Abstract
Performance-based assessments of everyday living skills have been shown to be highly correlated with cognitive functioning in schizophrenia and bipolar disorder, as well as being predictive of deficits in real-world outcomes such as independent living and employment. In this study, we expand our assessments of impairments in everyday living skills to China, evaluating people with schizophrenia, bipolar disorder, and major depression, and comparing their performance to that of healthy controls. Samples of people with schizophrenia (N=272), bipolar disorder (n=61), major depression (n=50), and healthy controls (n=284) were examined with the Chinese version of the UCSD performance-based assessment, brief version (UPSA-B). Performance was compared across the groups and the association between age, gender, educational attainment, marital status, and UPSA-B scores was evaluated. When the performance on the UPSA was compared across the groups, with education as a covariate, significant effects of both diagnosis (F=86.3, p<.001) and education were found (F=228.3, p<.001). Sex and age did not contribute significantly when age and education were considered. Post-hoc comparisons revealed that total UPSA-B scores were lowest in the schizophrenia patients, followed by the patients with major depression. Patients with bipolar disorder did not differ from the healthy comparison subjects on overall performance. Scores for all groups were lower than previously reported in western samples (e.g., HC mean = 64). While diagnostic differences in UPSA-B scores are similar to those previously seen in western samples, the education effect is considerably more substantial. These data suggest that in developing countries educational attainment may be strongly associated with levels of adaptive outcomes and the utilization and interpretation of functional capacity measures be adjusted accordingly.
Keywords: Schizophrenia, Bipolar Disorder, Depression, Functional capacity, Performance based assessment
Introduction
Disability is associated with all major mental illnesses, including major depression, bipolar disorder, and schizophrenia. In schizophrenia, substantial deficits in everyday functioning are common and related to cognitive deficits (Green, et al., 2000). Global deficits as well as impairments in specific cognitive functioning domains have been reported (Dickinson, Ragland, et al., 2008); (Reichenberg & Harvey, 2007); (Leung et al. 2008). These impairments include deficits in episodic memory (Ranganath, Minzenberg, et al., 2008), processing speed (Dickinson, Ramsey, et al., 2007), and executive functioning, including working memory (Reichenberg, et al., 2007); (Lee & Park, 2005). In unipolar depression impairments in memory, visual-motor speed (Austin, Ross, et al., 1992), attentional set shifting, and sustained motor responses have been observed during acute episodes (Purcell, Maruff, et al., 1997), while during remission deficits in measures of visual-motor sequencing, executive function, immediate memory, and attention have been seen (Paradiso, Ohkubo, et al., 1997). In bipolar disorder impairments in verbal memory and executive functioning tasks have been reported in episodes of mania, depression and, euthymia (Martinez-Aran, Vieta, et al., 2004a); (Martinez-Aran, Vieta, et al., 2004b); (Zubieta, Huguelet, et al., 2001).
While there has been an increasing literature on cognitive impairments in these patient populations, fewer studies have focused on functional impairments and disability. Studies of functional impairment in unipolar depression reveal that real-world disability increases during episodes of depression but can return to a reduced level of impairment during remission. In one such study, functioning in everyday activities improved with remission, but social functioning remained impaired (Spijker, Graaf, et al., 2004). Others have observed that functional impairments are both severe and widespread, affecting marital quality, income, occupation, and education even in depressed patients who have sustained a two year remission (Coryell, Scheftner, et al., 1993). Severity of depression and anxiety symptoms (Naismith, Longley, et al., 2007); Spijker, et al., 2004), cumulative history of depression, time spent depressed, psychiatric comorbidities, personality traits, and perceived social support (Rytsala, Melartin, et al., 2006) have all been associated with real-world functional impairments in persons with unipolar depression. Studies of functional impairment in bipolar disorder reveal a similar extent of severe, enduring psychosocial disability (Huxley and Baldessarini, 2007). Predictors of functional impairment include poorer performance on tests of cognitive function (Wingo, Harvey, et al., 2009), total number of mood episodes (Martinez-Aran, et al., 2004a), extent of symptom remission, substance abuse (Dickerson, Origoni, et al., 2010), symptom severity, history of psychiatric hospitalizations, and maternal education (Dickerson, Boronow, et al., 2004).
