Abstract
Objective
Little is known about how families' experiences with immunization visits within the medical home may affect children's immunization status. We assessed the association between families' negative immunization experiences within the medical home and underimmunization.
Methods
We surveyed parents (n=392) of children aged 2–36 months about immunization experiences at community health centers, hospital-based clinics, private practices, and community-based organizations in New York City. We used Chi-square tests and odds ratios (ORs) to assess the relationship between medical home elements and parental immunization experience ratings. We used multivariable analysis to determine the association between negative experiences during immunization visits and underimmunization, controlling for insurance, maternal education, and receipt of benefits from the Special Supplemental Nutrition Program for Women, Infants, and Children.
Results
The majority of children were of Latino race/ethnicity and had Medicaid and a medical home. One-sixth (16.9%) of families reported a previous negative immunization experience, primarily related to the child's reaction, waiting time, and attitudes of medical and office staff. Parents' negative immunization experiences were associated with the absence of four components of the medical home: continuity of care, family-centered care, compassionate care, and comprehensive care. In addition, children in families who reported a negative experience were more likely to have been underimmunized (adjusted OR=2.00; 95% confidence interval 1.12, 3.58).
Conclusions
In a community in New York City, underimmunization of young children was associated with negative immunization experiences. Strategies to improve family experiences with immunization visits within the medical home (particularly around support for the family), medical and ancillary staff attitudes, and reduced waiting time may lead to improved immunization delivery.
For approximately one in four young children in the United States, the immunization process is derailed and they fail to complete their immunizations on time.1 According to the social learning model, people learn from their own and others' experiences, and these experiences may change subsequent behavior through positive or negative reinforcement. Therefore, the entire immunization experience, including the family's interaction with health-care providers and office staff, may color how families view immunizations. These experiences may then, in turn, affect parents' bringing their children in a timely fashion to the multiple primary care visits needed to complete the immunization process.2 Certain elements of the medical home, especially related to family-centered and compassionate care, may play an important role in families' immunization experiences. A medical home is a comprehensive approach to medical care with seven key elements: accessible, family-centered, continuous, comprehensive, coordinated, compassionate, and culturally effective care.3
Although studies in the U.S. and elsewhere have identified many factors associated with underimmunization, including satisfaction,1,4–14 relatively little is known about how previous immunization experiences shape immunization patterns. While it is expected that children with strong medical homes will return regularly for well-child visits, completing their immunizations on time, we do not know what aspect of the medical home might be most influential in supporting this process. Therefore, the objective of this study was to assess the association among families' immunization experiences, the medical home, and underimmunization.
METHODS
Survey methodology
From May 2007 to June 2008, we conducted a bilingual cross-sectional survey of parents of children aged 2–36 months with a focus on understanding factors that affected parental return for immunization visits. Parents were interviewed in a variety of settings in Northern Manhattan, a low-income community in New York City with predominantly Latino and African American families, as well as the adjacent neighborhoods of the Bronx, Upper East Side, and Upper West Side. Parents were purposefully sampled through community health centers (n=5), private practices (n=8), hospital-based clinics (n=2), and community-based organizations (n=7), with a particular focus on those who were members of racial/ethnic minority groups. For health-care facilities and some community-based organizations, parents were systematically approached in the waiting room at interview periods, which were selected to cover the periods the site was open, including days, weekends, and evenings. Using a random start, interviewers approached every third patient to be interviewed based on seating location; if that person refused, then the next person was approached. Parents were also recruited through parental groups at community-based organizations. Of the families who were approached, two-thirds agreed to be surveyed. After interviewers obtained signed informed consent, they verbally administered surveys in English or Spanish, depending on the family's preference. Participants received a $4 Metrocard for the New York City Transportation Authority (the value of a round-trip ride).
While the overall study focused on missed immunization visits, this analysis focused on factors affecting underimmunization. To link parental experiences with underimmunization, we asked parents for permission to view the child's immunization record, contained in the parent handheld card, clinical chart, and/or the immunization registry. Two-thirds (66.5%) of parents gave permission to view their child's immunization record, and 87.2% of those records were available for review (n=410).
