Abstract
Purpose
To assess patient navigation (PN) utilization and its impact on treatment interruptions and clinical trial enrollment among American Indian (AI) cancer patients.
Methods
Between February 2004 and September 2009, 332 AI cancer patients received PN services throughout cancer treatment. The PN program provided culturally-competent navigators to assist patients with navigating cancer therapy, obtaining medications, insurance issues, communicating with medical providers, and travel and lodging logistics. Data on utilization and trial enrollment were prospectively collected. Data for a historical control group of 70 AI patients who did not receive PN services were used to compare treatment interruptions among those undergoing PN during curative radiation therapy (subgroup of 123 patients).
Results
The median number of contacts with a navigator was 12 (range, 1-119). The median time spent with the navigator at first contact was 40 minutes (range 10-250 min.) and 15 min for subsequent contacts. Patients treated with radiation therapy with curative intent who underwent PN had fewer days of treatment interruption (mean, 1.7 days; 95% CI, 1.1-2.2 days) than historical controls who did not receive PN services (mean, 4.9 days; 95% CI, 2.9-6.9 days). Of the 332 patients, 72 (22%; 95% CI, 17-26%) were enrolled on a clinical treatment trial or cancer control protocol.
Conclusions
PN was associated with fewer treatment interruptions and relatively high rates of clinical trial enrollment among AI cancer patients compared to national reports.
INTRODUCTION
It is well-established that cancer-related health disparities exist with respect to race/ethnicity and socioeconomic status, 1-5 and American Indians (AI) in the Northern Plains region of the US exhibit some of the highest cancer mortality rates in the nation. 6, 7 Investigators have demonstrated that reasons underpinning health disparities among vulnerable populations are multi-factorial. 2, 8, 9 Studies have shown lower rates of screening utilization among AIs, 6, 10-12 as well as higher rates of presenting to medical care with advanced stages of cancer at diagnosis for AIs in this region. 13 In addition, AI cancer patients in the Northern Plains, where some of the largest reservation-base AI communities are located, demonstrate lack of trust of health care providers and hospitals,14 and negative attitudes about cancer treatment.15 American Indians in the Northern Plains reside in some of the poorest census tracts in the US, with almost half of individuals living below the federal poverty level and the unemployment rate at approximately 80% on some reservations.16 Furthermore, the Indian Health Service (I.H.S.) which provides health services to enrolled tribal members has been chronically under-funded thus hobbling a primary source of health care delivery for this vulnerable population. 17-19
As the field of health disparities research evolves from one of defining the extent and causes of disparate health outcomes to solutions to health inequities, patient navigation (PN) has emerged as a potential strategy to mitigate access barriers in targeted populations. The early model for cancer PN, established by Freeman and colleagues in Harlem, New York in the early 1990’s,20, 21 showed improved 5-yr survival (from 39% to 70%) for breast cancer patients in a low-income inner city population. Since that time multiple investigators have shown improvement in cancer-related health outcomes after implementation of PN services among various populations. 22-28 Most cancer PN studies have focused on increasing screening rates among minority populations or decreasing the time intervals between the various critical points in early cancer management such as that between detection of a screening test abnormality through diagnosis and initiation of cancer treatment. 24, 27, 29 Relatively few studies provide data on PN during cancer treatment itself.30 Data are needed on the intensity and nature of PN utilization during cancer treatment, and the impact of navigation on treatment-related outcomes. For example, treatment adherence may be improved by PN. This possibility is especially relevant for patients undergoing curative irradiation, a situation where treatment interruptions have been shown to impact survival and recurrence outcomes. 31-33 Another potential benefit of PN may be the ability to boost clinical trial enrollment among minority populations, through the presence of a culturally competent navigator to help establish trust and assist in identifying eligible patients which have typically been underrepresented in clinical trial participation.34, 35
In 2003, a review of the Rapid City Regional Hospital’s (Rapid City, South Dakota) tumor registry (from 1990-2003) revealed that AI cancer patients presented with disproportionately high rates of advanced-stage malignancy.13, 36 Subsequent to these findings a culturally-tailored PN program was implemented to assist AI cancer patients through the cancer care continuum from diagnosis through follow-up after cancer treatment completion. The purpose of this study is to report upon patient navigation utilization during cancer treatment and to evaluate potential impacts on clinical care.
