Abstract
Objective
To determine the effects of creation of a systemic to pulmonary venous atrial level communication (fenestration) at the time of the Fontan procedure on late outcomes.
Background
Fenestrations are frequently performed during Fontan procedures but late consequences are not well described.
Methods
Patient characteristics were compared between those with and without surgical fenestration among 536 subjects (mean 11.9 years) enrolled in the Pediatric Heart Network Fontan Cross-sectional Study. The status of the fenestration and the association of a currently patent fenestration with health status and measures of ventricular performance were investigated.
Results
Fenestration was performed in 361 patients (67%) and frequency differed by year and center (p<0.001 for each). After adjustment for center, age at Fontan, year of Fontan and prior superior cavopulmonary surgery, the fenestrated group had shorter length of Fontan hospital stay. At time of cross-sectional testing 8±3 years after Fontan, the fenestration remained open in 19% of subjects. Among those with confirmed fenestration closure, 59% were by catheter intervention, 1% by surgical intervention, and 40% had apparent spontaneous closure. Compared to those without evidence of a fenestration, subjects with a current fenestration were taking more medications (p=0.02) and had lower resting oxygen saturation (median 89 vs. 95%, p<.001). Functional health status, exercise performance, echocardiographic variables, prevalence of post Fontan stroke or thrombosis, and growth did not differ by current fenestration status.
Discussion
Surgical fenestration is associated with well demonstrated early postoperative benefits. This cross-sectional study found few associations between a persistent fenestration and deleterious later outcomes.
Keywords: Congenital Heart Disease, Cardiac surgery, Fontan procedure
Introduction
The Fontan procedure has provided excellent surgical palliation for many patients with functional single ventricle physiology and has evolved over time.(1) Creation of a systemic to pulmonary venous atrial level communication or fenestration at the time of Fontan completion may benefit patients by limiting Fontan pathway pressure and creating a right to left atrial shunt which may augment cardiac output and limit central venous pressure in the immediate postoperative period, at the expense of systemic desaturation with potential long term sequelae. Retrospective, single center reports suggest that in high risk patients, those with a fenestrated Fontan have shorter duration of pleural effusion and shorter length of hospital stay.(2,3) Subsequently, similar short term perioperative benefits of fenestration creation have been shown in a single center randomized study involving standard risk patients.(4) Although this procedure is now commonly performed, long-term benefits, if any, are not documented. Additionally, concerns remain about the need for later intervention to close the fenestration, as well as risks of persistent cyanosis and paradoxical embolization in patients with patent fenestrations.
The Pediatric Heart Network (PHN) Fontan Cross-Sectional database (5) provides a very well characterized cohort of surviving subjects from seven North American centers in which to examine whether creation of a fenestration at the time of Fontan is associated with long-term health status, medical complications, or laboratory measures of cardiac function. Additionally, comparisons can be made between subjects with a currently patent fenestration and those without.
Methods
Data for analyses described here were obtained from 536 subjects enrolled from seven clinical centers participating in the NIH/NHLBI-funded PHN Fontan Cross-Sectional Study. Subjects in this study were survivors of multi-stage surgical palliation for functional single ventricle culminating in a Fontan procedure who were aged 6 to 18 years at the time of sampling. Medical records were screened for 1078 patients, of whom 831 (77%) were deemed potentially eligible for participation. After being contacted, 637 patients (60%) were fully eligible, and consent was obtained for 546 (86%). Subjects with a hepatic vein exclusion procedure (n=10) were excluded from this analysis. The median time between Fontan surgery and study enrollment was 8.1 years. Complete details of the study design have been previously published.(6)
Measurements
Demographic data and descriptors of medical history before, during, and following the Fontan procedure were obtained by medical record review. Standardized assessment of functional health status was obtained using the Parent Report Child Health Questionnaire (CHQ P50). Physical performance was assessed using bicycle ergometry. (7) Ventricular size, function, atrioventricular valve and semilunar valve regurgitation as well as fenestration status were obtained using centrally-interpreted echocardiographic measurements. Resting brain natriuretic peptide concentration (BNP) was obtained and analyzed at a core laboratory.
