Abstract
Objectives
Physicians are seeing increasing numbers of parents who question the safety of vaccines or refuse to vaccinate their children. This study examined how frequently pediatricians in one New England state encounter parental vaccine safety concerns and vaccine refusals, how often physicians dismiss families from their practices for vaccine refusal, and how parental vaccine refusal impacts pediatricians personally.
Methods
The study consisted of a quantitative survey of primary care pediatricians in one New England state; 133 pediatricians completed the questionnaire. Variables examined included number of parental vaccine concerns and refusals seen by each physician, physicians' response to parental vaccine concerns and refusals, the personal impact of parental vaccine safety refusals on pediatricians, and respondent estimates of socioeconomic characteristics of families seen in their practices.
Results
The majority of responding pediatricians reported an increase in parental vaccine safety concerns and refusals. More than 30% of responding pediatricians have dismissed families because of their refusal to immunize. Suburban physicians caring for wealthier, better educated families experience more vaccine concerns and/or refusals and are more likely to dismiss families for vaccine refusal. Vaccine refusals have a negative personal impact on one-third of physician respondents.
Conclusions
Pediatricians in Connecticut are reporting increased levels of parental vaccine safety concerns and refusals. Physicians who report more parental vaccine safety concerns and refusals and who care for wealthier, better educated families are more likely to dismiss families who refuse vaccines and to be negatively affected by parental vaccine refusals, which may adversely impact childhood vaccination rates.
Childhood vaccination is one of the greatest triumphs of public health in the 20th century.1,2 While the incidence of most vaccine-preventable diseases remains at historically low levels in the United States, recent outbreaks of measles, mumps, pertussis, and Haemophilus influenza type B demonstrate the need to maintain high rates of immunization.3–5 Increases in parental vaccine safety concerns and vaccine refusal potentially threaten the gains made over the past century.6,7
Pediatricians are finding themselves increasingly at odds with parents who question the safety of vaccines or refuse vaccines.8,9 The incidence of parental vaccine concerns and/or refusals appears to be increasing.10–12 More than 20% of parents are reported to have significant concerns about the safety of childhood immunizations, and these concerns have been associated with a significant decrease in rates of immunizations in children.13–16 Approximately 15% of underimmunization has been attributed to parental vaccine safety concerns.11,17 Previous studies have suggested that children from white, higher socioeconomic status (SES) families are more likely to be undervaccinated, which is defined as refusing one or more vaccines by choice, while black, poorer children are more likely to be undervaccinated due to other factors.2,5,12
While many studies have examined parental beliefs about vaccine safety concerns and vaccine refusal, few have investigated physicians' experiences and responses to these issues. Physicians may be unwilling or unprepared to discuss vaccine safety issues with parents, and as many as 30% of pediatricians may dismiss families who choose not to vaccinate their children.1,10,18–20 Some primary care providers may have their own concerns about vaccine safety.21 How pediatricians address parental immunization concerns influences parental decisions about vaccinations, as physicians remain one of parents' most trusted sources of information in regard to childhood immunizations.7,9,10,15 The purpose of this study was to examine pediatricians' experience with and response to parental vaccine safety concerns and refusals in one New England state. The study examined rates of vaccine safety concerns, vaccine refusals and dismissal of families in relation to practice setting/type and the SES of families seen, and the personal impact of parental vaccine safety refusals on pediatricians.
METHODS
Participants
Study participants were drawn from the membership of the Hezekiah Beardsley Connecticut Chapter of the American Academy of Pediatrics (AAP) with the organization's permission. Approximately 50% of the 990 members are estimated to be primary care pediatricians currently in practice (Personal communication, Jillian Wood, Executive Director of the Connecticut Chapter of the AAP, December 2007). Participation was voluntary and anonymous.
Surveys were mailed to 600 pediatricians chosen by computer randomization during November and December 2007 and returned by February 2008. Sixteen surveys were returned as undeliverable. Of the remaining 584 surveys, 186 were returned—133 of them by actively practicing primary care pediatricians—for a total response rate of 31.8%. The other 53 surveys were returned by specialists or retired physicians. Only those surveys completed by practicing primary care pediatricians were included in the analysis. Estimating that half, or 292, of the 584 surveys sent to valid addresses were sent to active primary care pediatricians, then the response rate among primary care pediatricians would be estimated to be 45.5%. Using the estimate that one-half of the 990 members of the Connecticut Chapter of the AAP are practicing primary care pediatricians, then 26.9% (133/495) of these primary care pediatricians participated in this survey.