Recent advances in the assessment of disability in persons with severe mental illness have separated the measurement of the ability to perform everyday adaptive skills (referred to herein as “functional capacity”) from real-world functional outcomes, yielding a more precise set of predictors of outcome (Harvey, et al. 2007). In two studies of large samples of schizophrenia and bipolar patients, deficits on performance-based measures of everyday functioning efficiently predicted real world functional impairments. In the first (Mausbach, Harvey, et al., 2010), performance on a brief version (UPSA-B; (Mausbach, Harvey, et al., 2007) of the UCSD performance-based skills assessment (UPSA; (Patterson, Goldman, et al., 2001) predicted the level of residential independence in the combined sample, with diagnosis (schizophrenia vs. bipolar) adding no incremental predictive power. The second study (Bowie, Depp, et al., 2010) found that performance on the UPSA-B was a strong predictor of real-world outcomes in both patient samples, with minimal differences in the functional, cognitive, and symptomatic determinants of real-world functioning across the two diagnoses. Interestingly, the severity of both schizophrenia and bipolar (mania and depression) symptoms was correlated with real-world functional deficits in a manner independent of performance on the UPSA.
Some evidence has suggested that substantial differences in environmental conditions may have a minimal impact on performance-based measures of functional capacity and cognition. In a cross national study of schizophrenia patients in the United States and Sweden (Harvey, Helldin, et al., 2009a), no differences were found in functional capacity, cognitive performance, and clinician ratings of the ability to perform everyday living skills. In the same sample, residential independence varied significantly between the two countries, suggesting that performance-based measures may be less influenced by environmental factors than real-world outcomes. The interaction between cultural differences and everyday functioning in schizophrenia has been studied previously. Outcome in schizophrenia has been suggested to vary significantly between “lower and middle income” countries when compared to “high income” Western countries (Isaac, Chand, et al., 2007). However, in a study of Chinese patients in Hong Kong, Au et al. (2005) found that when they translated a real-world functioning scale, the St Louis Inventory of Community Living skills into Chinese, the scale was able to discriminate between patients discharged to different levels of community care. Further, in a study in Taiwan Jiang (1999) reported that patients with bipolar disorder had substantial residual disability after clinical recovery, suggesting that the characteristics of disability in bipolar disorder in Chinese patients seems similar to those reported in Western Cultures.
There have been no studies to date on functional capacity measures in schizophrenia patients in China and certainly no studies comparing healthy individuals to multiple samples of patients with different variants of severe mental illness. While the studies cited above suggest that functional disability associated with severe mental illness have similar characteristics, there are possible reasons that functional capacity measures would require come careful consideration in Chinese samples. Individuals with low levels of educational and vocational attainment, even without any evidence of mental illness, would be expected to be less likely to have experience with banking and using the telephone, both of which are central features of the UPSA-B. These differences may impact on performance on functional capacity measures and require this issue requires direct study in order to determine how these measures should be adjusted for use across different countries and cultures.
In this paper we present the results of a study measuring functional capacity in patients with schizophrenia, bipolar disorder, and major depression living in Beijing, China using a translated and culturally adapted version of the UPSA-B. Further, we examined a large sample of healthy individuals in order to understand normative performance on these ability measures in Beijing. We hypothesized that impairments in functional capacity are a central feature of severe mental illness, as indexed by a relative impairment in performance for the patient groups compared to the healthy sample. We also took advantage of the wide variation in educational attainment in this sample to examine whether level of education, as well as other demographic factors, influenced performance on functional capacity measures. As performance-based ability measures are used as outcome measures in clinical treatment studies (Green, Nuechterlein, et al., 2008), understanding their characteristics across different countries and cultures may help inform treatment of schizophrenia and bipolar illness. We expected that education would also have a notable impact on UPSA-B scores and were interested in whether this impact interacted with the presence of serious mental illness.
Method
Participants
Patient participants in this study met criteria for schizophrenia, bipolar disorder, or major depression (DSM-IV). Physically healthy patients who met DSM-IV (American Psychiatric Association, 2000) for schizophrenia, bipolar disorder and major depression were compared with 284 Chinese normal controls. All patients were recruited from among the inpatients of Beijing Hui-Long-Guan Hospital, a Beijing City owned psychiatric hospital. Diagnoses were made for each patient by two independent experienced psychiatrists and utilized structured interviews (a translated version of the SCID; First et al., 1995), access to detailed medical records, and relied on the DSM-IV criteria. Healthy controls were recruited from the local community, and selected for similarity to the patients in age and gender. Current mental status and personal or family history of any mental disorder was assessed by a clinical psychiatrist. None of the healthy control subjects presented a personal or family history of psychiatric disorder. All subjects were Han Chinese being recruited at the same period from the Beijing area.