In the analytic sample, we included immunization records in which the first tetanus-containing vaccine was given before six months of age (n=392) to reduce the chance of miscounting diphtheria-tetanus-acellular pertussis (DTaP) vaccine doses after age six months, if the first dose had not been recorded. Children with available immunization records were less likely to be African American and more likely to have a mother born in the U.S. than children without available records. The analytic sample was distributed among the sampling sites as follows: private practice (29.1%), community health center (18.4%), hospital-based clinic (29.1%), and community-based organization (23.4%). The Columbia University Medical Center Institutional Review Board approved the study.
Survey content
The survey tool designed for this study was based on input from formative focus groups of parents and providers from the community (n=22 participants), a previous survey used by the research team,15 the National Survey of Children's Health,16 and a literature review. We conducted four focus groups using a semistructured topic guide with parents from community-based organizations in Northern Manhattan, including Spanish-speaking and English-speaking parents of children who were fully immunized and those who were not. One focus group was conducted with pediatric providers.
Survey questions covered the topics of families' previous immunization experiences and the seven elements of the medical home (continuous, family-centered, compassionate, culturally effective, coordinated, comprehensive, and accessible care). Most questions were close-ended with four- or five-point Likert scale or dichotomous yes/no responses; a few open-ended questions with field-coded responses were also included. The survey was pretested and translated forward and backward into Spanish to ensure linguistic and cultural equivalency.
Variables
The primary outcome variable was if the child was ever underimmunized. For this study, we defined underimmunization as failure to receive the recommended vaccinations within one month of due date, according to the age-appropriate 4:3:1:3:3:1 series2—diphtheria-tetanus-pertussis, diphtheria-tetanus, or DTaP vaccine; polio vaccine; measles-containing vaccine; Haemophilus influenzae type b (Hib) vaccine; hepatitis B vaccine; and varicella vaccine. Due to the Hib shortage during the survey period, children who were up-to-date (UTD) except for Hib were considered UTD.
The main independent variable was at least one negative previous immunization experience. Parents were asked to rate their last two immunization visits on a scale from 0 to 10, with 10 being the best possible experience. For either of those visits, if a parent gave a rating from 0 to 5, the family was considered to have had a previous negative immunization experience. Parents were also asked why they gave that rating. In addition, parents were asked for their preferences regarding immunization practices, such as who should administer the immunization, and they were asked to rate their perceived presence of the seven elements of the medical home (continuous, accessible, comprehensive, coordinated, family-centered, compassionate, and culturally effective care).3
Analysis
Focus group transcripts were analyzed using ATLAS.ti software17 for content analysis. Categories were generated inductively by the research assistant and the principal investigator based on participants' comments, and a codebook was created. Transcripts were then coded and used both for survey design and to provide parental examples of factors that were found to be significant on statistical analysis.
The survey data were analyzed to assess parental reasons for immunization experience ratings and the relationship between medical home elements and parental ratings, using frequency distributions, Chi-square tests, and odds ratios (ORs) with 95% confidence intervals (CIs). Multivariable analysis was used to assess the association between underimmunization and previous negative experiences, controlling for factors known to be associated with underimmunization, including insurance and socioeconomic status, as measured by maternal education and receipt of benefits from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Adjusted ORs (AORs) and 95% CIs are reported. All statistical analyses were conducted using SPSS® version 17.0.18
RESULTS
Respondent characteristics
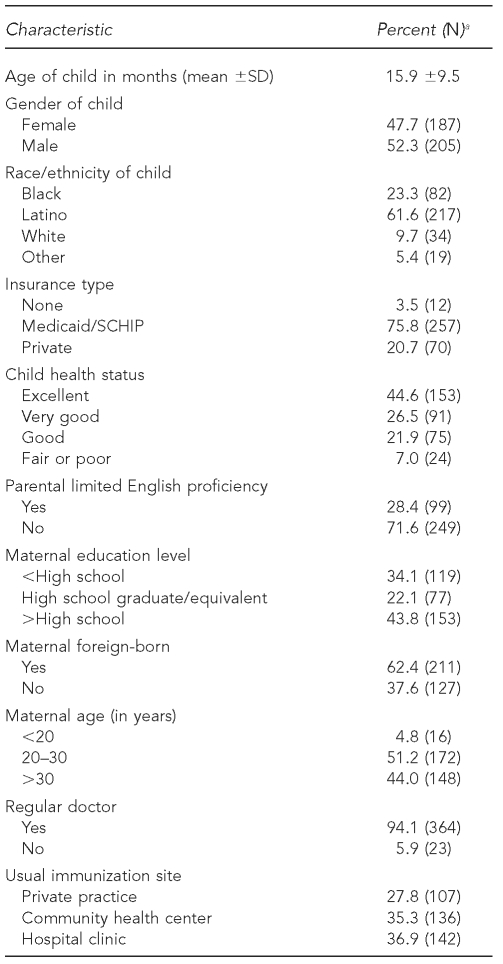
The mean age of the children of respondents was 15.9 (standard deviation [SD] = 69.5) months. The majority of children were Latino, were covered by -Medicaid or State Children's Health Insurance Program (SCHIP), and were in excellent or very good health. The majority of mothers had completed a high school education, more than half were foreign-born, and more than one-fourth had limited English proficiency. Almost all had a medical home, and the source of care was split fairly evenly among private practices, community health centers, and hospital-based clinics (Table 1).