Instrument and procedures
We developed a 28-item questionnaire specifically for this study, drawing variables primarily from two studies: Freed et al. and Flanagan-Klygis and colleagues.8,19 Dr. Freed graciously shared the questionnaire from his study, and we adapted several questions on this study's survey from that questionnaire.8
The variables examined included percentage of pediatricians who experience vaccine safety concerns and vaccine refusals; which vaccines are most likely to be refused by parents; whether pediatricians have seen an increase in parental vaccine safety concerns and refusals; measures taken by the physicians when families refuse vaccines, with particular emphasis on dismissal of families from the practice; and how willing physicians were to discuss these issues with families. Sample questions from the survey included the following:
Over the last year, have you seen a change in the number of vaccine safety concerns and vaccine refusals by parents in your practice compared with five and 10 years ago? (Response choices: many fewer, fewer, no significant change, more, and many more)
What percentage of families with children aged 0–6 years in your practice do you estimate have expressed concerns about vaccine safety in the last year? (Response choices: 0%–5%, 6%–10%, 11%–25%, 26%–50%, and >50%)
How has the issue of vaccine refusal impacted you personally in your practice? (Response choices: little to no impact; positive impact—deepens my relationships with families; mildly annoying—it is part of being a pediatrician; negative impact—increased time and less respect for medical doctors; and has decreased my overall satisfaction with pediatrics)
Other variables included demographics of the pediatricians and practice characteristics such as urban, suburban, or rural location; and group, solo, hospital, or clinic-based practice. Physicians were asked to estimate the family SES and parental education levels that best represented the majority of their patient population, with possible SES choices of poor, working class, middle class, or upper middle class/upper class. The survey instrument was informally pretested by several practicing pediatricians in the New York metropolitan area and revised accordingly.
We mailed the survey and a cover letter with a stamped, addressed return envelope to the 600 randomly selected participants during November and December 2007, with the option of completing the survey on paper or online using SurveyMonkey.com; 6% of respondents completed it online. Reminder cards were sent out one week later. The study received exempt status from the Office of Research Administration of New York Medical College.
Data analysis
We performed data analysis using SPSS® version 11.5.22 We calculated frequencies for all variables in the survey, and performed Chi-square analyses for variables of interest. Where cell size was small (<5), Fisher's exact test was used.
RESULTS
Demographics of physicians, practices, and parents of patients
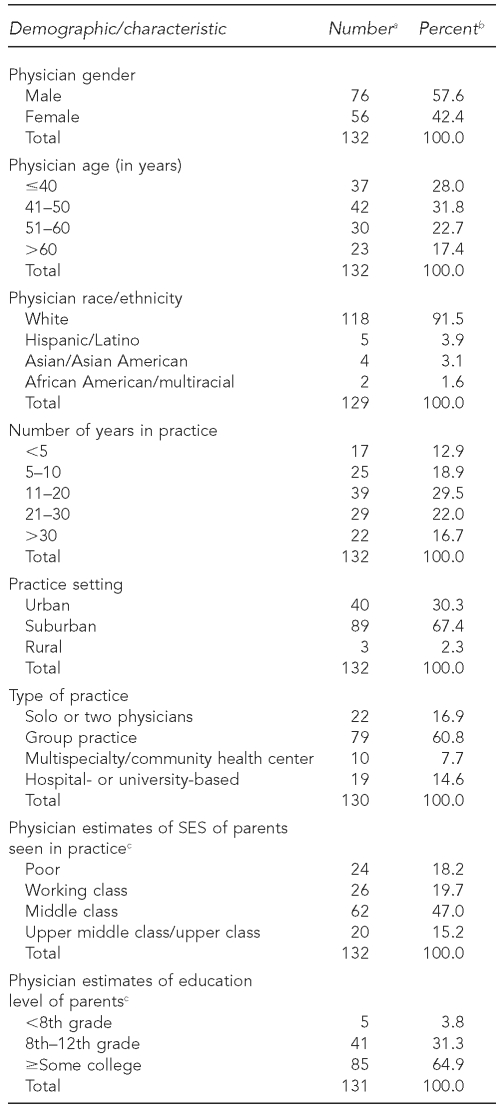
Demographic and practice characteristics of the 133 respondents are shown in Table 1. Suburban/rural practice setting was significantly associated with practice type, parental SES (as estimated by physicians), and parental education level (as estimated by physicians). More than 96% of suburban practices were group or solo practices compared with one-third of urban practices (p<0.001). Suburban practices had significantly higher physician-reported parental SES (82.4% vs. 15.0%, p<0.001) and physician-reported parental education level (81.3% vs. 25.6%, p<0.001) than urban practices. No other significant associations were found among gender, age, or race/ethnicity of pediatricians when compared with practice setting, type, and physician-estimated parental SES and parental education level.
Table 1.