A complete medical history and physical examination were obtained from all subjects. Any subjects with physical abnormalities were excluded. Neither the patients nor the control subjects suffered from drug or alcohol abuse/dependence. All subjects gave signed, informed consent to participate in the study, which was approved by the Institutional Review Board, Beijing Hui LongGuan hospital. Three hundred patients with schizophrenia, 70 patients with bipolar disorder and 60 patients with major depression were approached on inpatient units at the hospital. As far as agreement to participate, twenty-eight patients (9.3%) with schizophrenia, 9 (12.9%) with bipolar disorder and 10 (16.7%) with major depression declined to take part in the study. Three hundred healthy controls were approached, and 16 (5.3%) declined. Among the healthy controls, 4 (1.3%) had to be excluded due to a psychiatric diagnosis.
Performance Based Measure of Functional Capacity
The UCSD Performance-Based Skills Assessment, Brief Version (UPSA-B) is designed to directly assess everyday functioning in persons with severe mental illness (Mausbach, et al., 2007). The UPSA-B is based on the original UCSD Performance Based Skills Assessment (UPSA) which was designed to assess the capacity of persons with schizophrenia to perform the tasks necessary for daily functioning (Patterson, et al., 2001). The UPSA-B consists of two subscales (financial and communication) from the original UPSA which correspond with total UPSA-B Score. In the financial portion of the skills assessment, the participant must count out given amounts from real currency, make change, and fill out a check to pay a utility bill. The communication domain requires that the participant make emergency calls, call directory assistance to obtain a telephone number, call the number, and then reschedule an appointment. The scores on the UBSA-B are standardized to a 100-point scale, consistent with scoring of the original UPSA, which allows for comparison with previous studies that used the original version of the UPSA.
The Chinese version of the UPSA- B was developed for use in research studies with Han Chinese populations. Tasks were modified in order to be congruent with local functional demands, including changing currency management tasks, telephone numbers, and appointment formats. Further, the check writing task was changed in order to reflect more realistic local demands, which included making a bank withdrawal and requesting a bank check to pay a bill. After the tasks were modified, the instructions were translated into Mandarin by Jin Fan, PhD (Mt. Sinai School of Medicine, New York, NY) and then back translated by one of the authors, XZ and then examined by another of the authors PDH.
The assessments were administered by trained testers who were native Mandarin speakers. Testers did not know the educational levels of the participants and were not informed of the diagnosis of the psychiatric patients in the study.
Demographic Factors
We used categorical ranking of milestone achievements derived from self report, informant, and clinical chart data. These included years of education and completion of educational milestones (primary school or less, middle school, secondary school, college or higher) and marital status (ever married, never married). Other demographic information including age and sex were also collected for use in these analyses.
Data Analyses
A general linear model analysis of variance (SPSS version 17) was used to compare total UPSA-B scores between subject groups: healthy control, schizophrenia, bipolar disorder, and major depression. Regression analyses were used to examine the correlations between the demographic variables of age, education, and marital status on UPSA-B scores. The performance on individual items was expressed as the average correct for the dichotomous items, leading to proportion scores that were examined parametrically. Although we present education categorically in figures for ease of viewing, all analyses were performed with education as a continuous variable.
Results
Demographic characteristics of the study participants are presented by diagnostic category in Table 1. Males were over-represented in the schizophrenia sample (65%) and females over-represented in the depressed sample (65%) when compared to the healthy control group. Across groups schizophrenia patients were the least likely to have ever been married (48%), followed by bipolar patients (43%), depressed patients (18%), and healthy controls (8%). Level of education was lowest in the schizophrenia sample though there was wide variability in level of education in all groups. Internal consistency of the UPSA-B was examined with coefficient alpha in the schizophrenia patients and healthy controls, with these reliabilities being quite suitable: .84 in the schizophrenia sample and .87 in the healthy controls.
Table 1.
