons living in public housing (29% in 2006) relative to persons not in public housing (17% in 2006).
Table 1.
Characteristics of Health and Retirement Study participants by history of living in public housing
| Reported living in subsidized housing (1995–2006) | ||
|---|---|---|
| Yes n=567 | No n=15,615 | |
| Age, years ± SD | 73.3 ± 10.3 | 67.4 ± 10.8 |
| Ethnicity | % | |
| Black, Non-Latino | 38.4 | 13.0 |
| Latino | 16.2 | 8.9 |
| White, Non-Latino | 45.5 | 78.1 |
| Women | 76.6 | 59.2 |
| Education ≤high school | 83.9 | 55.7 |
| Median net worth, mean | $500 | $218,000 |
| Self-rated health poor/fair | 57.3 | 26.9 |
| Self-reported conditions | ||
| Hypertension | 75.2 | 56.7 |
| Diabetes | 32.6 | 19.4 |
| Heart conditions | 37.5 | 25.1 |
| Stroke | 14.4 | 7.8 |
| Cancer | 16.2 | 14.8 |
| Arthritis | 78.5 | 60.9 |
| Psychiatric problems | 32.8 | 17.0 |
| Incontinence | 25.7 | 21.1 |
| Fallen in past 2 years | 38.7 | 31.9 |
The sociodemographic and chronic conditions of participants are shown stratified by ethnicity and public housing status in Table 2. Within each ethnic stratification, persons reporting having lived in public housing between 1995 and 2006 had less net worth, less educational attainment, and were more likely to rate their health as fair or poor relative to community-dwelling elders with no history of living in public housing. In each of the ethnic groups, the prevalence of psychiatric problems, arthritis, diabetes, heart conditions, and hypertension was far greater in persons with a history of living in public housing than those who did not. Regardless of public housing history, incontinence was less frequently reported by Blacks and Latinos relative to non-Latino White respondents.
Table 2.
Characteristics of participants stratified by ethnicity and history of living in public housing
| Black | Latino | White | ||||
|---|---|---|---|---|---|---|
| Public housing | Public housing | Public housing | ||||
| Yes (n=221) | No (n=2,027) | Yes (n=93) | No (n=1,391) | Yes (n=262) | No (n=12,197) | |
| Age, year ± SD | 70.9 ± 9.8 | 65.5 ± 10.4 | 73.2 ± 11.1 | 63.9 ± 10.7 | 75.3 ± 9.9 | 68.1 ± 10.8 |
| % | ||||||
| Women | 79.2 | 62.2 | 69.9 | 62.0 | 76.7 | 58.1 |
| Education ≤high school | 85.5 | 64.4 | 92.5 | 78.1 | 79.4 | 51.6 |
| Median net worth | $1 | $58,000 | $20 | $70,000 | $2000 | $285,000 |
| Self-rated health poor/fair | 57.0 | 37.1 | 73.1 | 48.3 | 51.9 | 22.8 |
| Hypertension | 83.7 | 71.7 | 72.0 | 54.9 | 69.1 | 54.4 |
| Diabetes | 38.9 | 28.8 | 45.2 | 28.0 | 22.9 | 16.9 |
| Heart conditions | 35.8 | 22.5 | 28.0 | 16.1 | 42.4 | 26.5 |
| Stroke | 17.2 | 10.1 | 6.5 | 4.8 | 14.9 | 7.8 |
| Cancer | 15.4 | 11.4 | 10.8 | 9.1 | 18.7 | 16.1 |
| Arthritis | 74.7 | 61.7 | 79.6 | 52.3 | 81.3 | 61.7 |
| Psychiatric problems | 27.2 | 14.0 | 33.3 | 21.9 | 37.4 | 17.0 |
| Incontinence | 19.9 | 15.6 | 19.4 | 13.3 | 32.8 | 22.9 |
| Fallen in past 2 years | 32.0 | 28.6 | 40.2 | 31.3 | 43.5 | 32.5 |
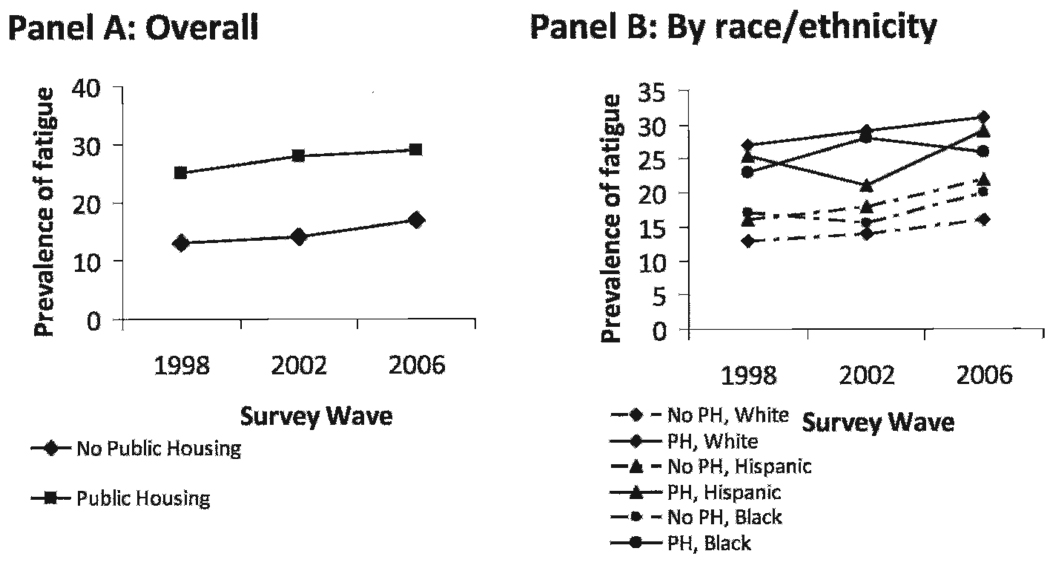
Figure 1 shows the prevalence of fatigue by public housing status overall (Panel A) and by ethnicity (Panel B). Regardless of ethnic group, persons living in public housing were more likely to report fatigue compared to persons not living in public housing. In 2006, 31% of White elders living in public housing reported complaints of fatigue relative to 16% of White elders not in public housing. Similar differences between those living in public housing were observed for Hispanics (public housing 2006, 29% vs no-public housing 2006, 22%) and Blacks (public housing 2006, 26% vs. no-public housing 2006, 20%).
Fig 1.
Prevalence of fatigue stratified by history of public housing
DISCUSSION