Statistical Analysis
Exploratory analyses incorporating graphical and tabular displays assessed evidence in favor of trends and associations. Sample means, medians and proportions accompanied by 95% confidence intervals provided descriptive summaries. Crude comparisons of subjects with and without surgical fenestration employed Student’s t and chi-square test statistics. Covariate-adjusted comparisons were obtained by multiple linear and logistic regression analyses. Smoothed estimates of the proportion of subjects who underwent surgical fenestration was performed as a function of time were obtained using generalized additive mixed models with study center entered as a random effect. Graphical analyses of the time to hospital discharge following Fontan surgery for this cohort of Fontan survivors were performed using the Kaplan-Meier method, with significance testing via log rank tests, with covariate-adjusted models for time to discharge constructed using Cox proportional hazards regression. Analyses were performed using SAS software version 9.2 (SAS Institute, Cary, NC) and the R system version 2.8.1 (R Foundation for Statistical Computing, Vienna, Austria).
Adjustment for covariates
We have learned in previous analyses that many of the results of tests performed at the time of cross sectional evaluation differed among age groups. Exercise performance decreased with age.(7) Echocardiographic measured mass-to-volume ratio, dP/dt and Tei index also varied by age.(5) Therefore for outcomes measured at the time of cross-sectional testing (e.g.,CHQ-P50, echocardiography, and exercise testing) age adjusted comparisons are reported. Because the cohort of patients with a current fenestration were younger and followed for less time since Fontan completion, medical history variables collected since Fontan hospitalization are also reported using age-adjusted comparisons. Medication use among Fontan patients and performance of certain catheter interventions varied considerably across the seven participating centers in the PHN.(8,9) Therefore where center or era differences might exist we adjusted for subject age at Fontan cross sectional enrollment, year that Fontan surgery was performed, and study center. Based on previously observed association between the performance of cavopulmonary anastomosis (Stage II) procedures and fenestration performance, the presence or absence of a prior Stage II surgery was also included as a control factor in the post Fontan medical history outcomes.
The Fontan Cross-Sectional Study protocol was approved by the PHN Protocol Review Committee and an independent Data and Safety Monitoring Board, as well as Institutional Review Boards at each of the seven clinical centers and the Data Coordinating Center. All centers followed the same protocol and study procedures.
Results
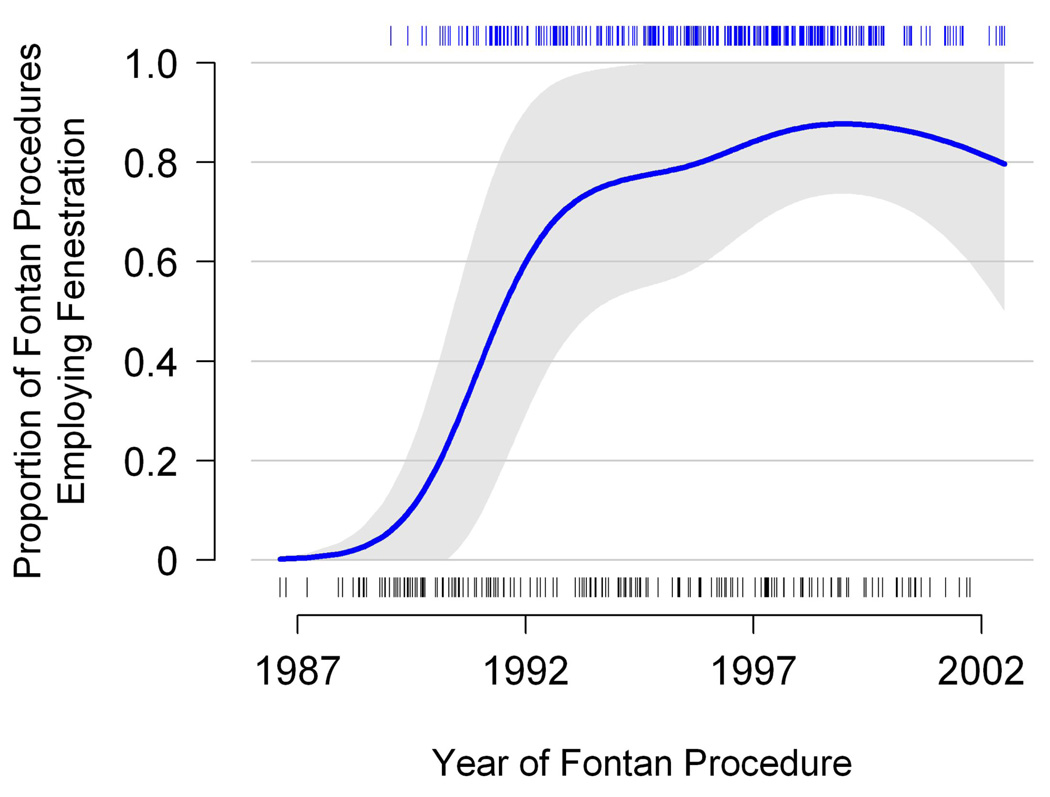
Among this enrolled cohort of Fontan survivors, there was a rapid increase in the performance of a surgical fenestration between 1987 and 1992 (Figure 1). After 1992, the proportion of Fontan procedures that included surgical fenestration remained about 80%. Although the use of fenestration increased over this time period at all centers, the percentage of subjects receiving a fenestration varied widely among centers, (13% to 91 %, p <0.001).