Demographic Characteristics and Performance on UPSA-B
| Schizophrenia (n=272) |
Bipolar (n=61) |
Depressed (n=50) |
Healthy Control (n=284) |
|||||
|---|---|---|---|---|---|---|---|---|
| % Male | 65 | 59 | 35 | 44 | ||||
| % Never Married | 48 | 43 | 14 | 8 | ||||
| Mean Age (SD) | 45.47 (12.4) | 38.31 (11.3) | 53.35 (14.6) | 47.92 (11.6) | ||||
| Education | ||||||||
| % Elementary | 7 | 10 | 22 | 15 | ||||
| % Middle School | 40 | 26 | 42 | 36 | ||||
| % High School | 38 | 39 | 18 | 34 | ||||
| % College or more | 15 | 25 | 18 | 15 | ||||
| Mean Education (SD) | 9.43 (6.4) | 10.21 (4.3) | 9.36 (5.4) | 10.50 (4.8) | ||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| UPSA-B Scaled Score | 37.59 | 26.12 | 55.24 | 20.35 | 47.90 | 22.77 | 64.31 | 23.33 |
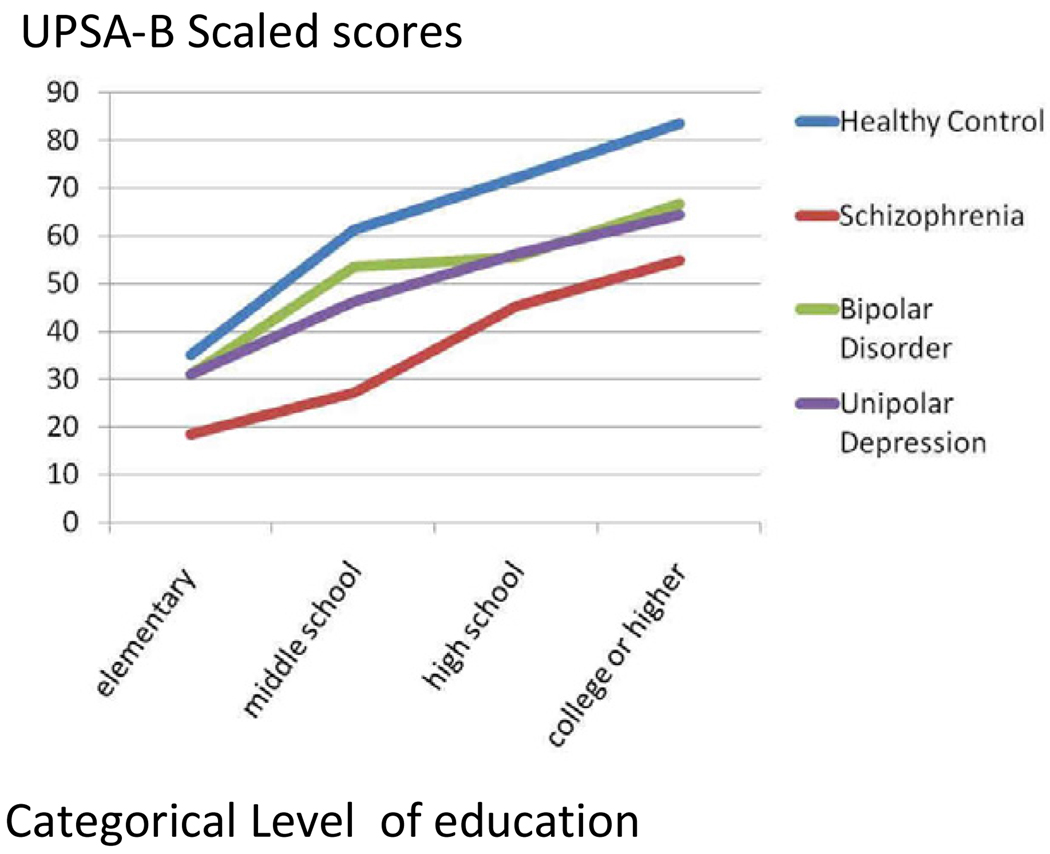
Performance on the total score for the UPSA-B was lowest in patients with schizophrenia (see Table 1) followed by patients with major depression. Figure 1 presents UPSA-B Score as a function of categorical educational attainment in patients with schizophrenia, bipolar disorder, major depression, and healthy controls. In a simultaneous entry regression analysis examining the influence of age, education, sex, and marital status on UPSA-B scores, only education entered the equation, F=109.2, p<.001, while the other three demographic variables did not enter the equation, all F< 2.02, all p>.22.
Figure 1.