METHODS
Study population
Between January 2004 and September 2009, 375 AI cancer patients presented to Rapid City Regional Hospital (RCRH) Cancer Care Institute (CCI) in Rapid City, South Dakota and were approached and offered the services of a culturally competent patient navigator. Of those, 43 patients (11%) refused patient navigation for the following reasons: 39 felt that PN was not necessary; 2 patients did not trust a patient navigator to be involved in their care; and 2 patients did not specify a reason. The remaining 332 AI cancer patients were enrolled on a PN protocol for PN throughout cancer treatment. Patients were identified and enrolled on the protocol at first visit to CCI if at all possible or as soon as possible if eligibility capture was not established at first visit. Race was self-identified by the patient.
All AI patients presenting to RCRH with a diagnosis of malignancy were eligible to participate. Rapid City Regional Hospital serves as the major secondary and tertiary cancer care provider for more than 70,000 adult AIs in the region which includes the Oglala Sioux Tribe (Pine Ridge), Cheyenne River Sioux Tribe, Rosebud Sioux Tribe, and the Rapid City AI population. All AI patients in this study reside in one of these communities, but eligibility for participation was not restricted to specific tribal affiliation. The RCRH’s Investigation Review Board (IRB) granted approval to conduct the PN intervention and study. In addition, the protocol was also approved by the following entities prior to initiation: the IRB of the Aberdeen Area Indian Health Service (IHS), Aberdeen Area IHS Tribal Chairman’s Health Board, Tribal Councils and Health Departments (Cheyenne River Sioux Tribe, Oglala Sioux Tribe, Rosebud Sioux Tribe), and IHS Hospital Chief Executive Officers (Cheyenne River IHS Hospital, Pine Ridge (Oglala) IHS Hospital, Rapid City Sioux San IHS Hospital, and Rosebud IHS Hospital).
Patient navigation program
In 2003, RCRH was awarded a Cancer Disparities Research Partnership (CDRP) grant to study cancer-related disparities previously documented in this vulnerable population 6, 7, 13 and to increase clinical trial availability and enrollment in this medically underserved region.37 Since that time a multifaceted, community-based participatory research and intervention effort, called the Walking Forward Program,13, 36, 38, 39 has been developed to explore root causes of disparities, increase cancer screening and education, enroll patients on and educate them about clinical trials, and to provide comprehensive, culturally-tailored PN throughout cancer treatment. Through this effort, AI cancer patients were offered PN services whereby patients were assisted in navigating the medical system by trained, culturally-competent staff to serve as advocates through the cancer care continuum after cancer diagnosis. The patient navigators assist with coordinating appointments, insurance issues, following up on tests, obtaining medications and specialty services or devices, facilitating transportation and lodging, and offer psycho-social support during treatment. In addition to the hospital-based navigators, the navigation program also includes community research representatives (CRR) who work closely with the hospital staff and are embedded in the surrounding AI communities provide cancer education, network with local heath resources, and serve as liaisons between the cancer center, hospital-based patient navigators, and patients or tribal governments. Patient education materials were translated into the Lakota language. The cancer center staff members involved in this effort were either closely connected with or are members of the American Indian communities served by this program. More details regarding the development of this PN program have been described elsewhere in the literature. 39, 40
Utilization data collection and statistical analysis
We prospectively collected data regarding needs addressed and services rendered for each contact with the patient navigator. The navigator completed a contact sheet at each interaction with a patient whether it was by phone or in person. The barriers that were addressed and time spent with the patient were recorded for each contact. Data were tracked as patients moved through the cancer care continuum from diagnosis (if it occurred at CCI) and evaluation through follow-up/surveillance after treatment completion. Contact with the navigator occurred either in person, on the telephone (except for the initial contact, which was always in person), or in some cases the navigator went to homes or hotel rooms of patients to offer assistance when patients were too sick to come to CCI for scheduled treatments. In addition, patient demographics, cancer site, stage and treatment information were abstracted from the medical record or obtained at enrollment interviews. Data were de-identified, and all analyses were performed using SPSS version 17.0 statistical software (Apache Software Foundation). Analysis of variance was performed to test for difference between means. Confidence intervals (CI) were calculated for proportions and means where appropriate and used along with proportions and means to describe general characteristics.
