Abstract
Objective
To characterize patterns of Emergency Medical Technician (EMT) partner familiarity in three Emergency Medical Services (EMS) agencies.
Study Design/Data Sources
We utilized a case study design and retrospective review of administrative data from three EMS agencies and 182 EMTs over 12 months. We used the Kruskal–Wallis test and Bonferroni corrected p-values to compare measures of partner familiarity. Measures included the annual mean number of partners, rate of partners per 10 shifts, mean shifts per EMT, and proportion of shifts worked with same partner. We standardized select measures by size of agency to account for a greater number of possible partnerships in larger agencies.
Principal Findings
Across all agencies, the mean number of shifts worked annually by EMTs was (mean [SD]) 77.3 (59.8). The unstandardized mean number of EMT partnerships was 19.3 (12.4) and did not vary across EMS agencies after standardizing by agency size (p = .328). The unstandardized mean rate of EMT partnerships for every 10 shifts worked was 4.0 (2.7) and varied across agencies after standardizing (p<.001). The mean proportion of shifts worked with the same partner was 34.8 percent and varied across agencies (p<.001).
Conclusions
There was wide variation in select measures of EMT partner familiarity.
Keywords: Emergency Medical Services, partnerships, teamwork
Teamwork is fundamental to the delivery of care in prehospital Emergency Medical Services (EMS) (Williams, Rose, and Simon 1999). Teams of Emergency Medical Technicians (EMTs), who usually work on ambulances in teams of two (dyads), respond to urgent and nonurgent medical emergencies. Unlike most health care teams, EMTs work in isolation, trained to follow written protocols developed by physicians. All EMTs are exposed to hazardous work conditions, including violent patients (Corbett, Grange, and Thomas 1998; Grange and Corbett 2002;). Their risk of injury and death is greater than the general public's (Maguire et al. 2002; Maguire et al. 2005; Reichard and Jackson 2010;). Furthermore, medical errors, accidents, and adverse events occur frequently in EMS (Rittenberger, Beck, and Paris 2005; Wang et al. 2006; Wang et al. 2008; Wang et al. 2009a,b;). Positive teamwork is associated with reduced errors and improved patient safety in multiple health care settings (Kohn, Corrigan, and Donaldson 2000; Lemieux-Charles and McGuire 2006;). Similar evidence in the EMS environment is not available.
Teamwork is a set of coordinated behaviors and actions that contribute to reaching shared or common goals (Salas and Fiore 2004). Theorists agree that teams develop team-related behaviors over time and through shared experiences (Chidambaram and Bostrom 1997; Tuckman 1965;). Newly formed teams have few shared experiences, which may make them susceptible to error or poor performance. In a review of aviation accidents from 1978 to 1990, investigators linked 70 percent of accidents to pilot and copilot teams flying together for the first time (Board 1994). In a study of air traffic control teams, Smith-Jentsch et al. (2009) determined that individuals provided less back-up when working with unfamiliar partners.
One impediment to partner familiarity is workforce turnover. More than 50 percent of EMS agency directors have reported problems maintaining an adequate workforce of EMTs (Freeman, Slifkin, and Patterson 2009). This rapid turnover may influence the degree of EMT partner familiarity and account for adverse outcomes in EMT team performance (Brown et al. 1996; Bayley et al. 2007; Eschmann et al. 2010;). We do not know of any investigations of EMT partner familiarity.
To begin to understand the interaction of teams and EMS outcomes, we sought to characterize EMT partner familiarity in a sample of three EMS agencies.
METHODS
Study Design
We received approval from the University of Pittsburgh Institutional Review Board to use a case study design and review of administrative data from three EMS agencies. We selected this design given the exploratory nature of this research and expense and resources associated with multisite studies.
Data Source and Study Setting
We recruited a convenience sample of three EMS agencies (Agencies A–C) from the Midwest and northwest U.S. Census regions. We collected data related to their activities in 2008. Table 1 highlights the agency characteristics, including staffing, agency model/type, geography, and annual patient contacts.