To our knowledge, this study is the first to provide a comparison of the health status and symptoms of older persons living in public housing relative to other community-dwelling elders. The nationally representative estimates provided confirm that the distribution of ethnicity among residents of public housing is disproportionate to patterns in the United States with about 38% of tenants of public housing Black and about 16% Hispanic. Regardless of ethnicity, persons living in public housing settings are more likely to experience fatigue, have poorer self-rated health, and comorbid conditions.
Elders experiencing sustained tiredness over time subsequently report difficulty completing activities of daily living.12 The number of chronic illnesses increases with age;13 and cancer, congestive heart failure, and chronic pain are known to be associated with high rates of fatigue.14 This holds true in our analysis, as evidenced by increased incidence of pain and stroke for those in public housing compared to other community-dwelling elders. Fatigue is also a known symptom response to stress. Residents of public housing report being bothered by neighborhood crime (29%), street noise or traffic (17%), odors (14%), and other problems (19%).15 We were unable to evaluate the extent to which contextual factors (eg, living in a racially segregated area) or environmental factors such as crime rates contributed to the prevalence of fatigue, but there is growing support of the relationships between living environment, socioeconomic position, exposure to stress, physiological response and health status.16,17 High levels of perceived stress, loneliness, and poor social and emotional functioning are common correlates of depression, and their association with fatigue is thought to be mediated via depression which may be related to the increased rate of psychiatric illness for those in public housing.
This study confirms that elders who reside in public housing settings represent a special population of community-dwelling elders. Public housing units are typically located in economically depressed areas,18 whose residents continue to experience poor health status.16 The rate of disability is twice that of other community-dwelling elders with over half of these elders reporting difficulty with daily activities such as walking and climbing stairs compared to one-quarter of elders residing in other independent community settings.19 In addition, one-third of elders in public housing settings cite limitations in their ability to complete tasks such as getting to and from doctor’s appointments and grocery shopping.20 Of these elders, most prefer to remain in their housing settings as opposed to moving to more protected environments of care.21 The basic physical conditions of the dwelling space as well as neighborhood conditions can play a role in health outcomes. Poor structure within the home as well as inadequate access to and from the dwelling can contribute to falls and accidents as well as restricting mobility outside of the home. Avoidance of physical activity, such as walking outdoors, owing to neighborhood safety issues increases social isolation and may contribute to decreased mobility over time.22 Each of these factors, in turn, may play a role in the development and severity of fatigue over time. Assessing symptom prevalence and severity will increase our understanding of the daily living experience and health status of elders in public housing. Developing care models to meet the needs and match the challenges of living in public housing are sorely needed. Considered altogether, the challenges facing older persons in public housing combined with symptom recognition must be considered when determining strategies to care for those who age in place.