Table 1.
Characteristics of participants (n=392) in a study of parents' experiences at children's immunization visits, New York City, 2007–2008
aNumbers shown do not all total 392, as some respondents did not answer all questions. Percentages are based on number of responses.
SD = standard deviation
SCHIP = State Children's Health Insurance Program
Previous negative immunization experiences
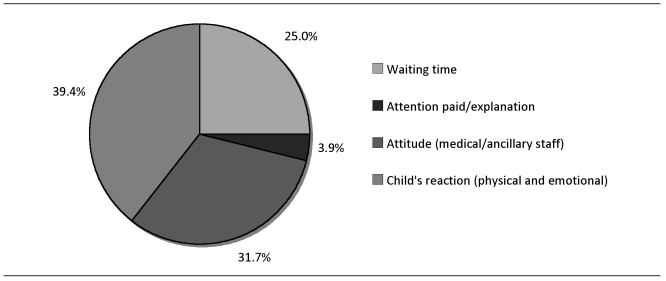
The mean rating parents assigned their last immunization experience was 8.5 (SD = ±2.3), ranging from 0 to 10 with an interquartile ratio of 2.0. One-sixth (16.9%) of families had a previous negative immunization experience. The most common reasons for a poor rating were the child's negative physical or emotional response to the immunization (39.4%) and discomfort with the attitude of the health-care provider or medical staff (31.7%) (Figure). The majority (73.2%) of the negative ratings due to the child's reaction to the immunization were because of the child's emotional reaction (e.g., crying). The same factors for a negative experience were noted in the focus groups, where parents related how they were distressed by their child's reaction, which was further compounded by a lack of support and information during and after immunizations, as illustrated by these comments:
Figure.
Reported primary reasons why families gave previous immunization experience a negative rating in a study of parents' experiences at children's immunization visits, New York City, 2007–2008
The worst part. .. was a lot of shots. .. I thought the nurse could have probably handled it a little bit different. .. I felt like I had to be on their side more than on his [my son's] side, which. .. I felt real[ly] bad that day when I went home. .. because I felt like he felt like he was alone. Like I was with the doctors with giving him this shot.. . .
The baby was getting a fever and reacting to the immunization, and [we] went to the emergency room, and they said, “Well there's nothing wrong, go home.” So, how does that influence you when you think about going to the doctor the next time your baby needs a shot?
Parents identified specific immunization practices that could improve the child's immunization experience. For some, these practices included preferences for immunization delivery: 68.7% of all parents preferred the doctor to give the immunization, and 70.7% felt it was very important that whoever gave the immunization gave it quickly. Others gave preferences for how the person administering the vaccine followed up after immunizations were given. Seventy percent felt it was very important and 11.4% felt it was somewhat important that the person giving the immunization also help calm the child down afterward. Finally, 62.5% felt it was important that the child be given some sort of treat afterward, such as a sticker.
The next most common reason for a negative immunization experience rating was the attitude of the medical and administrative staff. The attitude of doctors, nurses, or office staff or a lack of professionalism accounted for almost one-third of the reasons for negative ratings. Among the parents' comments were the following:
Because there are some [providers]. .. that upon entering, they cuddle them, they hug them, they give them kisses, things like that. So, they create a nice environment for the child. But there are others that sit them down—BAM, BAM, BAM—and goodbye, we will see you next time. That is no good.