Figure 1. Smoothed proportion of subjects with surgical fenestration, by year.
Rug plots at top and bottom record the dates of fenestrated and non-fenestrated procedures respectively. Estimated were obtained using generalized additive mixed models. A 95% confidence interval is displayed as a shaded region.
Medical History Prior to the Fontan Procedure
Subject and medical history characteristics before and at the Fontan procedure are shown in Table 1. Age at cross-sectional study enrollment was approximately two years older among the subjects with no surgical fenestration, 13.2±3.6 vs. 11.2±3.2, p<.001. Subjects who underwent fenestration were more likely to have had prior Stage II procedures, (84% vs. 54%, p=0.005); have significant pre-existing atrioventricular valve (AV) regurgitation (40% vs. 24%, p<0.001); and have had a history of thrombosis prior to the Fontan procedure (6% vs. 2%, p=0.04) than those who did not undergo fenestration. At the pre-Fontan catheterization, subjects who went on to have a fenestration had higher systemic arterial oxygen saturations (85±5% vs. 83±5%, p<0.001) and lower ventricular end diastolic pressures (7.6 vs. 8.3 mm Hg, p=0.02) compared to those who did not undergo fenestration. When adjusted for center, age at enrollment, and year of Fontan procedure, there was no difference in numbers of surgical procedures and catheter interventions prior to Fontan completion between subjects who did and did not undergo surgical fenestration.
Table 1.
Patient Characteristics by Surgical Fenestration Status.
| Fenestration (N=361) Mean ± SD or % |
No Fenestration (N=175) Mean ± SD or % |
P-Value | |
|---|---|---|---|
| DEMOGRAPHICS | |||
| Age at study enrollment, years | 11.2±3.2 | 13.2±3.6 | <.001 |
| Age at Fontan, years | 3.5±2.3 | 3.3±1.8 | 0.4 |
| Male | 60% | 58% | 0.6 |
| MEDICAL HISTORY: PRIOR TO FONTAN PROCEDURE | |||
| Anatomy | 0.3 | ||
| Double Inlet Left Ventricle | 13% | 18% | |
| Mitral atresia | 6% | 5% | |
| Tricuspid atresia | 21% | 26% | |
| Unbalanced Atrioventricular canal | 4% | 5% | |
| Heterotaxy | 8% | 7% | |
| Hypoplastic left heart syndrome | 23% | 15% | .06 |
| Other | 26% | 24% | |
| Stage II performed | 84% | 54% | .005* |
| Prior surgical procedures | 3.3 ± 2.0 | 2.5 ± 1.7 | 0.3* |
| Prior non-stage II surgeries | 2.4 ± 1.9 | 1.9± 1.5 | 0.3* |
| Prior Catheter interventions | 0.9 ± 1.2 | 0.4 ± 0.7 | 0.2* |
| Severity of AV valve regurgitation | <.001 | ||
| None/trivial | 60% | 76% | |
| Mild | 33% | 23% | |
| Moderate/severe | 7% | 1% | |
| EDP, mmHg | 7.6±3.4 | 8.3±3.0 | 0.02 |
| Mean PA pressure, mmHg | 11.2±3.1 | 11.8±3.9 | 0.1 |
| Oxygen saturation, % | 84.6±4.9 | 82.8±5.3 | <.001 |
| Decreased ventricular function | 18% | 17% | 0.9 |
| Arrhythmia | 20% | 24% | 0.3 |
| Thrombosis | 6% | 2% | 0.04 |
| MEDICAL HISTORY: FONTAN PROCEDURE | |||
| Weight for age at Fontan, percentile | 26±28 | 28±27 | 0.5 |
| Height for age at Fontan, percentile | 32±29 | 32±28 | 0.8 |
| Type of Fontan | <.001 | ||
| AP connection | 6% | 30% | |
| TCPC intracardiac tunnel | 65% | 45% | |
| TCPC extracardiac tunnel | 14% | 12% | |
| TCPC extracardiac conduit | 15% | 8% | |
| Other | 1% | 5% | |
adjusted for center, age at enrollment, year of Fontan
LV= left ventricle, RV= right ventricle, AV= atrioventricular. EDP= end diastolic pressure, PA= pulmonary artery, AP = atriopulmonary, TCPC= total cavopulmonary connection
Consistent with the association with age and era, surgical fenestration was related to the type of Fontan procedure performed; fenestration was more prevalent among subjects with total cavopulmonary connections and less prevalent among subjects on whom an atriopulmonary connection was performed.