Table 1.
Demographics of the Study Sample
| EMS Agency | |||
|---|---|---|---|
| A | B | C | |
| Size of workforce | |||
| <25 | |||
| 25–49 | n = 41 | ||
| 50–100 | n = 67 | n = 81 | |
| >100 | |||
| Staffing mix | |||
| All paid staff | X | X | |
| Mix of paid and volunteer staff | X | ||
| All volunteer staff | |||
| Self-described model type | |||
| Hospital based | X | X | |
| Gov't/third service | |||
| Private freestanding | X | ||
| Fire based | |||
| Service geography | |||
| Rural | X | ||
| Urban | X | X | |
| Annual patient contacts | |||
| ≤2,500 | |||
| 2,501–5,000 | |||
| 5,000–10,000 | X | X | |
| >10,000 | X | ||
EMS, Emergency Medical Service.
The three agencies have slightly different shift patterns and work scheduling processes. Agency A utilizes an 8-, 12-, and 24-hour shift schedule option maintained by a single supervisor. EMTs at this agency send shift requests directly to the supervisor. The supervisor then assigns shifts based on input from EMTs, the agency director, and changes in EMT availability. Agency B also utilizes an 8-, 12-, and 24-hour shift schedule. While some EMTs at Agency B are on rotating schedules, most must request a specific shift and schedule. Agency B's shift supervisor considers requests when assigning shift partners and gives priority to EMTs who need to make up hours due to absenteeism. Agency C utilizes a 12- and 24-hour shift schedule and assigns EMTs similarly to Agency B.
The total number of EMTs varied across EMS agency and ranged from 41 at Agency A to 81 at Agency C (Table 1). Agencies B and C employed an all-paid staff while EMTs at Agency A were a mix of paid and volunteer. Agencies B and C were hospital-based EMS models while Agency A was a private-freestanding service model. Two of the three agencies served a mostly urban area and have annual volumes between 5,000 and 10,000 patients. Agency C served a mostly rural area and has an annual volume of over 10,000 patients.
Measures and Data Collection
Standardized measures of partner familiarity for EMS are limited. We calculated four measures of EMT partner familiarity consistent with previous research of aviation crews (Smith-Jentsch et al. 2009). These measures included the annual mean shifts per EMT, mean number of different partnerships per EMT, rate of EMT partnerships per 10 shifts worked, and proportion of shifts that an EMT worked with same partner.
We based all calculations on information from EMS agency employee shift records and patient care reports retrieved by EMS agency officials from January 1, 2008 to December 31, 2008. Agency officials searched these records to identify “who worked with whom” (EMT partnerships/dyads) on all shifts over the study period. Officials validated partnerships against patient care reports when needed. Data were collected via a secure Internet-based data collection tool.
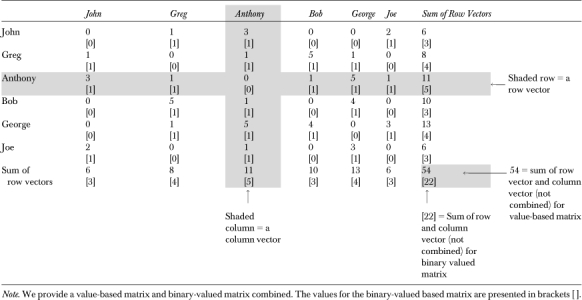
We stored all data in matrix format rather than conventional databases to account for the varied patterns and number of partnerships across agencies and individual employees. In these value-based matrices, individual cells contained the total number of times two EMTs worked as partners; their cumulative shifts worked together over 1 year. In our example matrix (Table 2), Anthony worked three shifts with John, one shift with Greg, one shift with Bob, five shifts with George, one shift with George, and one shift with Joe. We created symmetric matrices for each agency, with zeros along the diagonal representing zero shifts worked alone (without a partner). We also created binary-valued matrices to calculate measures related to EMT partnerships, apart from the number of shifts (e.g., mean number of different partnerships per EMT). Binary-valued matrices are similar in size and shape to value-based matrices with the one exception being the data contained within the cell. All cell values in binary-valued matrices are 0 or 1. We created binary-valued matrices by placing a 1 in the cells of value-based matrices containing nonzero values. A value of 1 was used to indicate when a pair of EMTs worked at least one shift together and 0 when the dyad recorded no shifts as partners. For example, in Table 2, we replaced the value of 5 for the Anthony and George partnership with a 1.
