Abstract
Objective
To determine the comparative effectiveness of common pleural drainage procedures for treatment of pneumonia complicated by parapneumonic effusion (i.e., complicated pneumonia).
Design
Multicenter retrospective cohort study.
Setting
40 children’s hospitals contributing data to the Pediatric Health Information System.
Participants
Children with complicated pneumonia requiring pleural drainage.
Main Exposures
Initial drainage procedures were categorized as chest tube without fibrinolysis, chest tube with fibrinolysis, video-assisted thoracoscopic surgery (VATS), and thoracotomy.
Main Outcome Measures
Length of stay (LOS), additional drainage procedures, readmission within 14 days of discharge, and hospital costs.
Results
Initial procedures among 3,500 patients included chest tube without fibrinolysis (n=1,762), chest tube with fibrinolysis (n=623), VATS (n=408), and thoracotomy (n=797). Median age was 4.1 years. Overall, 716 (20.5%) patients received an additional drainage procedure (range, 6.8%–44.8% across individual hospitals). The median LOS was 10 days (range, 7–14 days across individual hospitals). The median readmission rate was 3.8% (range, 0.8%–33.3%). In multivariable analysis, differences in LOS by initial procedure type were not significant. Patients undergoing initial chest tube placement with or without fibrinolysis were more likely to require additional drainage procedures. However, initial chest tube without fibrinolysis was the least costly strategy.
Conclusion
There is variability in the treatment and outcomes of children with complicated pneumonia. Outcomes were similar in patients undergoing initial chest tube placement with or without fibrinolysis. Those undergoing VATS received fewer additional drainage procedures but had no differences in LOS compared with other strategies.
Keywords: pneumonia, empyema, pleural, empyema, epidemiology, thoracostomy, comparative effectiveness research
INTRODUCTION
Community-acquired pneumonia, the most common serious bacterial infection in childhood, may be complicated by parapneumonic effusion (i.e., complicated pneumonia).1 Children with complicated pneumonia require prolonged hospitalization and frequently undergo multiple pleural fluid drainage procedures.2 Additionally, the incidence of complicated pneumonia has increased,3–7 making the need to define appropriate therapy even more pressing. Defining appropriate therapy is challenging for the individual physician as a result of inconsistent and insufficient evidence, and wide variation in treatment practices.2, 8
Historically, thoracotomy was performed only if initial chest tube placement did not lead to clinical improvement.9, 10 Several authors, noting the rapid resolution of symptoms in children undergoing earlier thoracotomy, advocated for the use of thoracotomy as initial therapy rather than as a procedure of last resort.11–14 The advent of less invasive techniques such as video-assisted thoracoscopic surgery (VATS) has served as an additional impetus to consider surgical drainage as the initial treatment strategy.15–18 Few well-designed studies have examined the relative efficacy of these interventions.2, 19–22 Published randomized trials were single center, enrolled few patients, and arrived at different conclusions.19, 21, 22 In addition, these trials did not examine other important outcomes such as requirement for additional pleural fluid drainage procedures and hospital readmission. Two large retrospective multicenter studies found modest reductions in length of stay (LOS) and substantial decreases in the requirement for additional pleural fluid drainage procedures in children undergoing initial VATS compared with initial chest tube placement.2, 20 However, Shah et al2 included relatively few patients undergoing VATS. Li et al20 combined patients undergoing initial thoracentesis, initial chest tube placement, late pleural fluid drainage (by any method), and no pleural fluid drainage into a single “non-operative management” category, precluding conclusions about the relative benefits of chest tube placement compared with VATS. Neither study2, 20 examined the role of chemical fibrinolysis, a therapy which has been associated with outcomes comparable to VATS in two small randomized trials.21, 22
The objectives of this multicenter study were to describe the variation in the initial management strategy along with associated outcomes of complicated pneumonia in childhood and to determine the comparative effectiveness of different pleural fluid drainage procedures.
METHODS
Data Source
The Pediatric Health Information System (PHIS), which contains resource utilization data from 40 freestanding children’s hospitals, provided data for this multicenter retrospective cohort study. Participating hospitals are located in non-competing markets of 27 states plus the District of Columbia. The PHIS database includes patient demographics, diagnoses, and procedures as well as data for all drugs, radiologic studies, laboratory tests, and supplies charged to each patient. Data are de-identified, however encrypted medical record numbers allow for tracking individual patients across admissions. The Child Health Corporation of America (Shawnee Mission, KS) and participating hospitals jointly assure data quality and reliability as described previously.23, 24 The Children’s Hospital of Philadelphia Institutional Review Board reviewed and approved this study.
Patients
Children ≤18 years of age receiving a pleural drainage procedure for complicated pneumonia were eligible if they were discharged from participating hospitals between January 1, 2004 and June 30, 2009. Study participants met the following criteria: 1) discharge diagnosis of pneumonia (International Classification of Diseases, 9th revision [ICD-9] discharge diagnosis codes 480.x-483.x, 485.x-487.x), 2) discharge diagnosis of pleural effusion (ICD-9 codes 510.0, 510.9, 511.0, 511.1, or 511.9), and 3) billing charge for antibiotics on the first day of hospitalization. Additionally, the primary discharge diagnosis had to be either pneumonia or pleural effusion. Patients were excluded if they did not undergo pleural fluid drainage or if their initial pleural fluid drainage procedure was thoracentesis.
Study Definitions
Pleural drainage procedures were identified using ICD-9 procedure codes for thoracentesis (34.91), chest tube placement (34.04), video-assisted thoracoscopic surgery (VATS; 34.21), and thoracotomy (34.02 or 34.09). Fibrinolysis was defined as receipt of urokinase, streptokinase, or alteplase within two days of initial chest tube placement.
Acute conditions or complications included influenza (487, 487.0, 487.1, 487.8, 488, or V04.81) and hemolytic-uremic syndrome (283.11). Chronic comorbid conditions (CCCs) (e.g., malignancy) were identified using a previously reported classification scheme.25 Billing data were used to classify receipt of mechanical ventilation and medications on the first day of hospitalization.
Measured Outcomes
The primary outcomes were hospital LOS (both overall and post-initial procedure), requirement for additional pleural drainage procedures, total cost for index hospitalization, all-cause readmission within 14 days after index hospital discharge, and total cost of the episode (accounting for the cost of readmissions).
Measured Exposures
The primary exposure of interest was the initial pleural fluid drainage procedure, classified as chest tube placement without fibrinolysis, chest tube placement with fibrinolysis, VATS, or thoracotomy.
