Abstract
A 52-year-old man with left indirect groin hernia was admitted for elective inguinal repair using the totally extraperitoneal (TEP) approach. After an uneventful intubation, TEP repair of the hernia was performed with three midline trocars. Immediately after extubation, the patient noted severe chest pain. There was a decrease in PaO2 saturation, and neck subcutaneous emphysema was detected. There was no emphysema of the abdomen or of the back. A chest film and thoracic computed tomographic (CT) scan confirmed the presence of pneumomediastinum without pneumothorax. The patient was discharged without complications.
Keywords: Totally extraperitoneal hernia repair, Laparoscopy, Pneumomediastinum
INTRODUCTION
The role of laparoscopic herniorraphy (LH) remains controversial. The totally extraperitoneal (TEP) method is essentially a laparoscopic modification of Stoppa's repair.1 Certain potential intraoperative complications have been reported with laparoscopic hernia repair.2 We report a case of pneumomediastinum and subcutaneous emphysema of the neck, without pneumothorax, after TEP repair.
CASE REPORT
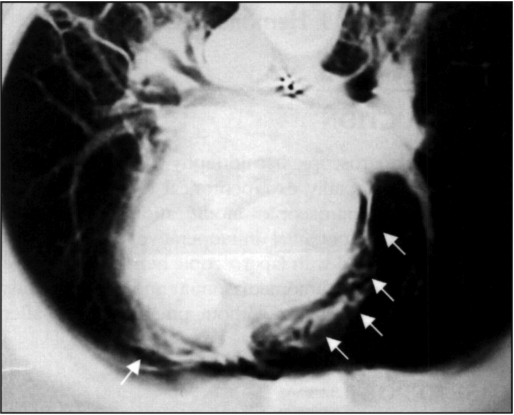
A 52-year-old man, American Society of Anesthesiologists (ASA) level I, 75 kg, 173 cm, with left indirect groin hernia was admitted for elective inguinal repair using the TEP operation. After an uneventful intubation, TEP repair of the hernia utilizing three midline trocars technique was performed. At the beginning of the procedure, SO2 was 98%, blood pressure 140/65 and FetCO2 was 34 mm Hg. Operation time was 32 minutes, with a mean intra-abdominal pressure of 11-12 mm Hg. During the procedure, a small noncomplicated break of the peritoneum was detected and closed with staples. No hemodynamic changes were detected. Immediately after extubation, the patient had severe chest pain, O2 saturation decreased to 84%, FetCO2 increased to 44 mm Hg, and subcutaneous emphysema of the neck was detected. There was no emphysema of the abdomen or of the back. A chest film and thoracic computed tomographic (CT) scan (Figure 1) confirmed the presence of pneumomediastinum without pneumothorax. Fiberoptic bronchoscopy did not reveal any tear in the upper airway. After two hours of mechanical ventilation, the emphysema resolved, and the patient was extubated without any problem. The patient was discharged asymptomatic 48 hours after surgery.
Figure 1.
CT thoracic scan with arrows showing pneumomediastinum.
DISCUSSION
Theoretical advantages of laparoscopic hernioplasty are less pain and a quicker return to normal activity. Complications of TEP laparoscopic hernioplasty are reported infrequently. Bowel, bladder and vessel injuries, bleeding in the preperitoneal space, severe testicular pain, hemoscrotum or nerve entrapment1 noted with TEP hernioplasty have also have been described in open procedures. The detractors of LH mainly criticize the laparoscopic approach as usually being performed under general anesthesia with higher costs and an unknown recurrence rate. However, large series have been published showing a low recurrence rate (0% - 1%).1 In fact, LH is now performed as a day-case procedure.3 TEP repair is performed by dissecting the preperitoneal space and insufflating carbon dioxide to maintain an operative space without pneumoperitoneum. This method potentially avoids the risks of intra-abdominal organ lesions and peritoneal adhesions.
Air may enter the mediastinum from the esophagus, trachea, bronchi, lung, neck, abdomen or retroperitoneal space, producing mediastinal emphysema or pneumomediastinum. Pneumomediastinum is a very rare complication of intra-abdominal laparoscopic procedures.4,5 CO2 usually passes through the hiatus secondary to a congenital anomaly, weak points, defects or a tear in the diaphragm. High-working CO2 pressure or a prolonged insufflation time can also lead to pneumomediastinum. A recent article described a TEP procedure complicated by hypercarbia and the development of massive subcutaneous emphysema without hemodynamic instability.
This was thought to be due to a high intra-abdominal insufflation pressure that ranged between 14 and 18 mm Hg.2
Two cases of pneumothorax have also been previously described during TEP.6,7 It is thought that pneumothorax as a complication of TEP is most likely related to high insufflation pressure and the length of the procedure, itself. Both cases occurred in healthy patients without hiatal or diaphragmatic hernia, and the condition was solved without the placement of a chest tube. Pneumomediastinum was present in both cases.
A retroperitoneal route could be postulated on extraperitoneal procedures, but no retroperitoneal air was present on CT, and no back emphysema was detected. In our case, a hiatal route is the most reasonable explanation for the occurance of pneumomediatinum as insufflation time was short, working pressure was low, and bronchoscopy ruled out an airway disruption.
We conclude that pneumomediastinum can occur after extraperitoneal laparoscopic hernia procedures due to small tears in the peritoneum that occur even with low-working pressures. Only early diagnosis and treatment can avoid serious complications.
References:
- 1. Wegener ME, Arregui MA. Laparoscopic totally extraperitoneal herniorraphy. Problems Gen Surg. 1995;12(1):185–191 [Google Scholar]
- 2. Klopfenstein CE, Gaggero G, Mamie C, Morel P, Forster A. Laparoscopic extraperitoneal inguinal hernia repair complicated by subcutaneous emphysema. Can J Anaesth. 1995;42(6):523–525 [DOI] [PubMed] [Google Scholar]
- 3. Evans DS, Ghaneh P, Khan IM. Day-case laparoscopic hernia repair. Br J Surg. 1996;83:1361–1363 [DOI] [PubMed] [Google Scholar]
- 4. Cunningham AJ. Laparoscopy surgery: anesthesic implications. Surg Endosc. 1994;8(11):1272–1284 [DOI] [PubMed] [Google Scholar]
- 5. Overdijk LE, Rademaker BM, Ringers J, Odoom JA. Laparoscopic fundoplication: a new technique with new complications? J Clin Anesth. 1994;6(4):321–323 [DOI] [PubMed] [Google Scholar]
- 6. Ferzli GS, Kiel T, Hurwitz B, et al. Pneumothorax as a complication of laparoscopic inguinal hernia repair. Surg Endosc. 1997;11:152–153 [DOI] [PubMed] [Google Scholar]
- 7. Murray DP, Rankin RA, Lackey C. Bilateral pneumothoraces complicating peritoneoscopy. Gastrointest Endosc. 1984;30:45–46 [DOI] [PubMed] [Google Scholar]