Table 2.
Example Matrix
 |
Statistical Analysis
For each agency, we used the value-based matrix with 12 months of EMT shift counts to calculate the annual number of scheduled shifts per agency. In example Table 2, this calculation is illustrated by dividing the row vector sum (54) by 2, producing 27. We used the same matrix to calculate the mean number of shifts per EMT by dividing the row vector sum by total agency employees.
For each agency, we used a 12-month binary-valued matrix to calculate the mean number of different partnerships. This calculation is illustrated in Table 2 by dividing the sum of row vectors[22] by total EMTs (n = 6). We calculated the rate of different EMT partners per 10 shifts worked by dividing the total number of partners by total shifts worked and multiplying that figure by 10. Using Table 2, we divide [5] partners for Anthony by 11 total shifts to compute a rate of 4.5 partners for every 10 shifts worked. Finally, we excluded EMTs with 0 shifts worked (n = 1) and calculated the proportion of an EMT's shifts that were spent with his or her most frequent partner. For each EMT, we divided the maximum number of shifts for a particular partnership by his or her total number of shifts.
For each agency, we calculated the mean, SD, minimum, maximum, and corresponding 95 percent confidence intervals for the number of shifts per EMT, number of different partnerships per EMT, rate of different partnerships per 10 shifts worked, and proportion of shifts worked with most frequent partner. We standardized two measures (number of different partnerships per EMT and rate of different partnerships per 10 shifts worked) to account for variations in size of agency and opportunities for EMT partnerships. We standardized these measures by dividing each EMT individual measure (e.g., the total number of different partnerships per annum) by the number of possible partners in an EMT's agency. For example, if EMT1234 in Agency A worked with 20 different partners over the study period, we would divide 20 by 40—one minus the total number of EMT employees (e.g., n = 41). Standardization addresses concerns that larger agencies have more partnership opportunities and potentially larger mean partnerships per EMT. With our sample of three EMS agencies (two of fairly similar size), we felt it inappropriate to construct models with agency size as a control/confounding variable. We did not standardize the mean number of shifts per EMT or the proportion of shifts worked with most frequent partner. These measures are dependent on shifts, not partnerships. Unlike the partnerships per EMT and rate of partnerships per 10 shifts worked, where we know the maximum possible number of unique partnerships, we do not know the maximum number of shifts an EMT can work. Standardization of these shift-specific measures would be based on incomplete information and produce potentially misleading results.
We compared our two standardized and two unstandardized measures across agencies using the Kruskal–Wallis test. We calculated means, SDs, minimum, and maximum values, and 95 percent confidence intervals for each measure. We used Bonferroni-corrected significance levels to account for multiple comparisons when the null hypothesis of no difference across agencies was rejected. We used UCINET version 6.205 and STATA/SE version 11.0 for all statistical analyses.
RESULTS
We present the standardized and unstandardized measures in Table 3. Below we present unstandardized figures and where applicable we present p-values corresponding to comparisons of standardized measures. Across all agencies, there were approximately 7,200 total EMT shifts with the maximum of 3,606 at Agency C. We identified wide variation in total number of shifts per EMT across EMS agencies (Table 3; p<.001). The mean number of shifts per EMT was similar for agencies A and C (95.9 versus 90.2), but different for Agencies A and B (95.9 versus 50.7; p<.001) and B and C (50.7 versus 90.2; p<.001).