Statistical Analysis
Variables were summarized using frequencies and percentages for categorical variables, and median, interquartile range (IQR), and range for continuous variables. Outcomes by initial pleural drainage procedure were compared using Chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables.
Multivariable analysis was performed to account for potential confounding by observed baseline variables. For dichotomous outcome variables, modeling consisted of logistic regression using generalized estimating equations to account for hospital clustering. For continuous variables, a mixed model approach was used, treating hospital as a random effect. Log transformation was applied to the right-skewed outcome variables (LOS and cost). Cost outcomes remained skewed following log transformation, thus gamma mixed models were applied.26–29 Odds ratios and 95% confidence intervals (CIs) were reported for comparison of dichotomous outcomes and the adjusted means and 95% CIs were reported for continuous outcomes after appropriate back transformation.
Additional analyses addressed the potential impact of confounding by indication inherent in any observational study. First, patients with an underlying CCC were excluded to ensure that our results would be generalizable to otherwise healthy children with community-acquired pneumonia. Second, patients undergoing pleural drainage >2 days after hospitalization were excluded to minimize the effect of residual confounding related to differences in timing of the initial drainage procedure. Third, the analysis was repeated using a generalized propensity score as an additional method to account for confounding by indication for the initial drainage procedure.30 Propensity scores, constructed using a multivariable generalized logit model, included all variables listed in Table 1. The inverse of the propensity score was included as a weight in each multivariable model described above. Only the primary multivariable analyses are presented as the results of the propensity score analysis were nearly identical to the primary analyses.
Table 1.
Characteristics of patients with complicated pneumonia requiring pleural fluid drainage, stratified by initial pleural fluid drainage procedure.a
| Overall | Chest Tube without Fibrinolysis | Chest Tube with Fibrinolysis | Thoracotomy | VATS | p | |
|---|---|---|---|---|---|---|
| N | 3500 | 1672 (47.8) | 623 (17.8) | 797 (22.8) | 408 (11.7) | |
| Age | ||||||
| <1 year | 335 (9.6) | 176 (10.5) | 56 (9.0) | 78 (9.8) | 25 (6.1) | |
| 1 year | 475 (13.6) | 238 (14.2) | 98 (15.7) | 92 (11.5) | 47 (11.5) | 0.003 |
| 2–4 years | 1230 (35.1) | 548 (32.8) | 203 (32.6) | 310 (38.9) | 169 (41.4) | |
| 5–9 years | 897 (25.6) | 412 (24.6) | 170 (27.3) | 199 (25.0) | 116 (28.4) | |
| 10–14 years | 324 (9.3) | 167 (10.0) | 61 (9.8) | 65 (8.2) | 31 (7.6) | |
| 15–18 years | 193 (5.5) | 106 (6.3) | 29 (4.6) | 40 (5.0) | 18 (4.4) | |
| >18 years | 46 (1.3) | 25 (1.5) | 6 (0.96) | 13 (1.6) | 2 (0.5) | |
| Comorbid Conditions | ||||||
| Cardiac | 69 (2.0) | 43 (2.6) | 14 (2.3) | 12 (1.5) | 0 (0.0) | 0.006 |
| Malignancy | 81 (2.3) | 31 (1.9) | 18 (2.9) | 21 (2.6) | 11 (2.7) | 0.375 |
| Neurological | 138 (3.9) | 73 (4.4) | 20 (3.2) | 34 (4.3) | 11 (2.7) | 0.313 |
| Any Other Condition | 202 (5.8) | 96 (5.7) | 40 (6.4) | 47 (5.9) | 19 (4.7) | 0.696 |
| Payer | ||||||
| Government | 1240 (35.6) | 630 (37.8) | 224 (36.0) | 259 (32.7) | 127 (31.3) | <0.001 |
| Private | 1383 (39.7) | 607 (36.4) | 283 (45.4) | 310 (39.2) | 183 (45.07) | |
| Other | 864 (24.8) | 430 (25.8) | 116 (18.6) | 222 (28.1) | 96 (23.65) | |
| Race | ||||||
| Non-Hispanic White | 1746 (51.9) | 838 (51.6) | 358 (59.7) | 361 (47.8) | 189 (48.7) | <0.001 |
| Non-Hispanic Black | 601 (17.9) | 318 (19.6) | 90 (15.0) | 128 (17.0) | 65 (16.8) | |
| Hispanic | 588 (17.5) | 280 (17.3) | 73 (12.2) | 155 (20.5) | 80 (20.6) | |
| Asian | 117 (3.5) | 47 (2.9) | 20 (3.3) | 37 (4.9) | 13 (3.4) | |
| Other | 314 (9.3) | 140 (8.6) | 59 (9.8) | 74 (9.8) | 41 (10.6) | |
| Male Sex | 1912 (54.6) | 923 (55.2) | 336 (53.9) | 439 (55.1) | 214 (52.5) | 0.755 |
| Radiology | ||||||
| CT, no US | 1200 (34.3) | 600 (35.9) | 184 (29.5) | 280 (35.1) | 136 (33.3) | <0.001 |
| CT and US | 221 (6.3) | 84 (5.0) | 53 (8.5) | 61 (7.7) | 23 (5.6) | |
| US, no CT | 799 (22.8) | 324 (19.4) | 178 (28.6) | 200 (25.1) | 97 (23.8) | |
| No US, no CT | 1280 (36.6) | 664 (39.7) | 208 (33.4) | 256 (32.1) | 152 (37.3) | |
| Empiric Antibiotic Regimen | ||||||
| Cephalosporins alone | 448 (12.8) | 181 (10.83) | 126 (20.2) | 73 (9.2) | 68 (16.7) | <0.001 |
| Cephalosporin and clindamycin | 797 (22.8) | 359 (21.5) | 145 (23.3) | 184 (23.1) | 109 (26.7) | |
| Other antibiotic combination | 167 (4.8) | 82 (4.9) | 30 (4.8) | 38 (4.8) | 17 (4.2) | |
| Cephalosporin and vancomyin | 2088 (59.7) | 1050 (62.8) | 322 (51.7) | 502 (63.0) | 214 (52.5) | |
| Mechanical ventilation | 494 (14.1) | 251 (15.0) | 75 (12.0) | 114 (14.3) | 54 (13.2) | 0.307 |
| Corticosteroids | 520 (14.9) | 291 (17.4) | 72 (11.6) | 114 (14.3) | 43 (10.5) | <0.001 |
| Blood product transfusionsb | 761 (21.7) | 387 (23.2) | 145 (23.3) | 161 (20.2) | 68 (16.7) | 0.018 |
| Vasoactive infusionsc | 381 (10.9) | 223 (13.3) | 63 (10.1) | 72 (9.0) | 23 (5.6) | <0.001 |
| Admission to intensive care | 1397 (39.9) | 731 (43.7) | 234 (37.6) | 296 (37.1) | 136 (33.3) | <0.001 |
| Extracorporeal membranous oxygenation | 18 (0.5) | 13 (0.8) | 2 (0.3) | 3 (0.4) | 0 (0.0) | 0.163 |
| Hemolytic-uremic syndrome | 31 (0.9) | 15 (0.9) | 6 (1.0) | 7 (0.9) | 3 (0.7) | 0.985 |
| Influenza | 108 (3.1) | 53 (3.2) | 27 (4.3) | 23 (2.9) | 5 (1.2) | 0.044 |
| Arterial blood gas measurements | 0 (0,1) | 0 (0, 2) | 0 (0,1) | 0 (0, 1) | 0 (0, 1) | <0.001 |
| Days to first procedure | 1 (0, 3) | 1 (0, 2) | 1 (1, 3) | 1 (1, 3) | 1 (1, 3) | <0.001 |
Abbreviations: CT, computed tomography; US, ultrasound
Values listed as number (percent) or median (interquartile range)
Blood product transfusions included administration of packed red blood cells, cryoprecipitate, fresh frozen plasma, or platelets.