Demographics and characteristics of physicians, practices, and their patients' parents in a study of Connecticut pediatricians' experience with parental vaccine concerns, 2007–2008
aTotals showing n<133 indicate missing data.
bPercentages are based on number of responses.
cAs estimated by physicians
SES = socioeconomic status
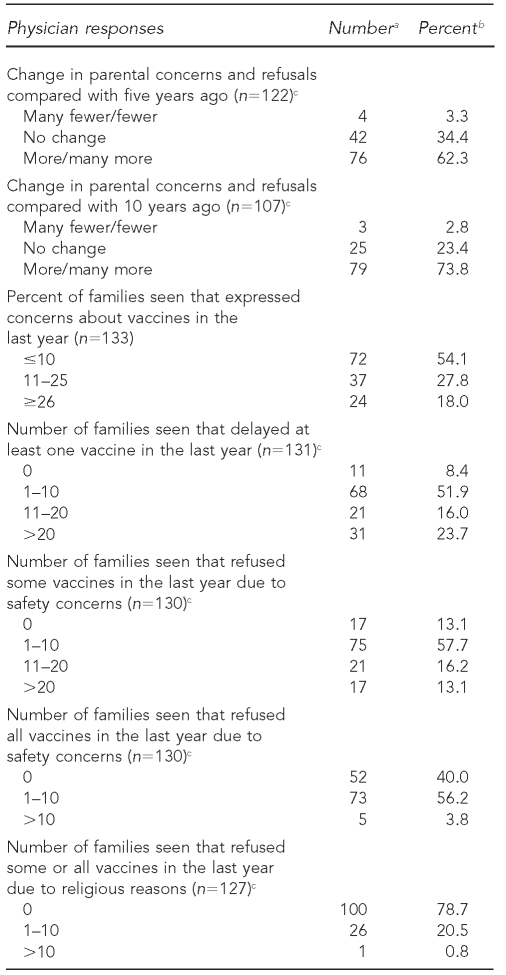
Trends in parental vaccine concerns and/or refusals
Nearly three-quarters of responding pediatricians noted an increase in parental concerns and refusals compared with 10 years ago, with 62% noting an increase in the last five years (Table 2). Almost one-fifth (18%) of pediatricians noted that more than 25% of their families had expressed concerns about vaccines and almost 30% of pediatricians reported that 11 or more families had refused some vaccines for safety reasons. More than 60% of respondents had at least one family refuse all vaccines for safety concerns in the last year. The vaccines most likely to be refused by families were those for influenza, measles-mumps-rubella, rotavirus, and varicella. Polio and Haemophilus influenzae type b vaccines were least likely to be refused.
Table 2.
Physician respondents' experience with parental vaccine safety concerns and refusals in a study of Connecticut pediatricians, 2007–2008
aAll numbers are as estimated by physicians.
bPercentages are based on number of responses. Percentages may not add to 100 due to rounding.
cTotals showing n<133 indicate missing data.
Practice characteristics and vaccine concerns and/or refusals
More suburban/rural physicians reported increased parental vaccine concerns and refusals than physicians in urban practices when compared with both five years ago (70.9% vs. 40.6%, p<0.01) and 10 years ago (84.6% vs. 42.9% p<0.001). Suburban/rural physicians were more likely than urban physicians to report more parents expressing concerns about vaccines in the last year (58.7% vs. 17.5%, p<0.001), families that delayed at least one vaccine (98.9% vs. 74.4%, p<0.001), and families that refused some vaccines (91.1% vs. 76.9%, p<0.05). There was a similar but not significant trend between suburban and urban practice settings for families that refused all vaccines (65.9% vs. 44.7%, p=0.54). Physicians in group practices and solo or two-physician practices were more likely to report more concerns and more vaccine delays and refusals of some/all vaccines when compared with respondents who practiced in community health centers, multispecialty groups, or university or hospital settings (p<0.01) (data not shown).
Parental SES and vaccine concerns and/or refusals
Higher physician-reported parental SES was positively associated with physician reporting of more parental vaccine concerns and refusals compared with five years ago (71.3% vs. 43.9%, p<0.001) and 10 years ago (85.9% vs. 48.6%, p<0.001) relative to lower physician-reported parental SES. This association also held true for the physician-reported percentage of families expressing vaccine safety concerns (61.0% vs. 22.4%, p<0.001), delaying vaccines (98.7% vs. 79.6%, p<0.001), refusing some vaccines (91.3% vs. 79.6%, p<0.05), or refusing all vaccines (66.7% vs. 50.0%, p<0.01). Similar patterns of association were found for pediatrician-estimated parental education levels (data not shown).
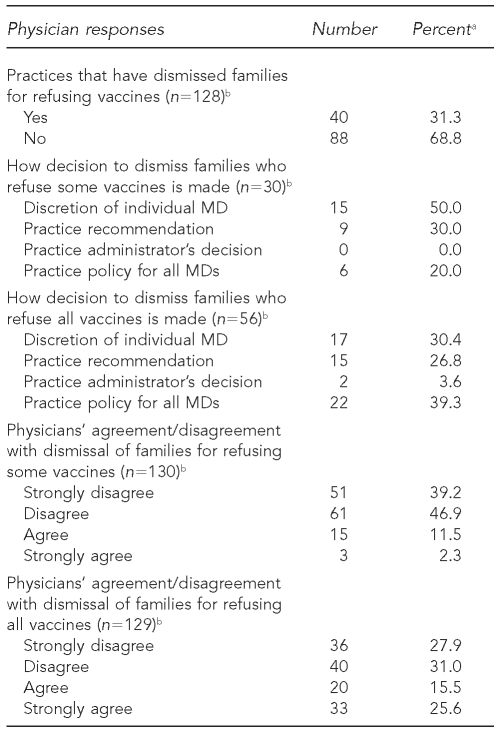
Dismissal of families who refuse vaccines
More than 30% of responding physicians reported families who had been asked to leave the practice due to the families' decision not to vaccinate their children (Table 3). Among respondents who had dismissed families who refused all vaccines, about 30% noted that in their practice, the decision to dismiss was at the discretion of individual physicians. However, nearly 40% of respondents who dismissed families noted that it was their practice's policy to dismiss families who refused all vaccines.