Status Following Fontan Procedure
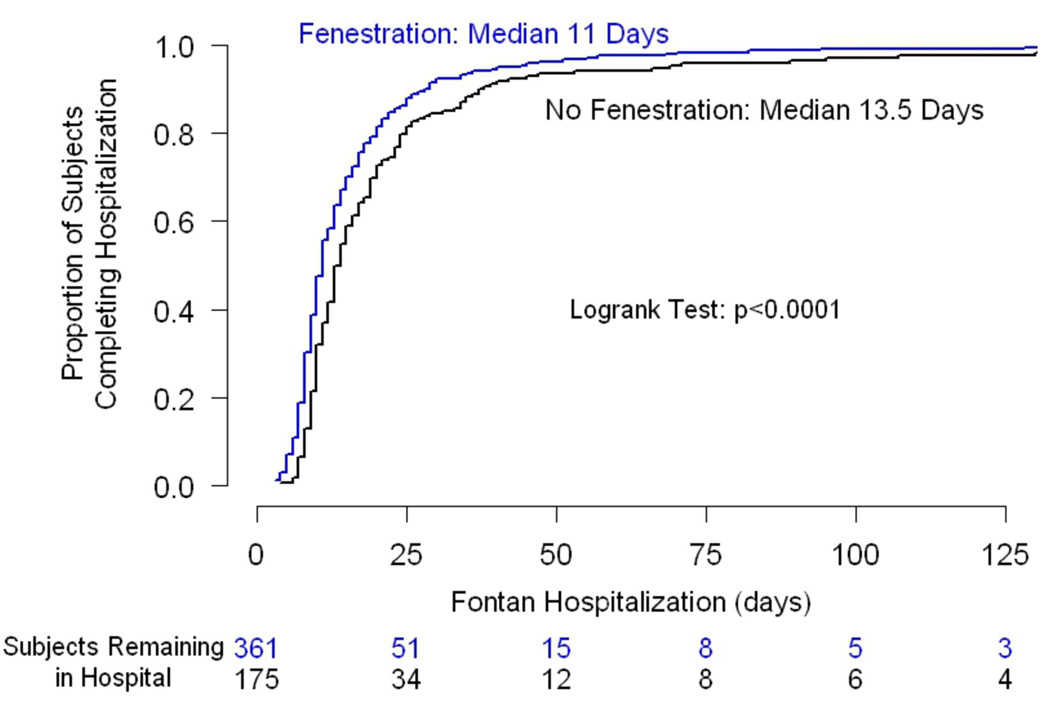
Subjects with surgical fenestration had median length of stay approximately 2.5 days shorter than subjects without fenestration (p<0.001) (Figure 2). This association remained significant after adjusting for study center, age at enrollment, year of Fontan, and performance of a Stage II procedure (p=0.05).
Figure 2. Proportion of subjects achieving hospital discharge following the Fontan procedure, as a function of time since the start of the Fontan hospitalization.
Proportion estimates were obtained using the Kaplan-Meier method in this cohort of Fontan survivors enrolling in this cross sectional study.
Medical history during and after the Fontan hospitalization is shown in Table 2. After adjusting for age, year at Fontan, and performance of a Stage II procedure, we found associations between surgical fenestration and increased number of discharge medications and increased number of post Fontan catheter interventions (excluding procedures related to the fenestration itself). The two most common catheter interventions performed in the fenestrated group were coiling of systemic venous collateral and coiling of aortopulmonary collaterals.
Table 2.