UPSA-B Scores as a Function of Education Completed
When performance on the UPSA-B was compared across the groups, using education as a covariate, a significant effect of diagnosis (F = 86.3, p < .001) was found and education manifested a substantial covariate effect (F = 228.3, p < .001). The interaction of Diagnosis × Education was not significant, F=2.24, p=0.23. When the analysis was repeated with categorical educational attainment instead of years of education, the results were very similar: F=197.6, p<.001. Post hoc follow-up tests found that patients with schizophrenia and major depression performed significantly more poorly on the total score than healthy control subjects (p<.05). Performance on UPSA-B total score did not differ significantly between patients with bipolar disorder and healthy controls and between bipolar and unipolar patients (but the affective patient samples are smaller than the schizophrenia healthy comparison groups). At all levels of educational attainment, total UPSA-B scores were significantly lower in the schizophrenia patients than in all other groups. While total score on UPSA-B revealed more impairment in everyday functioning among patients with schizophrenia, specific item scores suggested differential sensitivity to deficits in patients with severe mental illness.
In order to examine these differences, we performed a one-way ANOVA for each item, comparing the average scores for each of the items across the four patient groups. We used Scheffe follow-up tests to examine specific differences between the groups and applied the Bonferroni correction to the results of the 19 ANOVAs (.05/19=.002). Table 2 shows the differences in performance across all of the items between the groups of research participants. The overall between-groups analyses revealed statistically significant overall Bonferroni corrected differences in performance of all items on the UPSA-B except for writing the correct date on a bank check. The patients with schizophrenia were more impaired than the healthy controls on all but that one item, indicating that all items were sensitive to schizophrenia collapsed across educational attainment levels when the two largest samples were compared.
Table 2.
Individual Item Performance and between Group Differences on UPSA-B Items
| Financial Skill 1: Counting money and making change | P | F | |||||||
| 1a: Show me 1.03 in coins | Schizophrenia | = | Bipolar | = | Depression | < | HC | <0.001 | 21.25 |
| Mean Correct responses | 52 | 52 | 57 | 81 | |||||
| 1b: Show me 6.74 in coins | Schizophrenia | < | Depression | = | Bipolar | = | HC | <0.001 | 30.79 |
| Mean Correct responses | 59 | 80 | 87 | 90 | |||||
| 1c: Show me 12.18 in coins | Schizophrenia | < | Depression | = | Bipolar | = | HC | <0.001 | 18.74 |
| Mean Correct responses | 65 | 82 | 84 | 88 | |||||
| 1d: Make change from 10.00 | Schizophrenia | = | Depression | < | Bipolar | = | HC | <0.001 | 24.50 |
| Mean Correct responses | 46 | 43 | 66 | 78 | |||||
| Financial Skill 2: Paying a bill | |||||||||
| 2a: Date check | Schizophrenia | = | HC | = | Depression | = | Bipolar | 0.067 | 2.41 |
| Mean Correct responses | 43 | 51 | 55 | 61 | |||||
| 2b: Write full name of remitter | Schizophrenia | = | Depression | = | Bipolar | < | HC | <0.001 | 24.00 |
| Mean Correct responses | 37 | 43 | 62 | 70 | |||||
| 2c: Write full name of payee | Schizophrenia1 | = | Depression | = | HC | = | Bipolar | 0.001 | 5.80 |
| Mean Correct responses | 25 | 29 | 40 | 41 | |||||
| 2d: Write account number | Schizophrenia1 | = | Depression | = | Bipolar | = | HC | <0.001 | 27.17 |
| Mean Correct responses | 43 | 59 | 73 | 77 | |||||
| 2e: Write amount in words | Schizophrenia1 | = | Depression | = | Bipolar | = | HC | <0.001 | 20.30 |
| Mean Correct responses | 21 | 35 | 39 | 51 | |||||
| 2f: Write amount in numbers | Schizophrenia | < | Depression | = | HC | = | Bipolar | <0.001 | 14.26 |
| Mean Correct responses | 46 | 61 | 71 | 72 | |||||
| Communication Skill: Dialing telephone numbers and calling to reschedule an appointment | |||||||||
| 3a: Dial medical emergency number | Schizophrenia | < | Depression | = | HC | = | Bipolar | <0.001 | 44.99 |
| Mean Correct responses | 41 | 74 | 78 | 81 | |||||
| 3b: Call directory assistance to obtain a telephone number | Schizophrenia | < | Bipolar | = | Depression | = | HC | <0.001 | 8.68 |
| Mean Correct responses | 46 | 59 | 66 | 66 | |||||
| 3c: Check the telephone number | Schizophrenia | < | Depression | = | HC | = | Bipolar | <0.001 | 10.84 |
| Mean Correct responses | 49 | 63 | 73 | 79 | |||||
| 3d: Dial number from memory | Schizophrenia | = | Depression | < | Bipolar | = | HC | <0.001 | 35.18 |
| Mean Correct responses | 45 | 37 | 66 | 81 | |||||
| 3e: Find phone number needed to reschedule physical exam | Schizophrenia | = | Depression | = | Bipolar | < | HC | <0.001 | 22.27 |
| Mean Correct responses | 60 | 65 | 70 | 89 | |||||
| 3f: Leave accurate message requesting to reschedule exam | Schizophrenia | = | Bipolar | = | Depression | < | HC | <0.001 | 33.13 |
| Mean Correct responses | 35 | 49 | 53 | 70 | |||||
| 3g: Recall items to bring to physical exam: insurance card | Schizophrenia | < | Bipolar | = | Depression | = | HC | <0.001 | 26.70 |
| Mean Correct responses | 18 | 28 | 31 | 49 | |||||
| 3h: Recall items to bring to physical exam: medication list | Schizophrenia | < | Depression | = | Bipolar | = | HC | <0.001 | 23.60 |
| Mean Correct responses | 21 | 28 | 31 | 49 | |||||
| 3i: Recall preparation required: fast for blood work | Schizophrenia | = | Bipolar | = | Depression | < | HC | <0.001 | 86.57 |
| Mean Correct responses | 16 | 18 | 21 | 72 | |||||
Note.