Analysis of treatment interruptions
We performed an analysis of radiation treatment (RT) delays for patients treated with RT with curative intent. Those treated with curative intent were the focus of this analysis because data exists that shows RT treatment delays can result in compromise of cancer control and survival outcomes for some cancers that are curable at presentation.31-33 Details of cancer treatment were compiled by a review of the radiation therapy records and hospital chart. Complete data regarding chemotherapy details and interruptions were not available to our staff members who are housed in the department of radiation oncology; therefore, analyses regarding chemotherapy interruptions were not performed as part of this study. For the purposes of comparison, 72 consecutive AI patients treated with RT with curative intent at CCI between April 1991 and April 2004 and who did not undergo PN during treatment were identified to serve as a control group for comparison of days of RT treatment interruptions. Two patients did not complete RT and their data were not analyzed. For the remaining 70 patients (68 treated prior to the availability of PN services and 2 who refused PN services early in the program’s existence), RT charts were retrospectively reviewed to ascertain how many days of treatment delay occurred as well as whether the treatment delay was due to machine maintenance or repair versus other reasons (e.g., weather or patient cancelled for other reasons). Delays due to RT machine maintenance or repair was not considered a day of treatment delay.
Clinical trial availability
Rapid City Cancer Care Institute has primary membership and access to clinical trials through the North Central Cancer Treatment Group (NCCTG). The center also has clinical trial access as an affiliate of the Radiation Therapy Oncology Group (RTOG), Eastern Cooperative Oncology Group (ECOG), National Surgical Adjuvant Breast and Bowel Project (NSABP), Gynecologic Oncology Group (GOG) and Cancer Therapy Evaluation Program (CTEP). In addition, cancer treatment trials were written for prostate and breast cancer under the auspices of the CDRP grant program. During the time of the study approximately 75 cancer-related clinical trials were open. Clinical trial enrollment data were prospectively tracked for all navigated patients.
RESULTS
Patient and cancer-specific characteristics for the study population
Table 1 shows patient characteristics among navigated patients. The largest percentage of patients resides on the Pine Ridge (Oglala Sioux) reservation which is located approximately 100 miles from Rapid City (over 2 hours by car if no inclement weather). The median distance lived from CCI (one way) for all patients was 121 miles (range, 10-444 miles), and it should be noted that road conditions on the reservations are such that travel is slower than that possible on average U.S. highways, even in the absence of inclement weather. The primary payer source for medical bills was Medicare for a third of patients and the next most common primary payer was the Indian Health Service in 25% of patients. Very few patients did not speak English (2%), but 36% of patients did speak the Lakota language.
Table 1.
Sociodemographic characteristics of navigated patients. 332 patients undergoing patient navigation between 2/2004 and 9/2009
| Characteristic | number | Percent |
|---|---|---|
| Total number of patients navigated | 332 | |
| Gender | ||
| Male | 151 | 45 % |
| Female | 181 | 55% |
| Median age | 60 years | |
| Range | 16-89 years | |
| Reservation/Tribal community geographical affiliation (not tribal enrollment affiliation) | ||
| Pine Ridge/Oglala Sioux | 160 | 49 % |
| Rosebud Sioux | 61 | 19 % |
| Cheyenne River | 54 | 16 % |
| Standing Rock Sioux | 3 | 1 % |
| Rapid City (Sioux San) | 33 | 10 % |
| Other tribal affiliation | 18 | 6 % |
| Distance lived from cancer center (one way) | ||
| Median | 121 miles | |
| Range | 10-444 miles | |
| Primary payor of medical bills | ||
| Medicare | 110 | 33 % |
| Indian Health Service | 82 | 25 % |
| Medicaid | 51 | 16 % |
| VA | 32 | 10 % |
| Private insurer | 52 | 16 % |
| Uninsured | 2 | 1 % |
| No of patients who do not speak English | 5 | 2% |
| Speak Lakota language | ||
| Yes | 117 | 36% |
| No | 133 | 40% |
| Missing data | 79 | 24% |
The majority of patients, 205 (62%), underwent cancer treatment with curative intent, and 112 (34%) underwent palliative treatment, corresponding to the similar percentage of patients who presented with stage IV disease (37%). The remaining 15 (5%) did not have their treatment intent established before discontinuing care at CCI (e.g., underwent only consultation or one visit at CCI but sought PN services at the time of that consult.) At the time of this analysis 113 (34%) patients had died, 76 (67%) of whom were Stage III or IV at diagnosis.
Patient navigation utilization
Patients were most commonly referred or recruited to the PN program by a CRR or PN program staff member within the hospital (119 patients, 36%); or by their treating physician or oncology nurse (89 patients, 27%). The remaining 124 (37%) patients sought PN through self-referral or referral by someone other than hospital or grant program staff. All 332 patients had at least one visit with a patient navigator and the median time spent with the navigator at initial contact was 40 minutes (range, 10-250 minutes; mean 45 minutes; mode 60 minutes). The median number of contacts with a navigator per patient was 12 (range, 1-119 contacts.) The mode number of contacts was one contact, with 39 patients (12%) having only one contact with a PN. The median time spent with the navigator for subsequent contacts with a navigator after the initial visit was 15 minutes.