Status After Fontan Surgery.
| Fenestration | No Fenestration | Adjusted | ||||
|---|---|---|---|---|---|---|
| Characteristics | Mean±SD/% | Median | Mean±SD/% | Median | P | P* |
| N | 361 | 175 | ||||
| Length of hospital stay (days) | 16.1±20.1 | 11.0 | 21.9±26.0 | 13.5 | <.001 | 0.05 |
| Postoperative complications (#) | 1.4±1.9 | 1.0 | 2.8±2.6 | 2.0 | <.001 | 0.3 |
| Pericardial effusion | 7% | 21% | <.001 | 0.3 | ||
| Pleural effusion | 21% | 35% | <.001 | 0.3 | ||
| Discharge medications (#) | 4±1 | 4 | 3±2 | 3 | 0.003 | 0.02 |
| Antithrombotic | 77% | 50% | <.001 | 0.02 | ||
| ACEi | 67% | 24% | <.001 | <.001 | ||
| Diuretics | 96% | 91% | 0.02 | 0.3 | ||
| POST-FONTAN | ||||||
| Catheter interventions (#) (Excluding fenestration related procedures) |
0.6±1.0 | 0.3±0.9 | 0.001 | 0.03 | ||
| Number of surgeries | 0.3±0.8 | 0.5±1.1 | 0.2 | 0.2 | ||
| Stroke | 2% | 1% | 0.5 | 0.3 | ||
| Thrombosis | 7% | 7% | 0.9 | 0.8 | ||
| PLE | 3% | 6% | 0.1 | 0.2 | ||
| Arrhythmia | 19% | 24% | 0.2 | 0.5 | ||
adjusted for center, year of Fontan, age at enrollment, and performance of Stage II
ACEi= angiotensin converting enzyme inhibtion, PLE= protein losing enteropathy
Fenestration was not associated with post-Fontan stroke, ventricular dysfunction, thrombosis, protein losing enteropathy (PLE), or arrhythmia even when the analyses were adjusted for age at enrollment, age at Fontan, center, and performance of a Stage II procedure.
Fate of the Surgical Fenestration
An echocardiographic core laboratory determined “current” fenestration status at study enrollment (a median 8.1 years after Fontan surgery) in 527 of the 536 subjects (98%). Of the 361 subjects who had surgical fenestration at Fontan, 356 had an available echocardiogram (99%). At the time of cross sectional testing the fenestration was open in 69 (19%) and closed in 227 (63%). It was not possible to clearly delineate the fenestration status in 60 (17%) of subjects.
In the 227 subjects who had a closed fenestration at study enrollment, 91 (40%) are assumed to have had spontaneous closure because no surgical procedures or catheter interventions were performed after the Fontan procedure. Of those subjects with an intervention;133 (59%) of these underwent closure by catheter intervention, and 3 (1%) underwent closure during a surgical procedure. For subjects who underwent fenestration closure, the mean interval between Fontan surgery and interventional closure was 8.5 ± 3.5 yr (range 1 day to 11 years). Considering only the catheter related fenestration closures, 116 were closed by a septal occluder device, 3 by a coil, and 14 by closure of a of a purse string placed around the fenestration at the time of Fontan surgery.
Comparisons of Subjects According to Current Fenestration Status
Comparisons of the 69 subjects who had an open fenestration at study enrollment to the 458 subjects without any atrial level communication assessed by study echocardiogram are shown in Table 3. The group with a current fenestration was younger and had been followed for less time since Fontan (mean 7.1 vs. 8.7 years, p<0.001). Those with a current fenestration were more likely to have had a prior Stage II procedure and to have an intra cardiac lateral tunnel type Fontan. Patients with a current fenestration had lower resting oxygen saturation than those without a current fenestration (89 vs. 95%, p<.001). The two groups did not differ with respect to functional health assessed by Child Health Questionnaire CHQ PF50 summary scores. Height and weight percentile calculated at the time of cross-sectional testing did not differ by fenestration status. Brain natriuretic peptide levels, angiographic and echocardiographic measures of ventricular performance, and exercise variables did not differ by current fenestration status, nor did they differ in respect to Post-Fontan complications, including number of additional interventional procedures, stroke, thrombosis, or PLE.
Table 3.