These findings must be considered with several limitations in mind. All health status indicators and symptoms of fatigue were based on self-report. Some research suggests that independent of physical and psychosocial health variables, Whites are more likely than Blacks to report favorable self-rated health.23 Others suggest that Black patients with osteoarthritis often underestimate symptoms such as pain, as well as disability.24 The potential for differential reporting by ethnicity must be considered when interpreting the findings. Regardless, the potential for this bias does not hamper the comparisons of persons living in public housing to other community-dwelling elders within each ethnic stratum. Lastly, we may have diluted differences between Hispanics and other ethnic groups by aggregating all Hispanics, regardless of interview language. Recent research suggests that health status measures may vary greatly as a function of language spoken.25
There are 3.4 million of the 35 million elders in the United States who live in poverty and are eligible for housing assistance programs.8 Among older households, 1.2 million had worst case housing needs in 2001 defined as below 50% of median family income in the area, more than half income going toward rent and utilities or living in severely substandard housing, and receiving no government housing assistance.26 Among this group, 40% were at least 75 years of age and 43% were Black renters.27 We have provided a snapshot of the health status and symptom of fatigue among those in public housing. Understanding the health status of these oft-neglected elders may inform future innovations in public housing development to meet the needs of a growing segment of society.
ACKNOWLEDGMENTS
Dr. Lapane is funded by award number UL1RR031990 from the National Center for Research and NIH Roadmap for Medical Research, National Institutes of Health. Dr. Mezuk is supported by the Building Interdisciplinary Research Careers inWomen’s Health (BIRCWH) program at Virginia Commonwealth University (K12 HD055881).
Footnotes
AUTHOR CONTRIBUTIONS
Design concept of study: Parsons, Mezuk, Ratliff, Lapane
Acquisition of data: Parsons, Mezuk, Ratliff, Lapane
Data analysis and interpretation: Parsons, Mezuk, Ratliff, Lapane
Manuscript draft: Parsons, Mezuk, Ratliff, Lapane
Statistical expertise: Parsons, Mezuk, Ratliff, Lapane
Acquisition of funding: Parsons, Mezuk, Ratliff, Lapane
Administrative: Parsons, Mezuk, Ratliff, Lapane
Supervision: Parsons, Mezuk, Ratliff, Lapane
REFERENCES
- 1.Wilden R, Redfoot D. Adding Assisted Living Services to Subsidized Housing: Serving Frail Older Persons with Low Income. Washington, DC: AARP Public Policy Institute; 2002. [Google Scholar]
- 2.Haley BA, Gray RW. U.S. Department of Housing and Urban Development Office of Policy Development and Research Section 202 Supportive Housing for the Elderly: Program Status and Performance Measurement. 2008 [Google Scholar]
- 3.Roman C, Knight C, Chalfin A, et al. The relation of the perceived environment to fear, physical activity, and health in public housing developments: evidence from Chicago. J Public Health Policy. 2009;30:S286–S308. doi: 10.1057/jphp.2008.62. [DOI] [PubMed] [Google Scholar]
- 4.Stewart TS, Woodard RM, Rosen AB, et al. The impact of symptoms and impairment on overall health in US national health data. Med Care. 2008;469:954–962. doi: 10.1097/MLR.0b013e318179199f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walke L, Gallo W, Tinnetti M, et al. The burden of symptoms among community-dwelling older persons with advanced chronic disease. Arch Intern Med. 2004;164:2321–2324. doi: 10.1001/archinte.164.21.2321. [DOI] [PubMed] [Google Scholar]
- 6.Vestergaard S, Nayfield S, Patel K, et al. Fatigue in a representative population of older persons and its association with functional impairment, functional limitation, and disability. J Gerontol A Biol Sci Med Sci. 2009;64:176–182. doi: 10.1093/gerona/gln017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hardy S, Studenski S. Fatigue predicts mortality in older adults. J Am Geriatr Soc. 2008;56:1910–1914. doi: 10.1111/j.1532-5415.2008.01957.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeNavas-Watt C, Proctor B, Lee C. U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. [Last accessed December 1, 2010];Income, Poverty and Health Insurance Coverage in the United States. 2005 Available at: http://www.census.gov/prod/2006pubs/p60-231.pdf.