Vasoactive infusions included dobutamine, dopamine, epinephrine, norepinephrine, vasopressin, and milrinone.
Medical records of a randomly selected subset of subjects from 6 hospitals were reviewed to determine the accuracy of our algorithm in identifying patients with complicated pneumonia; these subjects represented ~1% of the study population. For the purposes of medical record review, complicated pneumonia was defined by the following: 1) radiologically-confirmed lung infiltrate; 2) moderate or large pleural effusion; and 3) signs and symptoms of lower respiratory tract infection. Complicated pneumonia was identified in 118 of 120 reviewed subjects for a positive predictive value of 98.3%.
All analyses were clustered by hospital. Analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC). A two-tailed P<0.05 was considered statistically significant.
RESULTS
Patient Characteristics
During the study period, 9,680 subjects had complicated pneumonia. Subjects were excluded if they did not have a pleural drainage procedure (n=5,798), or if thoracentesis was the first pleural fluid drainage procedure performed (n=382). The remaining 3,500 patients were included. Demographic characteristics are summarized in Table 1. The median patient age was 4.1 years (IQR: 2.1–7.2 years). An underlying CCC was present in 424 (12.1%) patients. There was no association between type of drainage procedure and mechanical ventilation. However, factors associated with more severe systemic illness, such as blood product transfusion, were more common among those undergoing initial chest tube placement with or without fibrinolysis (Table 1).
Initial Pleural Fluid Drainage Procedures
The primary procedures included chest tube without fibrinolysis (47.8%); chest tube with fibrinolysis (17.8%); thoracotomy (22.8%); and VATS (11.7%) (Table 1). The proportion of patients undergoing primary chest tube placement with fibrinolysis increased over time from 14.2% in 2004 to 30.0% in 2009 (P<0.001; chi-square test for trend). The initial procedure varied by hospital with the greatest proportion of patients undergoing primary chest tube placement without fibrinolysis at 28 (70.0%) hospitals, chest tube placement with fibrinolysis at 5 (12.5%) hospitals, thoracotomy at 5 (12.5%) hospitals, and VATS at 2 (5.0%) hospitals (Figure 1). The median proportion of patients undergoing primary VATS across all hospitals was 11.5% (IQR: 3.9%–26.5%) (Figure 1). The median time to first procedure was 1 day (IQR: 0–3 days).
Figure 1.
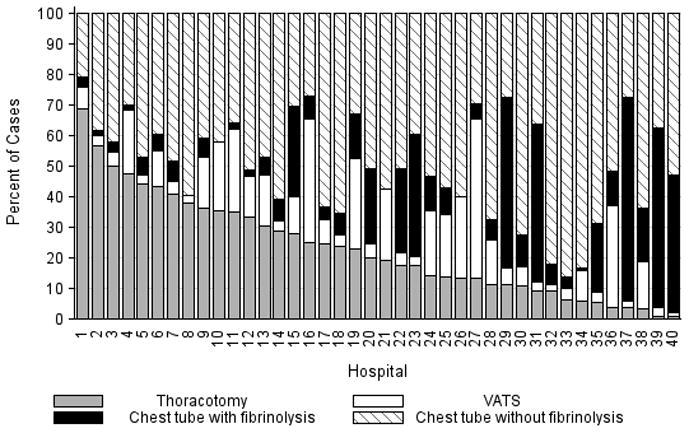
Distribution of initial procedure type by hospital. The y-axis shows the percentage of patients undergoing specific pleural fluid drainage procedures. Each number on the x-axis represents data from one hospital.
Outcome Measures
Variation in outcomes occurred across hospitals. Additional pleural drainage procedures were performed in a median of 20.9% of patients with a range of 6.8% to 44.8% (IQR: 14.5%–25.3%) of patients across all hospitals. Median LOS was 10 days with a range of 7 to 14 days (IQR: 8.5–11 days) and the median LOS following the initial pleural fluid drainage procedure was 8 days with a range of 6 to 13 days (IQR: 7–8 days). Variation in timing of the initial pleural fluid drainage procedure explained 9.6% of the variability in LOS (Spearman rho, 0.31; p<0.001).
Overall, 118 (3.4%) patients were readmitted within 14 days of index discharge; the median readmission rate was 3.8% with a range of 0.8% to 33.3% (IQR: 2.1%–5.8%) across hospitals. The median total cost of the index hospitalization was $19,574 (IQR: $13,791-$31,063). The total cost for the index hospitalization exceeded $54,215 for 10% of patients and the total cost of the episode exceeded $55,208 for 10% of patients. Unadjusted outcomes, stratified by primary pleural fluid drainage procedure, are summarized in Table 2.
Table 2.
