Abstract
Tricuspid regurgitation secondary to percutaneous lead extraction is uncommon, and it rarely requires surgical intervention. Most tricuspid regurgitation occurs during the implantation of tined leads, which can be entrapped in the tricuspid valve apparatus and may require immediate withdrawal. Severe tricuspid regurgitation as a sequela of extracting chronically implanted leads has rarely been reported. Herein, we report a case of torrential tricuspid regurgitation in a 67-year-old woman after the extraction of a permanent pacemaker lead. The regurgitation was confirmed on transesophageal echocardiography during lead extraction, and the tricuspid valve was successfully repaired with suture bicuspidization of the valve and the support of ring annuloplasty. A short review of the relevant literature follows the case report.
Key words: Cardiology/instrumentation; echocardiography; electrodes, implanted; heart injuries/diagnosis/etiology; pacemaker, artificial/adverse effects/instrumentation; treatment outcome; tricuspid valve/injuries; wounds, penetrating/etiology
Tricuspid regurgitation (TR) after the percutaneous extraction of pacemaker and implantable defibrillator leads is uncommon, but if it is severe, it may require surgical intervention. Herein, we present the case of a patient who had TR secondary to the extraction of a permanent pacemaker, and we report our diagnostic and corrective surgical actions. We also briefly review the relevant medical literature.
Case Report
In 2006, a 67-year-old woman with sick sinus syndrome underwent replacement of a permanent pacemaker generator that had reached end of life. The pacemaker had been implanted when the patient was age 45, and the 1st generator had been replaced when she was age 56. After the 2nd generator was replaced, the patient developed pacemaker pocket (and lead) infection, which was treated conservatively with antibiotics. Her recovery was further complicated by generator erosion. The patient underwent surgery to extract the generator and infected lead and to place a temporary pacemaker. During lead extraction, which was done under transesophageal echocardiographic (TEE) guidance, a small piece of papillary muscle was avulsed, causing moderate TR without pericardial effusion or tamponade. The patient remained hemodynamically stable.
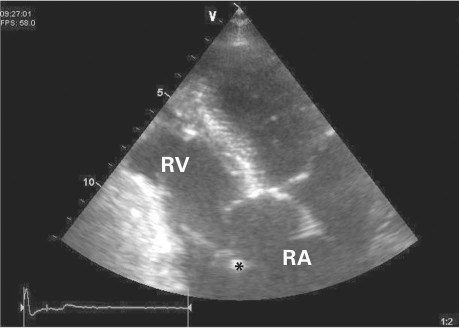
After nearly 2 weeks of conservative treatment, the patient developed right-sided cardiac failure that was resistant to medical therapy. She was afebrile, and blood cultures were sterile for microbial growth. A harsh, parasternal pansystolic murmur of TR (grade 3) increased upon the Carvallo maneuver. A transthoracic echocardiogram (TTE) revealed torrential TR, a freely mobile posterior leaflet with torn chordae tendineae attached, and an avulsed papillary muscle (Fig. 1). We decided to intervene surgically to repair or replace the tricuspid valve. A preoperative coronary angiogram revealed normal coronary anatomy.
Fig. 1 Transthoracic echocardiogram shows an avulsed papillary muscle (asterisk).
RA = right atrium; RV = right ventricle
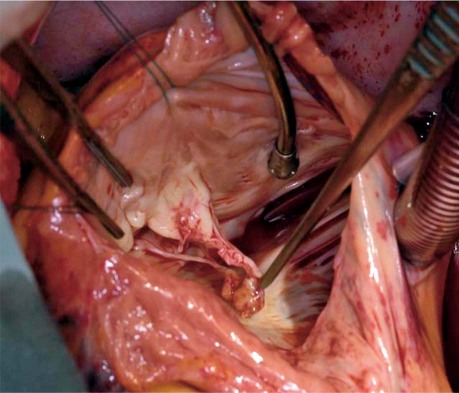
Intraoperatively, TEE revealed a small fibrotic mass at the junction of the superior vena cava and right atrium. After full heparinization of the patient, cardiopulmonary bypass was instituted with central aortic and bicaval venous cannulation. Myocardial protection was achieved through antegrade and retrograde administration of tepid cardioplegic solution. The dilated right atrium was opened obliquely, and the valvular anatomy was inspected. The fibrotic mass was excised (a subsequent microbial culture study ruled out endocarditis vegetation). The posterior papillary muscle was completely torn from the base of its attachment at the right ventricular (RV) free wall, with partial avulsion of the anterior papillary muscle and torn chordae (Fig. 2).
