Abstract
Background:
The exploitation and utilization of vast varieties of herbal extracts may serve as alternative measures to deter aggregation of deoxygenated sickle cell hemoglobin (deoxyHbS) molecules.
Objective:
The present in vitro study ascertained the capacity of three medicinal plants, namely, Anacardium occidentale, Psidium guajava, and Terminalia catappa, to alter polymerization of HbS.
Materials and Methods:
Spectrophotometric method was used to monitor the level of polymerization of hemolysate HbS molecules treated with sodium metabisulfite (Na2 S2 O5) at a regular interval of 30 s for a period of 180 s in the presence of separate aqueous extracts of A. occidentale, P. guajava, and T. catappa. At time intervals of 30 s, the level of polymerization was expressed as percentage of absorbance relative to the control sample at the 180th s.
Results:
Although extracts of the three medicinal plants caused significant (P < 0.05) reduction in polymerization of deoxyHbS molecules, the corresponding capacity in this regard diminished with increase in incubation time. Aqueous extract of P. guajava exhibited the highest capacity to reduced polymerization of deoxyHbS molecules. Whereas at t > 60 s, extract concentration of 400 mg% of A. occidentale activated polymerization of deoxyHbS molecules by 6.23±1.34, 14.53±1.67, 21.15±1.89, and 24.42±1.09%, 800 mg% of T. catappa at t > 30 s gave values of 2.50±1.93, 5.09±1.96, 10.00±0.99, 15.38±1.33, and 17.31±0.97%.
Conclusion:
The capacity of the three medicinal plants to interfere with polymerization of deoxyHbS molecules depended on the duration of incubation and concentration of the extracts.
Keywords: A. occidentale, DeoxyHbS, Polymerization, P. guajava, T. catappa
INTRODUCTION
Cashew (Anacardium occidentale) is a multipurpose tree of the Amazon and African rainforest that grows up to 15 m high. It has a thick and tortuous trunk with branches so winding that they frequently reach the ground. The cashew fruit is a rich source of vitamins, minerals, and other essential nutrients.[1] Volatile compounds present in the fruit include esters, terpenes, and carboxylic acids.[2] The bark and leaves of cashew are a rich source of tannins, a group of plant chemicals with documented biological activity.[3] The bark, leaves, and shell oil around the nut are used medicinally as anti-inflammatory[3] and astringent preparations, which may be why cashew is effective in treating diarrhea.[4] Several clinical studies have shown that these biochemicals curb the darkening effect of aging by inhibiting tyrosinase activity,[5] protective against laboratory-induced diabetes,[6,7] treatment of leishmanial ulcers due to Leishmania (Viannia)[8] and are toxic to certain cancer cells.[1] Antimicrobial properties of A. occidentale against E. coli,[4,9] Pseudomonas,[4] and Helicobacter pylori considered to cause acute gastritis and stomach ulcers have been reported.[10]
Guava (Psidium guajava) is a tropical and semi-tropical plant. The branches are crooked, causing opposite leaves to overlap. The flowers are white, incurved petals, 2 or 3 in the leaf axils. The fruit is small, 3–6 cm long, pear-shaped, reddish-yellow when ripe.[11] Lectin chemicals in leaves of P. guajava have been shown to bind to E. coli,[12] preventing its adhesion to the intestinal wall and thus preventing infection.[13] P. guajava fruit intake decreases blood pressure and serum high-density lipoprotein/cholesterol levels.[14,15] The leaves of the guava tree in decoction are recommended for gastroenteritis,[16] ulcers, vaginal and uterine problems, and where an astringent remedy is needed.[1] Also, it has been used for spasms,[17] fevers, worm infections, kidney dysfunctions, epilepsy, diabetes, and cerebral infections.[1]
Indian almond (Terminalia catappa) tree can reach a height of 35 m (110 ft). It grows upright and forms a symmetrical crown with horizontal branches distinctively arranged in tiers. As the tree ages, the crown will become increasingly flattened and eventually take on a vase shape.[18] Indian almond leaves contain several different flavonoids, including kaempferol and quercetin.[19] Flavonoids have been shown to possess a range of biological activities that are consistent with them contributing to the protection against degenerative diseases, such as cancer, diabetes, cardiovascular diseases, and cataract.[20–22] It is also rich in various tannins; astringent, bitter plant polyphenols that either bind and precipitate or denature protein molecules.[19] While the juice of the leaves is used as a folk remedy against various ailments that damage the skin, such as scabies and leprosy, the leaves themselves are used to dress rheumatic joints.[23] The young leaves are ingested by people suffering from intestinal parasites, dysentery, and are believed to help get rid of colic in babies.[24]
The sickle cell hemoglobin (HbS) is a product of a defective genetic code of hemoglobin molecule.[25] The HbS molecule is prone to deoxygenation-induced polymerization and exhibits a relatively low insolubility. The reason for this phenomenon is the consequence of substitution on the beta (β) chain of HbS molecule, a polar glutamic acid residue with nonpolar valine molecule, thereby generating a sticky patch.[26,27] Specifically, only this one β6Glu→Val residue of each tetramer resides in an intermolecular contact region for deoxyHbS aggregation. The hydrophobic valine side chain appears to fit into a hydrophobic pocket formed by β88 leucine and β85 phenylalanine residues on an adjacent hemoglobin molecule.[28] The normal glutamic acid would not easily fit into this pocket explaining at least part of why deoxyHbS does not polymerize. The model described in sequential steps includes nucleation, growth, and subsequent alignment of the molecule into microfibrils parallel to each other with the resultant membrane deformity and damage.[29,30] Characteristically, the red cells’ normal biconcave disc appearance is distorted to a spiculated sickle shape. This aberrant cell distortion accounts for the pathophysiology in this disease, namely, hemolytic anemia, vascular stasis, occlusion, and thrombosis.