Unadjusted outcomes of patients with complicated pneumonia undergoing pleural fluid drainage, stratified by initial pleural fluid drainage procedure.a
| Overall | Chest Tube without Fibrinolysis | Chest Tube with Fibrinolysis | Thoracotomy | VATS | P-valueb | |
|---|---|---|---|---|---|---|
| Additional Procedure | 716 (20.5) | 331 (19.8) | 144 (23.1) | 197 (24.7) | 44 (10.8) | <0.001 |
| Readmission within 14 days | 118 (3.4) | 54 (3.3) | 13 (2.1) | 32 (4.0) | 19 (4.7) | 0.096 |
| Total LOS (days) | 10 (7, 14) | 10 (7, 14) | 9 (7, 13) | 10 (7, 14) | 9 (7, 12) | <.001 |
| Post-initial Procedure LOS (days) | 8 (5, 12) | 8 (6, 12) | 7 (5, 10) | 8 (5,12) | 7 (5,10) | <0.001 |
| Total Cost, Index Hospitalization ($)e | 19319 (13358, 30955) | 19951 (13576, 32018)c | 19565 (13209, 32778)d | 20352 (14351, 31343) | 17918 (13531, 25166) | 0.016 |
| Total Cost, Episode of Illness ($)e | 19831 (13927, 31749) | 20151 (13764, 32653) | 19593 (13210, 32861) | 20573 (14419, 31753) | 18344 (13835, 25462) | 0.029 |
Values listed as number (percent) or median (interquartile range); P<.05 considered statistically significant
Chi-square test for categorical variables and Kruskal-Wallis test for continuous variables
P=0.008 compared with VATS (pairwise comparison)
P=0.057 compared with VATS (pairwise comparison)
Hospital charges were adjusted for hospital location using the Centers for Medicare and Medicaid price/wage index and converted to costs using hospital-level cost-to-charge ratios.
Abbreviations: VATS, video-assisted thoracoscopic surgery
In multivariable analysis, differences in total LOS and post-procedure LOS were not significant (Table 3). The odds of additional drainage procedures were higher for all drainage procedures compared with initial VATS (Table 3). Patients undergoing initial chest tube placement with fibrinolysis were less likely to require readmission compared with patients undergoing initial VATS (Table 3). The total cost for the episode of illness (including the cost of readmission) was significantly less for those undergoing primary chest tube placement without fibrinolysis compared with primary VATS. The results of subanalyses excluding patients with an underlying CCC (Appendix, Table 4) and restricting the cohort to patients undergoing pleural drainage within two days of admission (Appendix, Table 5) were similar to the results of our primary analysis with one exception; in the latter subanalysis, children undergoing initial chest tube placement without fibrinolysis were also less likely to require readmission compared with patients undergoing initial VATS.
Table 3.
Multivariable analysis of the association between initial pleural fluid drainage procedure and outcomes for children with complicated pneumonia.
| Adjusted OR (95% CI)a | P-value | |
|---|---|---|
| Additional Pleural Drainage Procedure | ||
| Chest tube without fibrinolysis | 1.82 (1.10–3.00) | 0.019 |
| Chest tube with fibrinolysis | 2.31 (1.44–3.72) | <0.001 |
| Thoracotomy | 2.59 (1.62–4.14) | <0.001 |
| VATS | Reference | … |
| Readmission within 14 days | ||
| Chest tube without fibrinolysis | 0.61 (0.36–1.05) | 0.077 |
| Chest tube with fibrinolysis | 0.45 (0.23–0.86) | 0.015 |
| Thoracotomy | 0.85 (0.52–1.39) | 0.521 |
| VATS | Reference | … |
| Adjusted Mean (95% CI)a | P-value | |
| Total LOS (days) | ||
| Chest tube without fibrinolysis | 8.0 (7.8–8.2) | 0.339 |
| Chest tube with fibrinolysis | 8.1 (7.9–8.3) | 0.812 |
| Thoracotomy | 8.1 (7.9–8.3) | 0.632 |
| VATS | 8.1 (7.9–8.3) | Ref |
| Post-Initial Procedure LOS (days) | ||
| Chest tube without fibrinolysis | 7.3 (7.0–7.5) | 0.512 |
| Chest tube with fibrinolysis | 7.5 (7.2–7.8) | 0.239 |
| Thoracotomy | 7.3 (7.0–7.6) | 0.841 |
| VATS | 7.3 (7.1–7.6) | Reference |
| Total Cost, Index Hospitalization ($) | ||
| Chest tube without fibrinolysis | 22928 (22000–23895 | 0.012 |
| Chest tube with fibrinolysis | 23621 (22631–24655) | 0.657 |
| Thoracotomy | 23386 (22419–24395 | 0.262 |
| VATS | 23820 (22808–24878) | Reference |
| Total Cost, Episode of Illness ($) | ||
| Chest tube without fibrinolysis | 23218 (22278–24199) | 0.004 |
| Chest tube with fibrinolysis | 23749 (22752–24790) | 0.253 |
| Thoracotomy | 23673 (22693–24696) | 0.131 |
| VATS | 24280 (23244–25362) | Reference |
All models adjusted for age, sex, race, month of admission, primary payer, radiologic imaging performed, empiric antibiotic therapy, concurrent diagnosis of influenza or hemolytic uremic syndrome, presence of underlying chronic comorbid conditions, timing of primary pleural fluid drainage procedure, and receipt of corticosteroids and requirement for mechanical ventilation, blood product transfusions, vasoactive infusions, intensive care unit hospitalization, extracorporeal membranous oxygenation, and arterial blood gas measurements within the first two days of hospitalization and clustered on hospital.
Abbreviations: OR, odds ratio; VATS, video-assisted thoracoscopic surgery
DISCUSSION
This multicenter study is the largest to evaluate the management of children hospitalized with complicated pneumonia. We found considerable variation in initial management and outcomes across hospitals. Differences in timing of the initial drainage procedure explained only a small amount of the variability in outcomes. Children undergoing initial VATS less commonly required additional drainage procedures while children undergoing initial chest tube placement with fibrinolysis less commonly required readmission. Differences in total and post-procedure LOS were not statistically significant. Differences in cost, while statistically significant, were of marginal relevance.
Previous studies have also shown significant variation in treatment and outcomes of children with complicated pneumonia across hospitals.2, 8 Our study provides data from additional hospitals, includes a substantially larger number of patients undergoing initial VATS, distinguishes between fibrinolysis recipients and non-recipients, and is the first to compare outcomes between four different initial drainage strategies. The creation of national consensus guidelines might reduce variability in initial management strategies, although the variability in outcomes across hospitals in the current study could not be explained simply by differences in the type or timing of the initial drainage procedure. Thus, future studies examining hospital-level factors may play an important role in improving quality of care for children with complicated pneumonia.