Schizophrenia worse than HC is the only significant difference between groups.
In contrast, patients with affective disorders were more variable in their impairments. There were 7 items on which at least one of the affective samples was more impaired than the HC group, even with the reduced power and conservative nature of the post hoc statistical tests.
Discussion
These results suggest that among patients with severe mental illness living in China, patients with schizophrenia have more significant deficits in everyday living skills than healthy individuals and, in some domains, patients with affective disorders. UPSA-B scores for all groups were lower than previously reported in western samples. For example, in the current study average UPSA-B total score for healthy controls was 64, which is comparable to the total score obtained by schizophrenia patients in recently studied Western samples (Harvey, et al., 2009a). In the Chinese sample, the highest educated subjects had scores consistent with those seen previously in US samples, for both schizophrenia patients (Mean=78) and healthy controls (Mean=83). In addition, in this study of people in China, education exerted a significant influence on functional capacity, an influence that is much more substantial than that observed in a recent study of patients living in the United States and in Sweden. This implies, pending replication, that in developing countries the level of education is a more influential determinant of functional outcome than in western nations. It is also the case that extremely low levels of education are not often found in healthy comparison subjects in US studies. Therefore, cross national approaches to studying and treating severe mental illness should include consideration of patients’ level of educational attainment, because education apparently exerted similar influences on performance in healthy individuals and patients with schizophrenia.
The mechanism of influence of education on functional capacity is likely channeled through opportunity and daily life complexity. Individuals with very low levels of education who reside in developing countries, even in large cities, are unlikely to use telephones, schedule appointments, and have bank accounts. It would not be reasonable to expect that in an assessment situation they would be able to perform skilled acts that they may have never even observed previously. Careful consideration of the extent of prior educational attainment and extent of relevant life experiences may be prudent when implementing such assessments in developing countries, particularly in clinical treatment studies. Given the challenges in implementing multi-site treatment studies under more optimal circumstances (Keefe and Harvey, 2008) performance-based functional outcomes measures may have to be adapted and validated prior to their implementation in such environments.
There are several limitations of the study. These limitations include the smaller sample size of the two affective disorder samples. This is likely the reason that the current bipolar sample did not differ from the healthy comparison group despite performing about 0.5 SD more poorly on the UPSA total score. Further, the item by item analyses were performed on a purely post hoc basis and would require replication. We did not collect detailed information on histories of residential status, so we cannot link these results into independence in residence. It is likely that independence in residential status has different implications in Western as opposed to developing nations and may have substantially different features in regions with larger extended families, more housing challenges, and differences in the cohesiveness of basic family structure. All patients were assessed as inpatients, so these results might be different for ambulatory patients. This status cannot account for the differences we detected between the patient groups. Inpatient treatment is more common in China than in Western Cultures. Thus, clinical treatment studies that use performance-based outcomes measures might also recruit from such treatment sites. We did not have systematically obtained ratings of clinical symptom severity for these patients, so we cannot examine the relationships, if any, between symptoms and functional capacity measures. As we note above, there were no such correlations detected in several different samples of patients in the past. Finally, we do not have clinical ratings of real-world functioning or performance on neuropsychological assessments available for the entire sample. As a result, our focus is entirely on functional capacity and this is the largest sample of healthy controls ever tested with a functional capacity assessment in a mental health study.
