Abstract
Background:
Laparoscopic cholecystectomy is characterized by a short hospital stay. Hence, pain control on the day of surgery is increasingly important. The aim of this study was to evaluate the effect of intraperitoneal bupivacaine on pain relief following laparoscopic cholecystectomy.
Methods:
Sixty patients undergoing elective laparoscopic cholecystectomy were prospectively randomized into 2 groups. Following removal of the gallbladder, group A received 100 mg of bupivacaine in 50 cc of saline, installed into the gallbladder bed and right subphrenic space. Group B received saline without bupivacaine. Pain was assessed using a visual/analog scale at fixed-time intervals.
Results:
No significant difference occurred in the average pain levels between the groups at 1, 2, 4, and 14 hours postsurgery. The average analgesic requirement was lower in the bupivacaine group, but this did not reach statistical significance.
Conclusion:
Application of intraperitoneal bupivacaine did not attenuate pain following laparoscopic cholecystectomy, and no role exists for its routine use.
Keywords: Laparoscopy, Cholecystectomy, Postoperative pain, Bupivacaine
INTRODUCTION
The introduction of laparoscopic techniques into general surgery has dramatically changed our attitudes about the postoperative course of patients after cholecystectomy. Laparoscopic cholecystectomy is characterized by a short hospital stay and an early return to normal activity. Typically, patients are discharged home on the first postoperative day. As experience has expanded, a few recently reported series have shown that this operation is safe and feasible as an outpatient procedure in properly selected patients.1–3 Thus, pain relief and patient comfort on the day of surgery have become increasingly important, as the need for analgesics may delay discharge on the same day.
Pain on the day of surgery is typically a diffuse abdominal pain, more so to the right upper quadrant, and radiates to the right shoulder.4 We assumed that this pain is mainly generated by irritation of the peritoneum, especially at the right upper abdomen, and hypothesized that the application of a local anesthetic agent into the peritoneal cavity would reduce this pain.
The aim of this study was to evaluate the use of intraperitoneal bupivacaine on pain relief following laparoscopic cholecystectomy.
MATERIALS AND METHODS
Sixty patients undergoing elective laparoscopic cholecystectomy were prospectively randomized into 2 groups. Group A received 100 mg of bupivacaine diluted in 50 mL of saline and installed into the peritoneal cavity. Group B received intraperitoneal saline. Following removal of the gallbladder and thorough irrigation, a feeding tube was inserted through the 5 mm trocar at the right upper quadrant, and its tip was guided using a grasping instrument inserted through the subxyphoid port. The solution was then released into the gallbladder bed and right subphrenic space, and the gas and instruments were removed.
Pain was assessed using a visual/analog scale of 1 to 10, at 1, 2, 4 and 14 hours after the end of the operation. All the patients were allowed to receive analgesic medications as needed, and the requirement of these medications was recorded. Analgesic medications included 1 mg per Kg of intramuscular meperidine on the day of surgery, and 5 mg of oral oxycodone with 325 mg of acetaminophen on the following day, except in cases of allergy to these drugs.
The patients, the surgeons, and the nursing staff were blinded to the randomization. Anesthesia was administered according to a uniform study protocol to minimize the effect of different anesthesia drugs and techniques on the study results.
The study was approved by the local investigational review board for clinical studies, and all the patients gave their informed consent.
Patients in whom the procedure was converted to an open procedure and patients in whom a drain was left in the peritoneal cavity were excluded from the study.
Statistical analysis was performed using a two-tailed t test and chi-square analysis, and significance was determined as p<0.05.
RESULTS
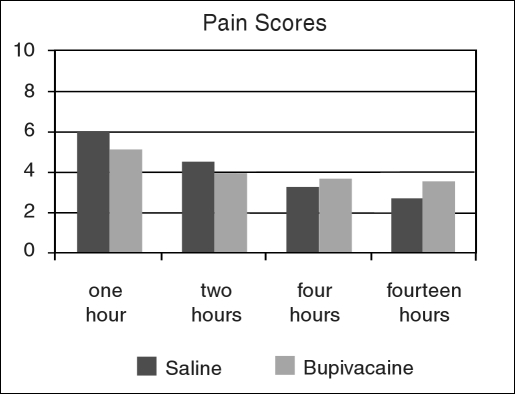
Nine patients were excluded from the study for the reasons mentioned above, leaving 51 patients for the data analysis. Twenty-six of them received bupivacaine, and 25 received saline. Mean age and sex distribution did not differ significantly between the two groups (Table 1). No significant difference occurred in the average pain levels between patients who received intraperitoneal bupivacaine and patients who received saline at all the time intervals (Figure 1). Furthermore, the difference between the average pain scores of the two groups was less than one at all time intervals, suggesting that this difference is not clinically significant.
Table 1.
Demographic data of the study groups.
| Bupivacaine (n=26) | Saline (n=25) | |
|---|---|---|
| Male | 9 | 7 |
| Female | 17 | 18 |
| Mean Age | 45 | 43.5 |
Figure 1.