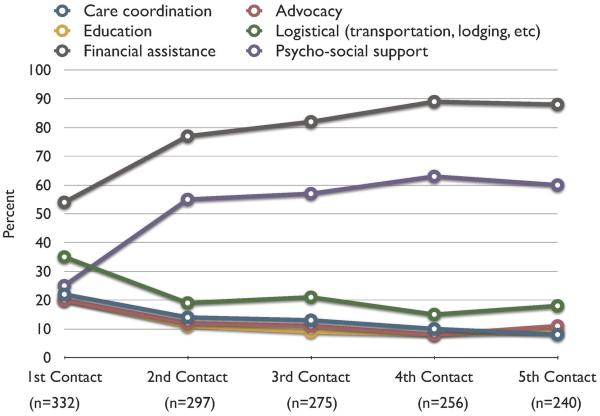
For the initial PN contact, the majority of patients were referred to PN for financial assistance (54%) or logistical support, e.g. travel and lodging help (35%). Other reasons included (> 1 reason possible): psycho-social support (35%), care coordination (22%), advocacy (20%), or education (20%). Figure 1 illustrates the reasons for accessing PN services for subsequent visits through the first five contacts with a PN. Generally, a decreasing proportion of patients accessed a PN for help with case management or care coordination after the first visit, but requests for help with financial assistance increased after the first visit. Requests for psycho-social support also increased over the first five contacts with the PN. A higher proportion of patients requested help with advocacy or cancer care education during the first contact with the PN than at subsequent visits through the first five contacts.
Figure 1. Trends in reason for accessing the patient navigator services.
The chart shows the percent of patients seeking various types of assistance from patient navigator through the first five contacts with the navigator.
Table 2 shows cancer and treatment related characteristics of the study population. Patients undergoing RT had more contacts with a navigator than those not receiving RT (mean, 25 vs. 13 contacts, respectively; p=0.0001), as did those receiving chemotherapy vs. those who did not (mean, 24 vs. 15 contacts, respectively; p=0.001). Patients who received both chemotherapy and RT also had more encounters with a navigator than those not receiving both modalities (mean, 30 vs. 16 contacts, respectively; p=0.0001). Patients undergoing curative treatment had an average of 21 contacts with a navigator compared to 17 contacts for patients receiving palliative treatment (p=0.02).
Table 2.
Cancer patient and treatment-related characteristics of the 332 navigated patients
| Characteristic | number | Percent |
|---|---|---|
| Type of cancer | ||
| Breast | 74 | 23% |
| Lung | 50 | 15% |
| Prostate | 42 | 13% |
| Colo-rectal | 42 | 13% |
| Hematologic | 26 | 8% |
| Gynecologic | 20 | 6% |
| Head and neck | 21 | 6% |
| Gastric/Pancreas/hepatocellular | 15 | 5% |
| Non-prostate GU (renal, penile, testicular) | 18 | 5% |
| Sarcoma/Skin | 5 | 2% |
| Brain | 5 | 2% |
| Unknown primary site | 7 | 2% |
| Thyroid | 4 | 1% |
| Stage at enrollment into PN program* | ||
| In situ disease | 7 | 2% |
| Stage I | 40 | 12% |
| Stage II | 81 | 24% |
| Stage III | 66 | 20% |
| Stage IV | 92 | 37% |
| Radiation therapy received/planned | 200 | 60% |
| At CCI | 188 | 56% |
| At another facility | 12 | 4% |
| Treatment intent for those receiving RT at CCI | ||
| Curative | 129 | 69% |
| Palliative | 59 | 31% |
| Chemotherapy received/planned | 161 | 49% |
| Chemo received outside CCI | 27 | 8% |
| Chemo received at CCI | 134 | 41% |
| Pt underwent surgery for their cancer | ||
| Yes | 167 | 51% |
| No | 141 | 43% |
| Missing | 21 | 6% |
Treatment interruptions
For the historical control group of 70 AI pts treated curatively but who did not receive PN during their treatment, the average number of treatment days missed was 4.9 days, 95% CI 2.9-6.9 (range, 0-43 days). Of the 332 navigated patients, 188 received RT at CCI. Of these, 129 were treated with curative intent, 59 were treated with palliative intent. Of the 129 pts undergoing RT with curative intent, 6 did not complete their radiation treatment course. For the remaining 123 patients treated with curative RT, mean number of days of treatment delay=1.7, 95% CI 1.1-2.2 (range, 0-20).The mean number of days missed for the two groups was statistically significant (p=0.0001) (Table 3). There was no significant difference in the proportion of patients who did not complete treatment (p > 0.05). The proportion of days missed in each group due to weather was not significantly different (4% for the control group and 5% for the navigated group, p>0.05)
Table 3.
