Abstract
Patients are frequently referred to physical therapy with the diagnosis of shoulder and arm pain. During examination and evaluation of the patient, the physical therapist must consider all potential causes of the patient’s symptoms. Three questions are used as the conceptual basis for a diagnosis-based clinical decision rule in the management of mechanical and non-mechanical musculoskeletal pain when addressing the differential diagnosis of a patient’s condition. This single patient case report describes the use of these three questions in the differential diagnosis of shoulder and arm pain. A 44-year-old male was referred with a diagnosis of shoulder impingement syndrome. Each of the three questions for differential diagnosis was addressed, and clinical tests and examination findings were used to differentiate the origin of the patient’s symptoms. The intervention provided is outlined along with the patient’s response to the different treatment strategies provided. This case identifies the need for a systematic method of differential diagnosis so that patients are appropriately managed.
Keywords: Arm pain, Cervical radiculopathy, Differential diagnosis, Shoulder impingement
Pain experienced in the shoulder, upper, and lower arm can be as a result of a myriad of medical conditions,1 including mechanical pain from nearby musculoskeletal structures such as the shoulder or the cervical spine,2–4 or from regional structures such as the thoracic spine and brachial plexus.5 Non-mechanical tissues such as metastasis of surrounding bones or referred pain from the viscera can also cause arm pain.6,7 Appropriate questioning during the history and selected physical measurements can assist in determining whether the pain is mechanical or non-mechanical in nature.
Murphy and Hurwitz advocate the use of three diagnostic questions as a conceptual basis for a clinical decision making rule in the management of mechanical and non-mechanical musculoskeletal pain.8 The first question, ‘Are the patient’s symptoms reflective of a visceral disorder or a serious or potentially life-threatening illness’, should trigger the therapist to consider whether the signs and symptoms could be arising from non-mechanical conditions such as cancer of the surrounding bone or soft tissues, visceral pathology, fracture, disease of the gastrointesitinal tract, or seronegative spondyloarthropathy. The second question, ‘From where is the patient’s pain arising’ does not involve narrowly identifying one structural source of the pain; rather, the therapist tries to understand the characteristics about the pain source. This leads the therapist to use the appropriate tests and measures early in the physical examination to rule out conditions. The third and final question ‘What has gone wrong with this person as a whole that would cause the pain experience to develop and persist’, encourages the therapist to consider what other variables are present that serve to maintain or perpetuate the pain experience. Possible factors for consideration are depression, passive coping, central pain hypersensitivity, and fear.
The use of these three questions in the management of mechanical and non-mechanical musculoskeletal pain allows recognition of conditions outside the boundaries of the clinician’s practice.8 Tests chosen based on the information gleaned in the second question are used later in the physical examination as diagnostic tests and are confirmatory in nature.9,10 Contributory conditions which may affect prognosis can be recognized and management can be altered to affect these conditions as well. The process allows best use of current test metrics (e.g. sensitivity and specificity) and improves the likelihood of proper management of the patient during unknown or missed diagnoses. Subsequently, the goal of this resident’s case report is to demonstrate the dynamics of the diagnosis-based clinical decision rule for the management of a patient presenting with vague arm pain who was medically diagnosed with shoulder impingement syndrome. The true mechanical nature of the patient’s condition is outlined and contributory elements are addressed by following this systematic approach.
Case Description
Patient history
The patient was a 44-year-old male who worked full-time in the administration offices of a local university. The patient spent over 80% of his day seated at his desk working on his computer. The patient did report a positive history for hypertension which was at the time controlled medically. The patient had no other medical history that was compelling.
The patient reported a 6-week history of pain in his left arm. The pain had started insidiously and had not diminished in intensity. Subsequently, the patient sought medical care from his primary care physician. The patient’s primary care physician diagnosed the arm pain as rotator cuff tendonitis, and the patient was referred to a sports medicine clinic for further evaluation. The sports medicine physician diagnosed the patient as having symptoms of shoulder impingement and added that it was possible the patient also had pathology of the subscapularis. The patient was prescribed a steroid anti-inflammatory (steroid dosepak)at this time. The patient reported that the dosepak provided minimal relief from the pain. Two weeks later, the sports medicine physician injected the patient’s left posterior shoulder with cortisone. According to the patient, the pain relief was greater with the injection than the dosepak but still minimal.
