Abstract
Background
Socioeconomic position (SEP) in childhood and adulthood influences the risk of adult psychiatric disorder. This paper investigates first how cumulative childhood manual SEP influences the risk for mid-life depressive and anxiety disorders and secondly the effects of health selection based on psychological disorder in childhood and psychological distress in early adulthood on mid-life social position.
Methods
9,377 participants of the 1958 Birth Cohort were followed up at 45 years with the Revised Clinical Interview Schedule to measure depressive and anxiety disorders. SEP was measured by Registrar General Social Class in childhood (ages 7, 11 and 16 years) and adulthood (ages 23, 33 and 42 years). Internalising and externalising disorders were also measured in childhood.
Results
Cumulative manual SEP in childhood was weakly associated with increased risk of mid-life disorder. Childhood internalising and externalising disorders were associated with less upward social mobility and manual adult social position. Psychological disorder on three occasions in childhood was associated with manual adult occupational status (OR = 3.33, 95% CI 2.63–4.21) even after adjusting for childhood SEP and malaise score at 42 years.
Conclusions
Both social causation and health selection contribute to the association of childhood socioeconomic disadvantage and mid-life depressive and anxiety disorders. Tackling accumulation of disadvantage and understanding and treating childhood psychological disorders and their educational and occupational consequences could reduce the risk of mid-life psychiatric disorders.
Keywords: Social class, Depression, Anxiety disorders, Cohort studies, Causality
Introduction
Exposure to socioeconomic disadvantage in childhood as well as adulthood may explain the association of adult depressive and anxiety disorders with manual socioeconomic position (SEP) [2, 14, 25, 29, 41]. In social causation models, childhood SEP directly predicts adult psychiatric disorder, largely depressive and anxiety disorders. There are several models for social causation across the life course; childhood socioeconomic disadvantage may be linked to adult psychiatric disorder by either ‘critical period’ pathway or risk accumulation models [15, 21, 24]. In critical period models, there is exposure to socioeconomic disadvantage in childhood whose effects, sometimes on biological systems, such as the HPA axis, remain latent until adulthood and whose effects are independent of adult exposure to adversity. In pathway models, exposure to socioeconomic disadvantage in childhood sets up a life course trajectory in which early exposure to disadvantage tends to lead to further disadvantage which increases the risk of psychiatric disorders. Socioeconomic disadvantage may include experiences of repeated disappointment and lack of opportunity contributing to low aspirations and negative affectivity; interrupted or low quality parenting (parental loss, poor parental mental health, low parental expectations, caregiver changes), residential mobility and lack of access to social and human capital [7, 18, 35]: psychosocial risk factors outside the scope of this paper. Across the life course, greater exposure to negative life events, less resources and coping skills to deal with them may increase the risk of psychological disorder [2, 9]. An important linking factor may be education: socioeconomic disadvantage will restrict access to education, may mean it is less valued, and if educational attainment is subsequently low, may restrict employment opportunities and the development of human capital [32, 46].
In this paper, risk accumulation, or cumulative socioeconomic disadvantage, refers to repeated exposure to hardship across the life course as measured by own or parental manual SEP. Socioeconomic disadvantage may also be associated with early onset of both mental and physical illness that may interfere with social and educational development and upward social mobility. Thus, associations between SEP and adult psychiatric disorder may also result from health selection whereby people with psychological disorder in childhood, either brought forward by childhood socioeconomic disadvantage or independently of SEP, are selected into manual adult SEP [6, 45]. Thus, childhood psychological disorder may influence adult social position.
A recent analysis of the 1958 British Birth Cohort reported that the association between manual childhood SEP at a single point (age 7 years) and increased risk of mid-life depressive and anxiety disorders was accounted for by adjustment for adult SEP [49]. This suggested that the influence of socioeconomic disadvantage in childhood on the risk of mid-life depressive and anxiety disorders in this cohort may be indirect and might be mediated through adult socioeconomic disadvantage. In contrast, other cohort studies show independent effects of childhood SEP on adult mental health [12, 14, 41]. Furthermore, the effect of adult SEP on risk of mid-life disorders was much diminished by adjustment for childhood psychological disorders. This paper examines the ways in which childhood SEP is linked to mid-life depressive and anxiety disorders in the 1958 Birth Cohort (Fig. 1). We examine the following questions: Is there evidence for an accumulation model (i.e. do effects of exposure to childhood and adulthood socioeconomic disadvantage accumulate to increase risk of adult disorder)? Is there evidence that the association of SEP and mid-life disorder results from health selection due to psychological disorder in childhood or early adulthood psychological distress?
Fig. 1.
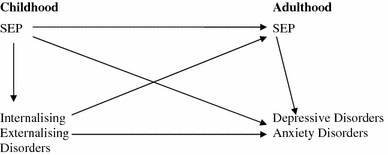
A model of lifecourse manual SEP and adult depressive and anxiety disorders
We hypothesise that (1) accumulation of exposure to socioeconomic disadvantage across childhood will be associated with increased risk of mid-life disorder independently of accumulation of exposure to socioeconomic disadvantage across adulthood; (2) cumulative exposure to socioeconomic disadvantage in childhood and adulthood will mediate the increased risk of mid-life disorders associated with childhood psychological disorders; and (3) childhood psychological disorder and early adulthood distress will influence mid-life SEP independently of childhood SEP and mid-life disorder.