The development of chemical modification agents that reduce the tendency of deoxyHbS to aggregate representsan important chemotherapeutic goal. Whereas hemoglobin carbamylation by cyanate[31,32] is a potentially effective antisickling agent, methyl acetylphosphate (MAP)has been reported to bind to the 2,3-diphosphoglycerate (2,3-DPG)binding site of hemoglobin, where it selectively acetylates residues,resulting in increased solubility of deoxyHbS molecules.[33] In vitro studies by Abdulmalik et al[34] reported that 5-hydroxymethyl-2-furfural (5HMF) forms a high-affinity Schiff-base adduct with HbS molecules and inhibits red cell sickling. Hydroxyurea[35] and 2-imidazolines[36] are among the few developed antisickling agents, which interfere and disrupt the contact point that promotes aggregation of deoxyHbS molecules.
However, limitations of these antisickling agents are undesirable structural andfunctional changes of hemoglobin as well as toxicity resulting from modifications of other protein molecules.[25,31–33] The exploitation and utilization of vast varieties of herbal extracts may serve as alternative measures to deter aggregation of deoxyHbS molecules. Moreover, the specimens are commonly consumed plant materials and pose little or no toxic effects. Therefore, the present study seeks to ascertain the capacity of three medicinal plants (A. occidentale, P. guajava, and T. catappa) to interfere with polymerization of HbS molecules.
MATERIALS AND METHODS
Collection of plant specimens
Fresh samples of A. occidentale, P. guajava, and T. catappa leaves were harvested between July and August 2010, from trees within the environment of Imo State University, Owerri, Nigeria. The plant specimens were identified and authenticated by Dr. F. N. Mbagwu at the Herbarium in the Department of Plant Science and Biotechnology. A voucher specimen was deposited at the Herbarium for reference purposes.
Preparation of aqueous extract of plant specimen
The samples were washed under continuous current of distilled water for 15 min and air dried at room temperature for 60 min. The separate leaves were dried for 5 h in an oven at 60°C to become crispy, and ground with ceramic mortar and pestle. Two grams (2 g) each, of the pulverized specimen was suspended in 100 mL of distilled water and allowed to stand for 6 h at 37°C. The aqueous extracts (2 g%) of A. occidentale, P. guajava, and T. catappa leaves were obtained by filteration with Whatman No. 2 filter paper. The prepared extracts were kept at 4°C in a refrigerator for at least 24 h before subsequent tests. Serial dilutions of the aqueous extracts in the order of 200, 400, 600, and 800 mg% were used for polymerization analyses.
Collection of blood samples/preparation of erythrocyte hemolysate
Five milliliters (5.0 mL) of human venous blood samples of HbSS genotype were collected by venipuncture and stored in EDTA anticoagulant tubes. The blood samples were obtained between July and August 2010, from 9 male volunteers (59-79 kg) in the age group of 21–34 years attending clinics at the Federal Medical Center (FMC), Imo State University Teaching Hospital (IMSUTH), Orlu, St. John Clinic/Medical Diagnostic Laboratories, Avigram Medical Diagnostic Laboratories, and Qualitech Medical Diagnostic Laboratories. These centers are located in Owerri, Imo State, Nigeria. The Institutional Review Board of the Department of Biochemistry, Imo State University, Owerri, Nigeria, granted approval for this study and all volunteers involved signed an informed consent form. This study was in accordance with the ethical principles that have their origins in the Declaration of Helsinki.
The erythrocytes were washed by centrifugation methods as described by Tsakiris et al.[37] Within 2 h of collection of blood samples, portions of 1.0 mL of the samples were introduced into centrifuge test tubes containing 3.0 mL of buffer solution pH = 7.4: 250 mM tris (hydroxyl methyl) amino ethane-HCl (Tris-HCl)/140 mM NaCl/1.0 mM MgCl2/10 mM glucose). The erythrocytes were separated from plasma by centrifugation at 1200g for 10 min, washed 3 times by the same centrifugation method with the buffer solution. The erythrocytes were finally resuspended in 1.0 mL of this buffer and stored at 4°C. The washed erythrocytes were lysed by freezing/thawing as described by Galbraith and Watts,[38] and Kamber et al.[39] The erythrocyte hemolysate was used for polymerization analyses.
Polymerization studies
Sodium metabisulfite {Na2 S2 O5; (BDH, UK)}-induced polymerization of HbS molecules was ascertained as described previously by Iwu et al[40] with minor modification according to Chikezie et al.[41] The underlying principle is that HbS molecules undergo gelation when deprived of oxygen; Na2S2O3 was used as a reductant. The level of polymerization was monitored by recording increasing absorbance of the assay mixture with time. A 0.1 mL of HbS hemolysate was introduced into a test tube, followed by 0.5 mL of phosphate-buffered saline solution (PBS, 9 g NaCl, 1.71 g Na2HPO4.2H2O, 2.43 g NaH2PO4.2H2PO4.2H2O per liter of distilled water, pH = 7.4) and 1.0 mL of distilled water. The mixture was transferred into a cuvette and 3.4 mL of 2 g% aqueous solution of Na2S2O5 was added. The absorbance of the assay mixture was recorded with a spectrophotometer (SPECTRONIC 20, Labtech—Digital Blood Analyzer®) at every 30 s for 180 s at λmax = 700 nm (control sample). This procedure was repeated by substituting the distilled water with 1.0 mL of corresponding four increasing concentrations of the separate extracts (test sample).