Table 3.
Agency Shifts and EMT Familiarity
| Mean (SD) [Minimum, Maximum] (95% Confidence Interval) | ||||
|---|---|---|---|---|
| Overall (pooled) | Agency A | Agency B | Agency C | |
| Number of EMTs | N = 188 EMTs | N = 41 EMTs | N = 67 EMTs | N = 80 EMTs |
| Number of shifts | N = 7,268 | N = 1,965 | N = 1,697 | N = 3,606 |
| The mean no. of shifts per EMT | 77.3 (59.8)** | 95.9 (52.3) | 50.7 (40.8) | 90.2 (68.8) |
| [1, 229] | [6, 211] | [1, 171] | [1, 229] | |
| (68.7, 85.9) | (79.3, 112.4) | (40.7, 60.6) | (75.0, 105.3) | |
| Partnerships per EMT (unstandardized) | 19.3 (12.4) | 13.5 (5.5) | 18.8 (12.0) | 22.7 (14.2) |
| [1, 51] | [1, 27] | [1, 41] | [1, 51] | |
| (17.5, 21.1) | (11.7, 15.2) | (15.9, 21.7) | (19.6, 25.8) | |
| Standardized | NS0.29 (0.17) | 0.33 (0.13) | 0.28 (0.18) | 0.28 (0.18) |
| [0.01, 0.67] | [0.02, 0.67] | [0.01, 0.62] | [0.01, 0.64] | |
| (0.27, 0.32) | (0.29, 0.38) | (0.24, 0.33) | (0.24, 0.32) | |
| Rate of partnerships per 10 shifts worked (unstandardized) | 4.0 (2.7) | 1.9 (1.4) | 5.3 (2.7) | 4.0 (2.6) |
| [0.3, 10.0] | [0.3, 8.3] | [1.4, 10.0] | [1.1, 10.0] | |
| (3.6, 4.4) | (1.5, 2.4) | (4.6, 6.0) | (3.5, 4.6) | |
| Standardized | 0.06 (0.04)** | 0.05 (0.04) | 0.08 (0.04) | 0.05 (0.03) |
| [0.01, 0.21] | [0.01, 0.21] | [0.02, 0.15] | [0.01, 0.12] | |
| (0.05, 0.07) | (0.04, 0.06) | (0.07, 0.09) | (0.04, 0.06) | |
| Proportion of shifts worked with most frequent partner | 34.8%** | 37.9% | 31.4% | 36.1% |
| [6.2%, 100%] | [10%, 100%] | [8.6%, 100%] | [6.2%, 100%] | |
| (33.2%, 36.4%) | (34.6%, 41.2%) | (46.4%, 59.5%) | (33.6%, 38.6%) | |
Note. We offer the following interpretation of standardized measures. The 0.29 standardized mean number of partnerships per EMT can be interpreted as a measure of EMT partnership penetration—indicating that, on average, EMTs in these agencies worked with approximately 29% of all possible partners in the agency over 12 months. One may interpret 0.06 for the standardized rate of partnerships per 10 shifts worked as follows: on average, EMTs worked with one-sixteenth of all possible partners in the agency for every 10 shifts worked.
, Measures differ across agencies at the p<.001 level.
EMT, Emergency Medical Technician; NS, the measures do not differ across agencies, p>.05.
EMT Partner Familiarity
Across all agencies, EMTs worked with a mean of 19.3 (12.4) different EMT partners over 12 months (Table 3). The mean number of EMT partnerships did not differ across agencies after standardizing by size of agency (p = .328).
The rate of EMT partnerships per every 10 shifts worked was 4.0 (SD 2.7) and varied across EMS agencies after standardizing for size of agency (Table 3; p<.001). The minimum rate was 0.3 and is interpreted as three partners for every 100 shifts. The rate at Agency B was 2.7 times greater than the rate for Agency A (Table 3; p<.001) and 1.3 times greater than Agency C (p<.001). The rate at Agency C was twice that of Agency A, but was not significant.