Subject Profiles by Current Fenestration Status.
| Fenestration (N = 69) Mean ± SD or % |
No Fenestration Detected (N = 458) Mean ± SD or % |
P-Value | |
|---|---|---|---|
| Age at enrollment, yrs | 10.7±3.3 | 12.0±3.4 | 0.002 |
| Age at Fontan, yrs | 3.7±2.3 | 3.4±2.1 | 0.3 |
| Years since Fontan | 7.1±3.2 | 8.7±3.5 | <.001 |
| Male | 61% | 59% | 0.9 |
| Stage II performed | 93% | 80% | 0.005* |
| Anatomy | 0.3 | ||
| Double Inlet Left Ventricle | 12% | 15% | |
| Mitral atresia | 7% | 5% | |
| Tricuspid atresia | 13% | 24% | |
| Unbalanced Atrioventricular canal | 3% | 4% | |
| Heterotaxy | 9% | 7% | |
| Hypoplastic left heart syndrome | 26% | 19% | |
| Other | 30% | 25% | |
| Type of Fontan | 0.001 | ||
| AP connection | 0% | 16% | |
| TCPC intracardiac tunnel | 80% | 56% | |
| TCPC extracardiac tunnel lateral | 9% | 14% | |
| TCPC extracardiac conduit | 10% | 13% | |
| Other | 1% | 2% | |
| Post Fontan Medical History | |||
| Weight for age at study, percentile | 29±28 | 35±31 | 0.2 |
| Height for age at study, percentile | 36±30 | 42±33 | 0.2 |
| Cardiac surgical procedures | 0.3±0.6 | 0.4±1.0 | 0.8* |
| Catheter interventions | 0.5±1.2 | 0.5±1.0 | 0.3* |
| Stroke | 0% | 2% | 1.0* |
| Thrombosis | 4% | 8% | 0.3* |
| PLE | 3% | 4% | 1.0* |
| Arrhythmia | 21% | 20% | 0.5* |
| Functional Health Assessed by Child Health Questionnaire (CHQ50) | |||
| Physical Summary Score | 46±10 | 45±12 | 0.4* |
| Psychosocial Summary Score | 46±11 | 48±11 | 0.8* |
| Echocardiography | |||
| Echo EF, % | 58±10 | 59±10 | 0.6* |
| Mass:volume ratio z score | 1.2±0.5 | 1.2±0.4 | 0.5* |
| dP/dt, mm Hg/s | 1575±1026 | 1374±908 | 0.3* |
| Exercise Testing | |||
| Resting O2 saturation (%) | 89±5 | 95±4 | <.001* |
| Peak VO2 (ml/kg/min) | 25±6 | 27±6 | 0.2* |
| % Predicted peak VO2 | 63±14 | 67±15 | 0.1* |
| VO2 at VAT (ml/kg/min) | 16±4 | 18±6 | 0.1* |
| % Predicted VO2 at VAT | 67±14 | 77±22 | 0.1* |
| BNP (pg/ml) | 34±72 | 25±44 | 1.0* |
Age-adjusted comparisons
LV= left ventricle, RV= right ventricle, AP = atriopulmonary, TCPC= total cavopulmonary connection, PLE= protein losing enteropathy, EDV= end diastolic volume, ESV= end systolic volume, EF=ejection fraction, O2= oxygen, VO2= maximal oxygen consumption, VAT= ventilatory anaerobic threshold
Discussion
We report a large multicenter cohort of single ventricle patients palliated with a Fontan procedure and demonstrate a dramatic change in surgical practice over time in the use of a surgical fenestration. Fenestration was first introduced in 1990 in an effort to improve the perioperative course for high-risk patients,(2) over 80% of subjects in our cohort had an atrial fenestration at the time of the Fontan operation after 1992. The population evaluated in this cross-sectional study included patients in the pre-fenestration era. Thus, the majority of subjects who did not have a fenestration were from the early time period. They were also somewhat older at the time of evaluation, less likely to have had a Stage II operation performed, and more likely to have had an atriopulmonary connection which was the methodology of the original Fontan operation.(9) In the current study we attempted to control for era effect by adjusting for patient age and year of Fontan and to control for practice variation by adjusting for study center. After adjusting for these factors, surgical fenestration was associated with decreased length of Fontan hospital stay. This cross-sectional study found few associations between a persistent fenestration and deleterious later outcomes.
Preoperative risk factors do not consistently identify patients who may have poorer outcomes after the Fontan procedure which has led some to suggest that some patients undergoing the Fontan do not require routine fenestration.(10,11) This large multi-center study supports the numerous single center reports indicating that an atrial fenestration carried out at the time of the Fontan operation shortens hospital stay.(3, 4, 12) Not appreciated in prior studies, we found an increased use of cardiac medications at discharge in the fenestration group. After adjusting for subject age and center, increased use of angiotensin converting enzyme inhibitors and antithrombotics in the fenestration group was still observed.