Patients with initial thoracotomy or chest tube placement with or without fibrinolysis more commonly received additional drainage procedures than patients with initial VATS. This difference remained when patients with CCCs were excluded from the analysis and when the analysis was limited to patients undergoing pleural fluid drainage within 2 days of hospitalization. Several small, randomized trials demonstrated conflicting results when comparing initial chest tube placement with fibrinolysis and VATS. St. Peter et al22 reported that 3 (17%) of 18 patients undergoing initial chest tube placement with fibrinolysis and none of the 18 patients undergoing initial VATS received additional pleural drainage procedures. Sonnappa et al21 found no differences between the two groups. Kurt et al19 did not state the proportion of patients receiving additional procedures. However, the mean number of drainage procedures was 2.25 among the 8 patients undergoing initial chest tube placement while none of the 10 patients with VATS received additional drainage.19
Thoracotomy is often perceived as a “definitive” procedure for treatment of complicated pneumonia. However, several possibilities exist to explain why additional procedures were performed less frequently in patients undergoing initial VATS compared with initial thoracotomy. The limited visual field in thoracotomy may lead to greater residual disease postoperatively in those receiving thoracotomy compared with VATS.31 Additionally, thoracotomy substantially disrupts the integrity of the chest wall and is consequently associated with complications such as bleeding and air leak into the pleural cavity more often than VATS.31, 32 It is thus possible that some of the additional procedures in patients receiving initial thoracotomy were necessary for management of thoracotomy-associated complications rather than for failure of the initial drainage procedure.
Similar to the randomized trials by Sonnappa et al21 and St. Peter et al,22 differences in the overall and post-procedure LOS were not significant among patients undergoing initial VATS compared with initial chest tube placement with fibrinolysis. However, chest tube placement without fibrinolysis did not result in significant differences in LOS compared with initial VATS. In the only pediatric randomized trial, the 29 intrapleural urokinase recipients had a 2 day shorter LOS compared with the 29 intrapleural saline recipients.33 Several small, randomized controlled trials of adults with complicated pneumonia reported improved pleural fluid drainage among intrapleural fibrinolysis recipients compared with non-recipients.34–36 However, a large multicenter randomized trial in adults found no differences in mortality, requirement for surgical drainage, or LOS between intrapleural streptokinase and placebo recipients.37 Subsequent meta-analyses of randomized trials in adults also demonstrated no benefit to fibrinolysis.38, 39 In the context of the increasing use of intrapleural fibrinolysis in children with complicated pneumonia, our results highlight the need for a large, multicenter randomized controlled trial to determine whether chest tube with fibrinolysis is superior to chest tube alone.
Two small randomized trials21, 22 and a decision analysis40 identified chest tube with fibrinolysis as the most economical approach to children with complicated pneumonia. However, the costs did not differ significantly between patients undergoing initial VATS or initial chest tube placement with fibrinolysis in our study. The least costly approach was initial chest tube placement without fibrinolysis. Unlike the randomized controlled trials, we considered costs associated with readmissions in determining the total costs. Shah et al41 found no difference in total charges for patients undergoing initial VATS compared with initial chest tube placement; however, patients undergoing initial VATS were concentrated in a few centers, making it difficult to determine the relative importance of procedural and hospital factors.
This multicenter observational study has several limitations. First, discharge diagnosis coding may be unreliable for specific diseases. However, our rigorous definition of complicated pneumonia, supported by the high positive predictive value as verified by medical record review, minimizes the likelihood of misclassification.
Second, unmeasured confounding or residual confounding by indication for the method of pleural drainage may occur, potentially influencing our results in two disparate ways. If patients with more severe systemic illness were too unstable for operative interventions, then our results would be biased towards worse outcomes for children undergoing initial chest tube placement. We adjusted for several variables associated with a greater systemic severity of illness, including intensive care unit admission, making this possibility less likely. We also could not account for some factors associated with more severe local disease such as the size and character of the effusion. We suspect that patients with more extensive local disease (i.e., loculated effusions) would have worse outcomes than other patients, regardless of initial procedure, and that these patients would also be more likely to undergo primary surgical drainage. Thus, this study may have underestimated the benefit of initial surgical drainage (e.g., VATS) compared with non-surgical drainage (i.e., chest tube placement).
Third, misclassification of the method of initial pleural drainage may have occurred. Patients transferred from another institution following chest tube placement could either be classified as not receiving pleural drainage and thus excluded from the study or classified as having initial VATS or thoracotomy if the reason for transfer was chest tube treatment failure. Additionally, we could not distinguish routine use of fibrinolysis from fibrinolysis to maintain chest tube patency. Whether such misclassification would falsely minimize or maximize differences in outcomes between the various groups remains uncertain. Fourth, because this study only included tertiary care children’s hospitals, these data are not generalizable to community settings. VATS requires specialized surgical training that may be unavailable in some areas. Finally, this study demonstrates the relative efficacy of various pleural fluid drainage procedures on short-term clinical outcomes and resource utilization. However, long-term functional outcomes should be measured in future prospective studies.
In conclusion, emphasis on evidence driven treatment to optimize care has led to an increasing examination of unwarranted practice variation.42 The lack of evidence for best practice makes it difficult to define ‘unwarranted’ variation in the treatment of complicated pneumonia. Our study demonstrates the large variability in practice and raises additional questions regarding the optimal drainage strategies. Published randomized trials have focused on comparisons between chest tube placement with fibrinolysis and VATS. However, our data suggest that future randomized trials should include chest tube placement without fibrinolysis as a treatment strategy. In determining the current best treatment for patients with complicated pneumonia, a clinician must weigh the impact of needing an additional procedure in approximately one-quarter of patients undergoing initial chest tube placement (with or without fibrinolysis) with the risks of general anesthesia and readmission in patients undergoing initial VATS.
Acknowledgments
Dr. Hall had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the analysis.
Sources of funding: Dr. Shah received support from the National Institute of Allergy and Infectious Diseases (K01 AI73729) and the Robert Wood Johnson Foundation under its Physician Faculty Scholar program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ABBREVIATIONS USED IN THE MANUSCRIPT
- CCC
Chronic comorbid condition
- CI
Confidence interval
- ICD-9
International classification of diseases, 9th revision
- IQR
Interquartile range
- LOS
Length of stay
- VATS
Video-assisted thoracoscopic surgery
Appendix
Table 4.