The proportion of shifts that EMTs worked with their most frequent partner was 35 percent overall and varied across EMS agencies (Table 3; p<.001). The pairwise difference in proportions between Agencies A and B (37.9 versus 36.1 percent) was significant (p<.001), whereas the difference between B and C (5 percent) was not. The proportion of shifts worked with the most frequent partner decreased from 59 percent among EMTs that worked with ≤5 partners to 29 percent among EMTs that worked with >10 partners. Among EMTs that worked with more than 10 partners, the proportion varied across EMS agencies (p = .041).
DISCUSSION
Teams and teamwork are important throughout health care, with “many teams formed without much forethought … and many teams failing for any number of reasons” (Salas and Fiore 2004). We identified variations in EMT team formation and the limited amount of time that many have with one unique partner.
Prior studies of partner familiarity are limited. In a review of air-carrier accidents, the proportion of flights configured with pilot and copilot teams working on their first flight together ranged from 2.8 to 10.5 percent among four large and small air carriers (Board 1994). In a study of air-traffic control teams, the mean number of months teams of two or three worked together was 25.6 (range 3–95 months) (Smith-Jentsch et al. 2009). In a study of knee and hip surgeries, physicians, nurses, and other surgical teammates worked an average of 4.4 (SD 2.9) surgeries with any one partner over previous 5 years (Reagans, Argote, and Brooks 2005).
Our findings raise questions about EMT team development as a result of policies or procedures used to configure EMT teams. EMTs worked with >19 different partners annually and spent only one-third of all their work time with their most familiar partner. Do these patterns give EMTs enough time to develop norms and positive teamwork behavior? There is reason to believe the answer is no. EMS care is fast paced and delivered in uncontrollable environments. Teams of EMTs must rapidly recognize patient signs and symptoms and deliver stabilizing and often life-saving care. On every call, EMTs must form a general patient impression, assess patient mental status, obtain condition specific information from patient or bystanders, identify possible allergies, pertinent past medical history, medication and food intake, and events leading up to the illness or injury. The EMTs must evaluate vital signs, dress and bandage wounds, administer care, stabilize the patient, and transfer the patient without injury or adverse event. These actions must be executed quickly, efficiently, and with limited interruption. Unfortunately, most EMTs receive no or little training to skillfully engage in behaviors that can improve efficiency and reduce error (i.e., identifying a team leader, engaging in closed loop communication, or providing back-up assistance when partners fall behind). Traditional EMT education and training emphasizes individual, not teamwork competencies.
Newly formed teams and partners with a limited history are much less likely to perform as well as experienced teams (Board 1994; Harrison et al. 2003; Smith-Jentsch et al. 2009;). New partners may feel anxiety, confusion, or apprehension (Gersick 1988, 1989). EMTs in this study may experience such feelings 4 out of every 10 shifts. The actions and skills required to function as an effective partner may require lengthy learning curves. A new partner may be unclear about his/her partner's expectations and hesitant to speak up when necessary. Among new hires, probationary periods may limit role, responsibilities, and willingness to speak up and be actively involved (Reagans, Argote, and Brooks 2005). In agencies with a low safety culture, speaking up to a senior EMT set in his or her ways may be taboo and create an uncomfortable work experience. The quality of the first-time partnerships are important because they can set the tone for all the meetings that follow (Gersick 1988, 1989).
