Abstract
Purpose
Hematopoietic cell transplant patients are among the most vulnerable and acutely ill cancer populations (Bevans, Mitchell, & Marden, 2008). The responsibility of caring for the daily physical and psychosocial needs of these patients after transplant is placed mostly on family caregivers(Williams, 2007). The purpose of this descriptive correlational research study was to describe caregiving experiences of 56 caregivers of HCT patients 3–12 months following transplant.
Methods & Sample
Patients and caregivers were recruited from two west coast regional transplant programs in the United States. Variables studied were: relationship quality, rewards of caregiving, predictability, role strain, patient function, caregiving activities, and caregiver quality of life (QOL).
Key Results
Results indicated that all areas of role strain are significantly negatively correlated with caregiver's QOL. Predictability was negatively associated with problem solving and emotional strain indicating that as the level of predictability of the situation decreases, caregiver strain and problem solving increase. Predictability was positively correlated to caregiver QOL indicating that as the situation is more predictable caregiver QOL increases. Emotional strain, problem-solving strain, and usual care strain were significantly positively related, indicating that emotional strain and problem solving strain increased together. As usual care strain increased, so did problem-solving strain and emotional strain.
Conclusions
Suggestions for interventions include assessing and responding to caregiver issues such as emotional strain, problem-solving strain, usual care strain, unpredictability, and QOL. Examples of caregiver-focused interventions include providing timely appropriate information about these caregiver concerns including elements that make the caregiving situation predictable, and incorporating best practices for preventing and minimizing
Keywords: HCT Transplant, Caregivers, Predictability, Role Strain, Quality of Life
Background
Introduction
Changes in the health care system within the United States such as the need to decrease inpatient costs and medical care have moved much of the Hematopoietic Blood and Marrow Transplant (HCT) process and recovery from the inpatient to the outpatient setting (Rizzo, et al., 1999). (For this article the term “HCT” is synonymous with the terms “stem cell transplant”, and “bone marrow transplant”). As a result of this change in the setting of care, the responsibility of safely caring for these medically complicated patients following HCT is placed mostly on family caregivers who are expected to recognize and respond appropriately to rapid changes in patient condition. We define “caregiver” as one who regularly assists the patient with medical tasks and/or activities of daily living, and who assists or lives with the patient at least 10 hours a week. Despite the acuity of the patients and the potential for caregivers' actions to influence patients' outcomes, little information is available on what caregivers do for these vulnerable patients. The purpose of this research is to describe the caregiving process, including the tasks performed and the view of the experience of caring for hematologic cancer patients who have undergone allogeneic transplants.
Review of the Literature
Transplant process
In HCT, either the patient's own cells are harvested and stored and then reinfused (autologous HCT) or hematopoietic stem cells from a histologically compatible sibling or matched unrelated donor are collected from marrow or from the peripheral circulation and infused (allogeneic HCT). The goal of therapy is to destroy malignant cells using: 1) myeloablative doses of treatment (usually in the form of chemotherapy and/or radiation therapy) followed by HCT to rescue the patient from the profound hematologic toxicities of this high intensity treatment, or 2) reduced intensity treatment coupled with a “graft versus disease” effect of allogeneic HCT in which donor immune cells induce an immunologic response that eradicates malignant cells(Sandmaier, 2004). The donor material typically engrafts after 10 to 20 days, and starts to make functional white and red blood cells, platelets, and over time, additional immune system components. Early complications may include mucositis, fatigue, nausea and vomiting, diarrhoea, pancytopenia, pain, infection, and immune suppression (Ford, 2004). Many of these complications can occur at any time during recovery and persist for days to months following transplant. Graft versus host disease (GVHD), which occurs when the donor marrow recognizes the patients' usual organs as foreign, is a major risk following allogeneic HCT. Prevention of and treatment for GVHD requires profound immune suppression for months to years, which exposes patients to steroid dependency and continued high risk for infection. Patients who receive autologous transplants are rescued with their own peripheral stem cells and are not at risk for GVHD, experience fewer complications, and recover more quickly (Grant, Cooke, Bhatia, & Forman, 2005; Horowitz, 2004).
Informal caregivers
Within the last 15–20 years, descriptive studies have identified the needs, burdens and experiences of family caregivers of HCT patients. A recent Institute of Medicine report on psychosocial cancer care states that the patients' and families' psychosocial needs are not being adequately addressed during cancer care (IOM, 2007) and the results of the studies of family caregivers of HCT patients support this conclusion throughout the HCT patient's trajectory (Eldredge, et al., 2006)(Fife, Monahan, Abonour, Wood, & Stump, 2009b)(Foxall & Gaston-Johansson, 1996)(Gaston-Johansson, Lachica, Fall-Dickson, & Kennedy, 2004)(Williams, 2007).
Early literature in the 1990's identified high levels of distress, anxiety, and fatigue in caregivers of HCT patients (Foxall & Gaston-Johansson, 1996; Keogh, O'Riordan, McNamara, Duggan, & McCann, 1998). In addition to managing complex medical care, family members report uncertainty about the development of life threatening complications and whether or not the patient will survive (Haberman, 1995; Kelley, 1998; Stetz, McDonald, & Compton, 1996). As the patients' health improves, reintegrating patients back into the family system is difficult (Eilers, 2007). Family caregivers reported that higher amounts of caregiving were related to lower reports of physical health in HCT and that caregivers showed less attention to personal health concerns, experienced exhaustion, and limited their own social interactions (Foxall & Gaston-Johansson, 1996; Rivera, 1997).