Where
At/c =Absorbance of test/control sample at time = t s.
Ac180th s = Absorbance of control sample at the 180th s.
Statistical analyses
The results were expressed in terms of arithmetic means (X) ± standard deviation (SD). The statistical significance of the difference between the means was evaluated by Student’s t test.[42]
RESULTS
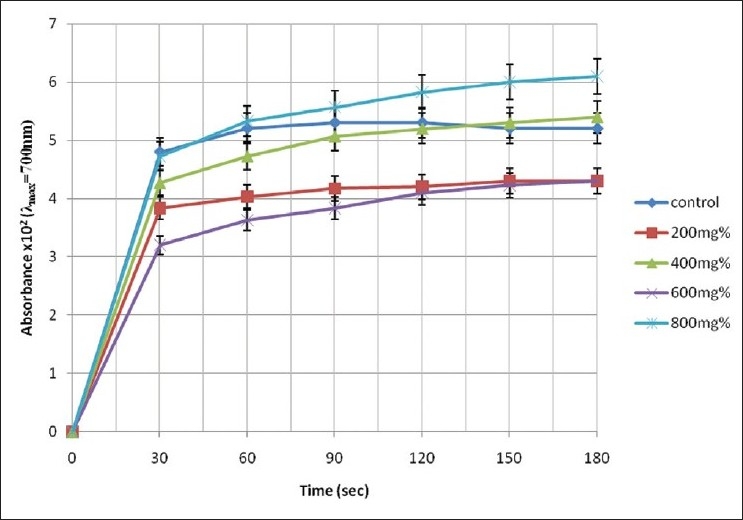
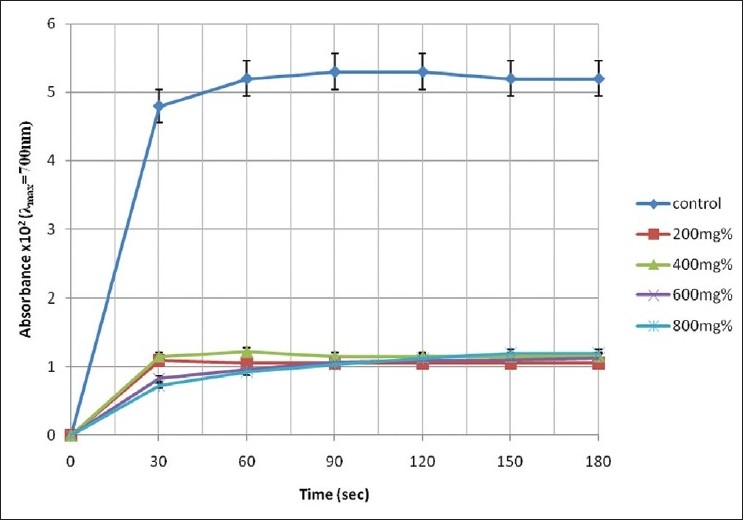
The pattern of increase in absorbance of the assay mixture with experimental time is illustrated in Figures 1–3.
Figure 1.
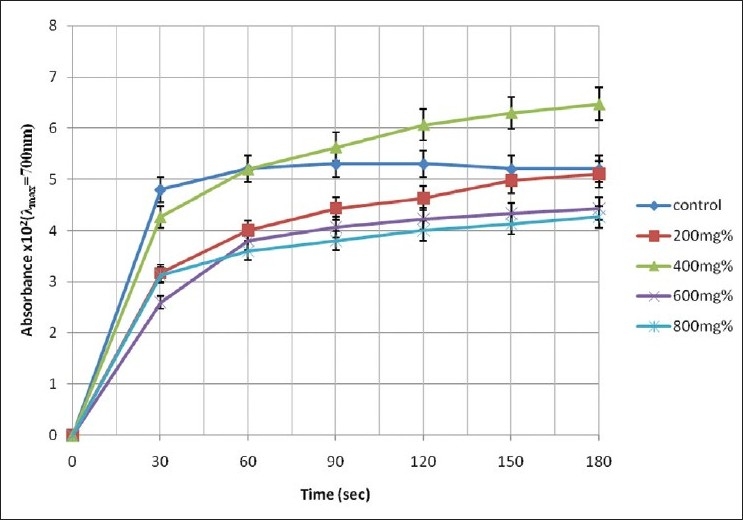
Change in absorbance of erythrocyte haemolysate of HbSS genotype in the presence of aqueous extract of A. occidentale
Figure 3.
Change in absorbance of erythrocyte haemolysate of HbSS genotype in the presence of aqueous extract of T. catappa
A cursory look at Figures 1–3 shows that the rate of increase in absorbance was more rapid within the time range of 0 < t < 30 s than subsequent time intervals. The control sample gave absorbance of 0.052 ± 0.05 units at t = 180 s representing 100% polymerization of deoxyHbS molecules. However, the test sample containing 400 mg% of A. occidentale gave a maximum absorbance of 0.0647 ± 0.004 units at the 180th s (polymerization = 126.86%). Furthermore, Figure 2 shows that the test sample containing 800 mg% of P. guajava exhibited the lowest absorbance value of 0/0073 ± 0.01 units at t = 30 s corresponding to 14.31 ± 2.11% polymerization [Table 1].