Days of treatment interruption for American Indian patients undergoing curative radiation therapy
| N | Average days of treatment interruption |
95% CI (days) | |
|---|---|---|---|
| Historical controls (no patient navigation) |
70 | 4.9 | 2.9-6.9 |
| Patients with patient navigation during treatment |
123 | 1.7 | 1.1-2.2 |
CI=confidence intervals
Clinical trial and protocol enrollment
Among the 332 patients enrolled on the patient navigator protocol, 72 (22%; 95%, CI 17-26%) were enrolled on a clinical treatment trial or cancer control protocol. Specifically, 50 patients participated in a molecular genetic study for presence of ataxia-telangectasia mutation (ATM); 17 were enrolled clinical treatment trial (10 of these were enrolled on a cooperative group trial); and 5 patients were enrolled on both the ATM study and a clinical treatment trial.
DISCUSSION
In this study we demonstrate that American Indian cancer patients receiving PN services while undergoing curative RT as part of their cancer treatment have significantly fewer RT interruptions than their historical counterparts who did not undergo PN. Furthermore, our data reveal a high rate of clinical trial enrollment among AI cancer patients receiving PN services when compared to previous studies which have shown low rates (<1%) of clinical trial participation for AIs. 34, 35, 41 We also describe PN utilization patterns for AI patients receiving cancer treatment to provide insight into the resources necessary to provide cancer treatment navigation services to this or a similar population. Specifically, our study contributes unique information about the number of navigator-patient interactions, the time resources typical of these interactions, and the types of services requested in these interactions during cancer treatment for a population with significant health access barriers. Patients who underwent more intensive treatment regiments tended to more heavily utilize PN services.
Much of the PN literature addressing care of cancer patients focuses on increasing screening incidence and/or decreasing intervals between screening and diagnostic management of initiation of treatment for various cancers,28-30, 42, 43 and most studies do show improvement in the corresponding outcomes when PN is available. American Indians specifically have been shown to benefit from PN in the setting of facilitating screening and timely diagnostic follow-up.29, 44 However, few studies report upon the role of PN after a patient is diagnosed and undergoing the rigors of cancer treatment, 30, 45 arguably a time when patients may experience more barriers due logistical complexities and financial burden of receiving many weeks or months of treatment e.g., RT or chemotherapy. Some of the reports that have been published on PN during cancer treatment show improvement in patient satisfaction or decrease in barriers to care.46, 47 Ell and colleagues 24 showed that treatment adherence was improved compared to previous studies among patients who were randomized to either enhanced usual care (written resource navigation information) or active PN, although there was no statistical difference between the two navigation approaches. Only one other study offers utilization data regarding the types of barriers addressed and the amount of time navigators spend with cancer patients.48
Our finding of fewer treatment interruptions for patients undergoing curative RT is one that has important implications for this population that has been shown to have disparately high cancer mortality. It has been demonstrated that prolonged RT interruption is a predictor for loco-regional relapse among patients treated for head and neck cancers.32, 33 Similarly, it has been established that prolongation of the RT course during treatment for cervical cancer—a disease that disproportionately affects poor and minority women, and for which AI women in the Northern plains have the highest incidence and mortality 6, 49-- is associated with increased risk for local recurrence and poorer survival outcomes.31 Patient navigation, in this study, seems to offer an effective strategy to mitigate barriers that may prolong definitive cancer treatment.
Multiple studies have indicated that clinical trial participation among AI cancer patients is low with trial accrual rates of < 1%.34, 35, 41 Reasons underpinning low minority participation in clinical trials are multi-factorial and may differ across regions as well as between racial/ethnic groups.50, 51 In this region, it has previously been shown that AI cancer patients exhibit relatively high rates of medical mistrust and dissatisfaction with prior health care received.14 Our PN program specifically targets health access barriers in this population and seeks to address them in a culturally-sensitive manner while partnering with tribal communities. This effort toward establishing rapport with AI patients and communities to meet their needs may account for our relatively higher proportion of AI patients willing to enroll on clinical trials.