Recent literature has continued to support these findings and identified additional QOL concerns, including concerns specific to marital dyads. Research on the physical and psychological components of family caregiver QOL revealed family caregivers experience more cognitive dysfunction than controls, and experience psychological issues such as fear, ineffective coping, depression, anxiety, hopelessness, spiritual distress, and conflict in decision–making as the patient recovers (Aslan, et al., 2006; Bishop, et al., 2007). Marital issues and social relationships have been a recent focus of transplant and oncology caregiver research (Aslan, et al., 2006; Bishop, et al., 2007; Boyle, et al., 2000; Cooke, Gemmill, & Grant, 2008; Gaston-Johansson, et al., 2004; Illingworth, Forbat, Hubbard, & Kearney, 2010; S. Langer, Abrams, & Syrjala, 2003; S. L. Langer, Yi, Storer, & Syrjala, 2009; Schumacher, Stewart, & Archbold, 2007; Williams, 2007). Findings indicate that caregivers who have poor social support, face a challenging caregiver burden, and experience less marital satisfaction, less spiritual well being and more loneliness than survivors(Bishop, et al., 2009; Boyle, et al., 2000; Molassiotis, Wilson, Blair, Howe, & Cavet, 2010).
There has been an increase in survival time following HCT over the decades. This increase in survival has sparked an interest in the concept of quality of life (QOL) of both transplant recipients and family caregivers (Schmidt, et al., 1993). Quality of life is defined as the well-being of an individual and the level of that person's satisfaction with life (Grant, Padilla, Ferrell, & Rhiner, 1990), and is commonly measured along physical, psychological, social, and spiritual domains. Spouses of HCT patients report minimal physical disruption in QOL, but experience high levels of emotional disruption, depression and fatigue in comparison to peer-nominated controls; caregivers' fatigue scores are increased during the caregiving experience and are remarkably similar to HCT recipient fatigue scores(Bishop, et al., 2004). Caregivers' reported elevated fatigue and depression levels must be interpreted with caution because commonly used scales often include symptoms that might be related to caregiving activities, such as sleep disruption. Bishop's study addressed many of the research design concerns of QOL researchers; it included a relatively large sample, recruited participants from multiple sites, and included a comparison group(Bishop, et al., 2004). However, the time since patient transplant was long (average of 7.1 years, range of 1 to 22 years) indicating that participants were likely to be in a relatively stable phase of their recovery when caregiving demands are minimal and most predictable. Because this study did not relate QOL to other constructs, it does not provide the information needed to support development of caregiving intervention studies. Although we recognize caregiving as a process over time, most of the studies of family caregivers of HCT recipients are cross-sectional, collect data at a single point in time, do not include several of the variables – such as rewards of caregiving responses in research with other family caregiving situations, and do not address the potential for complex interrelationships among study variables.
Preliminary work
In previous research, family caregiving processes were explored during the first 100 days following autologous HCT (Eldredge, et al., 2006). Aims of this study include 1)exploring patterns of caregiving, in autologous transplant recipient function during early recovery from transplant; 2) examining the relationships among caregiver demographics, relationship quality, preparedness, autologous recipient function, predictability of caregiving, caregiver role strain, and rewards of caregiving; and 3) examining the relative contribution of caregiver age, preparedness, relationship quality, and recipient function to explaining caregiver role strain and rewards of caregiving. Results indicated that although caregiving was consistently rewarding, the activities that were rated as most difficult for caregivers were related to supporting the recipients' emotional well-being. Disruption in HCT recipient emotional functioning resolved more slowly than disruption in physical functioning and disruption in emotional functioning accounted for caregiver role strain at weeks 2 and 6 of recovery Also, higher caregiving reward scores were explained by the preparedness of the caregiver with higher preparedness associated with higher reward (Eldredge, et al., 2006). Thus, as caregivers felt better prepared in their role, they felt better about the care they were giving.
Summary
Because family caregivers of HCT recipients have extensive responsibility for recipients' well-being and safety, systematic examination of the caregiving process and the outcomes of caregiving and quality of life is a critical next step in the research. Knowing what the process of family caregiving involves and how it impacts the caregiver can provide content for creating a testable intervention for HCT family caregivers. The study reported here parallels previous work and turns the focus to caregivers of the sickest patients, allogeneic HCT recipients, over the first year following transplant. In this population recovery requires up to at least one year following transplant and, thus, requires a long-term commitment of the family caregiver. Further, this study highlights relationships among several concepts that have been sensitive to nursing intervention in other caregiving populations; namely mutuality or relationship between patient and caregiver, caregiver burden, and quality of life. (Albert, Litvin, Kleban, & Brody, 1991; Carter, et al., 1998; Lawton, Moss, Kleban, Glicksman, & Rovine, 1991; Mor, Guadagnoli, & Wool, 1988; Oberst & Scott, 1988; Schumacher, 1996; Schumacher, Stewart, & Archbold, 1998; Shyu, Archbold, & Imle, 1998).
Purpose/Aims
The purpose of this research is to describe the caregiving process of caregivers of allogeneic HCT patients. The specific aims of this study are to describe caregivers' ongoing caregiving activities; describe caregiving role strain, worry, and rewards of caregiving; describe caregiver quality of life, depression, fatigue, and intrusive events; and explore relationships among outcomes of caregiving and caregiver quality of life
Design/Research
The design approach is a descriptive correlational study that explored the caregiving process and outcomes for caregivers of patients recovering from allogeneic HCT.