Average pain levels, on a visual/analog scale of 1 to 10, at fixed time intervals from completion of the surgical procedure.
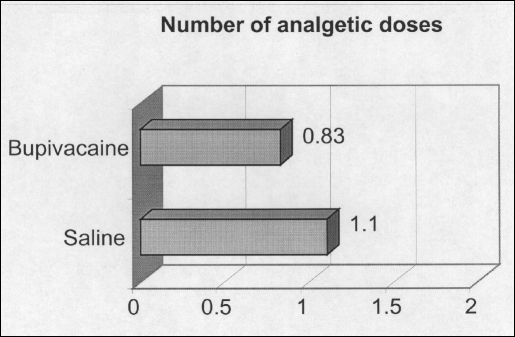
The average analgesic requirement was lower in the bupivacaine group, but this did not reach statistical significance (Figure 2).
Figure 2.
Average number of doses of analgetic medications per patient in each group. Each analgetic dose consisted of 1 mg/kg of meperidine (except in cases of meperidine allergy).
DISCUSSION
Although minimally invasive surgery is characterized by reduced pain, it is not painless.5 Patients undergoing laparoscopic cholecystectomy suffer considerable pain on the day of surgery, frequently requiring narcotic analgesics. The average pain scores of the entire group in our series was 5.5 in a scale of 1 to 10 in 1 hour, 4.25 in 2 hours, and 3.3 in 4 hours postsurgery.
The pain characteristics suggest an intra-abdominal origin, and it seems unlikely that this pain is generated mainly by the small skin incisions. Studies of local anesthetics infiltrated into the skin wounds report reduced postoperative pain only to a minor degree.6,7 Pain may be generated by stretching of the abdominal wall duringthe pneumoperitoneum, by the local dissection, or by irritation of the peritoneum from blood, bile spillage, or by the CO2 used for creation of the pneumoperitoneum.
We assumed that early postoperative pain was mainly generated by irritation of the peritoneum, and the application of a local anesthetic agent may attenuate this pain. Previous studies have suggested that the use of local anesthetics to block the afferent pain sensation may reduce the central hyper-excitability of the dorsal horn neurons in the spinal cord, in response to surgical trauma.8 Clinical studies of intraperitoneal bupivacaine have had inconsistent results. Whereas few authors have found a statistically significant difference with the use of local anesthetics,8–13 others, including those of this study, could not repeat these results.4,14–17 Furthermore, in a few of the studies that have found a statistically significant difference with the use of bupivacaine, the difference between the average pain scores was less than 1 in a scale of 1 to 10.9,12 Although this difference was foundto be significant in statistical tests, it is doubtful whether such a difference is of clinical significance.
This study suggests that intraperitoneal bupivacaine installed at the end of the procedure did not attenuate pain following laparoscopic cholecystectomy. Pasqualucci et al18 and Mraovic et al10 have suggested that application of local anesthetics prior to the dissection of the gallbladder may enhance the effect and reduce pain. The sensory nerves conducting pain sensation to the posterior horn of the spinal cord transmit impulses during the dissection and may turn into a hyper-excitable state.18 Thus, application of the local anesthetic after the dissection is completed may not significantly attenuate the excitability of these nerves. Blocking these nerves prior to the dissection may result in more successful attenuation of pain following laparoscopic cholecystectomy.
The cause of the early postoperative pain in laparoscopic cholecystectomy is not clearly understood. The CO2 used to create the pneumoperitoneum may induce local changes that irritate the peritoneum, such as local acidosis due to CO2 dissolution in the peritoneal tissue. Because the gas is equally distributed in the peritoneal cavity, application of a local anesthetic agent to the right upper quadrant may not be sufficient to attenuate this pain. Use of a higher volume of local anesthetic solution, sufficient to irrigate most of the peritoneal cavity, may also improve the effect on pain after laparoscopy. However, because absorption of the drug from the peritoneum occurs, care should be taken not to administer overdoses of these agents.
CONCLUSION
Intraperitoneal bupivacaine did not attenuate pain following laparoscopic cholecystectomy in this study. These results suggest that no role exists for the use of intraperitoneal bupivacaine, in the fashion described here, in laparoscopic cholecystectomy. Further studies are needed to establish the role of intraperitoneal bupivacaine for pain relief in laparoscopic surgery.
Footnotes
Presented at the 8th International Meeting of Laparoendoscopic Surgeons, SLS Annual Meeting Endo Expo ‘99, December 4-7, 1999, in New York City, USA
Statement of Disclosure: None of the authors have any financial interest in any commercial drug, device, equipment, or instrument that is the subject of this article. This study was not supported by any commercial or drug company.
Contributor Information
Oded Zmora, Departments of Surgery and Transplantation..
Orit Stolik-Dollberg, Department of Anesthesiology..
Barak Bar-Zakai, Departments of Surgery and Transplantation..