Figure 2.
Change in absorbance of erythrocyte haemolysate of HbSS genotype in the presence of aqueous extract of P. guajava
Table 1.
Comparative levels of polymerization of deoxyHbS (t = 180th s) in the presence of aqueous extracts of Anacardium occidentale, Psidium guajava, and Terminalia catappa
| Time (s) | Polymerization (%) |
||||||
|---|---|---|---|---|---|---|---|
| 0 | 30 | 60 | 90 | 120 | 150 | 180 | |
| Control (n = 9) | 0.00 ± 0.00 | 93.53 ± 1.06 | 100.00 ± 1.14 | 101.96 ± 1.13 | 101.96 ± 2.14 | 101.37 ± 1.02 | 100.00 ± 0.65 |
| [A. occidentale]; n = 9 | |||||||
| 200 mg% | 0.00 ± 0.00 | 62.16 ± 1.03 | 78.43 ± 1.02 | 86.86 ± 1.13 | 90.78 ± 0.95 | 97.45 ± 0.99 | 100.00 ± 1.33 |
| 400 mg% | 0.00 ± 0.00 | 83.73 ± 0.97 | 101.96 ± 1.00 | 110.39 ± 0.95 | 119.65 ± 1.07 | 123.53 ± 0.56 | 126.86 ± 1.78 |
| 600 mg% | 0.00 ± 0.00 | 50.98 ± 1.06 | 74.51 ± 0.98 | 79.98 ± 0.99 | 82.94 ± 0.56 | 84.90 ± 1.22 | 86.86 ± 1.11 |
| 800 mg% | 0.00 ± 0.00 | 61.37 ± 0.96 | 70.59 ± 1.00 | 74.51 ± 1.66 | 78.43 ± 1.88 | 80.98 ± 0.96 | 83.73 ± 1.33 |
| [P. guajava]; n = 9 | |||||||
| 200 mg% | 0.00 ± 0.00 | 21.37 ± 1.34 | 20.59 ± 2.32 | 20.59 ± 2.11 | 20.61 ± 1.88 | 20.62 ± 2.00 | 20.63 ± 2.22 |
| 400 mg% | 0.00 ± 0.00 | 22.55 ± 0.77 | 23.92 ± 0.99 | 22.55 ± 1.23 | 22.56 ± 1.34 | 22.57 ± 1.77 | 22.55 ± 1.00 |
| 600 mg% | 0.00 ± 0.00 | 16.27 ± 0.88 | 19.02 ± 1.54 | 20.98 ± 1.43 | 21.57 ± 0.97 | 21.76 ± 0.98 | 22.16 ± 1.34 |
| 800 mg% | 0.00 ± 0.00 | 14.31 ± 2.11 | 18.24 ± 1.78 | 20.20 ± 1.56 | 22.16 ± 2.00 | 23.53 ± 1.32 | 23.53 ± 1.43 |
| [T. catappa]; n = 9 | |||||||
| 200 mg% | 0.00 ± 0.00 | 75.10 ± 1.34 | 79.02 ± 2.34 | 81.76 ± 2.43 | 82.35 ± 1.09 | 84.31 ± 1.22 | 84.31 ± 1.89 |
| 400 mg% | 0.00 ± 0.00 | 83.73 ± 1.43 | 92.75 ± 1.54 | 94.41 ± 1.43 | 101.96 ± 1.32 | 103.92 ± 0.97 | 105.88 ± 0.76 |
| 600 mg% | 0.00 ± 0.00 | 62.75 ± 1.90 | 71.18 ± 1.43 | 75.10 ± 1.09 | 80.39 ± 0.98 | 82.94 ± 0.89 | 84.31 ± 1.00 |
| 800 mg% | 0.00 ± 0.00 | 92.75 ± 1.23 | 104.51 ± 0.85 | 109.22 ± 1.33 | 114.31 ± 1.11 | 117.64 ± 1.37 | 119.61 ± 1.20 |
The results are means (X) ± SD of nine (n = 9) determinations
The levels of polymerization of deoxyHbS at specific time intervals compared with the control sample at the 180th s are presented in Table 1. In the control sample, although the levels of polymerization of deoxyHbS molecules were higher at t = 90, 120, and 150 s, they were not significantly different when compared with the value at t = 180 s (P < 0.05). Addition of 200, 600, and 800 mg% aqueous extracts of A. occidentale to the assay mixture caused reduction of deoxyHbS polymerization within the experimental period (t = 0–180 s). However, the capacity of the three mentioned concentrations of A. occidentale to inhibit polymerization of deoxyHbS molecules diminished as the experimental time progressed. Specifically, Table 2 shows that in the presence of extract concentrations of 200, 600, and 800 mg%, the capacity of A. occidentale to inhibit deoxyHbS polymerization fell within the ranges of 33.96%-1.92%, 45.83%-14.81%, and 34.79%-17.88%, respectively. Extract concentration of 400 mg% of A. occidentale caused reduction in polymerization of deoxyHbS molecules at t = 30 s; representing 11.04% ± 1.43% inhibition [Table 2]. Paradoxically, further increases in incubation time engendered activation of deoxyHbS polymerization above the control/reference values (t = 180 s; 100% polymerization; Table 2). Furthermore, Table 2 shows at every time interval of 30 s, within the values of t > 60 s, the levels of activation gave 6.23% ± 1.34%, 14.53% ± 1.67%, 21.15% ± 1.89%, and 24.42% ± 1.09%.