Like, one day I couldn't get off in time, so then they [said], “You were supposed to be here at this time.” I said, “Well, I had to work.” They had an attitude.. . .
Finally, about one-fourth of negative reasons were attributed to waiting time in the office:
.. . but sometimes you don't have the time to sit around and wait. .. I had to go to work, so I still couldn't wait around for a shot.
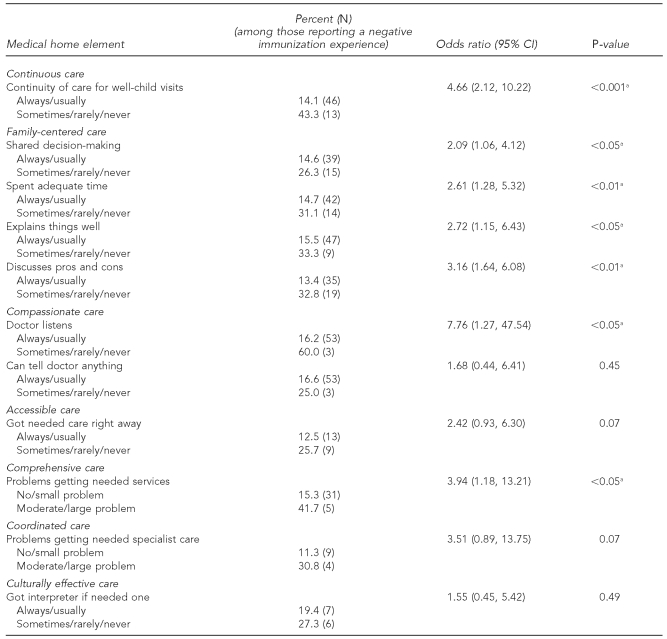
Relationship between negative immunization experiences and medical home elements
Parents' negative immunization experiences were associated with the absence of four components of the medical home: continuity of care, family-centered care, compassionate care, and comprehensive care (Table 2). Families whose child sometimes, rarely, or never saw the same provider for well-child checkups were more likely to report a negative experience than those who saw the same provider usually or always (OR=4.66, 95% CI 2.12, 10.22). In the focus groups, parents remarked on this lack of continuity:
Table 2.
Relationship between medical home elements and negative immunization experiences in a study of parents' experiences at children's immunization visits, New York City, 2007–2008
aStatistically significant
CI = confidence interval
I don't like that. Because you cannot build up a relationship with a doctor if every time you go, you're seeing someone different.
Likewise, families whose child's provider sometimes, rarely, or never engaged them in discussions about the pros and cons of health-care options had three times greater odds of having a negative immunization experience compared with those whose provider usually or always discussed options with them (OR=3.16, 95% CI 1.64, 6.08). Decreased levels of parental sharing in decision-making, provider explanation to parents, and providers' listening to parents also had a significant effect on ratings of immunization experiences (Table 2).
I think it's when the doctor communicates [with] my child, the reason for it, when he gets to understand [that] there's more than just that prick. .. [when the doctor explains] it's something that's going to be good for a while for you, that's going to make you healthy. So, the fact that he explains and talks to my child, that's important to me.
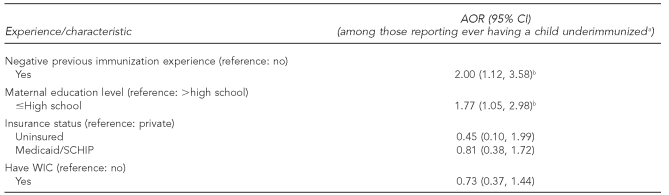
Relationship between negative immunization experiences and underimmunization
Negative immunization experience and ever not being UTD on immunizations were significantly related. Multivariable analysis showed that children in families who reported negative immunization experiences had two times greater odds of ever being underimmunized (AOR=2.00, 95% CI 1.12, 3.58) compared with those who had not reported a previous negative experience, after controlling for insurance, maternal education, and WIC (Table 3). This relationship may be mediated through missed immunization visits, as parents who had a negative immunization experience were also more likely to report missing an immunization visit than those who did not report a negative experience (AOR=2.19, 95% CI 1.07, 4.48), after controlling for the same factors listed previously.