Table 3.
Physicians' dismissal of families due to vaccine refusal and how the decision to dismiss is made in a study of Connecticut pediatricians, 2007–2008
aPercentages are based on number of responses. Percentages may not add to 100 due to rounding.
bTotals showing n<133 indicate missing data.
MD = doctor of medicine
Physician attitudes toward dismissal of families
More than 40% of physicians agreed (15.5%) or strongly agreed (25.6%) with dismissing families who refused all vaccines (Table 3). Suburban physicians were more likely to agree/strongly agree with dismissing families who refused all vaccines when compared with urban respondents (47.8% vs. 25.6%, p<0.05), although this was not true for dismissal of families refusing some vaccines (15.6% vs. 10.0%, p=0.677). As might be expected, pediatricians who agreed/strongly agreed with the policy of dismissing families who refuse all vaccines were more likely to report no such families in their practices compared with those physicians who disagreed with dismissing families who refuse vaccines (59.6% vs. 27.0%, p<0.001) (data not shown). This association did not hold true for families delaying vaccines or refusing only some vaccines.
Dismissal of families and practice characteristics and parental SES
Suburban/rural physicians were more likely to dismiss families from their practice for vaccine refusal when compared with urban physicians (38.2% vs. 15.8%, p<0.05). Similarly, approximately 40% of physicians in group practices reported dismissing families for refusing vaccines compared with only 12% of physicians practicing in hospital or university settings (p<0.05). Pediatricians who reported working with higher SES families (as estimated by physicians) were more likely to dismiss families for refusing vaccines than physicians who reported working with poor, working-class, or middle-class families (42.4% vs. 8.7%, 24.0%, and 35.0%, respectively, p<0.05). Pediatricians reporting more vaccine concerns and refusals in the last five years (77.5% vs. 53.2%, p<0.05) and 10 years (88.9% vs. 64.7%, p<0.05) were more likely to have dismissed families for vaccine refusal when compared with those reporting the same or fewer parental concerns (data not shown).
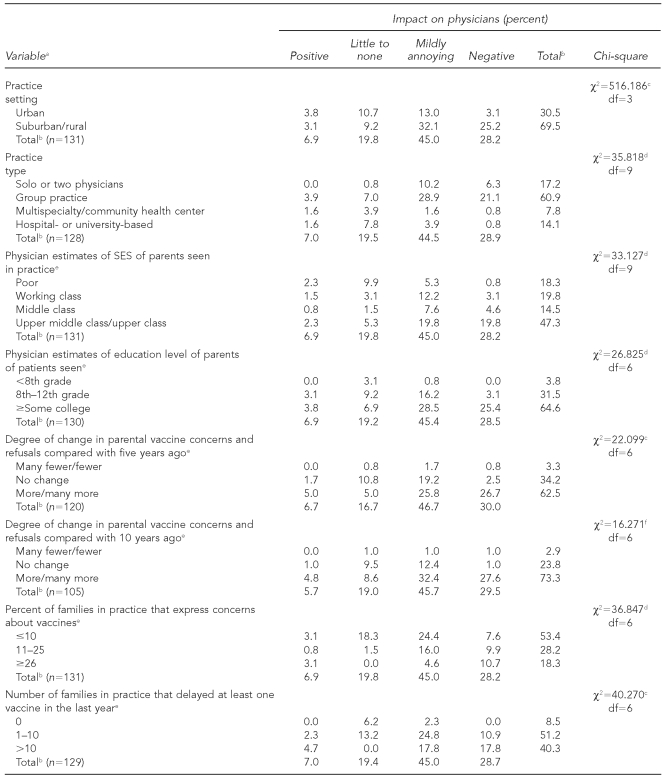
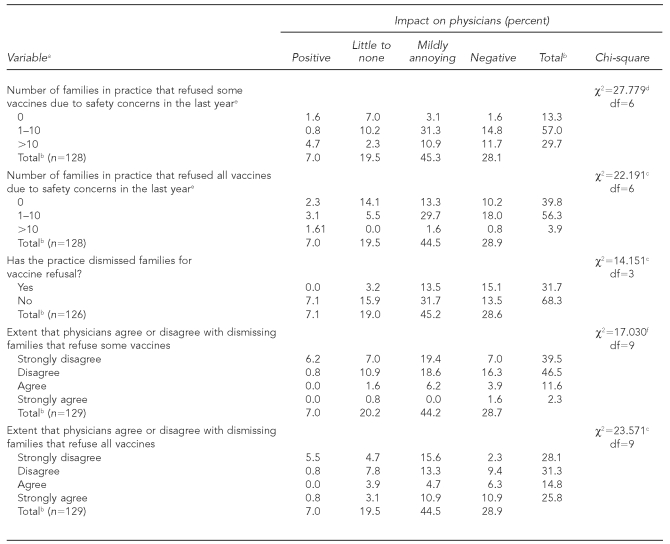
Impact of parental vaccine refusal on physicians
Forty-five percent of pediatricians responded that they found the issue of parental vaccine refusal “mildly annoying—it is part of being a pediatrician,” while 28% said it had a “negative impact” or “decreased their overall satisfaction with pediatrics.” Only 7% said it had a positive impact on them, and 20% said it had little to no impact. Negative personal impact was associated with practicing in suburban/rural areas when compared with practicing in an urban setting (25.2% vs. 3.1%, p<0.01); with group practices when compared with multispecialty/community centers or university/hospital settings (21.1% vs. 0.8%, p<0.001); with higher physician-estimated parental SES (19.8% upper middle class/upper class vs. 3.1% working class or 0.8% poor, p<0.001); and with higher physician-estimated parental education levels (25.4% some college vs. 3.1% ≤high school, p<0.001) (Table 4).