An X-ray was taken of the left shoulder which was found to be normal. The patient was then referred to PT with a diagnosis of shoulder impingement syndrome and a tight posterior capsule. The physician specifically requested that the patient be taught the ‘sleeper stretch’, which involves lying on one’s side and stretching the arm into internal rotation.11
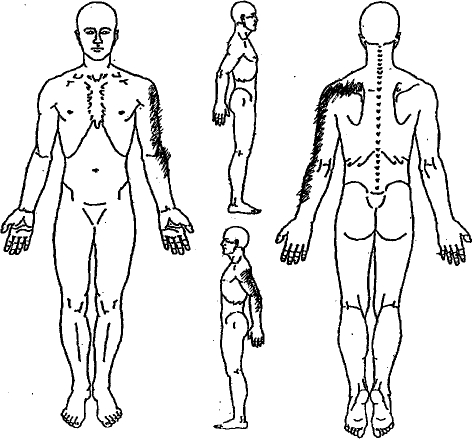
The patient rated his left arm pain as a 3/10 (0, no pain; 10, worst pain imaginable) in intensity on a numeric pain rating (NPR) scale at the time of the PT examination. He reported that the pain traveled from the left scapula down the left arm as far as the forearm (Fig. 1). The patient also reported that he had intermittent pain into the hand. The patient described the pain he experienced as ‘burning’, ‘throbbing’, and ‘sore’ in nature. The most intense pain that the patient had experienced in the past 24-hours had been 6/10 on the NPR scale. Furthermore, the patient described a cough that had started a week prior to the PT initial examination and appeared to have irritated his left arm pain. The patient also described difficulty sleeping at night due to pain in his left arm.
Figure 1.
Body chart of reported pain.
Clinical impression (following the patient history)
Following the patient history, the therapist considered several tentative differential diagnoses. It was possible that the patient’s symptoms were related to cardiac pathology due to a positive cardiac history. Further questioning in this area revealed that the patient had undergone a complete cardiac work up with stress testing a month earlier when his physician had suspected that the arm symptoms were cardiac related. The results of this testing were negative. Potential mechanical sources of the patient’s symptoms that were considered included the shoulder complex and the cervical spine.
Shoulder impingement was one of several shoulder pathologies that could be referring pain into the left arm.1 With pain radiating below the shoulder, it was necessary to clear the cervical spine as a potential source of the pain.3 The relationship of the cough to the exacerbation of arm pain also alerted the examiner to consider what mechanisms were contributing to the perpetuation of the pain.
Examination
The patient demonstrated poor unsupported sitting posture with an increased thoracic kyphosis and forward posture of the head. There was no appreciable difference in muscle bulk noted between the left and right upper quadrants. Based on the patient history, it was decided to rule out shoulder pathology and rule in the cervical spine as a potential source of the patient’s symptoms. This information was sought to answer the second question (source of pain) in the series of 3 proposed by Murphy and Hurwitz.8
Active range of motion (AROM) testing was completed of the left shoulder; there was no loss of motion noted or production of the patient’s pain with AROM or with overpressure into each direction. The Neer and Hawkins–Kennedy tests were then used to rule out shoulder impingement as a potential diagnosis. The metrics of both the Neer and Hawkins–Kennedy tests made each suitable during the screening process as both tests have high sensitivity, with Caliş et al.12 reporting sensitivity of the Neer test at 89% and of the Hawkins–Kennedy test at 92%. Tests with high sensitivity are appropriate to be used when screening for pathology; when the test is negative, it is appropriate to consider that the condition being tested is not present.13 When each test was performed, the patient’s pain was not produced and motion was symmetrical bilaterally. The patient demonstrated a negative lift-off test,14 which is a specific measure that is used for assessment of subscapularis involvement, and he demonstrated a negative external rotation lag sign which discounted the external rotators as a potential source of the pain.15
With negative findings for an association between the patient’s symptoms and the left shoulder, the assessment continued with examination of the cervical spine. Cervical extension was limited to 50% of the patient’s expected range of motion. The patient was reluctant to move further into extension because of increased pain felt in the left scapula and upper arm that was concordant with the patient’s pain. Cervical left rotation was also limited to 50% of the patient’s range in comparison to right cervical rotation, and this too increased the patient’s pain in the left upper arm. Cervical flexion and right rotation had minimal motion losses and did not increase pain reported in the left arm.