Table 2.
Relative levels of inhibition/activation of deoxyHbS polymerization (t = 30 s intervals) in the presence of aqueous extracts of Anacardium occidentale, Psidium guajava, and Terminalia catappa
| Time (s) | Polymerization inhibition/activation (%) |
|||||
|---|---|---|---|---|---|---|
| 30 | 60 | 90 | 120 | 150 | 180 | |
| [A. occidentale]; n = 9 | ||||||
| 200 mg% | 33.96 ± 1.54 | 23.08 ± 1.09 | 16.42 ± 0.98 | 12.64 ± 1.34 | 4.42 ± 1.11 | 1.92 ± 1.87 |
| 400 mg% | 11.04 ± 1.43 | 0.01 ± 0.11 | 6.23* ± 1.34 | 14.53* ± 1.67 | 21.15* ± 1.89 | 24.42* ± 1.09 |
| 600 mg% | 45.83 ± 1.34 | 26.92 ± 1.76 | 23.21 ± 1.09 | 20.19 ± 1.12 | 16.73 ± 1.66 | 14.81 ± 2.09 |
| 800 mg% | 34.79 ± 1.32 | 30.77 ± 0.99 | 28.30 ± 0.67 | 24.53 ± 0.89 | 20.58 ± 1.67 | 17.88 ± 1.77 |
| [P. guajava]; n = 9 | ||||||
| 200 mg% | 77.29 ± 1.01 | 79.81 ± 1.34 | 80.19 ± 1.78 | 80.17 ± 1.99 | 79.78 ± 1.00 | 79.77 ± 1.37 |
| 400 mg% | 76.04 ± 1.43 | 76.54 ± 1.32 | 78.30 ± 1.11 | 78.29 ± 1.09 | 77.86 ± 1.28 | 77.88 ± 0.99 |
| 600 mg% | 82.71 ± 1.00 | 81.35 ± 1.95 | 79.81 ± 1.45 | 79.25 ± 0.90 | 78.65 ± 0.69 | 78.27 ± 1.56 |
| 800 mg% | 84.79 ± 1.99 | 82.12 ± 1.98 | 80.57 ± 0.67 | 78.68 ± 1.07 | 76.92 ± 0.97 | 76.92 ± 1.43 |
| [T. catappa]; n = 9 | ||||||
| 200 mg% | 20.21 ± 1.77 | 22.50 ± 1.27 | 21.32 ± 1.34 | 20.75 ± 2.04 | 17.31 ± 1.09 | 17.31 ± 1.04 |
| 400 mg% | 11.04 ± 1.54 | 9.04 ± 1.00 | 4.34 ± 1.71 | 1.89 ± 1.90 | 1.89* ± 1.00 | 3.85 ± 1.43 |
| 600 mg% | 37.47 ± 1.48 | 30.19 ± 1.00 | 27.74 ± 1.07 | 22.64 ± 1.45 | 18.65 ± 1.04 | 17.31 ± 1.07 |
| 800 mg% | 1.46 ± 1.66 | 2.50* ± 1.93 | 5.09* ± 1.96 | 10.00* ± 0.99 | 15.38* ± 1.33 | 17.31* ± 0.97 |
The results are means (X) ± S.D of nine (n = 9) determinations
Activation (%)
The four concentrations of P. guajava reduced polymerization of deoxyHbS molecules throughout the experimental time [Table 1]. Specifically, aqueous concentration of 800 mg% caused maximum inhibition of 84.79% at the 30th s [Table 2], which corresponded to 14.31% polymerization compared with the control sample at t = 180 s [Table 1]. Generally, between t = 30-180 s, whereas the diminishing capacity of P. guajava extract to inhibit polymerization of deoxyHbS molecules were as follows: 600 mg% (4.44%) and 800 mg% (7.87%), inhibition was sustained and increased by 200 mg% (2.48%) and 400 mg% (1.84%).
Although 800 mg% extract concentration of T. catappa hindered polymerization of deoxyHbS by 1.46% at t = 30 s, further increases in experimental time (t > 60 s), engendered activation of the polymerization process. The levels of polymerization were 2.50%, 5.09%, 10.00%, 15.38%, and 17.31% greater than the control sample at corresponding time intervals of 30 s [Table 2]. Also, between the 150th and 180th s, extract concentration of 400 mg% caused activation of polymerization of deoxyHbS molecules by 1.89% and 3.85%, respectively [Table 2]. The maximum capacity of aqueous extract of T. catappa to inhibit polymerization of deoxyHbS molecules occurred at t = 30 s, in the presence of extract concentration of 600 mg%. However, the level of inhibition attenuated as experimental time progressed.
DISCUSSION
Noteworthy, polymerization of deoxyHbS is dependent on physiologic concentration of 2,3-DPG.[43] However, according to Ferrone et al,[44] 2,3-DPG contributes only a minor effect in predicting intracellular polymer formation. Therefore, in this study, the interplay of physiologic concentration of 2,3-DPG on HbS polymerization was neglected.