Theoretical Framework
Family caregiving is viewed from an interactionist perspective (Burr, 1979), suggesting that characteristics of and interactions among the caregiver, care receiver, and health care providers influence the nature of the caregiving situation and subsequent responses to caregiving (Archbold, et al., 1995). This study focuses only on caregivers' experiences. In this study, we assessed the caregiver's contextual factors, including age, gender, education, income, financial burden, mutuality, and caregivers' feelings of preparedness. The relevant concepts of mutuality, preparedness, predictability, and strain, were identified from the caregiver literature (Archbold, Stewart, Greenlick, & Harvath, 1990, 1992; Archbold, et al., 1995). Mutuality refers to the nature of the relationship between the patient and the family caregiver. Preparedness refers to how well prepared the caregiver is to provide care. Predictability refers to the predictability of the tasks and activities involved in caregiving. Strain involves measuring the role strain experienced by the caregiver. Family care variables were represented by the amount of care delivered, the predictability of the caregiving situation, caregivers' perceptions of recipients' current functional abilities, presence of GVHD, and remission status. Caregiver responses to caregiving included caregiver role strain, worry and rewards. Highest order outcomes included caregivers' reports of QOL, depression, fatigue, and level of intrusive thoughts about the disease and treatment
Sample
The convenience sample included 56 patients and caregivers that met the eligibility criteria and, who had undergone a transplant within 3–12 months. Physicians identified eligible patients for the study; therefore the sample was not consecutive. Subjects were recruited from two regional transplant programs on the west coast of the United States. Site #1 was a large transplant center on the southwest coast of the United States, and the second center was a smaller transplant center on the northwest coast of the United States. The caregiver was defined as one who regularly assisted with medical tasks and/or activities of daily living (living with patients or assisting at least 10 hours a week), who was 18 years or older; and had to speak and read English.
The transplant patients were contacted either in the clinic, by phone or by mail, and asked to nominate their primary caregiver for the study. Both patients and caregivers provided written consent. Research staff reviewed the packet of questionnaires with each care subject, including instructions for completing each section and for returning the completed packets. Study variables were selected to represent key elements of the theoretical framework and included: relationship quality, rewards of caregiving, predictability, role strain, patient function, caregiving activities, and quality of life. The packet of questionnaires was estimated to take caregivers 60–90 minutes to complete.
Questionnaires
The questionnaires used are described in Table 1 and briefly identified here.
Table 1.
Instruments and Psychometric Data
| Concept | Questionnaire Name | No. of Items | Internal Consistency | Scoring |
|---|---|---|---|---|
| 1 Demographics | Patient Demographics | 11 | NA | NA |
| Caregiver Demographics | 19 | NA | NA | |
| 2 Patient Function: Sleep and Rest | Sickness Impact Profile: SRb,c | 7 | .45 | Subscale- Items scored and transformed to 0–100% 100 = Most dysfunction |
| Emotional behavior | SIP- EB | 9 | .64 | |
| Home Management | SIP- HM | 10 | .81 | |
| Work | SIP- AW | 9 | .76 | |
| Recreation & Pastimes | SIP- RP | 8 | .71 | |
| 3 Caregiver Concepts | ||||
| Relationship Quality | Mutualitya, | 15 | .92 | 0–4 4 = high mutuality |
| Role Strain | Caregiver Role Straind,e | 98 | >.80 | 1–5 5 = very hard |
| Predictability | Predictabilityf | 8 | .84 | 0–4 4 = very predictable |
| Rewards | Rewards of Caregivingg | 14 | .89 | 0–4 4 = a great deal |
| 4 QOL | COH QOL Scale Familyh | 37 | .70 | 0–10 10 = highest QOL |
Sneeuw et al., 1997
Eldredge, 2004
Demographic Tool: Two demographic tools were created for the study to capture demographic patient and caregiver information. These tools were based on previous demographic tools used by the researchers in other studies. Both are filled out by the caregiver and asked about age, gender, education, marital and parenting status, living arrangements, and socioeconomic status.
Mutuality Scale measures quality of the relationship between the patient and the caregiver. The fifteen items include issues such as “seeing eye to eye”, closeness, sharing experiences, attachment, comfort from each other, emotional support, time together, and expression of warm feelings (Archbold, et al., 1990).
Sickness Impact Profile (SIP), a behaviourally-based measure of health status was used to measure disruption in patient function (Bergner, Bobbitt, Carter, & Gilson, 1981). Five of the twelve subscales were used: Sleep and Rest; Emotional Behaviour; Home Management; Ambulation, Recreation and Pastimes.
Caregiver Activities and Role Strain were measured with a 98 item investigator-developed instrument used to determine what activities are carried out by the caregiver and how difficult (hard) the activity is for the caregiver. The scale was developed to obtain a detailed picture of caregiving at home for elderly patients, including some with cancer (Archbold, et al., 1992; Eldredge, et al., 2006; Fife, Monahan, Abonour, Wood, & Stump, 2009a).
Predictability was measured with an 8-item scale described the consistency in the patterns for caregiving, and how predictable the patient's needs, care activities, and caregiver's routines were (Eldredge, et al., 2006; Fife, et al., 2009a).
Rewards of Caregiving was measured on a 14 item instrument that described the emotional and existential rewards caregivers experience in caring for their family members. The tool captured the degree that caregivers find aspects of their caregiving situations rewarding. (Fife, et al., 2009a).
QOL-Family is a questionnaire developed at the City of Hope for measuring quality of life in family members of cancer patients. (Ferrell, Cohen, Rhiner, & Rozek, 1991; Ferrell, Rhiner, Cohen, & Grant, 1991). It consists of four dimensions (physical, psychological, social and spiritual well being), and an overall score.
Results
A total of 56 patients and caregiver dyads were accrued to the study and completed the packet of questionnaires on one occasion. Forty patients were accrued from Site # 1, and sixteen were accrued from Site # 2. While patients represented approximately equal numbers of males and females, caregivers were predominantly female (Table 2). A large proportion of both patients and caregivers were college-educated. Combined household income was $50,000 or higher in over half of the patient and caregiver dyads. A small sample of Hispanics participated and most caregivers were white. The distribution of gender, marital status, educational attainment, ethnicity and race were not significantly different by site. However, the combined household income was significantly higher in the participants from Site #1.
Table 2.