The patient displayed a positive Spurling’s test. The metrics of the Spurling’s test make it an appropriate test to use to rule in cervical radiculopathy.16 A neurological examination of the left upper extremity revealed no alteration in deep tendon reflex activity between the right and left upper limbs. Cutaneous sensation was assessed with light touch, and it was found to be symmetrical between the two limbs. The myotomal examination revealed weakness of the left wrist extensors and flexors, biceps, and triceps. An upper limb tension test for the medial nerve was positive for increasing the patient’s symptoms. An attempt at supine cervical traction initially provided a slight reduction of the left arm pain. However, as the traction was released the pain rebounded to its original level and possibly even above the resting pain level. Traction, also known as cervical distraction, is a test that has high specificity when testing for cervical radiculopathy. The initial positive response to the traction added to the tentative diagnosis of cervical radiculopathy in addition to the other positive findings so far.
Clinical impression following the physical examination
A summary of the findings from the physical examination combined with the patient history is outlined in Table 1. In short, the findings that implicated the cervical spine far outweighed those suggestive of shoulder impingement.
Table 1. Summary of history and examination findings.
| Findings favoring the shoulder | Findings favoring the cervical spine |
| Pain location | Pain location |
| Positive Spurling’s test | |
| Positive cervical distraction test | |
| Positive upper limb tension test | |
| Pain provoked with cervical motion | |
| Negative Neer test | |
| Negative Hawkins–Kennedy test | |
| Pain-free AROM left shoulder | |
| Insidious onset |
Diagnosis and prognosis
The physical examination of this patient revealed that the origin of the patient’s symptoms was most likely the cervical spine and not the left shoulder. Movements of the cervical spine had produced the patient’s symptoms, and testing of the left shoulder had not produced the symptoms. These findings were coupled with myotomal weakness in the left upper extremity for the cervical sixth and seventh nerve roots. The patient exhibited significant decreased cervical rotation to the left [his concordant (symptomatic?) side], a positive Spurling’s sign, a positive upper limb tension sign, and a positive finding with the cervical distraction test. Wainner et al.16 demonstrated 4 of 4 positive results during a clinical examination yielding a positive likelihood ratio of 30.3 which further supported the initial diagnoses of cervical radiculopathy.
Two weeks after the physical therapy evaluation, radiography of the cervical spine (frontal, lateral, open mouth and oblique views) was performed and revealed multilevel degenerative disk disease as noted by the disk space loss and endplate osteophytosis most notable at C4–C5 and C5–C6. Uncovertebral hypertrophy was most notable at C3–C4 and C4–C5 with possible bilateral foraminal narrowing. A month later, a magnetic resonance imaging scan was taken (Fig. 2) and revealed a large disc herniation at C6–C7, which supported the signs and symptoms outlined during the clinical examination. It is not uncommon for imaging studies to portray disk herniations in patients who are asymptomatic.17 However, in the case of this study, the level of herniation corresponded with the myotomal weakness detected.
Figure 2.

Sagital magnetic resonance imaging scan of the cervical spine. The image displays disruption at the C6 segment. There is also osteophyte lipping at the margins of the vertebral bodies above the C6 level.