An overview of the present study showed increasing level of polymerization of deoxyHbS molecules with time that is consistent with the pattern described elsewhere.[41,45,46] In vitro deoxygenation of hemolysate HbS molecules by sodium metabisulfite caused progressive aggregation and polymerization of the individual hemoglobin molecules. The process of gelation (polymerization) of hemoglobin molecules resulted in increasing absorbance of the assay solution with time.
Although after 60 s, extract concentrations of 400 mg% of A. occidentale and 800 mg% of T. catappa activated polymerization of deoxyHbS molecules, the present study showed that aqueous extracts of the three medicinal plants (A. occidentale, P. guajava, and T. catappa) exhibited variable capacity to hinder polymerization of deoxyHbS molecules. In conformity with earlier reports of Oyewole et al,[47] a measure of inhibition of deoxyHbS polymerization by these extracts was found to be dose and time dependent. Previous reports have proposed the use of herbal preparations as candidate for management of sickle cell disease.[46–52] Their proposals were drawn from the fact that these plant extracts, from in vitro studies, exhibited antisickling/polymerization property. The findings of this research are comparable to those previous reports. Research findings have established that the capability of a biomolecule to impede in vitro polymerization depends on one or combinations of the following options.
The tendency and efficiency to bind to the complimentary contact region/site of deoxyHbS monomers.[34–36]
Modification of amino acid residues that contribute to the three-dimensional structures of HbS contact region and other critical sites.[32,33,47]
Stabilization of the R (relaxed) state of HbS molecule.[32,47,53,54]
The diminishing capacity of the three plant extracts to inhibit polymerization of deoxyHbS molecule with progression of experimental time suggest that the constituents of the extracts did not covalently modify the amino acid residues unlike other reported compounds.[25,31–36] Rather, the antipolymerization principles of the plant extracts may have formed a relatively weaker hydrophobic interactions with the contact regions of HbS molecules that temporarily reduced polymerization of HbS monomers. Furthermore, the protein/ligand associations may have transiently stabilized the R-state conformation, but were subsequently displaced by more thermodynamically favorable interactions that engendered and promoted hemoglobin polymerization. Therefore, the capacity of the three extracts to inhibit HbS polymerization was not sustained with the progress of experimental time.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Taylor L. The Healing Power of Rainforest Herbs. 2005. Available from: http://www.rain-tree.com/book2.htm. [retrieved on 2010 Aug 16]
- 2.Bicalho B, Rezende CM. Volatile compounds of cashew apple (Anacardium occidentale L.) Z. Naturforsch. 2001;56:35–9. doi: 10.1515/znc-2001-1-206. [DOI] [PubMed] [Google Scholar]
- 3.Mota ML, Thomas G, Barbosa-filho JM. Anti-inflammatory actions of tannins isolated from the bark of Anacardium occidentale L. J Ethnopharmacol. 1985;13:289–300. doi: 10.1016/0378-8741(85)90074-1. [DOI] [PubMed] [Google Scholar]
- 4.Kudi AC, Umoh JU, Eduvic LO, Getu J. Screening of some Nigerian medicinal plants for antibacterial activity. J Ethanopharm. 1999;67:225–8. doi: 10.1016/s0378-8741(98)00214-1. [DOI] [PubMed] [Google Scholar]
- 5.Kubo I, Kinst-Hori I, Yokokawa Y. Tyrosinase inhibitors from Anacardium occidentale fruits. J Nat Prod. 1994;57:545–51. doi: 10.1021/np50106a021. [DOI] [PubMed] [Google Scholar]
- 6.Swanston-Flatt SK, Day C, Flatt PR, Gould BJ, Bailey CJ. Glycaemic effects of traditional European plant treatments for diabetes.Studies in normal and streptozotocin diabetic mice. Diabetes Res. 1989;10:69–73. [PubMed] [Google Scholar]
- 7.Kamtchouing P, Sokeng SD, Moundipa PF, Watcho P, Jatsa HB, Lontsi D. Protective role of Anacardium occidentale extract against streptozotocin-induced diabetes in rats. J Ethnopharmacol. 1998;62:95–9. doi: 10.1016/s0378-8741(97)00159-1. [DOI] [PubMed] [Google Scholar]
- 8.Franca F. Plants used in the treatment of leishmanial ulcers due to Leishmania (Viannia) braziliensis in an endemic area of Bahia, Brazil. Rev Soc Bras Med Trop. 1996;29:229–32. doi: 10.1590/s0037-86821996000300002. [DOI] [PubMed] [Google Scholar]
- 9.Akinpelu DA. Antimicrobial activity of Anacardium occidentale bark. Filoterapia. 2001;72:286–7. doi: 10.1016/s0367-326x(00)00310-5. [DOI] [PubMed] [Google Scholar]