Demographics of patient and caregivers
| Characteristics | Patients N = 56 | Caregivers N = 56 |
|---|---|---|
| Gender | ||
| Female | 42.9% | 76% |
| Male | 57.1% | 24% |
| Marital Statusa | ||
| Married/Partnered | 75% | 91% |
| Divorced/Never Married | 25% | 9% |
| Education-highest degree completed | ||
| Less than High School graduate | 3.6% | 1.9% |
| High School graduate/General Equivalency Diploma | 26.8% | 18.9% |
| Some college or degree | 62.5% | 73.6% |
| Missing | 7.1% | 5.6% |
| Spanish, Hispanic, Latino | ||
| Yes | 16.1% | 13.2% |
| No | 83.9% | 86.8% |
| Race | ||
| White | 81.5% | 80.4% |
| Asian or Pacific Islander | 9.3% | 9.8% |
| Amer Indian/Alaska Native | 1.9% | 2.0% |
| Missing | 7.3% | 7.8% |
| Income-Combined Household | ||
| $1–$24,999 | 17.2% | |
| $25,000–$49,000 | 30.8% | |
| $50,000–$99,999 | 27.0% | |
| $100,000 and more | 25.0% |
Combined household income was significantly higher (p < .05) in the participants from Site #1.
Diagnoses of the patients included 45% acute leukemia, 33% myelodysplasia, 7% chronic leukemia, and 14% other hematologic malignancies (multiple myeloma, non Hodgkin's lymphoma). The conditioning regimen included total body radiation in 41% of the patients.
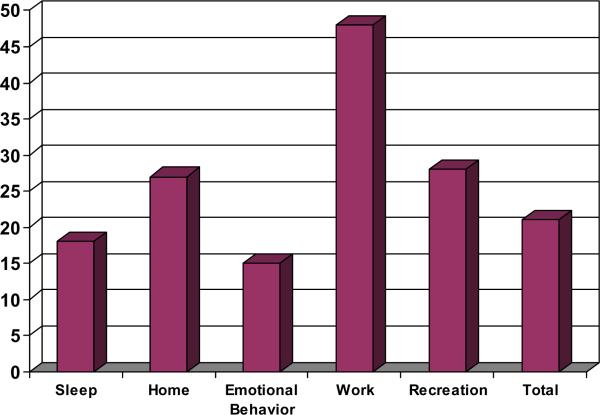
Scores on the SIP were used to describe the disruptions to the patients' lives as perceived by the caregiver. Scores for each of the subscales rated could range from 0 = no disruption to 100 = complete disruption. Scores for Emotional Behaviour, Sleep/Rest, Home Management, Recreation/Pastime, and Work and an overall score are found in Figure 1 and range from less than 20 to more than 40, with Work showing the highest disruption score. Total score including all subscales was 21.6 (sd = 15.0). Scores on the SIP provide a picture of the patient's ability to participate in many daily activities as perceived by the caregiver.
Figure 1.
Disruption in Recipient Function
Caregiver concepts included scores on mutuality, predictability, rewards of caregiving, caregiver role strain, and quality of life (Table 3). Mutuality revealed the highest score, followed by rewards and predictability. Role strain revealed low scores in all subscales and overall scoring. QOL at 6.0 showed moderate to poor quality of life for the participating caregivers.
Table 3.
Caregiver Concept Scores
| Concept | Score |
|---|---|
| Mean (SD) | |
| Mutuality* | 3.42 (.46) |
| Predictability* | 2.45 (.65) |
| Rewards* | 3.2 (69) |
| Role Strain** | |
| Problem Solving | 1.27 (1.08) |
| Emotional Support | 1.81 (.92) |
| Usual Care | 0.91 (.74) |
| Total | 0.97 (.66) |
| QOL*** | 6.0 (1.3) |
Scored 0 – 4 with 4=highest (best) score
Scored 1–5 with 5= high strain
Scored 1 – 10 with 10 = highest QOL
A rank ordering of caregiving activities by difficulty rating is found on Table 4. Results indicate that providing care to support the patient's emotional status, concerns about death, and other feelings were was ranked as the most difficult, while handling the caregivers' own emotions and providing physical care were the least difficult.
Table 4.
Caregiving Activities Mean Difficulty of the Ten Most Difficult Caregiving Activities
| Item | Mean* | SD | |
|---|---|---|---|
| 1 | Listen when feeling very sad or scared | 2.36 | 1.39 |
| 2 | Listen to concerns about cancer/treatment | 2.29 | 1.39 |
| 3 | Help with emotional ups and downs | 2.19 | 1.48 |
| 4 | Talk about feelings related to cancer | 2.00 | 1.56 |
| 5 | Talk about the possibility of death | 2.00 | 2.03 |
| 6 | Discuss the future | 1.93 | 1.27 |
| 7 | Deal with mood swings | 1.83 | 1.81 |
| 8 | Keep other family members informed | 1.78 | 1.15 |
| 9 | Handle his or her anger | 1.69 | 1.69 |
| 10 | Protect from exposure to microbes | 1.63 | 1.40 |
Scale = 1–5; with 5 = very difficult
Role strain scores were analyzed to reveal site differences. Independent t-tests revealed significant differences (p < .05) between the sites. Caregivers at Site #2 had more total role strain, problem solving strain and usual care strain (as well as fewer rewards and more disruption in function.
In order to explore the relationships between the caregiving concepts and caregiver QOL, a correlational analysis was conducted. (Table 6): All three areas of strain were significantly negatively correlated to QOL indicating that when usual care, problem-solving or emotional support are increased, overall quality of life scores decrease. The variable of predictability was associated with the three aspects of strain: usual care, problem solving, emotional support, indicating that as the situation was less predictable, strain in all three areas increased. Predictability was also positively correlated to quality of life indicating that as the situation was more predictable, quality of life increased. The various aspects of strain were interrelated, for example as the need for emotional support increased so did the need for problem solving. Also as usual care strain increased so did problem solving strain and emotional support strain.