The imaging findings provided further information to answer the third and final question that proposed by Murphy and Hurwitz8 regarding the perpetuation of the symptoms. The presence of large disc herniation, poor posture, and persistent coughing were all factors that would contribute to the perpetuation of the symptomology.
The patient’s prognosis at this time was considered good because he presented with several demographical and clinical findings that increase the likelihood of recovery. These findings were the presence of the symptoms in the non-dominant arm, being under 54 years of age, and that looking down did not worsen the symptoms. These findings fit the clinical prediction rule that was proposed by Cleland et al.18 that identified patients who were most likely to achieve success with physical therapy interventions.
Outcomes
The patient’s progress was tracked from visit to visit using the several measures. At each visit the patient reported his current pain using the NPR scale, his impression of his functional ability with the use of a percentage where 100% was full function and 0% was no function, and the global rate of change (GROC). The GROC is a 15-point scale that has been shown to provide a quick, flexible, and simple method of charting self-assessed clinical progress. Kamper et al.19 provided evidence that the GROC is clinically relevant, has adequate reproducibility, and is sensitive to change. The final measure used was the quickDASH, a refined outcome measure that was based on the Disabilities of the Arm, Shoulder, and Hand (DASH) scale. Referred with a diagnosis of shoulder impingement, the patient was provided with the quickDASH scale at intake. The quickDASH is a scale that utilizes 0–100%. Zero per cent corresponds to no limitations, and 100% corresponds to total limitation. As the majority of the patient’s functional limitations related to his left upper extremity, this self-reported outcomes measure still retain construct validity for use for a cervical related disorder.20 A summary of the outcomes for each visit is listed in Table 2.
Table 2. Summary of the patient’s symptoms throughout the course of treatment.
| Visits | Pain (current) | GROC | Level of function | DASH |
| 1 | 3 | NA | 80 | 50 |
| 2 | 3 | 0 | 80 | |
| 3 | 2 | −1 | 80 | |
| 4 | 3 | 1 | 80 | |
| 5 | 2 | −1 | 80 | 18 |
| 6 | 3 | −1 | 80 | |
| 7 | 2 | 0 | 80 | 14 |
| 8 | 2 | 2 | 90 | |
| 9 | 1 | 1 | 90 | 9 |
| 10 | 2 | 1 | 90 | |
| 11 | 1 | 2 | 90 | |
| 12 | 1 | 2 | 90 | 5 |
Note: GROC, global rating of change; quickDASH, disabilities of the shoulder and hand questionnaire.
Interventions
Management of cervical radiculopathy can be challenging. The literature suggests a multi-faceted or variety of treatment are appropriate in the management of patients with this condition.18 A summary of the treatment techniques and the days on which they were provided is provided in Table 3. The patient was seen for a total of 12 visits and was discharged by day 80 to continue his strength exercises.
Table 3. Summary of treatment provided.
| Intervention | Outcome | |
| Visit 1 | Initial evaluation, manual traction (30 seconds×3 reps), mechanical traction (15 pounds intermittent×3 minutes), workplace ergonomic assessment setup, home exercise program, and patient education (including, education about coughing contributions). | Mechanical traction was poorly tolerated by the patient, and the traction was discontinued after 3–4 minutes because the arm pain increased from 3/10 to 5/10. |
| Visit 2 | Manual traction (30 seconds×3 reps), mechanical traction (20 pounds intermittent×10 minutes) and deep cervical flexor strengthening exercises (in clinic and for a home exercise program). | Manual traction reduced resting symptoms. Again, there was no reduction of pain with mechanical traction thus this intervention was terminated. |
| Visit 3 | Reverse sustained natural apophyseal glides at the cervico-thoracic junction to increase motion in the upper thoracic spine. The patient was educated in the self-mobilization of the median nerve. Educated again about the significance of the continued coughing. | The patient’s symptoms were more irritated at the start of the session secondary to the coughing. There were no within session symptom changes. |
| Visits 4–8 | The patient returned reporting a gradual increase in sleep duration. Continued therapy was directed at the upper thoracic spine. Progression of the deep cervical flexor strength program to functional postures. | The patient demonstrated 75% or greater AROM of the cervical spine before feeling any left arm symptoms. |
| Visits 9–12 | Occasional arm pain – only triggered with a cough. Progressed strengthening of the triceps. Increased extensor stretch to the upper thoracic spine with the use of the mobilization belt and extension proximal to this. | Full AROM of the cervical spine without arm pain. Return of left triceps strength to 4+/5. |
Discussion
This case report describes the role of using three questions as a conceptual basis for a diagnoses-based clinical decision rule in the assessment of a patient with upper limb pain. This case is unique because it outlines the use of three questions when addressing the differential diagnosis of a patient’s condition.8 It was possible to arrive at a tentative diagnosis that established the patient’s symptoms were arising from the cervical spine and not from the left shoulder by using these questions.