Multivariable analysis of the association between initial pleural fluid drainage procedure and outcomes for children with complicated pneumonia while excluding those with underlying chronic comorbid conditions.
| Adjusted OR (95% CI)a | P-value | |
|---|---|---|
| Additional Pleural Drainage Procedure | ||
| Chest tube without fibrinolysis | 1.80 (1.05–3.10) | 0.033 |
| Chest tube with fibrinolysis | 2.29 (1.43–3.68) | <0.001 |
| Thoracotomy | 2.74 (1.72–4.37) | <0.001 |
| VATS | Reference | … |
| Readmission within 14 days | ||
| Chest tube without fibrinolysis | 0.60 (0.33–1.06) | 0.080 |
| Chest tube with fibrinolysis | 0.35 (0.15–0.82) | 0.016 |
| Thoracotomy | 0.72 (0.43–1.22) | 0.220 |
| VATS | Reference | … |
| Adjusted Mean (95% CI)a | P-value | |
| Total LOS (days) | ||
| Chest tube without fibrinolysis | 7.7 (7.6, 7.9) | 0.321 |
| Chest tube with fibrinolysis | 7.8 (7.6, 8) | 0.879 |
| Thoracotomy | 7.7 (7.5, 7.9) | 0.346 |
| VATS | 7.8 (7.6, 8) | Reference |
| Post-Initial Procedure LOS (days) | ||
| Chest tube without fibrinolysis | 6.7 (6.5, 6.9) | 0.496 |
| Chest tube with fibrinolysis | 6.9 (6.6, 7.1) | 0.377 |
| Thoracotomy | 6.7 (6.5, 6.9) | 0.632 |
| VATS | 6.7 (6.5, 7) | Reference |
| Total Cost, Index Hospitalization ($) | ||
| Chest tube without fibrinolysis | 20282 (19454, 21146) | 0.010 |
| Chest tube with fibrinolysis | 21021 (20125, 21958) | 0.790 |
| Thoracotomy | 20889 (20018, 21799) | 0.503 |
| VATS | 21133 (20224, 22084 | Reference |
| Total Cost, Episode of Illness ($) | ||
| Chest tube without fibrinolysis | 20423 (19587–21294) | 0.004 |
| Chest tube with fibrinolysis | 21188 (20282–22135) | 0.316 |
| Thoracotomy | 21007 (20128–21924) | 0.277 |
| VATS | 21414 (20488–22382) | Reference |
All models adjusted for age, sex, race, month of admission, primary payer, radiologic imaging performed, empiric antibiotic therapy, concurrent diagnosis of influenza or hemolytic uremic syndrome, timing of primary pleural fluid drainage procedure, and receipt of corticosteroids and requirement for mechanical ventilation, blood product transfusions, vasoactive infusions, intensive care unit hospitalization, extracorporeal membranous oxygenation, and arterial blood gas measurements within the first two days of hospitalization and clustered on hospital.
Abbreviations: OR, odds ratio; VATS, video-assisted thoracoscopic surgery
Table 5.
Multivariable analysis of the association between initial pleural fluid drainage procedure and outcomes for children with complicated pneumonia while excluding those with an initial pleural fluid drainage procedure more than 2 days after admission.
| Adjusted OR (95% CI)a | P-value | |
|---|---|---|
| Additional Pleural Drainage Procedure | ||
| Chest tube without fibrinolysis | 2.08 (1.19–3.63) | 0.010 |
| Chest tube with fibrinolysis | 2.45 (1.50–4.00) | <0.001 |
| Thoracotomy | 3.18 (2.06–4.90) | <0.001 |
| VATS | Reference | … |
| Readmission within 14 days | ||
| Chest tube without fibrinolysis | 0.51 (0.29–0.91) | 0.003 |
| Chest tube with fibrinolysis | 0.26 (0.11–0.63) | 0.021 |
| Thoracotomy | 0.54 (0.31–0.92) | 0.023 |
| VATS | Reference | … |
| Adjusted Mean (95% CI)a | P-value | |
| Total LOS (days) | ||
| Chest tube without fibrinolysis | 7.4 (7.0, 7.9) | 0.168 |
| Chest tube with fibrinolysis | 7.5 (7.0, 7.9) | 0.750 |
| Thoracotomy | 7.5 (7.1, 8.0) | 0.566 |
| VATS | 7.6 (7.1, 8.1) | Reference |
| Post-Initial Procedure LOS (days) | ||
| Chest tube without fibrinolysis | 7.4 (6.9, 7.9) | 0.140 |
| Chest tube with fibrinolysis | 7.5 (7.0, 8.1) | 0.977 |
| Thoracotomy | 7.5 (7.0, 8.0) | 0.717 |
| VATS | 7.5 (7.0, 8.1) | Reference |
| Total Cost, Index Hospitalization ($) | ||
| Chest tube without fibrinolysis | 22695 (20543, 25072 | 0.049 |
| Chest tube with fibrinolysis | 23633 (21317, 26201 | 0.865 |
| Thoracotomy | 23487 (21210, 26009 | 0.909 |
| VATS | 23539 (21193, 26145 | Reference |
| Total Cost, Episode of Illness ($) | ||
| Chest tube without fibrinolysis | 23089 (20881, 25530 | 0.014 |
| Chest tube with fibrinolysis | 23818 (21464, 26431 | 0.504 |
| Thoracotomy | 23859 (21524, 26446 | 0.485 |
| VATS | 24202 (21763, 26915 | Reference |
All models adjusted for age, sex, race, month of admission, primary payer, radiologic imaging performed, empiric antibiotic therapy, concurrent diagnosis of influenza or hemolytic uremic syndrome, timing of primary pleural fluid drainage procedure, and receipt of corticosteroids and requirement for mechanical ventilation, blood product transfusions, vasoactive infusions, intensive care unit hospitalization, extracorporeal membranous oxygenation, and arterial blood gas measurements within the first two days of hospitalization and clustered on hospital.
Abbreviations: OR, odds ratio; VATS, video-assisted thoracoscopic surgery
Footnotes
Conflicts of Interest: None
Contributor Information
Samir S. Shah, Division of Infectious Diseases, The Children’s Hospital of Philadelphia and the Departments of Pediatrics and Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia, PA.