Our study supports the role of PN in addressing health access barriers to cancer treatment, but it does so with certain limitations. First, our study is not a randomized trial and our analyses did not include a temporally parallel control group against which to compare outcomes. To ensure community-based participation and engagement it simply was not feasible for the purposes of comparison to deny half of AI patients the types of logistical support, financial assistance, and one-on-one advocacy offered by our navigators. In other words, community engagement necessary for the implementation of our effort might have been hindered if we had attempted to provide these services to fewer than all of the patients who desired PN services given the high level of need in the community being served.
More investigation is needed into the impact of PN,30, 45 and a coordinated, national effort is underway to provide critical insight into the role of PN in cancer care delivery as well as its cost-effectiveness. 52, 53 Until such data are available, data on working models that deliver care effectively via PN provide guidance that can be developed and tailored to various populations.
In conclusion, we have shown that PN is associated with fewer treatment interruptions among AI patients receiving curative RT for their cancer. We have also observed a high rate of clinical trial participation among AI, which have historically been underrepresented in clinical trial research. Furthermore, we characterize utilization specifics for our program to provide insight into resources entailed in administering a PN program in a regional health care center that provides health care to an underserved population. Further research is needed, not only into the cost-effectiveness of PN, but into other metrics of quality of care that may be improved with PN during cancer treatment.
Acknowledgments
This research was supported in part by National Institutes of Health/NCI grant # 5U56CA99010 (to D.G.P.). The opinions expressed in this paper are those of the author(s) and do not necessarily reflect the views of the National Cancer Institute or the National Institutes of Health.
REFERENCES
- 1.Haynes M, Smedley B. The unequal burden of cancer: an assessment of NIH research and programs for ethnic minorities and themedically underserved. National Academy Press; 1999. [PubMed] [Google Scholar]
- 2.Geiger H. Racial and ethnic disparities in diagnosis and treatment: a review of the evidence and consideration of causes. In: Smedley B, Smith A, Nelson A, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine: National Academies Press; Washington DC: 2003. pp. 415–54. [PubMed] [Google Scholar]
- 3.Smedley B, Stith A, Nelson A. Unequal Treatment:: Confronting Racial and Ethnic Disparities in Health Care. National Academy Press; 2003. [PubMed] [Google Scholar]
- 4.Freeman HP. Cancer in the socioeconomically disadvantaged. CA Cancer J Clin. 1989;39(5):266–88. doi: 10.3322/canjclin.39.5.266. [DOI] [PubMed] [Google Scholar]
- 5.Wilson RT, Adams-Cameron M, Burhansstipanov L, Roubidoux MA, Cobb N, Lynch CF, et al. Disparities in breast cancer treatment among American Indian, Hispanic and non-Hispanic White Women Enrolled in Medicare. J Health Care Poor Underserved. 2007;18(3):648–64. doi: 10.1353/hpu.2007.0071. [DOI] [PubMed] [Google Scholar]
- 6.Espey DK, Wu XC, Swan J, Wiggins C, Jim MA, Ward E, et al. Annual report to the nation on the status of cancer, 1975-2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110(10):2119–52. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- 7.Espey D, Paisano R, Cobb N. Cancer Mortality Among American Indians and Alaska Natives: Regional Differences, 1994-1998. Indian Health Service; 2003. [Google Scholar]
- 8.Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. Jama. 1998;279(22):1801–7. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- 9.Blackman DJ, Masi CM. Racial and ethnic disparities in breast cancer mortality: are we doing enough to address the root causes? J Clin Oncol. 2006;24(14):2170–8. doi: 10.1200/JCO.2005.05.4734. [DOI] [PubMed] [Google Scholar]
- 10.Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 11.Coughlin SS, Uhler RJ, Blackman DK. Breast and cervical cancer screening practices among American Indian and Alaska Native women in the United States, 1992-1997. Prev Med. 1999;29(4):287–95. doi: 10.1006/pmed.1999.0537. [DOI] [PubMed] [Google Scholar]
- 12.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97(6):1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 13.Petereit DG, Rogers D, Govern F, Coleman N, Osburn CH, Howard SP, et al. Increasing access to clinical cancer trials and emerging technologies for minority populations: the Native American Project. J Clin Oncol. 2004;22(22):4452–5. doi: 10.1200/JCO.2004.01.119. [DOI] [PubMed] [Google Scholar]