Fig. 2 Intraoperative photograph shows an avulsed papillary muscle of the tricuspid valve.
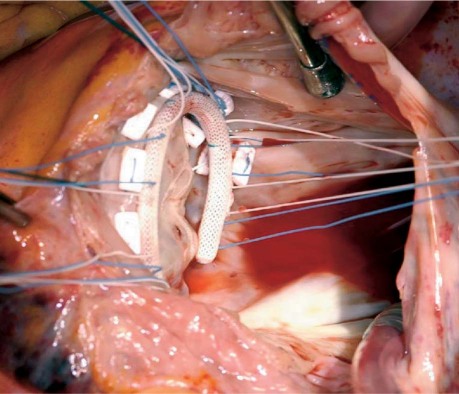
The torn posterior tricuspid leaflet was excised, and the anterior and septal leaflets were repaired with the use of continuous 4–0 Prolene suture, resulting in bicuspidization of the valve. The repair was supported by a size 34 annuloplasty ring (Fig. 3). The right atrium was closed, the heart was de-aired, and the patient was weaned from cardiopulmonary bypass. Both atrial appendages were ligated, epicardial pacing leads were attached to the RV, and a permanent pacemaker was implanted. Intraoperative TEE showed trace TR. The patient was transferred to the intensive care unit in stable condition. She recovered well and was discharged from the hospital on the 8th postoperative day. A pacemaker check was performed before discharge. The patient was placed on tapered diuretic therapy for 4 weeks. After 3 months, TTE showed trace TR, and at 1 and 2 years, mild TR was detected. As of May 2011, the patient was undergoing outpatient clinical monitoring and was reportedly well.
Fig. 3 Intraoperative photograph shows the repaired tricuspid valve.
Discussion
Percutaneous pacemaker leads are commonly extracted when they are infected or when structural failure is noted. Consequent TR is uncommon, and the need for surgical intervention is rare.1–3 Most TR occurs during implantation when tined leads become entrapped in the tricuspid valve apparatus, and their immediate withdrawal is required.4,5 There are few reports of TR as a sequela of extracting chronically implanted leads.6
The periprocedural mortality rate for lead extraction is reportedly between 0.4% and 0.8%. A study of 2,195 lead extractions yielded a 2.5% rate of postoperative death and near-fatal complication, and the investigators presented several preventive recommendations.7 Of note, some patients have multiple medical problems complicated by prolonged infections, which may result in high mortality rates after the procedure.1 It has been reported that, regardless of clinical presentation, the extravascular and intravascular body of the lead is infected even when the infection is local.3
The data are sparse with regard to the incidence of severe TR and its risk factors after percutaneous lead extraction. In 1 study, the incidence was reported to be 13%.2 However, some patients had mild TR before extraction, and the goal of the study was to evaluate new TR after extraction.2
Potential sequelae of lead extraction are bleeding and tears in the subclavian vein, tears in the superior vena cava, perforation of the right atrium or RV, tricuspid valve injury and rupture, hemopericardium, pulmonary embolism, and fatal ventricular and atrial arrhythmias. Most of these sequelae are related to technical difficulty in freeing the leads from myocardial scar tissue.7,8
Injuries to the tricuspid valve can vary from torn chordae to a completely avulsed valvular apparatus. Urgent surgical attention is required if severe TR develops after major damage to the chordae and papillary muscle avulsion or rupture, as seen in our patient. Our patient underwent successful tricuspid valve repair, with a good surgical outcome.