Matthew Hall, Child Health Corporation of America, Shawnee Mission, KS.
Jason G. Newland, Section of Infectious Diseases, Children’s Mercy Hospital and Clinics, University of Missouri-Kansas City, MO.
Thomas V. Brogan, Division of Critical Care, Seattle Children’s Hospital and the Department of Pediatrics, University of Washington School of Medicine, Seattle, WA.
Reid W. D. Farris, Division of Critical Care, Seattle Children’s Hospital and the Department of Pediatrics, University of Washington School of Medicine, Seattle, WA.
Derek J. Williams, Department of Pediatrics, Division of General Pediatrics, Vanderbilt University School of Medicine and the Monroe Carell, Jr. Children’s Hospital at Vanderbilt, Nashville, TN.
Gitte Larsen, Division of Pediatric Critical Care, Primary Children’s Medical Center, and the Department of Pediatrics, University of Utah, Salt Lake City, UT.
Bryan R. Fine, Division of Pediatric Hospital Medicine, Children’s Hospital of The King’s Daughters and the Department of Pediatrics, Eastern Virginia Medical School, Norfolk, VA.
James E. Levin, Department of Pediatrics, Children’s Hospital of Pittsburgh of UPMC, University of Pittsburgh Medical Center, Pittsburgh, PA.
Jeffrey S. Wagener, Section of Pulmonary Medicine, Department of Pediatrics, University of Colorado School of Medicine and The Children’s Hospital, Aurora, CO.
Patrick H. Conway, Division of General Pediatrics and Division of Health Policy and Clinical Effectiveness, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
Angela L. Myers, Section of Infectious Diseases, Children’s Mercy Hospital and Clinics, University of Missouri-Kansas City, MO.
References
- 1.Chonmaitree T, Powell KR. Parapneumonic pleural effusion and empyema in children. Review of a 19-year experience, 1962–1980. Clin Pediatr (Phila) 1983;22:414–9. doi: 10.1177/000992288302200603. [DOI] [PubMed] [Google Scholar]
- 2.Shah SS, DiCristina CM, Bell LM, Ten Have T, Metlay JP. Primary early thoracoscopy and reduction in length of hospital stay and additional procedures among children with complicated pneumonia: results of a multicenter retrospective cohort study. Arch Pediatr Adolesc Med. 2008;162:675–81. doi: 10.1001/archpedi.162.7.675. [DOI] [PubMed] [Google Scholar]
- 3.Li ST, Tancredi DJ. Empyema hospitalizations increased in US children despite pneumococcal conjugate vaccine. Pediatrics. 2010;125:26–33. doi: 10.1542/peds.2009-0184. [DOI] [PubMed] [Google Scholar]
- 4.Byington CL, Korgenski K, Daly J, Ampofo K, Pavia A, Mason EO. Impact of the pneumococcal conjugate vaccine on pneumococcal parapneumonic empyema. Pediatr Infect Dis J. 2006;25:250–4. doi: 10.1097/01.inf.0000202137.37642.ab. [DOI] [PubMed] [Google Scholar]
- 5.Hendrickson DJ, Blumberg DA, Joad JP, Jhawar S, McDonald RJ. Five-fold increase in pediatric parapneumonic empyema since introduction of pneumococcal conjugate vaccine. Pediatric Infectious Disease Journal. 2008;27:1030–32. doi: 10.1097/INF.0b013e31817e5188. [DOI] [PubMed] [Google Scholar]
- 6.Grijalva CG, Nuorti JP, Zhu Y, Griffin MR. Increasing incidence of empyema complicating childhood community-acquired pneumonia in the United States. Clin Infect Dis. 2010;50:805–13. doi: 10.1086/650573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee GE, Lorch SA, Sheffler-Collins S, Kronman MP, Shah SS. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126:204–13. doi: 10.1542/peds.2009-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langley JM, Kellner JD, Solomon N, et al. Empyema associated with community-acquired pneumonia: a Pediatric Investigator’s Collaborative Network on Infections in Canada (PICNIC) study. BMC Infect Dis. 2008;8:129. doi: 10.1186/1471-2334-8-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stiles QR, Lindesmith GG, Tucker BL, Meyer BW, Jones JC. Pleural empyema in children. Ann Thorac Surg. 1970;10:37–44. doi: 10.1016/s0003-4975(10)65563-4. [DOI] [PubMed] [Google Scholar]
- 10.Thomas DF, Glass JL, Baisch BF. Management of streptococcal empyema. Ann Thorac Surg. 1966;2:658–64. doi: 10.1016/s0003-4975(10)66636-2. [DOI] [PubMed] [Google Scholar]
- 11.Kern JA, Rodgers BM. Thoracoscopy in the management of empyema in children. J Pediatr Surg. 1993;28:1128–32. doi: 10.1016/0022-3468(93)90146-c. [DOI] [PubMed] [Google Scholar]
- 12.Khakoo GA, Goldstraw P, Hansell DM, Bush A. Surgical treatment of parapneumonic empyema. Pediatr Pulmonol. 1996;22:348–56. doi: 10.1002/(SICI)1099-0496(199612)22:6<348::AID-PPUL3>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 13.Kosloske AM, Cartwright KC. The controversial role of decortication in the management of pediatric empyema. J Thorac Cardiovasc Surg. 1988;96:166–70. [PubMed] [Google Scholar]
- 14.Rizalar R, Somuncu S, Bernay F, Ariturk E, Gunaydin M, Gurses N. Postpneumonic empyema in children treated by early decortication. Eur J Pediatr Surg. 1997;7:135–7. doi: 10.1055/s-2008-1071073. [DOI] [PubMed] [Google Scholar]
- 15.Gandhi RR, Stringel G. Video-assisted thoracoscopic surgery in the management of pediatric empyema. JSLS. 1997;1:251–3. [PMC free article] [PubMed] [Google Scholar]
- 16.Grewal H, Jackson RJ, Wagner CW, Smith SD. Early video-assisted thoracic surgery in the management of empyema. Pediatrics. 1999;103:e63. doi: 10.1542/peds.103.5.e63. [DOI] [PubMed] [Google Scholar]
- 17.Merry CM, Bufo AJ, Shah RS, Schropp KP, Lobe TE. Early definitive intervention by thoracoscopy in pediatric empyema. J Pediatr Surg. 1999;34:178–80. doi: 10.1016/s0022-3468(99)90252-x. discussion 80–1. [DOI] [PubMed] [Google Scholar]