- 9.Heeringa S, Connor J. Technical Description of the Health and Retirement Study Sample Design. Documentation Report. Ann Arbor, MI: University of Michigan; 1995. [Google Scholar]
- 10.Hauser RM, Willis RJ. Survey Design and Methodology in the Health and Retirement Study and the Wisconsin Longitudinal Study. In: Waite LJ, editor. Aging, Health, and Public Policy: Demographic and Economic Perspectives. New York: Population Council; 2005. pp. 209–235. [Google Scholar]
- 11.St.Clair P, Blake D, Bugliari D, et al. RAND HRS Data Documentation, Version J. [Last accessed on December 1, 2010];2010 Available at: http://hrsonline.isr.umich.edu/modules/meta/rand/randhrsj/randhrsj.pdf.
- 12.Avlund K, Rantanen T, Schroll M. Tiredness and subsequent disability in older adults: the role of walking limitations. J Gerontol Med Sci. 2006;61A(11):1201–1205. doi: 10.1093/gerona/61.11.1201. [DOI] [PubMed] [Google Scholar]
- 13.Avlund K, Pedersen AN, Schroll M. Functional decline from age 80 to 85: influence of preceding changes in tiredness in daily activities. Psychosom Med. 2003;65:771–777. doi: 10.1097/01.psy.0000082640.61645.bf. [DOI] [PubMed] [Google Scholar]
- 14.Winningham M, Barton-Burke M, editors. Fatigue in cancer: A Multidimensional Approach. Boston: Jones & Bartlett; 2000. [Google Scholar]
- 15.U.S. Department of Housing and Urban Development Office of Policy Development and Research. [Last accessed on December 1, 2010];Characteristics of HUD-Assisted Renters and Their Units in 2003. 2008 May; Available at: http://www.huduser.org/publications/pdf/Hud_asst_renters_report_p1.pdf.
- 16.Curry A, Latkin C. Community and structural level interventions as pathways to depression. Soc Sci Med. 2008;67(1):23–30. doi: 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krieger N, Chen JT, Rehkopf DH, et al. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95:312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Massey DS, Denton N. American Apartheid: Segregation and the Making of an Underclass. Cambridge: Harvard University Press; 1993. [Google Scholar]
- 19.Redfoot D, Kochera A. Targeting services to those most at risk: characteristics of residents in federally subsidized housing. J Housing Elderly. 2004;18(3–4):141. [Google Scholar]
- 20.Harahan MF, Sanders A, Stone R. A synthesis of findings from the study of affordable housing plus services for low and modest income older adults. [Last accessed on December 1, 2010];2006 Available at: http://www.huduser.org/portal/publications/affhsg/synthesis.html.
- 21.O’Keeffe J, O’Keeffe C, Bernard S. Using Medicaid to Cover Services for Elderly Persons in Residential Care Settings: State Policy Maker and Stakeholder Views in Six States. [Last accessed on December 1, 2010]; Available at: http://aspe.hhs.gov/daltcp/reports/med4rcs.htm.
- 22.Clarke P, Ailshire JA, Bader M, et al. Mobility disability and the urban built environment. Amer J Epidemiol. 2008;168(5):506–513. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spencer SM, Schulz R, Rooks RN, et al. Racial differences in self-rated health at similar levels of physical functioning: an examination of health pessimism in the health, aging, and body composition study. J Gerontol B Psychol Sci Soc Sci. 2009;64(1):87–94. doi: 10.1093/geronb/gbn007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burns R, Graney MJ, Lummus AC, et al. Differences of self-reported osteoarthritis disability and race. J Natl Med Assoc. 2007;99(9):1046–1051. [PMC free article] [PubMed] [Google Scholar]
- 25.Tirodkar MA, Song J, Chang RW, et al. Racial and ethnic differences in activities of daily living disability among the elderly: the case of Spanish speakers. Arch Phys Med Rehabil. 2008;89(7):1262–1266. doi: 10.1016/j.apmr.2007.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Department of Housing and Urban Development. [Last accessed on December 1, 2010];Report to Congress on Worst Case Housing Needs. 2003 Available at: http://www.huduser.org/portal/publications/affhsg/affhsgneed.html.
- 27.Engelhardt GV. Housing older Americans. Fannie Mae Papers. 2005;IV(1) [Google Scholar]