The study has several limitations. Our findings are limited to a case study design of three EMS agencies. Validation with a more representative and larger sample of EMS agencies is important. Second, the accuracy of our data may be decreased by undocumented changes in EMT partnerships right before a shift. We tried to address this by requesting use of multiple sources of data (i.e., roster records and patient care reports). To replicate our protocol with a larger sample, we recommend the addition of checks for accuracy and changes in the timing of data collection to weekly versus monthly. Third, the dyadic nature of our data means that observations are not nested within unique individuals, but rather nested within partnerships or dyads. The assumption of independence between subjects is violated. Fourth, we standardized several measures by size of agency workforce to facilitate comparing measures across our small sample of EMS agencies. In the ideal study, we would construct models for each outcome measure (e.g., number of different partners per EMT) with a sample of hundreds of differently sized EMS agencies. We would then utilize mixed models with agency size as a random effect. Findings would be interpreted as for every one unit change in agency size, the mean number of EMT partnerships—for example—increased/decreased by X units. Our study was exploratory in nature and aimed to provide a baseline characterization of patterns of partner familiarity utilizing a small convenient sample of EMS agencies. In our future research we will systematically sample agencies of all sizes.
CONCLUSIONS
Our findings indicate that on average an EMT works with 19 different partners over the course of the year and that there is significant variation in EMT partner familiarity across agencies. Given the literature on teams and safety, we suspect that these patterns contribute to poor EMS outcomes. Research on team structure and EMS outcomes is sorely needed.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Authors have no financial conflicts of interest. During the execution of this study, Dr. Patterson was supported by the Emergency Medicine Patient Safety Foundation (EMPSF) and Society for Academic Emergency Medicine (SAEM) Patient Safety Research Fellowship. Dr. Patterson is currently supported by a KL2 grant (KL2 RR024154) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on reengineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
REFERENCES
- Bayley R, Weinger M, Meador S, Slovis C. Impact of Ambulance Crew Configuration on Simulated Cardiac Arrest Resuscitation. Prehospital Emergency Care. 2007;12(1):62–8. doi: 10.1080/10903120701708011. [DOI] [PubMed] [Google Scholar]
- Board NTS. A Review of Flightcrew-Involved Major Accidents of U.S. Air Carriers, 1978 through 1990. Washington, DC: National Transportation Safety Board; 1994. [Google Scholar]
- Brown LH, Owens CFJ, March JA, Archino EA. Does Ambulance Crew Size Affect On-Scene Time or Number of Prehospital Interventions? Prehospital and Disaster Medicine. 1996;11(3):214–17. doi: 10.1017/s1049023x00042977. [DOI] [PubMed] [Google Scholar]
- Chidambaram L, Bostrom R. Group Development (I): A Review and Synthesis of Development Models. Group Decision and Negotiation. 1997;6(2):159–87. [Google Scholar]
- Corbett SW, Grange JT, Thomas TL. Exposure of Prehospital Care Providers to Violence. Prehospital Emergency Care. 1998;2(2):127–31. doi: 10.1080/10903129808958856. [DOI] [PubMed] [Google Scholar]
- Eschmann NM, Pirrallo RG, Aufderheide TP, Lerner EB. The Association between Emergency Medical Services Staffing Patterns and Out of Hospital Cardiac Arrest Survival. Prehospital Emergency Care. 2010;14(1):71–7. doi: 10.3109/10903120903349820. [DOI] [PubMed] [Google Scholar]
- Freeman VA, Slifkin R, Patterson PD. Recruitment and Retention in Rural and Urban EMS: Results from a National Survey of Local EMS Directors. Journal of Public Health Management and Practice. 2009;15(3):246–52. doi: 10.1097/PHH.0b013e3181a117fc. [DOI] [PubMed] [Google Scholar]