Methods
The 1958 Birth Cohort commenced as a perinatal mortality survey [3] that recruited 98% of all births in England, Scotland and Wales during a week in March 1958. The cohort members have been followed up at ages 7, 11, 16, 23, 33, 42 years and with a biomedical follow-up at age 45 years [39]. During the childhood surveys, the sample was augmented by immigrants to the UK who were born in the study week giving a total sample of 18,558 participants. Data were obtained from parents and schools (teachers and doctors) on participants at ages 7, 11 and 16 years and through personal interviews at ages 23, 33 and 42 years. After exclusions for death, emigration, permanent refusal, armed forces and long-term non-contacts, 11,971 participants still in contact with the study at 45 years were invited to a nurse-led biomedical assessment including a computer-assisted personal interview. The achieved sample was 9,377 with a response rate of 72% of the contacted sample, representing 59% of the eligible sample. Ethical approval for the survey was given by the South East Multi-Centre Research Ethics Committee (MREC).
SEP
Adult social position was based on current or most recent occupation at 23, 33, and 42 years and categorised using the British Registrar General classification [33] as ‘I and II’ professional/managerial/technical, ‘IIINM’ other non-manual, ‘IIIM’ skilled manual, and ‘IV and V’ unskilled manual. Both men and women were allocated to a manual or non-manual SEP on the basis of their own occupation. Childhood SEP at birth, 7, 11 and 16 years was categorised by father’s occupation using the same classification. Childhood and adulthood SEP was categorised as non-manual (I, II, IINM) and manual (IIIM, IV, V) for analyses. Social position in adulthood was also measured by housing tenure at ages 23, 33, and 42 years distinguishing homeowners from people with public housing, private rental housing and other residential arrangements. SEP was measured across four occasions in childhood (at birth, 7, 11 and 16 years) and three in adulthood (at 23, 33 and 42 years). Summary indices of manual SEP were derived separately for childhood and adulthood. For each of these scales, a respondent was classified as manual if they occupied manual SEP on any two occasions: non-manual SEP or only one occasion of manual SEP was scored as non-manual.
Depressive and anxiety disorders
Depressive and anxiety disorders in the previous week were measured by the Depression and Anxiety modules of the Revised Clinical Interview Schedule [23] administered by a nurse using a computer-assisted personal interview at age 45 years. Diagnoses were derived according to standard algorithms for ICD-10 diagnoses. A summary measure of ‘any diagnosis’ was derived that included ‘generalised anxiety disorder’, ‘depressive episode’, ‘any phobia’ (excluding specific phobias), and ‘panic disorder.’ ‘Generalised anxiety disorder’ and ‘depressive episode’ were also examined as separate outcomes.
Early adulthood psychological distress
Psychological distress at age 23 years was measured by the Malaise Inventory [44], a reliable measure of emotional disturbance and somatic symptoms [42]. The inventory has demonstrated validity in this population; [42] reliability for the scales was high in our sample (age 23 years, α = 0.76, N = 7,910). The Malaise Inventory provides a total score and a dichotomous measure of high versus low psychological distress; a score of 7 and above indicates a high level of psychological distress [28].
Childhood psychological disorder
Psychological disorder, comprised of internalising and externalising disorders, at ages 7 and 11 years was measured using the teacher-rated Bristol Social Adjustment Guides [51] comprising 146 items of behaviour, each of which belongs to 1 of 12 separate syndromes. The top 13% were defined as psychologically distressed based on earlier studies [11]. Internalising and externalising disorders at age 16 years were measured using the teacher version of the Rutter Scales [8]. Scales were derived for internalising disorders (α = 0.66, N = 7,225) and externalising disorders (α = 0.88, N = 7,179). For each scale, the top 13% were defined as psychologically distressed [11]. A cumulative scale was devised, counting the number of times participants met the criteria for psychological disorder (internalising and externalising disorders) across the phases at 7, 11 and 16 years (ranging from 0 to 6).
Statistical analysis
Logistic regression analyses were conducted to examine independent associations between accumulation of (1) childhood and (2) adulthood SEP and mid-life disorders (any diagnosis, generalised anxiety disorder and depressive episode) adjusting for sex. The effects of childhood SEP were then adjusted for adult SEP and vice versa and then both were additionally adjusted for childhood psychological disorder. Separate analyses assessed the effect of childhood and adulthood housing tenure on mid-life disorders. Interactions between SEP and sex were examined to test whether social gradients differed between women and men in relation to diagnosis. Interactions between childhood and adulthood SEP and mid-life disorder examined whether the effects of childhood manual SEP were influenced by manual adult SEP. We then examined the association between childhood disorders and mid-life disorder, adjusting for sex, sex and childhood SEP, and sex, childhood and adulthood SEP. We also tested for interactions between childhood SEP and childhood psychological disorders to examine whether manual childhood SEP increased the association of childhood and mid-life disorder. In further logistic regression analyses, we examined the association between childhood psychological disorders and adulthood social position at 42 years, adjusting for sex, sex and childhood SEP, and sex, childhood SEP and adult psychological distress at 42 years. We carried out the same analyses using housing tenure at 42 years as the outcome. We tested for interactions between childhood SEP and childhood psychological disorder. Sobel tests assessed partial or full mediation of the effect of childhood manual SEP on mid-life disorder by adulthood SEP: this tests whether the reduction in variance explained by the childhood manual SEP after adjustment for the mediators is statistically significant [26, 48].