The first question, ‘Are the patient’s symptoms reflective of a visceral disorder or a serious or potentially life-threatening illness?’, triggered the therapist to consider all potential causes of pain that could be experienced into the left arm. With a history of hypertension, the pain that the patient was experiencing could have been cardiac related. The patient’s recent cardiac testing did not reveal any abnormalities, and the fact that the patient’s left arm pain was influenced by musculoskeletal motion further confirmed that his left arm pain was from a mechanical mechanism and not from a visceral source. The importance of considering all the sources of pain was highlighted by Mamula et al.5 when a patient with what appeared to be cervical radiculopathy causing left arm pain actually had Parsonage–Turner syndrome.
The answer to the second question ‘From where is the patient’s pain arising?’ acts to further narrow the focus of the examination. Motion of the cervical spine produced the patient’s left arm pain. The shoulder testing was negative. This clear cause and effect relationship made it intuitive that the origin of the left arm symptoms was from the cervical spine. The use of the pain production with cervical motion acted as a suitable benchmark to assess the patient’s progress over the subsequent treatment sessions.
The third question ‘What has gone wrong with this person as a whole that would cause the pain experience to develop and persist?’, can be partially answered with the results of the imaging that was performed. It is clear that there were considerable degenerative changes at the joint and disk level in the mid-cervical spine. It is possible that the nature of the patient’s occupation that involved prolonged periods of sitting and working on the computer may have increased the stress on the compromised cervical structures. The repetitive coughing that the patient experienced in the early treatment sessions was a confounding factor in perpetuating the irritation of the cervical structures.
The role of using differential diagnosis in the evaluation is not new to physical therapists. There are numerous articles and books available on this topic that provide different frameworks for differential diagnosis.1,5–7,21 The complexity of these frameworks varies between publications. The use of the three questions proposed by Murphy and Hurwitz8 provided sequential steps to establish the origin of the patient’s symptoms while at the same time ruling out inaccurate sources of the patient’s symptoms. Using this framework in conjunction with the current knowledge of the metrics of the special tests used in the examination improves the likelihood that the correct diagnosis is identified.
Management of this patient’s condition was initially focused on establishing the nature of the problem. Once this was established, evidence-based care using the findings of Cleland and colleagues18 in the management of cervical radiculopathy was instigated. This approach ensured a short-term successful outcome with restoration of pain-free sleep and infrequent arm pain. There was also a sizable improvement in the quickDASH score (45 point improvement from the initial evaluation to the final session). This supports the initial choice to use the quickDASH to capture functional changes that occurred with arm pain that was a result of cervical pathology. Goode et al.20 have shown that outcomes measures are sensitive to identify changes in function for body regions other than where they traditionally used. The quickDASH reflects functional challenges associated with the upper extremities, and this is where the patient’s symptoms were located. Therefore, the scale still demonstrated construct validity for use.