Table 4.
How vaccine refusals have impacted physician respondents, with significantly associated variables, in a study of Connecticut pediatricians, 2007–2008
aTotals showing n<133 indicate missing data.
bPercentages may not add to 100 due to rounding.
cp<0.01
dp<0.001
eAs estimated by physicians
fp<0.05
df = degree of freedom
SES = socioeconomic status
Negative personal impact on physicians was associated with reporting more parental vaccine concerns/refusals compared with fewer concerns/refusals over the past five years (26.7% vs. 0.8%, p<0.01) and 10 years (27.6% vs. 1.0%, p<0.05); and with reporting a higher number of families who expressed vaccine concerns (10.7% of physicians with 10 or more families who expressed concerns vs. 7.6% of those with no families who expressed concerns, p<0.001), delayed vaccines (17.8% of physicians with 10 or more families who delayed vs. 0.0% of physicians with no families who delayed vaccines, p<0.001), or refused some vaccines (11.7% of physicians with 10 or more families who refused some vaccines vs. 1.6% of those with no families who refused some vaccines, p<0.001). Those reporting a negative impact were significantly more likely to dismiss families who refused vaccines, with almost 50% of those dismissing families reporting a negative personal impact compared with 20% of those not dismissing families (p<0.01). Respondents who agreed with the practice of dismissing families who refuse all vaccines were more likely to report a negative personal impact than those disagreeing with dismissing families (42.3% vs. 19.7%, p<0.01) (data not shown).
Comments by respondents
This survey elicited impassioned comments on the part of the respondents. One physician wrote about discussing vaccine refusals with parents: “Most times it does not matter. Parents have made up their minds. It is frustrating'” Another wrote that he/she was only “somewhat comfortable” discussing vaccine refusal with parents “because I get so mad'” The same physician said that the issue of vaccine refusal had decreased his/her overall satisfaction with pediatrics because “on some days it's horrible.” When asked about resources given to parents about vaccines, one physician commented, “For most families inclined to refuse vaccines, none of these works and I am becoming more inclined to dismiss these families.” Several respondents commented on how time-consuming it was to address parental vaccine concerns and refusals, with one physician noting, “I often spend too much time on this and it takes time away from others.” These comments were solicited responses to open text questions.
DISCUSSION
This is the first study to address how parental vaccine refusals impact physicians personally. In Hendricks' editorial about the article by Flanagan-Klygis et al.,19 he takes issue with the authors for assuming that parental vaccine refusals negatively affect the physician-parent relationship.23 The findings from the current study support Flanagan-Klygis and colleagues' assumption that parental vaccine refusals are viewed negatively by pediatricians.19 Physicians who report a negative impact are significantly more likely to self-report working in suburban, solo/group practices with families from higher physician-estimated SES, and to care for larger numbers of families with vaccine concerns and/or refusals. Perhaps most importantly, physicians who report being negatively impacted are significantly more likely to dismiss families who refuse vaccines.