Multiple imputation was used to address missing data on the analyses, using the ICE programme in STATA (Version 8.2). All psychological health and SEP variables reported in this paper were included in the imputation equations. Qualifications completed by 33 years, employment status at 33 and 45 years and household tenure in childhood and adulthood were also included as they were significantly associated with attrition [5]. All participants except 1,245 who had died during the course of the study were included in the imputation, but analyses were conducted only for those who participated in the 45-year study. Only four imputed values were used in the analyses of the dependent variable—depressive and anxiety disorders at 45 years. Missing data on the independent variables ranged from 3.5 to 18% except for social class at 16 years (26%), tenure at 16 years (24%), externalising at 16 years (23%) and internalising at 16 years (22%). Five imputation cycles were run and analyses indicated that the measures were stable across the imputations. Parameter estimates were combined across the five imputations using the MICOMBINE command in STATA. In order to address attrition, inverse probability weights were then estimated from a logistic regression model predicting participation in the 45-year study. Sex, all of the independent variables used in the imputation equations (except those measured at 45 years), and all significant two-way interactions linking independent variables with participation were used as predictors in this logistic regression. The weight was applied to all analyses presented in this paper. We also repeated these analyses using complete case analysis.
Results
At age 45 years, 6% of the total sample met the criteria for mid-life disorder (7.2% of women; 4.8% of men) [49]. Amongst participants with paternal manual SEP at age 7 years, 55.3% attained non-manual SEP by age 42 years.
Cumulative manual SEP and mid-life disorders
We examined the effects of repeated exposure to manual SEP in childhood and adulthood on risk of adult disorders (Table 1). Being in manual SEP two or more times during childhood was associated with a greater risk of any diagnosis at mid-life compared to those who were classified as being in manual SEP one or less times; this association was only marginally significant after adjustment for cumulative adulthood SEP and became non-significant after adjustment for child psychological disorder. A similar pattern of results was found when repeating the analyses using housing tenure during childhood instead. We then repeated the analyses using generalised anxiety disorder and depressive episode as outcomes at 45 years instead of any diagnosis. Both being in manual SEP in childhood and renting childhood tenure were more associated with generalised anxiety disorder (manual SEP: OR = 1.28, 95% CI 0.95–1.72; renting tenure: OR = 1.35, 95% CI 1.09–1.76) than with depressive episode (manual SEP: OR = 1.01, 95% CI 0.69–1.50; renting tenure: OR = 1.16, 95% CI 0.83–1.63) adjusting for sex, adult SEP or tenure, respectively, and childhood psychological disorder.
Table 1.
Associations of childhood and adulthood socioeconomic position and tenure with any diagnosis at 45 years adjusted for sex and childhood psychological disorder (N = 9,377): current prevalence and odds ratios
| N | % with any diagnosis | Adjusted for sex | Adjusted for sex and childhood or adulthood SEPa | Adjusted for sex, childhood or adulthood SEP, and childhood psychological disorder | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Socioeconomic position | ||||||||
| Childhood SEPb,c | ||||||||
| 0–1 times in manual | 2,614 | 4.7 | 1.00 | 1.00 | 1.00 | |||
| 2 or more times in manual | 6,763 | 6.7 | 1.46*** | 1.15, 1.85 | 1.28* | 1.00, 1.62 | 1.18 | 0.92, 1.51 |
| Adulthood SEPb,c | ||||||||
| 0–1 times in manual | 5,772 | 5.5 | 1.00 | 1.00 | 1.00 | |||
| 2 or more times in manual | 3,605 | 7.2 | 1.63*** | 1.31, 2.06 | 1.55*** | 1.23, 1.96 | 1.27* | 1.14, 1.80 |
| Adulthood SEP for malesb,c | ||||||||
| 0–1 times in manual | 3,584 | 3.7 | 1.00 | 1.00 | 1.00 | |||
| 2 or more times in manual | 1,081 | 8.4 | 1.21 | 0.85, 1.73 | 1.07 | 0.75, 1.55 | 0.88 | 0.60, 1.29 |
| Adulthood SEP for femalesb,c | ||||||||
| 0–1 times in manual | 3,586 | 5.6 | 1.00 | 1.00 | 1.00 | |||
| 2 or more times in manual | 1,126 | 12.5 | 2.03*** | 1.57, 2.63 | 1.98*** | 1.51, 2.61 | 1.63*** | 1.24, 2.16 |
| N | % with any diagnosis | Adjusted for sex | Adjusted for sex and childhood or adulthood tenurea | Adjusted for sex, childhood or adulthood tenure, and childhood psychological disorder | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Tenure | ||||||||
| Childhood tenureb,c | ||||||||
| 0–1 times in rented | 4,533 | 4.9 | 1.00 | 1.00 | 1.00 | |||
| 2 or more times in rented | 4,844 | 7.2 | 1.57*** | 1.30, 1.91 | 1.30** | 1.07, 1.59 | 1.22 | 0.99, 1.49 |
| Adulthood tenureb,c | ||||||||
| 0–1 times in rented | 7,170 | 4.7 | 1.00 | 1.00 | 1.00 | |||
| 2 or more times in rented | 2,207 | 10.5 | 2.51*** | 2.09, 3.03 | 2.37*** | 1.97, 2.85 | 2.04*** | 1.69, 2.48 |
% and N not weighted: all other analyses imputed and weighted
* p = 0.05, ** p = 0.01, *** p = 0.001
aChildhood SEP model adjusted for adulthood SEP; adulthood SEP model adjusted for childhood SEP. Childhood tenure model adjusted for adulthood tenure: adulthood tenure model adjusted for childhood tenure
bNumber of times in manual social class or number of times in rented tenure
cInteraction between childhood SEP and adulthood SEP p = 0.917; interaction between sex and childhood SEP p = 0.367; interaction between sex and adulthood SEP p = 0.016. Interaction between childhood tenure and adulthood tenure p = 0.239; interaction between sex and childhood tenure p = 0.115; interaction between sex and adulthood tenure p = 0.819
Accumulation of manual adult SEP was associated with increased risk of mid-life disorders which was undiminished by adjustment for childhood SEP. This association was diminished after further adjustment for childhood psychological disorder but remained statistically significant; strong associations were found using adulthood housing tenure instead of SEP (Table 1). The interaction between childhood and adult SEP that was tested to check whether there was evidence of moderation was not statistically significant. We then repeated the analyses using generalised anxiety disorder and depressive episode as outcomes at 45 years instead of any diagnosis. In contrast to the results with childhood SEP, there was a tendency for manual adult SEP to be more associated with depressive episode (manual SEP for females: OR = 1.84, 95% CI 1.22–2.77; renting tenure: OR = 2.22, 95% CI 1.61–3.07) than with generalised anxiety disorder (manual SEP: OR = 1.21, 95% CI 0.88–1.68; renting tenure: OR = 1.88, 95% CI 1.48–2.39) adjusting for sex, childhood SEP or tenure, and childhood psychological disorder. There was a significant interaction between adulthood SEP and sex (p = 0.049) for depressive episode, similar to that found with any diagnosis; this was not found for generalised anxiety disorder. Sobel tests reveal that adulthood SEP partially mediates the effect of childhood SEP on mid-life disorder (Sobel = 3.68, p < 0.001) and adulthood tenure partially mediates the effect of childhood tenure on mid-life disorders (Sobel = 8.17, p < 0.001). A similar pattern of results for the overall associations of childhood and adulthood SEP and mid-life disorders was shown in a complete case analysis.