Conclusion
This case report describes the evaluation and subsequent treatment of a patient who was originally diagnosed with shoulder pain. Using the three question approach, a systematic examination and evaluation was completed that accurately revealed the source of the patient’s symptoms. With specific questioning during the subjective portion of the evaluation and the use of tests for the left shoulder that had high sensitivity, the shoulder was eliminated early in the examination as a potential source of the patient’s symptoms. When using the metrics of special tests in this manner, a clinician avoids using tests that provide inaccurate information.
References
- 1.Pateder D, Berg J, Thal R. Neck and shoulder pain: differentiating cervical spine pathology from shoulder pathology. J Surg Orthop Adv 2009;18:170–4 [PubMed] [Google Scholar]
- 2.Tyler TF, Nicholas SJ, Lee SJ, Mullaney M, McHugh MP. Correction of posterior shoulder tightness is associated with symptom resolution in patients with internal impingement. Am J Sports Med 2010;38:114–9 [DOI] [PubMed] [Google Scholar]
- 3.Cook C. Orthopedic manual therapy. An evidence-based approach. Upper Saddle River, NJ: Pearson Prentice Hall; 2007 [Google Scholar]
- 4.Eubanks J. Cervical radiculopathy: nonoperative management of neck and radicular symptoms. Am Fam Physician 2010;81:33–40 [PubMed] [Google Scholar]
- 5.Mamula C, Erhard R, Piva S. Cervical radiculopathy or Parsonage–Turner syndrome: differential diagnosis of a patient with neck and upper extremity symptoms. J Ortho Sports Phys Ther 2005;35:659–64 [DOI] [PubMed] [Google Scholar]
- 6.Boissonnault W. Primary care for the physical therapist. Examination and triage. St. Louis, MO: Elsevier Saunders; 2005 [Google Scholar]
- 7.Goodman C, Kelly T. Differential diagnosis for physical therapists: screening for referral. Philadelphia, PA: Saunders; 2006 [Google Scholar]
- 8.Murphy D, Hurwitz E. A theoretical model for the development of a diagnosis-based clinical decision rule for the management of patients with spinal pain. BMC Musculoskelet Disord 2007;8:75–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook C, Hegedus E. Orthopedic physical examination tests. Upper Saddle River, NJ: Pearson Education; 2008 [Google Scholar]
- 10.Hegedus E. Studies of quality and impact on clinical diagnosis and decision-making. J Man Manip Ther 2010;18:5–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Ortho Sports Phys Ther 2007;37:108–14 [DOI] [PubMed] [Google Scholar]
- 12.Caliş M, Akgün K, Birtane M, Karacan I, Caliş H, Tüzün F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis 2000;59:44–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woolf A. History and physical examination. Best Pract Res Clin Rheumatol 2003;17:381–402 [DOI] [PubMed] [Google Scholar]
- 14.Gerber C, Krushell R. Isolated rupture of the tendon of the subscapularis muscle. J Bone Joint Surg Am 1991;73:389–94 [DOI] [PubMed] [Google Scholar]
- 15.Walch G, Boulahia A, Calderone S, Robinson A. The ‘dropping’ and ‘hornblower’s’signs in evaluation of rotator-cuff tears. J Bone Joint Surg Am 1998;80:624–8 [DOI] [PubMed] [Google Scholar]
- 16.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-reported measures for cervical radiculopathy. Spine 2003;28:52–62 [DOI] [PubMed] [Google Scholar]
- 17.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 1994;331:69–73 [DOI] [PubMed] [Google Scholar]
- 18.Cleland J, Fritz J, Whitman J, Heath R. Predictors of short-term outcome in people with a clinical diagnosis of cervical radiculopathy. Phys Ther 2007;87:1619–32 [DOI] [PubMed] [Google Scholar]
- 19.Kamper S, Maher C, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther 2009;17:163–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goode A, Cook C, Brown C, Isaacs R, Roman M, Richardson W. Differences in comorbities on low back pain and low back pain related leg pain. Pain Pract. 2010 Jun 30 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorski J, Schwartz L. Shoulder impingement presenting as neck pain. J Bone Joint Surg Am 2003;85:635–8 [DOI] [PubMed] [Google Scholar]