Table 6.
Correlations Among Key Study Variables (N=56)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Partner Age | Days TP | Function | Mutuality | Predict. | Strain PS | Strain ES | Strain UC | Rewards | QOL | ||
| Care | |||||||||||
| 1 | Partner Age | ||||||||||
| 2 | Days TP | −0.26 | |||||||||
| 3 | Function | −0.10 | −0.19 | ||||||||
| 4 | Mutuality | −0.05 | 0.01 | −0.19 | |||||||
| 5 | Predict. | 0.30 a | −0.01 | −0.50b | 0.06 | ||||||
| 6 | Strain PS | −0.26 | −0.11 | 0.61b | −0.12 | −0.60 b | |||||
| 7 | Strain ES | −0.29 | −0.03 | 0.58b | −0.04 | −0.57 b | 0.59b | ||||
| 8 | Strain UC | −0.11 | −0.11 | 0.69b | −0.01 | −0.64 | 0.82b | 0.60b | |||
| 9 | Rewards | −0.11 | −0.02 | 0.18 | 0.23 | 0.03 | 0.23 | 0.22 | 0.23 | ||
| 10 | QOL | 0.12 | 0.10 | −0.49b | 0.18 | 0.58b | −0.39b | −0.54b | −0.46b | 0.07 |
0.05 significance level
0.01 significance level
Regression analysis
Regression analysis was used in order to further explore the predictors of caregivers' QOL: Included in the analysis were the predictability of caregiving, and each of the strain subscales: emotional strain, usual care strain and problem-solving strain. This set of variables explained 43.1% of the variance in family caregiver quality of life (F5, 48 = 7.36; p< 001; Adj R2 = .37). The only significant unique predictor of family caregiver QOL was predictability of caregiving. (B = 76; t = 2.5; p. = .02). As caregivers felt that more of the caregiving was predictable, they experienced higher quality of life. Strain from providing emotional support was nearly significant (B = −43; t = −1.9; p = .06). There was a trend for caregivers who felt less strain from providing emotional support to report experiencing higher levels of QOL.
Discussion
Our study highlights the caregiving process of caregivers of allogeneic HCT patients. We explored several concepts related to this process; namely disruptions to patients as perceived by the caregivers and reported on the SIP, mutuality, predictability, rewards and role strain. Disruptions as experienced by patients have been reported by others. These studies have identified the high levels of distress, anxiety and fatigue in this population (Foxall & Gaston-Johansson, 1996) and the need for caregivers to manage a variety of psychological and physical symptoms experienced by these patients following discharge (Bevans, Mitchell, Marden, 2008). In our study findings of caregiving experiences for allogeneic transplant patients were consistent with these previous findings, and provided additional information on the caregiving tasks reported and the difficulty of those tasks as experienced by the caregivers. Disruption scores on the SIP revealed patient difficulties in sleep and emotional behaviour. This points to the need to prepare caregivers for addressing patients' emotional concerns. However, providing emotional support was the most difficult caregiving task reported by the caregivers in our study. . This finding is consistent with the findings of our previously reported longitudinal study of caregivers of autologous HCT recipients (Eldredge, et al., 2006). Within the rank order of “ten most difficult caregiving activities” (see Table 4) seven of the ten items involved coping with the emotional concerns of the transplant patient. Another descriptive study of caregivers of autologous transplant patients also found that “dealing with the physical and mental complications” post transplant was ranked number one by both transplant survivor and caregiver (Boyle, et al., 2000). Admittedly, the health care team focuses on the physical care issues after transplant, and often does not make the psychological issues priority. These results confirm findings of others and suggest that caregivers need more information about how to provide emotional support and what to expect about providing emotional support to their loved ones. An intervention testing the effects of assisting caregivers in providing emotional support is a necessary next step in improving the quality of life of BMT caregivers. Mutuality is a caregiving concept that addresses the strength of the relationship between the patient and the caregiver. In a study that included a variety of cancer diagnoses (Schumacher, Steward Archbold, 2007), results revealed that high mutuality when combined with high preparedness protected caregivers from mood disturbances (e.g. tension, depression, etc) as measured on the Profile of Mood States (McNair,Lorr, & Dropplemen, 1992)(McNair, 1992). For our study, mutuality scores were relatively high (mean = 3.42 on a 4 point scale), but predictability scores were lower (mean = 2.45 on a 4 point scale), and are thus likely to have contributed to the overall moderate to poor quality of life scores (mean of 6.0 on a 10 point scale). These results point to the need to include evaluation of mutuality in addressing caregivers' needs, and the importance of preparedness in protecting the emotional health of the caregivers.
Role strain evaluation in our study revealed challenges for patients in all aspects of strain – problem solving tasks, emotional support, and provision of usual care. As caregiver strain increased, whether related to the strain of care, of problem-solving or of emotional care, or giving usual care, the quality of life of the caregiver decreased. Caregiving for an allogeneic transplant patient can be very challenging, and there has been little focus on the psychosocial needs of caregivers (Bishop, et al., 2009). Some literature has suggested that caregivers can experience more or at least the same level of anxiety and depression as transplant survivors (Bishop, et al., 2009; S. Langer, et al., 2003). They also can experience isolation, limited social support, and less benefit finding from the transplant experience (Bishop, et al., 2007). They must “deal with emotional demands of caring for the patient in highly uncertain and unfamiliar situations, often while placing their own needs on hold” (S. Langer, et al., 2003). Brown and Stetz (1999) discuss in their theoretical model of caregiving that there is a great deal of suffering in the caregivers' emotional work involved with care of a severely ill patient (Brown & Stetz, 1999). Only recently, has there been a growing awareness of these challenges. Interventions for caregivers can address this area by including: 1) more education of the transplant trajectory, needed skills and resources, 2) problem solving and coping skills training, 3) referral to psychosocial series 4) and teaching of the priority of self-care (Cooke, et al., 2008).