Although considerable data regarding the early post-operative effects of a fenestration at Fontan has been previously reported, the long-term sequelae of a fenestration on clinical outcomes are less well studied. We found subjects with a history of surgical fenestration at the time of the Fontan operation had significantly greater numbers of catheter interventions even after excluding procedures carried out for modification of the fenestration itself. One might attribute this finding to the modern era when interventions are more common. However, after correcting for patent age, year of Fontan and center, we continued to identify a greater number of post Fontan catheter interventions in the group who underwent surgical fenestration.
Closure of a surgical fenestration has been advocated because of complications associated with persistent cyanosis, and increased risk of systemic thromboembolism. As expected, we found resting arterial oxygen saturation was significantly lower among the 69 subjects who were documented to have a persistent fenestration at a median of 8 years following the Fontan procedure. However, an increased incidence of either stroke or thrombosis was not found among the patients with a persistent atrial communication. This is consistent with smaller single center reports that did not find a difference in number of strokes (13) or occurrence of thrombosis (12) in Fontan subjects with patent fenestrations. Additionally we found no differences in the number of surgical or catheter interventions, incidence of PLE or incidence of arrhythmia between those with a current fenestration and those without. Echocardiographic measurements of ventricular function and mass to volume ratio as well as exercise performance, BNP levels, and growth parameters were similar in the two groups. Our findings are consistent with previous reports demonstrating that fenestration closure does not positively or negatively affect exercise capacity.(14) Functional health status as assessed by the CHQ PF50 also did not differ by current fenestration status. Overall, despite lower resting oxygen saturation, we did not identify any deleterious effects of a persistent fenestration in our cohort.
The long term fate of the surgical fenestration has not been well described. In our cohort, 40% of subjects with a surgical fenestration had apparent spontaneous closure Although the timing of such spontaneous closure is unknown, this finding is consistent with prior small reports that have documented spontaneous closure of fenestrations in 29% of subjects within 3 months.(15) Multiple centers have reported methods for closing fenestration. Indications for the procedure have also been proposed and risk factors associated with closure have been described (16,17) Closure of a fenestration improves oxygenation and may reduce the use of anti-congestive medication, but may result in increased use of antiarrhythmic agents following closure.(17) Some have suggested that indications for routine fenestration closure should be reconsidered because of potential long term benefits of increased cardiac output and decreased tachyarrhythmias in patients with patent fenestrations late after Fontan procedures. (18)
Limitations
The study cohort was limited to surviving subjects who agreed to participate in this study. The fates of patients who were not enrolled are necessarily unknown. Furthermore, the effects of fenestration and of interventional closure on early or late mortality, if any, could not be assessed in a cross-sectional study. We utilized a central echocardiography core laboratory to determine current fenestration status but images were not available in 19 subjects (3%) and inadequate to determine the status of the fenestration in 60 subjects (17%). This may have limited the power to detect differences between those with and without a current fenestration.
Conclusions
The percentage of Fontan procedures which included surgically created atrial fenestrations increased rapidly over time in subjects enrolled in this multicenter study. Subjects who had surgical fenestration creation at Fontan had a shorter length of stay, but received more medications at hospital discharge. Most fenestrations were later closed in the catheterization laboratory; however, a significant percentage demonstrated spontaneous closure. Subjects with persistent fenestrations at the time of the cross-sectional study had significantly lower resting oxygen saturation. A persistent fenestration however, was not associated with exercise performance, echocardiographic function, or functional health status. Although patients with a current fenestration are theoretically at ongoing risk for thromboembolic events, there was not an increased incidence of these potentially serious complications during the eight year follow-up period. Further longitudinal follow up of this cohort is necessary to determine long term consequences of a persistent fenestration.
Acknowledgments
Funding: Supported by U01 grants from the National Heart, Lung, and Blood Institute (HL068269, HL068270, HL068279, HL068281, HL068285, HL068292, HL068290, HL068288)
Abbreviations
- AV
atrioventricular valve
- BNP
brain natriuretic peptide concentration
- CHQ P50
Parent Report Child Health Questionnaire
- PHN
Pediatric Heart Network
- PLE
protein losing enteropathy
- Stage II
cavopulmonary anastomosis
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
No relationship with industry exists.