The role of childhood psychological disorder
We examined the association between childhood psychological disorders and any diagnosis at 45 years (Table 2). Childhood psychological disorders were strongly associated with mid-life disorders. This association was reduced slightly by adjustment for childhood SEP and further reduced by adjustment for adulthood SEP suggesting partial mediation by exposure to childhood and adult disadvantage. Similar results were found for internalising and externalising disorders separately and when housing tenure was substituted for SEP. Similar results were also found when generalised anxiety disorder and depressive episode were the outcomes at 45 years. The interaction between childhood SEP and childhood psychological disorders was not statistically significant.
Table 2.
Relationship between childhood psychological disorder and any diagnosis at age 45 years, adjusted for childhood SEP and adulthood SEP (N = 9,377)
| N | % with diagnosis | Adjusted for sex | Adjusted for sex and childhood SEP | Adjusted for sex, childhood SEP, and adulthood SEP | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Childhood mental health | ||||||||
| 0 | 5,111 | 4.6 | 1.00 | 1.00 | 1.00 | |||
| 1 | 2,468 | 6.5 | 1.50*** | 1.20, 1.88 | 1.46*** | 1.17, 1.84 | 1.43** | 1.14, 1.80 |
| 2 | 1,127 | 8.5 | 2.10*** | 1.55, 2.86 | 2.05*** | 1.51, 2.79 | 1.90*** | 1.38, 2.63 |
| 3 or more | 671 | 11.4 | 3.19*** | 2.36, 4.31 | 3.08*** | 2.27, 4.18 | 2.81*** | 2.07, 3.82 |
| Any internalising 7, 11 or 16 years | ||||||||
| No | 6,504 | 5.1 | 1.00 | 1.00 | 1.00 | |||
| Yes | 2,873 | 8.1 | 1.75*** | 1.45, 2.12 | 1.70*** | 1.41, 2.07 | 1.60*** | 1.31, 1.95 |
| Any externalising 7, 11 or 16 | ||||||||
| No | 6,949 | 5.3 | 1.00 | 1.00 | 1.00 | |||
| Yes | 2,428 | 8.1 | 1.74*** | 1.42, 2.11 | 1.68*** | 1.38, 2.05 | 1.56*** | 1.28, 1.92 |
% and N not weighted: all other analyses imputed and weighted. No significant interactions with: childhood psychological disorder × childhood SEP = 0.673, 0.868, 0.693; internalising × childhood SEP = 0.730; externalising × childhood SEP = 0.776
* p = 0.05, ** p = 0.01, *** p = 0.001
To assess potential health selection, we examined the proportion of participants with upward social mobility between ages 7 and 42 years by any childhood psychological disorder. In those without childhood psychological disorder, 65.3% of manual SEP in childhood became non-manual in adulthood, whereas in those with childhood psychological disorder 45.3% of manual SEP became non-manual. Odds ratios for the association between childhood psychological disorders and SEP at age 42 years adjusted for sex are reported in Table 3. Any internalising or externalising disorder at 7, 11 or 16 years and psychological distress at 23 years were strongly associated with manual SEP at age 42 years. These associations diminished slightly after adjustment for childhood SEP with little change after additionally adjusting for malaise score at 42 years. A similar pattern of results was shown for a complete case analysis. Strong associations were also found for childhood psychological disorder and housing tenure at 42 years adjusting for childhood tenure and malaise score at 42 years (Table 4). There was a significant interaction between any externalising disorder and childhood SEP. Consequently, we stratified the analysis by childhood SEP. A comparatively stronger association linked externalising disorders and being in manual SEP at 42 years amongst participants who had three or four reports of manual SEP in childhood (OR = 1.98, 95% CI 1.5–2.6; OR = 1.85, 95% CI 1.6–2.2) relative to participants who had not been in manual SEP (OR = 1.52, 95% CI 1.0–2.2). There was no interaction between childhood SEP and childhood psychological disorder. The odds ratios for SEP at 42 years by psychological distress at 23 years remained consistent despite adjustments.
Table 3.