The post transplant experience can be very unpredictable since the post recovery trajectory is uncertain and unexpected complications and readmissions are not uncommon (Grant, et al., 2005). Clearly family and caregiver predictability and control is not always possible and in the current study predictability was an important identified variable. Family caregiver QOL was related to predictability in caregiving, which suggests that ratings of quality of life could be improved if caregivers perceived caregiving as more predictable. Research indicates that transplant caregivers do experience more distress when the sense of personal control decreases and life disruption occurs (Fife, et al., 2009b). The concept of “preparedness” is similar to the variable of predictability. One study confirmed what others have reported for cancer patients in general -- that when caregivers of cancer patients feel less prepared, they experience more caregiver difficulty (Schumacher, et al., 2007). Predictability can also be equated with expectations. Williams explored concepts of commitment, expectations and negotiation and found that skillful management of expectations was a source of energy for caregivers, and negotiating the role effectively conserved caregiver energy and allowed important tasks to be accomplished efficiently whereas ambiguity in the caregiving role makes caregiving more difficult (Williams, 2007). The current study examined predictability after transplant and results showed it was less important than role strain, it was more important than mutuality. The problem of predictability may begin before transplant with caregiver expectations of the transplant trajectory, and their role and relationships with the medical staff. An interesting study which looked at the psychosocial adjustment of patients and caregivers prior to transplant found that caregivers reported problems with health care orientation, expectations and feeling uninformed and less connected with the medical staff even at the beginning of the transplant experience (Siston, et al., 2001). This points to the need for caregiver interventions to begin prior to transplant, and then continue after discharge when the role of the caregiver increases.
This study examined the relationships of the caregiving process and outcomes for caregivers of patients recovering from allogeneic HCT. The caregiver concepts of patient disruptions, mutuality, preparedness, and role strain provided valuable information in further understanding the challenges faced by this caregiver population. As with our previous study of caregivers of autologous transplant patients, the current study highlights the need to address caregivers' ability to deal with patients' emotional behaviour, as well as interventions for physical care. Formulating and testing a caregiver intervention that includes care of the patient as well as care for the caregiver is needed as a next step to meeting the challenges of caregivers of allogeneic cancer patients.
Limitations
One major limitation of our study is the small sample size. Recruiting caregivers of transplant patients is challenging and needs to be addressed in future studies with larger sample sizes. There were some important differences in caregiver responses between the two institutions, with one site having caregivers who reported more patient disruption, fewer rewards, and more strain. These differences were not evident in demographic characteristics (except for total household income). Since Site 1 had a considerably larger transplant program than Site 2, this might explain the large range of income and the resulting higher combined mean income. More information on specific recipient illness characteristics (disease, time from diagnosis to transplant, intensity of conditioning regimen) was not collected in this study as resources did not include auditing the medical record.
Implications for Practice, Research, and Education
Preparation for caregivers falls predominantly in the role of the nursing staff at most cancer centers. This holds true for caregivers of HCT patients. Results of this study confirm and expand on previous studies, and underscore the need for clear, consistent, and tailored education for caregivers. This dedicated group of individuals is essential to the care and recovery of the HCT patient, and their care continues for allogeneic patients, up to one year post transplant. Supporting them, providing psychoeducation and related resources from the beginning of transplant through the first year post discharge could provide valuable improvements in the quality of life of both patients and caregivers. It is time for intervention research with caregivers of HCT patients. The literature has begun to describe the challenges faced by HCT caregivers and this descriptive study adds to the information. Suggestions for nursing interventions include testing the inclusion of the caregiver in the psychosocial plan of care, examining the best practices for education of caregivers to enhance predictability, and offering tools to support the emotional strain of providing care.
Table 5.
Role Strain for Total Sample and By Site
| Strain | Combined | Site #1 | Site #2 | t Score |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Total | 0.97 (0.66) | 0.84 (0.63) | 1.32 (0.64) | 2.56a |
| Problem solving | 1.27 (1.08) | 1.05 (1.04) | 1.85 (0.98) | 2.64a |
| Emotional support | 1.81 (0.92) | 1.69 (0.88) | 2.12 (0.99) | 1.59 |
| Usual Care | 0.91 (0.74) | 0.76 (.073) | 1.25 (0.69) | 2.30a |
Significant @ p<0.05
Acknowledgments