Negative feelings on the part of physicians may interfere with their ability to communicate and form trusting relationships with families who refuse vaccines. Poor communication and dismissal of families limit open discussion with parents and may make it harder to convince hesitant parents to immunize their children.7,24 Several studies have postulated that the number of parental vaccine concerns is likely to have increased since 2000 due to the controversy over thimerosal in vaccines, increased media coverage of unfounded links between vaccines and autism, and the increased number of vaccines being recommended for children.2,10,20 This study suggests that such an increase in parental concerns may be the case, at least in Connecticut, as the great majority of respondents noted an increase in parental vaccine concerns in the last five to 10 years. Similar to national studies, 83% of pediatricians in this study reported parents in their practices who refused some vaccines, and 60% reported families who refused all vaccines.19
The physicians' perspective in this study supports findings from previous studies that children who are undervaccinated due to parental choice tend to be from families with higher SES and have parents with college degrees when compared with children who are fully vaccinated or who are undervaccinated due to other reasons.2,5 Most of these previous studies have addressed this issue by gathering information from parents about their SES and education level. This study supports these findings by examining physician-reported estimates of the SES and education levels of the families in their practices. Suburban respondents serving families with higher physician-estimated SES and education levels report “more or many more” parental vaccine safety concerns and refusals, significantly higher percentages of families with vaccine concerns, and more families delaying and refusing vaccines compared with their urban colleagues who care for poorer families with less educated parents. There are many potential reasons as to why this is the case. Wealthier parents may have better access to the Internet and media sources that discuss potential vaccine safety issues and more time to devote to investigating potential concerns. Also, families who are wealthier and more educated may feel more empowered to question physicians' and governmental recommendations about immunizations.
Only two previous studies have sought to determine how commonly physicians dismiss families who refuse vaccines from their practices. Our finding of more than 30% of respondents reporting having dismissed families for vaccine refusal is much higher when compared with findings from a 2001 survey of AAP fellows in which 5% of pediatricians routinely dismissed families who refused vaccines and 18% sometimes dismissed families, and it is similar to the 39% dismissal rate found when asking physicians what they would hypothetically do if parents refused vaccines.19,25
Physicians who practice in suburban areas and see families with higher physician-estimated SES were more likely to dismiss families who refuse vaccines than were physicians who practice in urban, hospital settings with poorer or working-class families (as estimated by physicians). Physicians who choose to practice in urban areas and hospital settings with poorer populations may inherently have different philosophies about terminating families when compared with their suburban colleagues. This is partly borne out by our study finding that urban physicians are significantly less likely to agree with the practice of dismissing families for refusing some or all vaccines than suburban physicians. However, this finding does not hold true for practice type or for physician-estimated parental SES or education level. Physicians who work in hospital or university settings and care for lower physician-reported SES families do not differ from other physicians in agreeing or disagreeing with the dismissal of families for vaccine refusal. Physicians who work in hospital or university settings may need to comply with institutional guidelines on dismissal of patients and, therefore, may be unable to act on their personal opinions about families who refuse vaccines. Physicians who work in private practices may have more leeway as to when or if they dismiss patients.
That physicians who dismiss families who refuse all vaccines report fewer of these families in their practices may result from both the actual dismissal of families and possible avoidance of these practices by parents who refuse vaccines. When some physicians choose to dismiss these families, the burden of caring for them may be shifted to other physicians in the community.26,27 Practices that do not dismiss vaccine-refusing families may find themselves with a higher proportion of these families whose care may require more physician time, energy, and patience. This hypothesis may be supported by our finding that physicians who report larger numbers of parents with concerns or refusals are significantly more likely to say that these issues have a negative impact on them personally. In addition, higher numbers of undervaccinated patients clustered in certain practices or communities put the whole community at increased risk for vaccine-preventable diseases.4,28
Health maintenance organizations have started to include vaccination rates as part of their pay-for-performance programs that reward physicians financially for meeting certain benchmarks, including childhood immunization rates.29–31 This practice may financially penalize physicians with larger numbers of undervaccinated children and further discourage physicians from caring for these children.32
The AAP, American Medical Association, and Centers for Disease Control and Prevention all recommend against discharging families from a practice based solely on the families' decision not to vaccinate.1,33–35 Physicians who favor dismissing families argue that refusing vaccines can be construed as a form of neglect, that vaccines are important both for the health of individual children and the public's health, and that parental vaccine refusal substantially undermines the physician-family relationship.7,36,37 Those arguing against dismissal question if physicians would terminate their relationship with families because parents smoke around an asthmatic child, allow children to ride in the back of pickup trucks, or contribute to their child's obesity by overfeeding, all actions that put children at risk and go against physician advice.20,36,38 Children whose parents refuse immunizations still deserve quality pediatric care. Dismissed families may seek care from practitioners who further encourage or are more tolerant of their decision not to vaccinate.9,36,39,40 One recent study found a small but significantly increased incidence of vaccine safety concerns among primary care providers who cared for children who were undervaccinated by choice compared with other providers.21
Limitations
This study was limited by its small sample size, which was chosen based on convenience. The trends in the number of vaccine concerns and/or refusals in the last five and 10 years may be underestimated due to newer physicians who have only recently started in practice being unable to answer these questions. There was a 31.8% total response rate, which leaves the potential for a significant nonresponse bias. It is possible that physicians choosing to respond were more affected by the issues of parental vaccine concerns and refusals. Even if suburban physicians were overrepresented, the findings still support more prevalent vaccine concerns and/or refusals among wealthier, better educated populations. Recall bias or inaccurate estimation by physicians concerning parental SES and education level, percentage of families with vaccine concerns, and those who have delayed or refused vaccines in their practices is possible. Differentiating between delaying and refusing a vaccine may be difficult, as parents may choose to get the vaccine at a later time. Physician estimation of families' SES and education level may be limited or inaccurate. While the estimates given by physicians may not be exact, they do reflect physicians' impressions of the numbers and characteristics of families they see with vaccine concerns and refusals, and this finding deserves further study.