Relationship between childhood psychological disorder and social class at 42 years, adjusted for the childhood SEP and malaise 42 years (N = 9,377)
| N | Adjusted for sex | Adjusted sex and childhood SEP | Adjusted sex, childhood SEP, and psychological disorder at 42 years | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Childhood mental health | |||||||
| 0 | 5,111 | 1.00 | 1.00 | 1.00 | |||
| 1 | 2,468 | 1.65*** | 1.47, 1.86 | 1.53*** | 1.36, 1.72 | 1.51*** | 1.34, 1.70 |
| 2 | 1,127 | 3.02*** | 2.45, 3.74 | 2.70*** | 2.18, 3.35 | 2.63*** | 2.13, 3.25 |
| 3 or more | 671 | 4.05*** | 3.21, 5.10 | 3.50*** | 2.76, 4.42 | 3.33*** | 2.63, 4.21 |
| Any internalising 7, 11 or 16 | |||||||
| No | 6,504 | 1.00 | 1.00 | 1.00 | |||
| Yes | 2,873 | 2.16*** | 1.95, 2.39 | 2.01*** | 1.81, 2.23 | 1.95*** | 1.76, 2.17 |
| Any externalising 7, 11 or 16 | |||||||
| No | 6,949 | 1.00 | 1.00 | 1.00 | |||
| Yes | 2,428 | 2.01*** | 1.77, 2.30 | 1.82*** | 1.60, 2.09 | 1.77*** | 1.55, 2.03 |
| Malaise 23 | |||||||
| No | 8,418 | 1.00 | 1.00 | 1.00 | |||
| Yes | 959 | 1.99*** | 1.66, 2.40 | 1.77*** | 1.47, 2.16 | 1.57*** | 1.29, 1.92 |
% and N not weighted: all other analyses imputed and weighted. No significant interactions with sex: childhood psychological disorder × sex = 0.282, 0.518, 0.535; internalising × sex 0.923; externalising × sex = 0.685; malaise 23 × sex = 0.584
* p = 0.05, ** p = 0.01, *** p = 0.001
Table 4.
Relationship between childhood psychological disorder and rented tenure at 42 years, adjusted for the childhood tenure and malaise 42 years (N = 9,377)
| N | Adjusted for sex | Adjusted sex and childhood tenure | Adjusted sex, childhood tenure, and psychological health at 42 years | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Childhood mental health | |||||||
| 0 | 5,111 | 1.00 | 1.00 | 1.00 | |||
| 1 | 2,467 | 1.78*** | 1.53, 2.06 | 1.69*** | 1.46, 1.97 | 1.63*** | 1.40, 1.90 |
| 2 | 1,127 | 3.10*** | 2.50, 3.86 | 2.84*** | 2.30, 3.50 | 2.67*** | 2.16, 3.29 |
| 3 or more | 671 | 5.49*** | 4.49, 6.71 | 4.79*** | 2.30, 3.50 | 4.30*** | 3.53, 5.23 |
| Any internalising 7, 11 or 16 | |||||||
| No | 6,504 | 1.00 | 1.00 | 1.00 | |||
| Yes | 2,873 | 2.28*** | 2.02, 2.57 | 2.14*** | 1.89, 2.41 | 2.02*** | 1.78, 2.29 |
| Any externalising 7, 11 or 16 | |||||||
| No | 6,949 | 1.00 | 1.00 | 1.00 | |||
| Yes | 2,428 | 2.43*** | 2.13, 2.78 | 2.24*** | 1.96, 2.57 | 2.13*** | 1.86, 2.43 |
| Malaise 23 | |||||||
| No | 8,418 | 1.00 | 1.00 | 1.00 | |||
| Yes | 959 | 2.60*** | 2.19, 3.07 | 2.33*** | 1.97, 2.77 | 1.80*** | 1.51, 2.15 |
% and N not weighted: all other analyses imputed and weighted. No significant interactions with sex: childhood psychological disorder × sex = 0.711, 0.822, 0.828; internalising × sex 0.998; externalising × sex = 0.254; malaise 23 × sex = 0.666
* p = 0.05, ** p = 0.01, *** p = 0.001
Discussion
Earlier studies have established the social gradient in malaise score at 23 and 33 years in this cohort [36, 38]. In this study, being socioeconomically disadvantaged in childhood only marginally increased the risk of mid-life disorder weakly supporting hypothesis 1 that accumulation of manual SEP in childhood is associated with increased risk of mid-life disorder independently of adult SEP. Part of the effects of childhood socioeconomic disadvantage were mediated through adult SEP. Being less socially advantaged in childhood and adulthood only partially mediated the association between childhood psychological disorders and mid-life disorder (hypothesis 2) meaning that the association between childhood psychological disorder and mid-life disorder was not explained by childhood or adulthood SEP. Childhood psychological disorder and early adulthood distress were associated with manual SEP and renting housing tenure in adulthood even after adjusting for childhood SEP, confirming health selection (hypothesis 3).
Strengths and weaknesses of the study
The main limitation of longitudinal study analysis is sample attrition and missing data. Indeed, missing data on manual SEP have been associated with poor mental health in this dataset. While the methods (imputation and weights) were designed to minimise the possible influence of attrition on findings [1, 50], we cannot be sure whether the results have not been influenced by attrition. Registrar General Social Class is not always sensitive to recent changes in occupational structure, may be less meaningful in women [10] and shows less consistent associations with mental health compared to income, economic difficulties and education [9, 22] but similar results were found using housing tenure. There are limitations to the Bristol Social Adjustment Guide and the Rutter Scales. These are less precise than some modern instruments. The absence of measures of parental psychopathology is a limitation but previous studies have found that this does not explain the association of parental SEP and later child disorder [16].