Reference List
- 1.Khairy P, Poirier N, Mercier LA. Univentricular heart. Circulation. 2007;115:800–812. doi: 10.1161/CIRCULATIONAHA.105.592378. [DOI] [PubMed] [Google Scholar]
- 2.Bridges ND, Lock JE, Castaneda AR. Baffle fenestration with subsequent transcatheter closure. Modification of the Fontan operation for patients at increased risk. Circulation. 1990;82:1681–1689. doi: 10.1161/01.cir.82.5.1681. [DOI] [PubMed] [Google Scholar]
- 3.Bridges ND, Mayer JE, Jr, Lock JE, et al. Effect of baffle fenestration on outcome of the modified Fontan operation. Circulation. 1992;86:1762–1769. doi: 10.1161/01.cir.86.6.1762. [DOI] [PubMed] [Google Scholar]
- 4.Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C. Fenestration improves clinical outcome of the fontan procedure: a prospective, randomized study. Circulation. 2002;105:207–212. doi: 10.1161/hc0202.102237. [DOI] [PubMed] [Google Scholar]
- 5.Anderson PA, Sleeper LA, Mahony L, et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol. 2008;52:85–98. doi: 10.1016/j.jacc.2008.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sleeper LA, Anderson P, Hsu DT, et al. Design of a large cross-sectional study to facilitate future clinical trials in children with the Fontan palliation. Am Heart J. 2006;152:427–433. doi: 10.1016/j.ahj.2006.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paridon SM, Mitchell PD, Colan SD, et al. A cross-sectional study of exercise performance during the first 2 decades of life after the Fontan operation. J Am Coll Cardiol. 2008;52:99–107. doi: 10.1016/j.jacc.2008.02.081. [DOI] [PubMed] [Google Scholar]
- 8.Anderson PA, Atz AM, Breitbart RE, et al. The Fontan Patient: Present Medical Therapy at Seven Pediatric Cardiology Centers (abstr) Circulation. 2005;112:420. [Google Scholar]
- 9.Fontan F, Baudet E. Surgical repair of tricuspid atresia. Thorax. 1971;26:240–248. doi: 10.1136/thx.26.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsu DT, Quaegebeur JM, Ing FF, Selber EJ, Lamour JM, Gersony WM. Outcome after the single-stage, nonfenestrated Fontan procedure. Circulation. 1997;96 II-40. [PubMed] [Google Scholar]
- 11.Thompson LD, Petrossian E, McElhinney DB, et al. Is it necessary to routinely fenestrate an extracardiac fontan? J Am Coll Cardiol. 1999;34:539–544. doi: 10.1016/s0735-1097(99)00228-4. [DOI] [PubMed] [Google Scholar]
- 12.Airan B, Sharma R, Choudhary SK, et al. Univentricular repair: is routine fenestration justified? Ann Thorac Surg. 2000;69:1900–1906. doi: 10.1016/s0003-4975(00)01247-9. [DOI] [PubMed] [Google Scholar]
- 13.du Plessis AJ, Chang AC, Wessel DL, et al. Cerebrovascular accidents following the Fontan operation. Pediatr Neurol. 1995;12:230–236. doi: 10.1016/0887-8994(95)00027-d. [DOI] [PubMed] [Google Scholar]
- 14.Meadows J, Lang P, Marx G, Rhodes J. Fontan fenestration closure has no acute effect on exercise capacity but improves ventilatory response to exercise. J Am Coll Cardiol. 2008;52:108–113. doi: 10.1016/j.jacc.2007.12.063. [DOI] [PubMed] [Google Scholar]
- 15.Sommer RJ, Recto M, Golinko RJ, Griepp RB. Transcatheter coil occlusion of surgical fenestration after Fontan operation. Circulation. 1996;94:249–252. doi: 10.1161/01.cir.94.3.249. [DOI] [PubMed] [Google Scholar]
- 16.Moore JW, Murdison KA, Baffa GM, Kashow K, Murphy JD. Transcatheter closure of fenestrations and excluded hepatic veins after fontan: versatility of the Amplatzer device. Am Heart J. 2000;140:534–540. doi: 10.1067/mhj.2000.108517. [DOI] [PubMed] [Google Scholar]
- 17.Goff DA, Blume ED, Gauvreau K, Mayer JE, Lock JE, Jenkins KJ. Clinical outcome of fenestrated Fontan patients after closure: the first 10 years. Circulation. 2000;102:2094–2099. doi: 10.1161/01.cir.102.17.2094. [DOI] [PubMed] [Google Scholar]
- 18.Ono M, Boethig D, Goerler H, Lange M, Westhoff-Bleck M, Breymann T. Clinical outcome of patients 20 years after Fontan operation--effect of fenestration on late morbidity. Eur J Cardiothorac Surg. 2006;30:923–929. doi: 10.1016/j.ejcts.2006.08.025. [DOI] [PubMed] [Google Scholar]