We do not know how well our sample represents the population of primary care pediatricians in Connecticut (regarding years in practice, practice setting, practice type, and physician demographics) and, therefore, cannot presume that our findings are generalizable to all primary care pediatricians in the state. Connecticut has a wealthy, educated population, and physicians and parents may differ from those in other areas of the U.S.41 The rate of vaccine refusal in Connecticut is low compared with other states; however, the rate is increasing, based on its number of non-medical school exemptions.42 Even if generalizable to Connecticut, these findings may not be generalizable to other states.
CONCLUSIONS
Pediatricians in Connecticut are reporting increased levels of parental vaccine safety concerns and vaccine refusals. This trend is especially significant for pediatricians who practice in suburban areas and report caring for wealthier, better educated families. Physicians who care for these suburban, affluent families are more likely to dismiss families for refusing vaccines and are more likely to report being personally negatively impacted by parental vaccine refusals.
Dismissing families who refuse vaccines limits open discussion with parents and may make it harder to convince hesitant parents to immunize their children. Continuing education concerning vaccines and parental vaccine concerns and refusals, including ethical considerations, might be helpful for physicians at this time of increasing parental concerns and refusals. A larger study of a more diverse group of pediatricians would improve our understanding of their experience with parental vaccine safety concerns and refusals and would help to inform best practices in response to these issues.
REFERENCES
- 1.Diekema DS, American Academy of Pediatrics Committee on Bioethics. Responding to parental refusals of immunization of children. Pediatrics. 2005;115:1428–31. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]
- 2.Gellin BG, Maibach EW, Marcuse EK. Do parents understand immunizations? A national telephone survey. Pediatrics. 2000;106:1097–102. doi: 10.1542/peds.106.5.1097. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (US). Summary of notifiable diseases. [cited 2008 Jan 8]. Available from: URL: http://www.cdc.gov/ncphi/disss/nndss/annsum/index.htm.
- 4.Parker AA, Staggs W, Dayan GH, Ortega-Sanchez IR, Rota PA, Lowe L, et al. Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States. N Engl J Med. 2006;355:447–55. doi: 10.1056/NEJMoa060775. [DOI] [PubMed] [Google Scholar]
- 5.Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics. 2004;114:187–95. doi: 10.1542/peds.114.1.187. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics. Strategies for pediatricians: addressing common concerns of vaccine-hesitant parents. [cited 2011 Mar 13]. Available from: URL: http://www.aap.org/immunization/pediatricians/pdf/Vaccine-Hesitant%20Parent_Final.pdf.
- 7.Levi BH. Addressing parents' concerns about childhood immunizations: a tutorial for primary care providers. Pediatrics. 2007;120:18–26. doi: 10.1542/peds.2006-2627. [DOI] [PubMed] [Google Scholar]
- 8.Freed GL, Clark SJ, Hibbs BF, Santoli JM. Parental vaccine safety concerns. The experiences of pediatricians and family physicians. Am J Prev Med. 2004;26:11–4. doi: 10.1016/j.amepre.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers' influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118:e1287–92. doi: 10.1542/peds.2006-0923. [DOI] [PubMed] [Google Scholar]
- 10.Fredrickson DD, Davis TC, Arnould CL, Kennen EM, Hurniston SG, Cross JT, et al. Childhood immunization refusal: provider and parent perceptions. Fam Med. 2004;36:431–9. [PubMed] [Google Scholar]
- 11.Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, et al. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114:e16–22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- 12.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360:1981–8. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 13.Allred NJ, Shaw KM, Santibanez TA, Rickert DL, Santoli JM. Parental vaccine safety concerns: results from the National Immunization Survey, 2001–2002. Am J Prev Med. 2005;28:221–4. doi: 10.1016/j.amepre.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 14.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125:654–9. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 15.Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics. 2008;122:718–25. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- 16.Shui IM, Weintraub ES, Gust DA. Parents concerned about vaccine safety: differences in race/ethnicity and attitudes. Am J Prev Med. 2006;31:244–51. doi: 10.1016/j.amepre.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Taylor JA, Darden PM, Brooks DA, Hendricks JW, Wasserman RC, Bocian AB. Association between parents' preferences and perceptions of barriers to vaccination and the immunization status of their children: a study from Pediatric Research in Office Settings and the National Medical Association. Pediatrics. 2002;110:1110–6. doi: 10.1542/peds.110.6.1110. [DOI] [PubMed] [Google Scholar]