Registrar General Social Class, based on occupation, measures both social prestige and material resources, as the status of an occupation is usually strongly associated with income [10, 19]. It is not an ideal measure for partialling out effects of social prestige from the effects of materialist explanations of social gradients. Material socioeconomic disadvantage is partly a risk factor for depressive and anxiety disorders because loss events, including, e.g., death of close persons, unemployment and ill-health are more frequently associated with manual SEP while access to material resources that can help buffer life events is less available [7]. On the other hand, social prestige may be more important in the causation of depressive and anxiety disorders than for physical illness [2, 13].
Accumulation of risk
In earlier analyses in this study, manual SEP in childhood only weakly predicted adult diagnoses but did predict adult depressive symptoms [40]. We found that the effect of cumulative childhood manual SEP was minimal after adjustment for adult SEP, while the cumulative effects of adult SEP were not influenced by adjustment for childhood SEP. The weaker associations with childhood SEP may partly reflect the greater time distance between SEP in childhood, compared to adult SEP, and mid-life disorder. However, other longitudinal studies have also found little or inconsistent associations between childhood SEP and either early adult [34] or mid-life disorder [20]. Childhood SEP has also predicted early adult anxiety disorders but not depressive disorders [30]; this is similar to our results in which childhood SEP was more strongly associated with generalised anxiety disorder at 45 years than with depressive episode. It seems possible that the effects of manual childhood SEP have less long-term effect in the intergenerationally upwardly mobile, similar to the findings with self-rated health [37]. The effects of cumulative adult manual SEP were confined to women which we had not predicted. However, in analyses with tenure rather than SEP, there was no sex interaction suggesting this result may be specifically related to SEP rather than the effect of material disadvantage being greater in women than men. Our findings weakly support either a pathway or an accumulation model linking childhood SEP and the risk of mid-life disorders [17]. They do not fit a ‘critical period’ model [19]. Investigation of predictors of psychosocial adjustment and educational achievement in childhood in this cohort favours a pathway model with material deprivation and family involvement as mediating factors [46]. It may be that the effect of manual childhood SEP is attenuated or modified by mid-life.
Health selection
In this study, we also found evidence for health selection in which having childhood psychological disorders increased the risk of being in manual SEP, or holding public or private rented housing tenure in adulthood [45]. Childhood psychological disorder affected adult SEP despite adjustment for childhood SEP and malaise at 42 years. The pattern of results was very similar in women and men despite the greater prevalence of psychiatric disorder in women and the different meaning of SEP in adult women and men. Poor self-rated health that often includes an element of mental health has also been associated with modest downward social mobility in this cohort [27]. In keeping with our finding that health selection associated with externalising disorder was increased by exposure to childhood manual SEP, Johnson et al. [16] found that childhood disruptive disorders predicted poor educational attainment. Manual SEP might increase the risk of academic failure and social exclusion in a child with ‘behaviour problems’. However, evidence for health selection has not always been found in other studies predicting early adult depressive and anxiety disorders [16, 30, 41] but it may be that individuals were not followed for long enough.
Childhood SEP, childhood psychological disorders and mid-life disorders
Could the effects of SEP on mid-life disorders be partly mediated through mental ill-health beginning in childhood and persisting into adulthood [31, 36]? The association between childhood and adult disorder was only minimally diminished by adjustment for childhood SEP. The continuance of childhood psychological disorder into mid-life cannot be explained by childhood disadvantage. However, because childhood psychological disorder predicts manual SEP in adulthood and is also related to mid-life disorders, childhood psychological disorder may be a partial explanation of the association of adult SEP and mid-life disorders. This concurs with no SEP effect on common mental disorders in a UK national study after adjustment for prior mental health [47]. Childhood psychological disorder may increase the likelihood of manual SEP in adulthood [45], partially mediated through failure in educational attainment [43] and thence occupational position [31]; in this cohort, poor childhood health was related to lower average adult earnings and poorer educational attainment [4] and childhood mental ill-health has been linked to risk of adult unemployment [32]. Health selection is not confined to the transition between childhood and adulthood; distress in early adulthood can still exert a limiting effect on upward social mobility between early adulthood and mid-life.
Conclusions
In summary, we found that both social causation and health selection played a part in the influence of childhood SEP on risk of common mental disorder in mid-life. With an increasing time interval between childhood SEP and risk of adult disorder, the magnitude of direct effects of childhood SEP on mental health diminishes and the influence of selective effects become more obvious. The association between these childhood disorders, which impair educational attainment and work functioning, and SEP is likely to be reciprocal: socioeconomic disadvantage is a risk factor for these disorders which in turn may impede upward social mobility across the life course. Exposure to manual SEP, up to mid-life, confers increased risk of these disorders in mid-life. A positive implication of these results is that if there is intergenerational upward mobility some of the risk associated with socioeconomically disadvantaged childhoods for these disorders can be diminished. Further research is needed on how childhood psychological disorders affect educational and occupational achievement. Paying greater attention to childhood and early adulthood psychological disorders and their consequences may yield benefits for mid-life mental health.