- 10.Ofusori D, Enaibe B, Adelakun A, Adesanya O, Ude R, Oluyemi K, et al. Microstructural studies of the effect of ethanolic extract of cashew stem bark Anacardium occidentale on the brain and kidney of swiss albino mice. Int J Alter Med. 2008;5:2. [Google Scholar]
- 11.Smith NJH, Williams JT, Plucknett DL, Talbot JP. Tropical Forests and Their Crops. London: Cornell University Press; 1992. [Google Scholar]
- 12.Coutino-Rodriguez R, Hernandez-Cruz P, Giles-Rios H. Lectins in fruits having gastrointestinal activity: Their participation in the hemagglutinating property of Escherichia coli O157:H7. Arch Med Res. 2001;32:251–7. doi: 10.1016/s0188-4409(01)00287-9. [DOI] [PubMed] [Google Scholar]
- 13.Lozoya X, Becerril G, Martínez M. Model of intraluminal perfusion of the guinea pig ileum in vitro in the study of the antidiarrheal properties of the guava (Psidium guajava) Arch Invest Med (Mex) 1990;21:155–62. [PubMed] [Google Scholar]
- 14.Singh RB, Rastogi SS, Singh NK, Ghosh S, Niaz MA. Effects of guava intake on serum total and high-density lipoprotein cholesterol levels and on systemic blood pressure. Am J Cardiol. 1992;70:1287–91. doi: 10.1016/0002-9149(92)90763-o. [DOI] [PubMed] [Google Scholar]
- 15.Singh RB, Rastogi SS, Singh NK, Ghosh S, Gupta S, Niaz MA. Can guava fruit intake decrease blood pressure and blood lipids? J Hum Hypertens. 1993;7:33–8. [PubMed] [Google Scholar]
- 16.Tona L, Kambu K, Mesia K, Cimanga K, Apers S, de Bruyne T, et al. Biological screening of traditional preparations from some medicinal plants used as antidiarrhoeal in Kinshasa, Congo. Phytomed. 1999;6:59–66. doi: 10.1016/S0944-7113(99)80036-1. [DOI] [PubMed] [Google Scholar]
- 17.Morales MA, Tortoriello J, Meckes M, Paz D, Lozoya X. Calcium-antagonist effect of quercetin and its relation with the spasmolytic properties of Psidium guajava L. Arch Med Res. 1994;25:17–21. [PubMed] [Google Scholar]
- 18.Corner EJ. Wayside Trees of Malaya. The Malayan Nature Society. (4th ed) 1997;Vol 1 [Google Scholar]
- 19.Indian Almond and Folk Medicine. Available from: http://www.romow.com/health-blog/indian-almond-and-folk-medicine/. [retrieved on 2010 Aug]
- 20.Block G, Patterson B, Subar A. vegetables and cancer prevention: A review of the epidemiological evidence. Nutr Cancer. 1992;18:1–29. doi: 10.1080/01635589209514201. [DOI] [PubMed] [Google Scholar]
- 21.Steinmetz KA, Potter JD. Vegetables, fruit, and cancer prevention: A review. J Am Diet Assoc. 1996;96:1027–39. doi: 10.1016/S0002-8223(96)00273-8. [DOI] [PubMed] [Google Scholar]
- 22.Knekt P, Kumpulainen J, Jarvinen R, Rissanen H, Heliovaara M, Reunanen A, et al. Flavonoid intake and risk of chronic diseases. Am J Clin Nutr. 2002;76:560–8. doi: 10.1093/ajcn/76.3.560. [DOI] [PubMed] [Google Scholar]
- 23.Indian Almond Leaves. Available from: www.indianalmondleaves.com/. [retrieved on 2010 Aug]
- 24.Tan R. Sea Almond Tree. Available from: http://tothefishcom/Aquarium-for-sale/indian-almond-leaves 2001 [retrieved on 2010 Aug]
- 25.Mehanna AS. Sickle cell anemia and antisickling agents then and now. Curr Med Chem. 2001;8:79–88. doi: 10.2174/0929867013373778. [DOI] [PubMed] [Google Scholar]
- 26.Martin DW. Structure and function of a protein - haemoglobin. In: Martin DW, Mayes PA, Rodwell VW, editors. Harper’s Review of Biochemistry. 9th ed. California:Lange: Medical Publications; 1983. [Google Scholar]
- 27.Bindon J. Natural selection and adaptation: Sickle cell. Available from: http://www.as.ua.edu/ant/bindon/ant475/Sicklecell/Sicklecell.pdf [retrieved on 2007 Feb 11]
- 28.Ivanova M, Jasuja R, Kwong S, Briehl RW, Ferrone FA. Nonideality and the nucleation of sickle hemoglobin. Biophys J. 2000;79:1016–22. doi: 10.1016/S0006-3495(00)76355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ferrone FA, Rotter MA. Crowding and the polymerization of sickle hemoglobin. J Mol Recognit. 2004;17:497–504. doi: 10.1002/jmr.698. [DOI] [PubMed] [Google Scholar]
- 30.Rotter MA, Kwong S, Briehl RW, Ferrone FA. Heterogeneous nucleation in sickle hemoglobin: Experimental validation of a structural mechanism. Biophys J. 2005;89:2677–84. doi: 10.1529/biophysj.105.067785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jensen M, Bunn HF, Halikas G, Kan YW, Nathan DG. Effects of cyanate and 2, 3-diphosphoglycerate on sickling relationship to oxygenation. J Clin Invest. 1973;52:2542–7. doi: 10.1172/JCI107445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manning JM, Acharya AS. The mechanism of action of two anti-sickling agents: Sodium cyanate and glyceraldehyde. Am J Pediatr Hematol Oncol. 1984;6:51–4. [PubMed] [Google Scholar]