- 14.Guadagnolo BA, Cina K, Helbig P, Molloy K, Reiner M, Cook EF, et al. Medical mistrust and less satisfaction with health care among Native Americans presenting for cancer treatment. J Health Care Poor Underserved. 2009;20(1):210–26. doi: 10.1353/hpu.0.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guadagnolo BA, Cina K, Helbig P, Molloy K, Reiner M, Cook EF, et al. Assessing cancer stage and screening disparities among Native American cancer patients. Public Health Rep. 2009;124(1):79–89. doi: 10.1177/003335490912400111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pine Ridge CDP. South Dakota-DP-3 . Profile of Selected Economic Characteristics. US Census Bureau; 2000. [Google Scholar]
- 17.Lillie-Blanton M, Roubideaux Y. Understanding and addressing the health care needs of American Indians and Alaska Natives. Am J Public Health. 2005;95(5):759–61. doi: 10.2105/AJPH.2005.063230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roubideaux Y. Perspectives on American Indian health. Am J Public Health. 2002;92(9):1401–3. doi: 10.2105/ajph.92.9.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zuckerman S, Haley J, Roubideaux Y, Lillie-Blanton M. Health service access, use, and insurance coverage among American Indians/Alaska Natives and Whites: what role does the Indian Health Service play? Am J Public Health. 2004;94(1):53–9. doi: 10.2105/ajph.94.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3(1):19–30. [PubMed] [Google Scholar]
- 21.Oluwole SF, Ali AO, Adu A, Blane BP, Barlow B, Oropeza R, et al. Impact of a cancer screening program on breast cancer stage at diagnosis in a medically underserved urban community. J Am Coll Surg. 2003;196(2):180–8. doi: 10.1016/S1072-7515(02)01765-9. [DOI] [PubMed] [Google Scholar]
- 22.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 Suppl):359–67. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 23.Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: a randomized clinical trial. Prev Med. 2007;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Ell K, Vourlekis B, Xie B, Nedjat-Haiem FR, Lee PJ, Muderspach L, et al. Cancer treatment adherence among low-income women with breast or gynecologic cancer: a randomized controlled trial of patient navigation. Cancer. 2009;115(19):4606–15. doi: 10.1002/cncr.24500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gabram SG, Lund MJ, Gardner J, Hatchett N, Bumpers HL, Okoli J, et al. Effects of an outreach and internal navigation program on breast cancer diagnosis in an urban cancer center with a large African-American population. Cancer. 2008;113(3):602–7. doi: 10.1002/cncr.23568. [DOI] [PubMed] [Google Scholar]
- 26.Frelix GD, Rosenblatt R, Solomon M, Vikram B. Breast cancer screening in underserved women in the Bronx. J Natl Med Assoc. 1999;91(4):195–200. [PMC free article] [PubMed] [Google Scholar]
- 27.Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85(1):114–24. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Christie J, Itzkowitz S, Lihau-Nkanza I, Castillo A, Redd W, Jandorf L. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008;100(3):278–84. doi: 10.1016/s0027-9684(15)31240-2. [DOI] [PubMed] [Google Scholar]
- 29.Dignan MB, Burhansstipanov L, Hariton J, Harjo L, Rattler T, Lee R, et al. A comparison of two Native American Navigator formats: face-to-face and telephone. Cancer Control. 2005;12(Suppl 2):28–33. doi: 10.1177/1073274805012004S05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petereit DG, Sarkaria JN, Chappell R, Fowler JF, Hartmann TJ, Kinsella TJ, et al. The adverse effect of treatment prolongation in cervical carcinoma. Int J Radiat Oncol Biol Phys. 1995;32(5):1301–7. doi: 10.1016/0360-3016(94)00635-X. [DOI] [PubMed] [Google Scholar]
- 32.McCloskey SA, Jaggernauth W, Rigual NR, Hicks WL, Jr., Popat SR, Sullivan M, et al. Radiation treatment interruptions greater than one week and low hemoglobin levels (12 g/dL) are predictors of local regional failure after definitive concurrent chemotherapy and intensity-modulated radiation therapy for squamous cell carcinoma of the head and neck. Am J Clin Oncol. 2009;32(6):587–91. doi: 10.1097/COC.0b013e3181967dd0. [DOI] [PubMed] [Google Scholar]
- 33.Rades D, Stoehr M, Kazic N, Hakim SG, Walz A, Schild SE, et al. Locally advanced stage IV squamous cell carcinoma of the head and neck: impact of pre-radiotherapy hemoglobin level and interruptions during radiotherapy. Int J Radiat Oncol Biol Phys. 2008;70(4):1108–14. doi: 10.1016/j.ijrobp.2007.07.2380. [DOI] [PubMed] [Google Scholar]