Acknowledgments
We thank the data providers: Centre for Longitudinal Studies, Institute of Education and National Birthday Trust Fund, National Children’s Bureau, City University Social Statistics Research Unit (original data producers). We thank Sam Harper for his comments on the paper. The biomedical examination was funded by Medical Research Council [G0000934], awarded under the Health of the Public initiative. Charlotte Clark is supported by an Engineering and Physical Sciences Research Fellowship. Bryan Rodgers is supported by Research Fellowships Nos 148948 and 366758 and by Program Grant No. 179805 from the National Health and Medical Research Council of Australia. Research at the Institute of Child Health and Great Ormond Street Hospital for Children NHS Trust benefits from R&D funding received from the NHS Executive.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Atherton K, Fuller E, Shepherd P, Strachan DP, Power C. Loss and representativeness in a biomedical survey at age 45 years: 1958 British birth cohort. J Epidemiol Community Health. 2008;622:16–23. doi: 10.1136/jech.2006.058966. [DOI] [PubMed] [Google Scholar]
- 2.Brown GW, Harris TO, Hepworth C. Loss, humiliation and entrapment among women developing depression: a patient and non-patient comparison. Psychol Med. 1995;25:7–21. doi: 10.1017/S003329170002804X. [DOI] [PubMed] [Google Scholar]
- 3.Butler NR, Bonham DG. Perinatal mortality: the first report of the 1958 British Perinatal Mortality Survey. Edinburgh: Churchill-Livingstone; 1963. [Google Scholar]
- 4.Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. J Health Econ. 2005;24:365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Clark C, Rodgers B, Caldwell T, Power C, Stansfeld S. Childhood and adulthood psychological ill health as predictors of mid-life affective and anxiety disorders: the 1958 British birth cohort. Arch Gen Psychiatry. 2007;64:668–678. doi: 10.1001/archpsyc.64.6.668. [DOI] [PubMed] [Google Scholar]
- 6.Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 7.Duncan GJ, Brooks-Gunn J. Consequences of growing up poor. New York: Russell Sage Foundation; 1997. [Google Scholar]
- 8.Elander J, Rutter M. Use and development of the Rutter parents’ and teachers’ scales. Int J Methods Psychiatr Res. 1996;6:63–78. doi: 10.1002/(SICI)1234-988X(199607)6:2<63::AID-MPR151>3.3.CO;2-M. [DOI] [Google Scholar]
- 9.Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders: a systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol. 2003;38:229–237. doi: 10.1007/s00127-003-0627-2. [DOI] [PubMed] [Google Scholar]
- 10.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1) J Epidemiol Community Health. 2006;60:7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghodsian M. Measuring behaviour in the school and home. In: Fogelman K, editor. Growing up in Britain. London: Macmillan Press; 1983. pp. 329–338. [Google Scholar]
- 12.Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Socioeconomic status in childhood and the lifetime risk of major depression. Int J Epidemiol. 2002;31(4):359–367. doi: 10.1093/ije/31.2.359. [DOI] [PubMed] [Google Scholar]
- 13.Griffin JM, Fuhrer R, Stansfeld SA, Marmot M. The importance of low control at work and home on depression and anxiety: do these effects vary by gender and social class? Soc Sci Med. 2002;54:783–798. doi: 10.1016/S0277-9536(01)00109-5. [DOI] [PubMed] [Google Scholar]
- 14.Harper S, Lynch J, Hsu WL, et al. Life course socioeconomic conditions and adult psychosocial functioning. Int J Epidemiol. 2002;31:395–403. doi: 10.1093/ije/31.2.395. [DOI] [PubMed] [Google Scholar]
- 15.Hertzman C, Power C. Child development as a determinant of health across the life course. Curr Paediatr. 2004;14:438–443. doi: 10.1016/j.cupe.2004.05.008. [DOI] [Google Scholar]
- 16.Johnson JG, Cohen P, Dohrenwend BP, et al. A longitudinal investigation of social causation and social selection processes involved in the association between socioeconomic status and psychiatric disorders. J Abnormal Psychol. 1999;108:490–499. doi: 10.1037/0021-843X.108.3.490. [DOI] [PubMed] [Google Scholar]
- 17.Kawachi I, Subramanian SV, Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health. 1999;56:647–652. doi: 10.1136/jech.56.9.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kendall GE, Li J. Early childhood socialization and social gradients in adult health: a commentary on Singh-Manoux and Marmot’s “Role of socialization in explaining social inequalities in health”. Soc Sci Med. 2005;61:2272–2276. doi: 10.1016/j.socscimed.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 19.Krieger N. A glossary for social epidemiology. J Epidemiol Community Health. 2001;55:693–700. doi: 10.1136/jech.55.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuh D, Hardy R, Rodgers B, Wadsworth ME. Lifetime risk factors for women’s psychological distress in midlife. Soc Sci Med. 2002;55:1957–1973. doi: 10.1016/S0277-9536(01)00324-0. [DOI] [PubMed] [Google Scholar]
- 21.Kuh D, Ben-Shlomo Y. A life course approach to chronic disease epidemiology. Oxford: Oxford University Press; 2004. [PubMed] [Google Scholar]
- 22.Laaksonen E, Martikainen P, Lahelma E, et al. Socioeconomic circumstances and common mental disorders among Finnish and British public sector employees: evidence from the Helsinki Health Study and the Whitehall II Study. Int J Epidemiol. 2007;36:776–786. doi: 10.1093/ije/dym074. [DOI] [PubMed] [Google Scholar]
- 23.Lewis G, Bebbington P, Brugha T, Farrell M, Gill B, Jenkins R, et al. Socio-economic status, standard of living, and neurotic disorder. Int Rev Psychiatry. 2003;15:91–96. doi: 10.1080/0954026021000045994. [DOI] [PubMed] [Google Scholar]