Funding Source: Oregon Health & Science University Faculty Intramural Research Award (D. Eldredge) & 5K24CA091442 from NCI (L. Nail) R01 CA107446 Standardized Nursing Intervention Protocol for HCT Patients (M. Grant)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Albert SM, Litvin SJ, Kleban MH, Brody EM. Caregiving daughters' perceptions of their own and their mothers' personalities. Gerontologist. 1991;31(4):476–482. doi: 10.1093/geront/31.4.476. [DOI] [PubMed] [Google Scholar]
- Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health. 1990;13(6):375–384. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Clinical assessment of mutuality and preparedness in family caregivers to frail older people. In: Funk EMTSG, Champagne MT, Copp LA, editors. Key Aspects of Elder Care. Springer; New York: 1992. pp. 328–339. [Google Scholar]
- Archbold PG, Stewart BJ, Miller LL, Harvath TA, Greenlick MR, Van Buren L, et al. The PREP system of nursing interventions: a pilot test with families caring for older members. Preparedness (PR), enrichment (E) and predictability (P) Res Nurs Health. 1995;18(1):3–16. doi: 10.1002/nur.4770180103. [DOI] [PubMed] [Google Scholar]
- Aslan O, Kav S, Meral C, Tekin F, Yesil H, Ozturk U, et al. Needs of lay caregivers of bone marrow transplant patients in Turkey: a multicenter study. Cancer Nurs. 2006;29(6):E1–7. doi: 10.1097/00002820-200611000-00014. [DOI] [PubMed] [Google Scholar]
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Bevans MF, Mitchell SA, Marden S. The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT) Support Care Cancer. 2008;16(11):1243–1254. doi: 10.1007/s00520-008-0420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop MM, Beaumont JL, Hahn EA, Cella D, Andrykowski MA, Brady MJ, et al. Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. J Clin Oncol. 2007;25(11):1403–1411. doi: 10.1200/JCO.2006.07.5705. [DOI] [PubMed] [Google Scholar]
- Bishop MM, Hahn EA, Cella D, Brady MJ, Andrykowski MA, Beaumont JL, et al. 2004 The Gift of Life Comes with a Price: The Impact of Hematopoietic Cell Transplantation on the Long-Term Quality of Life of Survivors and their Spouses (pp. Biology of Blood and Marrow Transplantation, Volume 10, Supplement 11, February 2004, Pages 2007–2008): IBMTR/ABMTR Mortimer M. Bortin. [Google Scholar]
- Bishop MM, Lee SJ, Beaumont JL, Andrykowski MA, Rizzo JD, Sobocinski KA, et al. The Preventive Health Behaviors of Long-Term Survivors Cancer and Hematopoietic Stem Cell Transplantation Compared to Matched Controls. Biol Blood Marrow Transplant. 2009 doi: 10.1016/j.bbmt.2009.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle D, Blodgett L, Gnesdiloff S, White J, Bamford AM, Sheridan M, et al. Caregiver quality of life after autologous bone marrow transplantation. Cancer Nurs. 2000;23(3):193–203. doi: 10.1097/00002820-200006000-00006. quiz 204–195. [DOI] [PubMed] [Google Scholar]
- Brown MA, Stetz K. The labor of caregiving: a theoretical model of caregiving during potentially fatal illness. Qual Health Res. 1999;9(2):182–197. doi: 10.1177/104973299129121776. [DOI] [PubMed] [Google Scholar]
- Burr WR, Leigh GK, Day RD, Constantine J. Symbolic interaction and the Family. In: Burr RHWR, Nye FI, Reiss I, editors. Contemporary Theories about the Family. Vol. 2. Free Press; New York: 1979. pp. 42–111. [Google Scholar]
- Carter JH, Stewart BJ, Archbold PG, Inoue I, Jaglin J, Lannon M, et al. Living with a person who has Parkinson's disease: the spouse's perspective by stage of disease. Parkinson's Study Group. Mov Disord. 1998;13(1):20–28. doi: 10.1002/mds.870130108. [DOI] [PubMed] [Google Scholar]
- Cooke L, Gemmill R, Grant M. Advanced practice nurses core competencies: a framework for developing and testing an advanced practice nurse discharge intervention. Clin Nurse Spec. 2008;22(5):218–225. doi: 10.1097/01.NUR.0000325366.15927.2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eilers J, Bree A. Family Issues and Perspectives. In: Schmidt-Pokorny S. E. a. K., editor. Blood and Marrow Stem Cell Transplantation: Principles, Practice and Nursing Insights. Third edition ed. Jones and Bartlett Publishers; Boston: 2007. [Google Scholar]
- Eldredge DH, Nail LM, Maziarz RT, Hansen LK, Ewing D, Archbold PG. Explaining family caregiver role strain following autologous blood and marrow transplantation. J Psychosoc Oncol. 2006;24(3):53–74. doi: 10.1300/J077v24n03_03. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, Cohen MZ, Rhiner M, Rozek A. Pain as a metaphor for illness. Part II: Family caregivers' management of pain. Oncol Nurs Forum. 1991;18(8):1315–1321. [PubMed] [Google Scholar]
- Ferrell BR, Rhiner M, Cohen MZ, Grant M. Pain as a metaphor for illness. Part I: Impact of cancer pain on family caregivers. Oncol Nurs Forum. 1991;18(8):1303–1309. [PubMed] [Google Scholar]
- Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplantation. 2009a;43(12):959–966. doi: 10.1038/bmt.2008.405. [DOI] [PubMed] [Google Scholar]
- Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplant. 2009b;43(12):959–966. doi: 10.1038/bmt.2008.405. [DOI] [PubMed] [Google Scholar]
- Ford RC, Campbell J, Madison J. Nursing Issues in Hematopoietic Cell Transplantation. In: Blume S. F. a. F. R. A. K. G., editor. Thomas' Hematopoietic Cell Transplantation. Third edition ed. Blackwell Science Ltd.; Malden, Massachusetts: 2004. pp. 469–482. [Google Scholar]
- Foxall MJ, Gaston-Johansson F. Burden and health outcomes of family caregivers of hospitalized bone marrow transplant patients. J Adv Nurs. 1996;24(5):915–923. doi: 10.1111/j.1365-2648.1996.tb02926.x. [DOI] [PubMed] [Google Scholar]