These data suggest that performance-based measures of everyday living skills are sensitive to the presence of major psychiatric conditions even when confounded by extreme variation in educational attainment. The effect of education was independent of diagnosis in this data set, suggesting that selection of participants for research could be stratified by education without biasing the performance of the subgroups. Further, the education signal was substantially greater than the influence of age, education, and marital status. At the same time, modification of performance-based task demands to local standards, in both everyday living and social skills domains, would be the optimal way to tailor functional assessments in a cross-cultural perspective. It will be important to separate life-long participant characteristics (i.e., education) from correlates of illness in order to effectively measure treatment effects on cognitive and functional deficits in severe mental illness in developing countries.
Acknowledgments
This research was supported by NIMH Grants K05-DA0454, P50-DA18827 and U01-MH79639 to Dr. Kosten and NIMH Grant MH 78775 to Dr. Harvey.
Dr. Harvey has a research grant from Astra-Zeneca Pharmaceuticals. He has served as consultant to Abbott Labs, Bristol-Myers-Squibb, Cypress Bioscience, En Vivo Pharma, Genentech, Merck and Company, Sunovion, Shire Pharma, and Teva Pharma.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The other authors report no disclosures.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington DC: Author; 2000. [Google Scholar]
- Au RW, Tam PW, Tam GW, Ungvari GS. Cross-cultural validation of the St. Louis Inventory of Community Living Skills for Chinese patients with schizophrenia in Hong Kong. Psychiatr Rehabil J. 2005;29:34–40. doi: 10.2975/29.2005.34.40. [DOI] [PubMed] [Google Scholar]
- Austin MP, Ross M, Murray C, O'Carroll RE, Ebmeier KP, Goodwin GM. Cognitive function in major depression. J Affect Disord. 1992;25:21–29. doi: 10.1016/0165-0327(92)90089-o. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Depp C, McGrath JA, Wolyniec P, Mausbach BT, Thornquist MH, Luke J, Patterson TL, Harvey PD, Pulver AE. Prediction of Real-World Functional Disability in Chronic Mental Disorders: A Comparison of Schizophrenia and Bipolar Disorder. Am J Psychiatry. 2010;167:1116–1124. doi: 10.1176/appi.ajp.2010.09101406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;150:720–727. doi: 10.1176/ajp.150.5.720. [DOI] [PubMed] [Google Scholar]
- Dickerson F, Origoni A, Stallings C, Khushalani S, Dickinson D, Medoff D. Occupational status and social adjustment six months after hospitalization early in the course of bipolar disorder: a prospective study. Bipolar Disord. 2010;12:10–20. doi: 10.1111/j.1399-5618.2009.00784.x. [DOI] [PubMed] [Google Scholar]
- Dickerson FB, Boronow JJ, Stallings CR, Origoni AE, Cole S, Yolken RH. Association between cognitive functioning and employment status of persons with bipolar disorder. Psychiatr Serv. 2004;55:54–58. doi: 10.1176/appi.ps.55.1.54. [DOI] [PubMed] [Google Scholar]
- Dickinson D, Ragland JD, Gold JM, Gur RC. General and specific cognitive deficits in schizophrenia: Goliath defeats David? Biol Psychiatry. 2008;64:823–827. doi: 10.1016/j.biopsych.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch Gen Psychiatry. 2007;64:532–542. doi: 10.1001/archpsyc.64.5.532. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin LS. User’s guide for the Structured Clinical Interview for DSM-IV Axis I (SCID-I) Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the “right stuff?”. Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Green MF, Nuechterlein KH, Kern RS, Baade LE, Fenton WS, Gold JM, Keefe RS, Mesholam-Gately R, Seidman LJ, Stover E, Marder SR. Functional co-primary measures for clinical trials in schizophrenia: results from the MATRICS Psychometric and Standardization Study. Am J Psychiatry. 2008;165:221–228. doi: 10.1176/appi.ajp.2007.07010089. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Helldin L, Bowie CR, Heaton RK, Olsson AK, Hjarthag F, Norlander T, Patterson TL. Performance-based measurement of functional disability in schizophrenia: a cross-national study in the United States and Sweden. Am J Psychiatry. 2009;166:821–827. doi: 10.1176/appi.ajp.2009.09010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, Velligan DI, Bellack AS. Performance-based measures of functional skills: usefulness in clinical treatment studies. Schizophrenia Bull. 2007;33:1138–1148. doi: 10.1093/schbul/sbm040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxley N, Baldessarini RJ. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9:183–196. doi: 10.1111/j.1399-5618.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- Isaac M, Chand P, Murthy P. Schizophrenia outcome measures in the wider international community. Br J Psychiatry Suppl. 2007;50:s71–s77. doi: 10.1192/bjp.191.50.s71. [DOI] [PubMed] [Google Scholar]