- 33.Xu ASL, Labotka RJ, London RE. Acetylation of human hemoglobin by methyl acetylphosphate: Evidence of broad regio-selectivity revealed by NMR studies. J Biol Chem. 1999;274:26629–32. doi: 10.1074/jbc.274.38.26629. [DOI] [PubMed] [Google Scholar]
- 34.Abdulmalik O, Safo MK, Chen Q, Yang J, Brugnara C, Ohene-Frempong K, et al. 5-hydroxymethyl-2-furfural modifies intracellular sickle haemoglobin and inhibits sickling red blood cells. Br J Haematol. 2005;128:552–61. doi: 10.1111/j.1365-2141.2004.05332.x. [DOI] [PubMed] [Google Scholar]
- 35.Charache S, Terrin M, Moore R, Dover G, Barton F, Eckert S, et al. The effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. N Engl J Med. 1995;332:1317–22. doi: 10.1056/NEJM199505183322001. [DOI] [PubMed] [Google Scholar]
- 36.Chang H, Ewert SM, Nagel RL. Identification of 2-imidazolines as anti-sickling agents. Am Soc Pharmacol Exp Therap. 1983;23:731–4. [PubMed] [Google Scholar]
- 37.Tsakiris S, Giannoulia-Karantana A, Simintzi I, Schulpis KH. The effect of aspartame metabolites on human erythrocyte membrane acetylcholinesterase activity. Pharmacol Res. 2005;53:1–5. doi: 10.1016/j.phrs.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 38.Galbraith DA, Watts DC. Changes in some cytoplasmic enzymes from red cells fractionated into age groups by centrifugation in Ficoll™/Triosil™ gradients: Comparison of normal human and patients with Duchenne muscular dystrophy. Biochem J. 1980;191:63–70. doi: 10.1042/bj1910063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kamber K, Poyiagi A, Delikonstantinos G. Modifications in the activities of membrane-bound enzymes during in vivo ageing of human and rabbit erythrocytes. Comp Biochem Physiol Br. 1984;77:95–9. doi: 10.1016/0305-0491(84)90228-1. [DOI] [PubMed] [Google Scholar]
- 40.Iwu MN, Igboko AO, Onwubiko H, Ndu UE. Effect of Cajanus cajan on gelation and oxygen affinity of sickle cell hemoglobin. J Ethnopharm. 1988;20:99–104. doi: 10.1016/0378-8741(88)90118-3. [DOI] [PubMed] [Google Scholar]
- 41.Chikezie PC, Chikezie CM, Amaragbulem PI. Effect of antimalarial drugs on polymerization of sickle cell hemoglobin (HbS) Turk J Biochem. 2010;35:41–4. [Google Scholar]
- 42.Saunders BD, Trapp RG. Association and prediction. In: Basic and Clinical Biostatistics. London: Prentice Hall International Inc; 1994. [Google Scholar]
- 43.Noguchi CT, Torchia DA, Schechter AN. Intracellular polymerization of sickle hemoglobin effects of cell heterogeneity. J Clin Invest. 1983;72:846–52. doi: 10.1172/JCI111055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nwaoguikpe RN, Uwakwe AA. The antisickling effects of dried fish (tilapia) and dried prawn (Astacus red) J Appl Sci Environ Mgt. 2005;9:115–9. [Google Scholar]
- 45.Ferrone F, Hofrichter AJ, Sunshine HR, Eaton WA. Kinetic studies on photolysis-induced gelation of sickle cell hemoglobin suggest a new mechanism. Biophys J. 1980;32:361–80. doi: 10.1016/S0006-3495(80)84962-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chikezie PC. Studies on the anti-sickling effect of Azadirachta indica and Veronica amygdalina on HbSS erythrocytes. Inter J Nat Appl Sci. 2006;2:24–8. [Google Scholar]
- 47.Oyewole OI, Malomo SO, Adebayo JO. Comparative studies on antisickling properties of thiocyanate, tellurite and hydroxyurea. Pak J Med Sci. 2008;24:18–22. [Google Scholar]
- 48.Ekeke GI, Shode FO. The Reversion of Sickled cells by Cajanus cajan. Planta Medica. 1985;6:504–7. [PubMed] [Google Scholar]
- 49.Kade IJ, Kotila OO, Ayeleso AO, Olaleye AA, Olawoye TL. Antisickling properties of Parquetina nigrescens. Biomed Res (Alligarh) 2003;14:185–8. [Google Scholar]
- 50.Okpuzor J, Adebesin O, Ogbunugafor H, Amadi I. The potential of medicinal plants in sickle cell disease control: A review. Inter J Biomed Health Sci. 2008;4:47–55. [Google Scholar]
- 51.Imaga NO, Gbenle GO, Okochi VI, Akanbi SO, Edeoghon SO, Oigbochie V, et al. Antisickling property of Carica papaya leaf extract. Afr J Biochem Res. 2009;3:102–6. [Google Scholar]
- 52.Imaga NO, Gbenle GO, Okochi VI, Adenekan SO, Edeoghon SO, Kehinde MO, et al. Antisickling and toxicological profiles of leaf and stem of Parquetina nigrescens L. J Med Plant Res. 2010;4:639–43. [Google Scholar]
- 53.Kark JA, Kale MP, Tarassoff PG, Woods M, Lessin LS. Inhibition of erythrocyte sickling in vitro by pyridoxal. J Clin Invest. 1988;62:888–91. doi: 10.1172/JCI109202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stuart J, Mojiminiyi FB, Stone PC, Culliford SJ, Ellory JC. Additive in vitro effects of anti-sickling drugs. Br J Haematol. 1994;86:820–3. doi: 10.1111/j.1365-2141.1994.tb04836.x. [DOI] [PubMed] [Google Scholar]