In the intraoperative evaluation of right-sided heart failure, TEE has been very useful in ruling out traumatic causes such as tricuspid valve injury, papillary muscle rupture, hematoma formation, ventricular perforation, hemopericardium, and regional wall-motion abnormality. In our patient, TEE helped to diagnose the partial inner RV-wall and papillary muscle avulsion without hemopericardium. In addition, TEE can exclude other causes of TR that can complicate lead infection, such as valve perforation, adherence between the leads and the leaflets, and tricuspid endocarditis. The TEE imaging can also disclose the type and extent of traumatic damage.9,10 Identifying partial rupture of a papillary muscle is of particular interest, because complete rupture may occur later.11
Conclusion
Because life-threatening tricuspid valve injury and injury to the valvular apparatus can happen during lead extraction, we recommend performing the procedure with TEE guidance and surgeons on standby. Torrential TR may require surgical attention if it is refractory to medical therapy.
Footnotes
Address for reprints: Deepak Mehrotra, MCh, FRACS, Department of Cardiothoracic Surgery, Waikato Hospital, Pembroke St., Hamilton 3200, New Zealand
E-mail: mr.dmehrotra@gmail.com
References
- 1.Henrikson CA, Brinker JA. High post-procedural mortality in lead extraction patients [abstract]. Heart Rhythm 2006;3 (5 Suppl):S12.
- 2.Assouan X, Thuny F, Deharo JC, Franceschi F, Djiane P. Severe tricuspid regurgitation after percutaneous ventricular lead extraction: incidence and predisposing factors [abstract]. Heart Rhythm 2006;3(5 Suppl):S12–S13.
- 3.Klug D, Wallet F, Kacet S, Courcol RJ. Detailed bacteriologic tests to identify the origin of transvenous pacing system infections indicate a high prevalence of multiple organisms. Am Heart J 2005;149(2):322–8. [DOI] [PubMed]
- 4.Res JC, De Cock CC, Van Rossum AC, Schreuder J. Entrapment of tined leads. Pacing Clin Electrophysiol 1989;12(10): 1583–5. [DOI] [PubMed]
- 5.Ong LS, Barold SS, Craver WL, Falkoff MD, Heinle RA. Partial avulsion of the tricuspid valve by tined pacing electrode. Am Heart J 1981;102(4):798–9. [DOI] [PubMed]
- 6.Lee ME, Chaux A, Matloff JM. Avulsion of a tricuspid valve leaflet during traction on an infected, entrapped endocardial pacemaker electrode. The role of electrode design. J Thorac Cardiovasc Surg 1977;74(3):433–5. [PubMed]
- 7.Smith HJ, Fearnot NE, Byrd CL, Wilkoff BL, Love CJ, Sellers TD. Five-years experience with intravascular lead extraction. U.S. Lead Extraction Database. Pacing Clin Electrophysiol 1994;17(11 Pt 2):2016–20. [DOI] [PubMed]
- 8.Byrd CL, Schwartz SJ, Hedin N. Intravascular techniques for extraction of permanent pacemaker leads. J Thorac Cardiovasc Surg 1991;101(6):989–97. [PubMed]
- 9.Rubio PA, al-Bassam MS. Pacemaker-lead puncture of the tricuspid valve. Successful diagnosis and treatment. Chest 1991; 99(6):1519–20. [DOI] [PubMed]
- 10.Jacobson AF, Whitley MA, Harrison SD, Cerqueira MD. Massive tricuspid regurgitation identified on renal flow scintigraphy. Clin Nucl Med 1991;16(10):767–9. [DOI] [PubMed]
- 11.Hilton T, Mezei L, Pearson AC. Delayed rupture of tricuspid papillary muscle following blunt chest trauma. Am Heart J 1990;119(6):1410–2. [DOI] [PubMed]