- Keefe RSE, Harvey PD. Implementation Considerations for Multi-site Clinical Trials with Cognitive Neuroscience Tasks. Schizophr Bull. 2008;34:656–663. doi: 10.1093/schbul/sbn042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J, Park S. Working memory impairments in schizophrenia: a meta-analysis. J Abnorm Psychol. 2005;114:599–611. doi: 10.1037/0021-843X.114.4.599. [DOI] [PubMed] [Google Scholar]
- Leung WW, Bowie CR, Harvey PD. Functional implications of neuropsychological normality and symptom remission in older outpatients diagnosed with schizophrenia: A cross-sectional study. J Int Neuropsychol Soc. 2008;14:479–488. doi: 10.1017/S1355617708080600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Aran A, Vieta E, Colom F, Torrent C, Sanchez-Moreno J, Reinares M, Benabarre A, Goikolea JM, Brugue E, Daban C, Salamero M. Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord. 2004a;6:224–232. doi: 10.1111/j.1399-5618.2004.00111.x. [DOI] [PubMed] [Google Scholar]
- Martinez-Aran A, Vieta E, Reinares M, Colom F, Torrent C, Sanchez-Moreno J, Benabarre A, Goikolea JM, Comes M, Salamero M. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry. 2004b;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull. 2007;33:1364–1372. doi: 10.1093/schbul/sbm014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Harvey PD, Pulver AE, Depp CA, Wolyniec PS, Thornquist MH, Luke JR, McGrath JA, Bowie CR, Patterson TL. Relationship of the Brief UCSD Performance-based Skills Assessment (UPSA-B) to multiple indicators of functioning in people with schizophrenia and bipolar disorder. Bipolar Disord. 2010;12:45–55. doi: 10.1111/j.1399-5618.2009.00787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naismith SL, Longley WA, Scott EM, Hickie IB. Disability in major depression related to self-rated and objectively-measured cognitive deficits: a preliminary study. BMC Psychiatry. 2007;7:32. doi: 10.1186/1471-244X-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradiso S, Ohkubo T, Robinson RG. Vegetative and psychological symptoms associated with depressed mood over the first two years after stroke. Int J Psychiatry Med. 1997;27:137–157. doi: 10.2190/BWJA-KQP3-7VUY-D06T. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Purcell R, Maruff P, Kyrios M, Pantelis C. Neuropsychological function in young patients with unipolar major depression. Psychol Med. 1997;27:1277–1285. doi: 10.1017/s0033291797005448. [DOI] [PubMed] [Google Scholar]
- Ranganath C, Minzenberg MJ, Ragland JD. The cognitive neuroscience of memory function and dysfunction in schizophrenia. Biol Psychiatry. 2008;64:18–25. doi: 10.1016/j.biopsych.2008.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichenberg A, Harvey PD. Neuropsychological impairments in schizophrenia: Integration of performance-based and brain imaging findings. Psychol Bull. 2007;133:833–858. doi: 10.1037/0033-2909.133.5.833. [DOI] [PubMed] [Google Scholar]
- Rytsala HJ, Melartin TK, Leskela US, Lestela-Mielonen PS, Sokero TP, Isometsa ET. Determinants of functional disability and social adjustment in major depressive disorder: a prospective study. J Nerv Ment Dis. 2006;194:570–576. doi: 10.1097/01.nmd.0000230394.21345.c4. [DOI] [PubMed] [Google Scholar]
- Spijker J, Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA. Functional disability and depression in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Acta Psychiatr Scand. 2004;110:208–214. doi: 10.1111/j.1600-0447.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- Wingo AP, Harvey PD, Baldessarini RJ. Neurocognitive impairment in bipolar disorder patients: functional implications. Bipolar Disord. 2009;11:113–125. doi: 10.1111/j.1399-5618.2009.00665.x. [DOI] [PubMed] [Google Scholar]
- Zubieta JK, Huguelet P, O'Neil RL, Giordani BJ. Cognitive function in euthymic bipolar I disorder. Psychiatry Res. 2001;102:9–20. doi: 10.1016/s0165-1781(01)00242-6. [DOI] [PubMed] [Google Scholar]