- 18.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holomboe ES. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 19.Flanagan-Klygis EA, Sharp L, Frader JE. Dismissing the family who refuses vaccines: a study of pediatrician attitudes. Arch Pediatr Adolesc Med. 2005;159:929–34. doi: 10.1001/archpedi.159.10.929. [DOI] [PubMed] [Google Scholar]
- 20.Lyren A, Leonard E. Vaccine refusal: issues for the primary care physician. Clin Pediatr (Phila) 2006;45:399–404. doi: 10.1177/0009922806289581. [DOI] [PubMed] [Google Scholar]
- 21.Salmon DA, Pan WK, Omer SB, Navar AM, Orenstein W, Marcuse EK, et al. Vaccine knowledge and practices of primary care providers of exempt vs. vaccinated children. Hum Vaccin. 2008;4:286–91. doi: 10.4161/hv.4.4.5752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SPSS, Inc. SPSS® for Windows: Version 11.5. Chicago: SPSS, Inc; 2002. [Google Scholar]
- 23.Hendricks JW. Does immunization refusal warrant discontinuing a physician-patient relationship? Arch Pediatr Adolesc Med. 2005;159:994. doi: 10.1001/archpedi.159.10.994. [DOI] [PubMed] [Google Scholar]
- 24.Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers: the role of information. Am J Prev Med. 2005;29:105–12. doi: 10.1016/j.amepre.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Evans G, O'Connor KG, Ake JK. Risk communication and pediatrician responses to vaccine refusal. Paper presented at the 37th National Immunization Conference of CDC; 2003 Mar 17; Chicago. [Google Scholar]
- 26.Balint J. There is a duty to treat noncompliant patients. Semin Dial. 2001;14:28–31. doi: 10.1046/j.1525-139x.2001.00010.x. [DOI] [PubMed] [Google Scholar]
- 27.Orentlicher D. From the Office of the General Counsel. Denying treatment to the noncompliant patient. JAMA. 1991;265:1579–82. [PubMed] [Google Scholar]
- 28.Kimmel SR. Vaccine adverse events: separating myth from reality. Am Fam Physician. 2002;66:2113–20. [PubMed] [Google Scholar]
- 29.Anthem Blue Cross and Blue Shield. 2008 primary care quality incentive program for primary care providers. [cited 2011 Mar 13]. Available from: URL: http://www.anthem.com/shared/noapplication/f5/s2/t0/pw_ad085215.pdf.
- 30.Freed GL, Uren RL. Pay-for-performance: an overview for pediatrics. J Pediatr. 2006;149:120–4. doi: 10.1016/j.jpeds.2006.03.023. [DOI] [PubMed] [Google Scholar]
- 31.Henley E. Pay-for-performance: what can you expect? J Fam Pract. 2005;54:609–12. [PubMed] [Google Scholar]
- 32.Chien AT, Dudley RA. Pay-for-performance in pediatrics: proceed with caution. Pediatrics. 2007;120:186–8. doi: 10.1542/peds.2007-1158. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics. Red book: 2006 report of the Committee on Infectious Diseases. In: Pickering LK, Baker CJ, Long SS, McMillan JA, editors. 27th ed. Elk Grove Village (IL): American Academy of Pediatrics; 2006. [Google Scholar]
- 34.American Medical Association. Report of the council on ethical and judicial affairs: pediatric decision-making. 2007. [cited 2008 Feb 18]. Available from: URL: http://www.ama-assn.org/ama1/pub/upload/mm/369/ceja_8i07.pdf.
- 35.Atkinson W, Hamborsky J, McIntyre L, Wolfe C, Centers for Disease Control and Prevention (US). 10th ed. Washington: CDC; 2007. Epidemiology and prevention of vaccine-preventable diseases. [Google Scholar]
- 36.Breach KE, Scott CA. Is it appropriate for a physician to dismiss a family for refusing all vaccinations? Fam Pract News. 2005;35:19. [Google Scholar]
- 37.Elston MP. Dismissing families: a critical issue. Arch Pediatr Adolesc Med. 2006;160:452–3. doi: 10.1001/archpedi.160.4.452-b. [DOI] [PubMed] [Google Scholar]
- 38.Kemper KJ. Dismissing families: a slippery slope. Arch Pediatr Adolesc Med. 2006;160:452–3. doi: 10.1001/archpedi.160.4.452-a. [DOI] [PubMed] [Google Scholar]
- 39.Halperin B, Melnychuk R, Downie J, Macdonald N. When is it permissible to dismiss a family who refuses vaccines? Legal, ethical and public health perspectives. Paediatr Child Health. 2007;12:843–5. doi: 10.1093/pch/12.10.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med. 2005;159:470–6. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- 41.Census Bureau (US). American factfinder. [cited 2008 Mar 14]. Available from: URL: http://factfinder.census.gov/home/saff/main.html?_lang=en.
- 42.Centers for Disease Control and Prevention (US). School and childcare vaccination surveys. [cited 2007 Nov 18]. Available from: URL: http://www.cdc.gov/vaccines/stats-surv/schoolsurv/default.htm#surveys.