- Gersick CJG. Time and Transition in Work Teams: Toward a New Model of Group Development. Academy of Managed Journal. 1988;31(1):9–41. [Google Scholar]
- Gersick CJG. Marking Time: Predictable Transitions in Task Groups. Academy of Managed Journal. 1989;32(2):274–309. [Google Scholar]
- Grange JT, Corbett SW. Violence against Emergency Medical Services Personnel. Prehospital Emergency Care. 2002;6(2):186–90. doi: 10.1080/10903120290938526. [DOI] [PubMed] [Google Scholar]
- Harrison DA, Mohammed S, McGrath JE, Florey AT, Vanderstoep SW. Time Matters in Team Performance: Effects of Member Familiarity, Entrainment, and Task Discontinuity on Speed and Quality. Personnel Psychology. 2003;56(3):633–69. [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies of Science; 2000. [PubMed] [Google Scholar]
- Lemieux-Charles L, McGuire WL. What Do We Know about Health Care Team Effectiveness? A Review of the Literature. Medical Care Research and Review. 2006;63(3):263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- Maguire BJ, Hunting KL, Guidotti TL, Smith GS. Occupational Injuries among Emergency Medical Services Personnel. Prehospital Emergency Care. 2005;9(4):405–11. doi: 10.1080/10903120500255065. [DOI] [PubMed] [Google Scholar]
- Maguire BJ, Hunting KL, Smith GS, Levick NR. Occupational Fatalities in Emergency Medical Services: A Hidden Crisis. Annals of Emergency Medicine. 2002;40(6):625–32. doi: 10.1067/mem.2002.128681. [DOI] [PubMed] [Google Scholar]
- Reagans R, Argote L, Brooks D. Individual Experience and Experience Working Together: Predicting Learning Rates from Knowing Who Knows What and Knowing How to Work Together. Management Science. 2005;51(6):869–81. [Google Scholar]
- Reichard AA, Jackson LL. Occupational Injuries among Emergency Responders. American Journal of Industrial Medicine. 2010;53(1):1–11. doi: 10.1002/ajim.20772. [DOI] [PubMed] [Google Scholar]
- Rittenberger JC, Beck PW, Paris PM. Errors of Omission in the Treatment of Prehospital Chest Pain Patients. Prehospital Emergency Care. 2005;9(1):2–7. doi: 10.1080/10903120590891688. [DOI] [PubMed] [Google Scholar]
- Salas E, Fiore SM. Why Team Cognition? An Overview. In: Salas E, Fiore SM, editors. Team Cognition: Understanding the Factors That Drive Process and Performance. p. 3. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Smith-Jentsch KA, Kraiger K, Cannon-Bowers JA, Salas E. Do Familiar Teammates Request and Accept More Backup? Transactive Memory in Air Traffic Control. Human Factors. 2009;51(2):181–92. doi: 10.1177/0018720809335367. [DOI] [PubMed] [Google Scholar]
- Tuckman BW. Developmental Sequence in Small Groups. Psychological Bulletin. 1965;63(6):384–99. doi: 10.1037/h0022100. [DOI] [PubMed] [Google Scholar]
- Wang HE, Fairbanks RJ, Shah MN, Abo BN, Yealy DM. Tort Claims and Adverse Events in Emergency Medical Services. Annals of Emergency Medicine. 2008;52(3):7. doi: 10.1016/j.annemergmed.2008.02.011. [DOI] [PubMed] [Google Scholar]
- Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedic Intubation Errors: Isolated Events or Symptoms of a Larger Problem? Health Affairs (Millwood) 2006;25(2):501–9. doi: 10.1377/hlthaff.25.2.501. [DOI] [PubMed] [Google Scholar]
- Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in Cardiopulmonary Resuscitation from Paramedic Endotracheal Intubations. Annals of Emergency Medicine. 2009a;54(5):645–52. doi: 10.1016/j.annemergmed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Wang HE, Weaver MD, Abo BN, Kaliappan R, Fairbanks RJ. Ambulance Stretcher Adverse Events. Quality and Safety in Health Care. 2009b;18(3):213–16. doi: 10.1136/qshc.2007.024562. [DOI] [PubMed] [Google Scholar]
- Williams KA, Rose WD, Simon R. Teamwork in Emergency Medical Services. Air Medical Journal. 1999;18(4):149–53. doi: 10.1016/s1067-991x(99)90028-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