- 24.Ljung R, Hallqvist J. Accumulation of adverse socioeconomic position over the entire life course and the risk of myocardial infarction among men and women: results from the Stockholm Heart Epidemiology Program (SHEEP) J Epidemiol Community Health. 2006;60:1080–1084. doi: 10.1136/jech.2006.047670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 26.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manor O, Matthews S, Power C. Health selection: the role of inter- and intra-generational mobility on social inequalities in health. Soc Sci Med. 2003;57:2217–2227. doi: 10.1016/S0277-9536(03)00097-2. [DOI] [PubMed] [Google Scholar]
- 28.Matthews S, Manor O, Power C. Social inequalities in health: are there gender differences? Soc Sci Med. 1999;48:49–60. doi: 10.1016/S0277-9536(98)00288-3. [DOI] [PubMed] [Google Scholar]
- 29.Melzer D, Fryers T, Jenkins R. Social inequalities and the distribution of the common mental disorders. Hove and New York: Psychology Press, Taylor & Francis Group; 2004. [Google Scholar]
- 30.Miech RA, Caspi A, Moffitt TE, et al. Low socioeconomic status and mental disorders: a longitudinal study of selection and causation during young adulthood. Am J Sociol. 1999;104:1096–1131. doi: 10.1086/210137. [DOI] [Google Scholar]
- 31.Miech R, Power C, Eaton WW. Disparities in psychological distress across education and sex: a longitudinal analysis of their persistence within a cohort over 19 years. Ann Epidemiol. 2007;17:289–295. doi: 10.1016/j.annepidem.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 32.Montgomery SM, Bartley MJ, Cook DG, et al. Health and social precursors of unemployment in young men in Great Britain. J Epidemiol Community Health. 1996;50:415–422. doi: 10.1136/jech.50.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Office of Population Census and Surveys (1980) Classification of occupations. HMSO, London
- 34.Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, Moffitt TE. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360:1640–1645. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poulton R, Caspi A. Commentary: how does socioeconomic disadvantage during childhood damage health in adulthood? Testing psychosocial pathways. Int J Epidemiol. 2005;434:344–345. doi: 10.1093/ije/dyi044. [DOI] [PubMed] [Google Scholar]
- 36.Power C, Manor O. Explaining social class differences in psychological health among young adults: a longitudinal perspective. Soc Psychiatry Psychiatr Epidemiol. 1992;27:284–291. doi: 10.1007/BF00788900. [DOI] [PubMed] [Google Scholar]
- 37.Power C, Manor O, Matthews S. The duration and timing of exposure: effects of socioeconomic environment on adult health. Am J Public Health. 1999;89:1059–1065. doi: 10.2105/AJPH.89.7.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Power C, Stansfeld SA, Matthews S, et al. Childhood and adulthood risk factors for socio-economic differentials in psychological distress: evidence from the 1958 British birth cohort. Soc Sci Med. 2002;55:1989–2004. doi: 10.1016/S0277-9536(01)00325-2. [DOI] [PubMed] [Google Scholar]
- 39.Power C, Elliott J. Cohort profile: 1958 British birth cohort (National Child Development Study) Int J Epidemiol. 2006;35:34–41. doi: 10.1093/ije/dyi183. [DOI] [PubMed] [Google Scholar]
- 40.Power C, Atherton K, Strachan DP, Shepherd P, Fuller E, Davis A, et al. Life-course influences on health in British adults: effects of socio-economic position in childhood and adulthood. Int J Epidemiol. 2007;36:532–539. doi: 10.1093/ije/dyl310. [DOI] [PubMed] [Google Scholar]
- 41.Ritsher JE, Warner V, Johnson JG, Dohrenwend BP. Inter-generational longitudinal study of social class and depression: a test of social causation and social selection models. Br J Psychiatry Suppl. 2001;40:s84–s90. doi: 10.1192/bjp.178.40.s84. [DOI] [PubMed] [Google Scholar]
- 42.Rodgers B, Pickles A, Power C, Collishaw S, Maughan B. Validity of the Malaise Inventory in general population samples. Soc Psychiatry Psychiatr Epidemiol. 1999;34:333–341. doi: 10.1007/s001270050153. [DOI] [PubMed] [Google Scholar]
- 43.Rothon C, Head J, Clark C, Klineberg E, Cattell V, Stansfeld S (2008) The impact of psychological distress on the educational achievement of adolescents at the end of compulsory education. Soc Psychiatry Psychiatr Epidemiol [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 44.Rutter ML. Psycho-social disorders in childhood, and their outcome in adult life. J R Coll Physicians Lond. 1970;4:211–218. [PMC free article] [PubMed] [Google Scholar]
- 45.Rutter M. Childhood experiences and adult psychosocial functioning. Ciba Found Symp. 1991;156:189–200. doi: 10.1002/9780470514047.ch12. [DOI] [PubMed] [Google Scholar]
- 46.Sacker A, Schoon I, Bartley M. Social inequality in educational achievement and psychosocial adjustment throughout childhood: magnitude and mechanisms. Soc Sci Med. 2002;55:863–880. doi: 10.1016/S0277-9536(01)00228-3. [DOI] [PubMed] [Google Scholar]
- 47.Skapinakis P, Weich S, Lewis G, Singleton N, Araya R. Socio-economic position and common mental disorders. Longitudinal study in the general population in the UK. Br J Psychiatry. 2006;189:109–117. doi: 10.1192/bjp.bp.105.014449. [DOI] [PubMed] [Google Scholar]
- 48.Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. San Francisco: Jossey-Bas; 1982. pp. 290–312. [Google Scholar]
- 49.Stansfeld SA, Clark C, Rodgers B, Caldwell T, Power C. Childhood and adult socio-economic position and mid-life depressive and anxiety disorders. Brit J Psychiatry. 2008;192:152–153. doi: 10.1192/bjp.bp.107.043208. [DOI] [PubMed] [Google Scholar]
- 50.Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stott DH. The social adjustment of children. London, England: University of London Press; 1969. [Google Scholar]