- 18.Stovroff M, Teague G, Heiss KF, Parker P, Ricketts RR. Thoracoscopy in the management of pediatric empyema. J Pediatr Surg. 1995;30:1211–5. doi: 10.1016/0022-3468(95)90025-x. [DOI] [PubMed] [Google Scholar]
- 19.Kurt BA, Winterhalter KM, Connors RH, Betz BW, Winters JW. Therapy of parapneumonic effusions in children: video-assisted thoracoscopic surgery versus conventional thoracostomy drainage. Pediatrics. 2006;118:e547–53. doi: 10.1542/peds.2005-2719. [DOI] [PubMed] [Google Scholar]
- 20.Li ST, Gates RL. Primary operative management for pediatric empyema: decreases in hospital length of stay and charges in a national sample. Arch Pediatr Adolesc Med. 2008;162:44–8. doi: 10.1001/archpediatrics.2007.10. [DOI] [PubMed] [Google Scholar]
- 21.Sonnappa S, Cohen G, Owens CM, et al. Comparison of urokinase and video-assisted thoracoscopic surgery for treatment of childhood empyema. Am J Respir Crit Care Med. 2006;174:221–7. doi: 10.1164/rccm.200601-027OC. [DOI] [PubMed] [Google Scholar]
- 22.St Peter SD, Tsao K, Spilde TL, et al. Thoracoscopic decortication vs tube thoracostomy with fibrinolysis for empyema in children: a prospective, randomized trial. J Pediatr Surg. 2009;44:106–11. doi: 10.1016/j.jpedsurg.2008.10.018. discussion 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008;299:2048–55. doi: 10.1001/jama.299.17.2048. [DOI] [PubMed] [Google Scholar]
- 24.Shah SS, Hall M, Srivastava R, Subramony A, Levin JE. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009;49:1369–76. doi: 10.1086/606048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107:E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 26.Barber J, Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy. 2004;9:197–204. doi: 10.1258/1355819042250249. [DOI] [PubMed] [Google Scholar]
- 27.Lee AH, Gracey M, Wang K, Yau KK. A robustified modeling approach to analyze pediatric length of stay. Ann Epidemiol. 2005;15:673–7. doi: 10.1016/j.annepidem.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 28.Mulla ZD, Gibbs SG, Aronoff DM. Correlates of length of stay, cost of care, and mortality among patients hospitalized for necrotizing fasciitis. Epidemiol Infect. 2007;135:868–76. doi: 10.1017/S0950268806007448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu EQ, Birnbaum HG, Zhang HF, Ivanova JI, Yang E, Mallet D. Health care costs of adults treated for attention-deficit/hyperactivity disorder who received alternative drug therapies. J Manag Care Pharm. 2007;13:561–9. doi: 10.18553/jmcp.2007.13.7.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imbens GW. The role of the propensity score in estimating dose-response functions. Biometrika. 2000;87:706–10. [Google Scholar]
- 31.Subramaniam R, Joseph VT, Tan GM, Goh A, Chay OM. Experience with video-assisted thoracoscopic surgery in the management of complicated pneumonia in children. J Pediatr Surg. 2001;36:316–9. doi: 10.1053/jpsu.2001.20705. [DOI] [PubMed] [Google Scholar]
- 32.Angelillo Mackinlay TA, Lyons GA, Chimondeguy DJ, Piedras MA, Angaramo G, Emery J. VATS debridement versus thoracotomy in the treatment of loculated postpneumonia empyema. Ann Thorac Surg. 1996;61:1626–30. doi: 10.1016/0003-4975(96)00194-4. [DOI] [PubMed] [Google Scholar]
- 33.Thomson AH, Hull J, Kumar MR, Wallis C, Balfour Lynn IM. Randomised trial of intrapleural urokinase in the treatment of childhood empyema. Thorax. 2002;57:343–7. doi: 10.1136/thorax.57.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bouros D, Schiza S, Tzanakis N, Chalkiadakis G, Drositis J, Siafakas N. Intrapleural urokinase versus normal saline in the treatment of complicated parapneumonic effusions and empyema. A randomized, double-blind study. Am J Respir Crit Care Med. 1999;159:37–42. doi: 10.1164/ajrccm.159.1.9803094. [DOI] [PubMed] [Google Scholar]
- 35.Davies RJ, Traill ZC, Gleeson FV. Randomised controlled trial of intrapleural streptokinase in community acquired pleural infection. Thorax. 1997;52:416–21. doi: 10.1136/thx.52.5.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diacon AH, Theron J, Schuurmans MM, Van de Wal BW, Bolliger CT. Intrapleural streptokinase for empyema and complicated parapneumonic effusions. Am J Respir Crit Care Med. 2004;170:49–53. doi: 10.1164/rccm.200312-1740OC. [DOI] [PubMed] [Google Scholar]
- 37.Maskell NA, Davies CW, Nunn AJ, et al. U.K. Controlled trial of intrapleural streptokinase for pleural infection. N Engl J Med. 2005;352:865–74. doi: 10.1056/NEJMoa042473. [DOI] [PubMed] [Google Scholar]
- 38.Cameron R, Davies HR. Intra-pleural fibrinolytic therapy versus conservative management in the treatment of adult parapneumonic effusions and empyema. Cochrane Database Syst Rev. 2008:CD002312. doi: 10.1002/14651858.CD002312.pub3. [DOI] [PubMed] [Google Scholar]
- 39.Tokuda Y, Matsushima D, Stein GH, Miyagi S. Intrapleural fibrinolytic agents for empyema and complicated parapneumonic effusions: a meta-analysis. Chest. 2006;129:783–90. doi: 10.1378/chest.129.3.783. [DOI] [PubMed] [Google Scholar]
- 40.Cohen E, Weinstein M, Fisman DN. Cost-effectiveness of competing strategies for the treatment of pediatric empyema. Pediatrics. 2008;121:e1250–7. doi: 10.1542/peds.2007-1886. [DOI] [PubMed] [Google Scholar]
- 41.Shah SS, Ten Have TR, Metlay JP. Costs of treating children with complicated pneumonia: a comparison of primary video-assisted thoracoscopic surgery and chest tube placement. Pediatr Pulmonol. 2010;45:71–7. doi: 10.1002/ppul.21143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goodman DC. Unwarranted variation in pediatric medical care. Pediatr Clin North Am. 2009;56:745–55. doi: 10.1016/j.pcl.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