- 34.Sateren WB, Trimble EL, Abrams J, Brawley O, Breen N, Ford L, et al. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. J Clin Oncol. 2002;20(8):2109–17. doi: 10.1200/JCO.2002.08.056. [DOI] [PubMed] [Google Scholar]
- 35.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. Journal of the American Medical Association. 2004;291(22):2720–6. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 36.Rogers D, Petereit DG. Cancer disparities research partnership in Lakota Country: clinical trials, patient services, and community education for the Oglala, Rosebud, and Cheyenne River Sioux tribes. Am J Public Health. 2005;95(12):2129–32. doi: 10.2105/AJPH.2004.053645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guidelines for Medically Underserved Area and Population Designation. US Dept. of Health and Human Services; 2008. [Google Scholar]
- 38.Petereit DG, Rogers D, Burhansstipanov L, Kaur J, Govern F, Howard SP, et al. Walking forward: the South Dakota Native American project. J Cancer Educ. 2005;20(1 Suppl):65–70. doi: 10.1207/s15430154jce2001s_14. [DOI] [PubMed] [Google Scholar]
- 39.Molloy K, Reiner M, Ratteree K, Cina K, Helbig P, Miner R, et al. Patient navigation and cultural competence in cancer care. Association of Community Cancer Centers Oncology Issues. 2007;22(5):38–41. [Google Scholar]
- 40.Petereit D, Molloy K, Reiner M, Helbig P, Cina K, Miner R, et al. Establishing a patient navigator program to reduce cancer disparities in the American Indian communities of western South Dakota: initial observations and results. Cancer Control. Journal of the Moffitt Cancer Center. 2008;15(3):254–59. doi: 10.1177/107327480801500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stewart JH, Bertoni AG, Staten JL, Levine EA, Gross CP. Participation in surgical oncology clinical trials: gender-, race/ethnicity-, and age-based disparities. Ann Surg Oncol. 2007;14(12):3328–34. doi: 10.1245/s10434-007-9500-y. [DOI] [PubMed] [Google Scholar]
- 42.Nash D, Azeez S, Vlahov D, Schori M. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006;83(2):231–43. doi: 10.1007/s11524-006-9029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weinrich SP, Boyd MD, Weinrich M, Greene F, Reynolds WA, Jr., Metlin C. Increasing prostate cancer screening in African American men with peer-educator and client-navigator interventions. J Cancer Educ. 1998;13(4):213–9. doi: 10.1080/08858199809528549. [DOI] [PubMed] [Google Scholar]
- 44.Burhansstipanov L, Dignan MB, Wound DB, Tenney M, Vigil G. Native American recruitment into breast cancer screening: the NAWWA project. J Cancer Educ. 2000;15(1):28–32. doi: 10.1080/08858190009528649. [DOI] [PubMed] [Google Scholar]
- 45.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005;104(4):848–55. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 46.Carroll JK, Humiston SG, Meldrum SC, Salamone CM, Jean-Pierre P, Epstein RM, et al. Patients’ experiences with navigation for cancer care. Patient Educ Couns. 2009 doi: 10.1016/j.pec.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Campbell C, Craig J, Eggert J, Bailey-Dorton C. Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncol Nurs Forum. 37(1):61–8. doi: 10.1188/10.ONF.61-68. [DOI] [PubMed] [Google Scholar]
- 48.Lin CJ, Schwaderer KA, Morgenlander KH, Ricci EM, Hoffman L, Martz E, et al. Factors associated with patient navigators’ time spent on reducing barriers to cancer treatment. J Natl Med Assoc. 2008;100(11):1290–7. doi: 10.1016/s0027-9684(15)31507-8. [DOI] [PubMed] [Google Scholar]
- 49.Haverkamp D, Espey D, Paisano R, Cobb N. Cancer Mortality among American Indians and Alaska Natives: Regional Differences, 1999-2003. Indian Health Service; Feb, 2008. [Google Scholar]
- 50.Bruner DW, Jones M, Buchanan D, Russo J. Reducing cancer disparities for minorities: a multidisciplinary research agenda to improve patient access to health systems, clinical trials, and effective cancer therapy. J Clin Oncol. 2006;24(14):2209–15. doi: 10.1200/JCO.2005.04.8116. [DOI] [PubMed] [Google Scholar]
- 51.Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer. 2008;112(2):228–42. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- 52.Freund KM, Battaglia TA, Calhoun E, Dudley DJ, Fiscella K, Paskett E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113(12):3391–9. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ramsey S, Whitley E, Mears VW, McKoy JM, Everhart RM, Caswell RJ, et al. Evaluating the cost-effectiveness of cancer patient navigation programs: conceptual and practical issues. Cancer. 2009;115(23):5394–403. doi: 10.1002/cncr.24603. [DOI] [PMC free article] [PubMed] [Google Scholar]