- Gaston-Johansson F, Lachica EM, Fall-Dickson JM, Kennedy MJ. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncol Nurs Forum. 2004;31(6):1161–1169. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- Grant M, Cooke L, Bhatia S, Forman S. Discharge and unscheduled readmissions of adult patients undergoing hematopoietic stem cell transplantation: implications for developing nursing interventions. Oncol Nurs Forum. 2005;32(1):E1–8. doi: 10.1188/05.onf.e1-e8. [DOI] [PubMed] [Google Scholar]
- Grant M, Padilla GV, Ferrell BR, Rhiner M. Assessment of quality of life with a single instrument. Semin Oncol Nurs. 1990;6(4):260–270. doi: 10.1016/0749-2081(90)90028-4. [DOI] [PubMed] [Google Scholar]
- Haberman M. The meaning of cancer therapy: bone marrow transplantation as an exemplar of therapy. Semin Oncol Nurs. 1995;11(1):23–31. doi: 10.1016/s0749-2081(95)80039-5. [DOI] [PubMed] [Google Scholar]
- Horowitz MM. Uses and Growth of Hematopoietc Cell Transplantation. In: Blume S. F. a. F. R. A. K. G., editor. Thomas' Hematopoietic Cell Transplantation. Third edition ed. Massachusetts Blackwell Science Ltd.; Malden: 2004. pp. 9–15. [Google Scholar]
- Illingworth N, Forbat L, Hubbard G, Kearney N. The importance of relationships in the experience of cancer: a re-working of the policy ideal of the whole-systems approach. Eur J Oncol Nurs. 2010;14(1):23–28. doi: 10.1016/j.ejon.2009.06.006. [DOI] [PubMed] [Google Scholar]
- IOM Cancer care for the whole patient: Meeting psychosocial health needs. 2007 [PubMed] [Google Scholar]
- Kelley CH, Haggerty McBride L, Rudder Randolph S, Leum EW, Lonergan JN. Homecare Management of the Blood Cell Transplant Patient. Third edition ed. Jones and Bartlett Publishers; Boston, USA: 1998. [Google Scholar]
- Keogh F, O'Riordan J, McNamara C, Duggan C, McCann SR. Psychosocial adaptation of patients and families following bone marrow transplantation: a prospective, longitudinal study. Bone Marrow Transplant. 1998;22(9):905–911. doi: 10.1038/sj.bmt.1701443. [DOI] [PubMed] [Google Scholar]
- Langer S, Abrams J, Syrjala K. Caregiver and patient marital satisfaction and affect following hematopoietic stem cell transplantation: a prospective, longitudinal investigation. Psychooncology. 2003;12(3):239–253. doi: 10.1002/pon.633. [DOI] [PubMed] [Google Scholar]
- Langer SL, Yi JC, Storer BE, Syrjala KL. Marital adjustment, satisfaction and dissolution among hematopoietic stem cell transplant patients and spouses: a prospective, five-year longitudinal investigation. Psychooncology. 2009 doi: 10.1002/pon.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol. 1991;46(4):P181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. EdITS Manual for the Profile of Mood States. Educational and Industrial Testing Service; San Diego: 1992. [Google Scholar]
- Molassiotis A, Wilson B, Blair S, Howe T, Cavet J. Unmet supportive care needs, psychological well-being and quality of life in patients living with multiple myeloma and their partners. Psychooncology. 2010 doi: 10.1002/pon.1710. [DOI] [PubMed] [Google Scholar]
- Mor V, Guadagnoli E, Wool M. The role of concrete services in cancer care. Adv Psychosom Med. 1988;18:102–118. doi: 10.1159/000415779. [DOI] [PubMed] [Google Scholar]
- Oberst MT, Scott DW. Postdischarge distress in surgically treated cancer patients and their spouses. Res Nurs Health. 1988;11(4):223–233. doi: 10.1002/nur.4770110404. [DOI] [PubMed] [Google Scholar]
- Rivera LM. Blood Cell Transplantation: It's Impact on one Family. Seminars in Oncology Nursing. 1997;13:194–199. doi: 10.1016/s0749-2081(97)80035-6. [DOI] [PubMed] [Google Scholar]
- Rizzo JD, Vogelsang GB, Krumm S, Frink B, Mock V, Bass EB. Outpatient-based bone marrow transplantation for hematologic malignancies: cost saving or cost shifting? J Clin Oncol. 1999;17(9):2811–2818. doi: 10.1200/JCO.1999.17.9.2811. [DOI] [PubMed] [Google Scholar]
- Sandmaier B, Strob R, editors. Nonmyeloablative therapy and hematopoietic cell transplantation for heamtologic disorders. 3rd Edition ed. Blackwell Science LTD.; Mass.: 2004. [Google Scholar]
- Schmidt GM, Niland JC, Forman SJ, Fonbuena PP, Dagis AC, Grant MM, et al. Extended follow-up in 212 long-term allogeneic bone marrow transplant survivors. Issues of quality of life. Transplantation. 1993;55(3):551–557. doi: 10.1097/00007890-199303000-00018. [DOI] [PubMed] [Google Scholar]
- Schumacher KL. Reconceptualizing family caregiving: family-based illness care during chemotherapy. Res Nurs Health. 1996;19(4):261–271. doi: 10.1002/(SICI)1098-240X(199608)19:4<261::AID-NUR1>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Stewart BJ, Archbold PG. Conceptualization and measurement of doing family caregiving well. Image J Nurs Sch. 1998;30(1):63–69. doi: 10.1111/j.1547-5069.1998.tb01238.x. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Stewart BJ, Archbold PG. Mutuality and preparedness moderate the effects of caregiving demand on cancer family caregiver outcomes. Nurs Res. 2007;56(6):425–433. doi: 10.1097/01.NNR.0000299852.75300.03. [DOI] [PubMed] [Google Scholar]
- Shyu YI, Archbold PG, Imle M. Finding a balance point: a process central to understanding family caregiving in Taiwanese families. Res Nurs Health. 1998;21(3):261–270. doi: 10.1002/(sici)1098-240x(199806)21:3<261::aid-nur9>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Siston AK, List MA, Daugherty CK, Banik DM, Menke C, Cornetta K, et al. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001;27(11):1181–1188. doi: 10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- Stetz KM, McDonald JC, Compton K. Needs and experiences of family caregivers during marrow transplantation. Oncol Nurs Forum. 1996;23(9):1422–1427. [PubMed] [Google Scholar]
- Williams LA. Whatever it takes: informal caregiving dynamics in blood and marrow transplantation. Oncol Nurs Forum. 2007;34(2):379–387. doi: 10.1188/07.ONF.379-387. [DOI] [PubMed] [Google Scholar]