Danny Rosin, Departments of Surgery and Transplantation..
Joseph Kuriansky, Departments of Surgery and Transplantation..
Moshe Shabtai, Departments of Surgery and Transplantation..
Azriel Perel, Department of Anesthesiology..
Amram Ayalon, Departments of Surgery and Transplantation..
References:
- 1. Mjaland O, Reader J, Aesboe V, Trondsen E, Buanes T. Outpatient laparoscopic cholecystectomy. Br J Surg. 1997;84:958–961 [DOI] [PubMed] [Google Scholar]
- 2. Keulmans Y, Eshuis J, de Haes H, de Wit LT, Gouma DJ. Laparoscopic cholecystectomy: day-care versus clinical observation. Ann Surg. 1998;228:734–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Simpson JP, Savarise MT, Moore J. Outpatients laparoscopic cholecystectomy: What predicts the need for admission? Am Surg. 1999;65:525–528 [PubMed] [Google Scholar]
- 4. Joris J, Thiry E, Paris P, Weerts J, Lamy M. Pain after laparoscopic cholecystectomy: characteristics and effect of intraperitoneal bupivacaine. Anesth Analg. 1995;81:379–384 [DOI] [PubMed] [Google Scholar]
- 5. Stevens HP, van de Berg M, Ruseler CH, Wereldmasa JC. Clinical and financial aspects of cholecystectomy: laparoscopic versus open technique. World J Surg. 1997;21:91–96 [DOI] [PubMed] [Google Scholar]
- 6. Kum CK, Wong CW, Goh PM, Ti TK. Comparative study of pain level and analgesic requirement after laparoscopic and open cholecystectomy. Surg Laparosc Endosc. 1994;4:139–141 [PubMed] [Google Scholar]
- 7. Dath D, Park AK. Randomized, controlled trial of bupiva-caine injection to decrease pain after laparoscopic cholecystectomy. Can J Surg. 1999;42:284–288 [PMC free article] [PubMed] [Google Scholar]
- 8. Dahl JB, Erichsen CJ, Fuglsang-Frederikson A, Kehlet H. Pain sensation and nociceptive reflex excitability in volunteers and surgical patients. Br J Anesth. 1992;69:117–121 [DOI] [PubMed] [Google Scholar]
- 9. Szem JW, Hydo L, Barie PS. A double blind evaluation of intraperitoneal bupivacaine vs saline for the reduction of postoperative pain and nausea after laparoscopic cholecystectomy. Surg Endosc. 1996;10:44–48 [DOI] [PubMed] [Google Scholar]
- 10. Mraovic B, Jurisic T, Kogler-Majeric V, Sustic A. Intraperitoneal bupivacaine for analgesia after laparoscopic cholecystectomy. Acta Anesthesiol Scand. 1997;41:193–196 [DOI] [PubMed] [Google Scholar]
- 11. Weber A, Munoz J, Garteiz D, Cueto J. Use of subdiaphragmatic bupivacaine installed to control postoperative pain after laparoscopic surgery. Surg Laparosc Endosc. 1997;7:6–8 [PubMed] [Google Scholar]
- 12. Tsimoyiannis EC, Glatzounis G, Lekkas ET, Siakas P, Jabarin M, Tzourou H. Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1998;8:416–420 [PubMed] [Google Scholar]
- 13. Cunniffe MG, McAnena OJ, Calleary J, Flynn N. A prospective randomized trial of intraperitoneal bupivacaine irrigation for management of shoulder-tip pain following laparoscopy. Am J Surg. 1998;176:258–261 [DOI] [PubMed] [Google Scholar]
- 14. Schulte-Steinberg H, Weninger E, Jokisch D, et al. Intraperitoneal versus intrapleural morphine or bupivacaine for pain after laparoscopic cholecystectomy. Anesthesiol. 1995;82:634–640 [DOI] [PubMed] [Google Scholar]
- 15. Scheinin B, Kellokumpu I, Ligdgren L, Haglund C, Rosenberg PH. Effect of intraperitoneal bupivacaine on pain after laparoscopic cholecystectomy. Acta Anesthesiol Scand. 1995;39:195–198 [DOI] [PubMed] [Google Scholar]
- 16. Raetzell M, Maier C, Schroder D, Wolf H. Intraperitoneal application of bupivacaine during laparoscopic cholecystectomy-risk and benefit? Anesth Analg. 1995;81:967–972 [DOI] [PubMed] [Google Scholar]
- 17. Johnson RC, Hedges AR, Morris R, Stamatakis JD. Ideal pain relief following laparoscopic cholecystectomy. Int J Clin Pract. 1999;53:16–18 [PubMed] [Google Scholar]
- 18. Pasqualucci A, De Angelis V, Contardo R, et al. Preemptive analgesia: Intraperitoneal local anesthetic in laparoscopic cholecystectomy. Anesthesiol. 1996;85:11–20 [DOI] [PubMed] [Google Scholar]