Table 3.
Multivariable analysis of relationship between negative immunization experiences and underimmunization in a study of parents' experiences at children's immunization visits, New York City, 2007–2008
aUnderimmunized was defined as failure to receive the recommended vaccinations within one month of due date, according to the age-appropriate 4:3:1:3:3:1 series—diphtheria-tetanus-pertussis, diphtheria-tetanus, or diphtheria-tetanus-acellular pertussis vaccine; polio vaccine; measles-containing vaccine; Haemophilus influenzae type b vaccine; hepatitis B vaccine; and varicella vaccine. Source: Centers for Disease Control and Prevention (US). Recommended immunization schedule for persons aged 0 through 6 years—United States 2010 [cited 2010 Nov 11]. Available from: URL: http://www.cdc.gov/vaccines/recs/schedules/child-schedule.htm
bStatistically significant
AOR = adjusted odds ratio
CI = confidence interval
SCHIP = State Children's Health Insurance Program
WIC = Special Supplemental Nutrition Program for Women, Infants, and Children
DISCUSSION
This study documents the association between negative immunization experiences and childhood underimmunization. These negative immunization experiences revolved around three main themes: a child's negative reaction to the immunization, the attitude of the medical and ancillary staff, and waiting time. Related to and underlying these contributors to negative experiences were perceived deficiencies in four specific medical home components—continuous, compassionate, family-centered, and comprehensive care. Interventions targeting these factors could improve families' immunization experiences, which, in turn, could contribute to increased timely immunization coverage rates.
Parents' perceptions of their child's emotional and physical reaction to receiving immunizations largely colored the immunization experience. Pain, or fear of pain, was a key factor that affected how a child experiences immunizations. Therefore, using techniques that decrease the pain associated with immunizations could reduce these negative experiences. Such techniques include the order in which vaccines are given, physical interventions such as positioning, psychological interventions such as distraction, and pharmacologic interventions such as topical anesthetics.19–21 The use of non-injectable vaccines, such as oral and intranasal preparations, may also be helpful. How a child copes with immunizations can also be influenced. Child coping and distress are related in large part to maternal anxiety and parent and staff behavior, as well as to a child's previous medical experiences.22,23 Therefore, support for the parent is imperative. Our study showed that parents did not want to feel responsible for restraining their child for an immunization. Although parents may need to help hold their child for immunization, interventions designed to reframe this holding from restraining to providing a parental comforting touch may improve both the parental and child experience.19,24 Small gestures such as giving stickers also seemed to improve parental perceptions and should be considered.
Parents also felt that staff behavior and attitude contributed to their immunization experience; lack of staff support for the parent or child made the immunization experience more difficult. This finding is consistent with a previous study that showed when staff kept a running commentary for children, during which the staff remarked on the child being brave and let the child know how soon they would be finished with the immunization, these children showed less stress than children for whom this commentary was not provided.25 Parental concern about staff attitudes encompassed the entire immunization experience, including interactions with office staff, not just the actual immunization process. Improving general parental satisfaction with primary care visits may, therefore, have a positive impact on immunizations, as has been suggested in previous studies linking parent satisfaction to health-care utilization, including immunizations.10,26 Satisfaction may have also been affected by waiting time, as many parents reported frustrations with waiting time. Previous studies have shown an association between waiting time and underimmunization.27
Parents' distress over the immunization process, and, specifically, perceptions of the lack of support and understanding they receive from their child's medical providers, is related to the underlying nature of the medical home. Our study documented that families whose medical home lacked continuity, compassionate, family-centered, and/or comprehensive care elements were more likely to have negative immunization experiences. Having a medical home has been recommended because of its associations with various improved health outcomes,3,28,29 including immunization coverage.30,31 This study shows how perceived absence of these medical home elements may influence the immunization process. Of note, the absence of these medical home elements may act through indirect processes, coloring how parents experience their child's visit rather than being an overt, attributable cause in the parents' minds. For example, while parents who had negative immunization experiences also reported that the provider did not spend adequate time or explain things well, these failures of communication were not common reasons why families gave an immunization experience a negative rating.
Limitations
This study had several limitations. First, parents were asked to rate their last two immunization visits retrospectively, and this may have introduced recall bias. Future studies could ask parents to rate their visit immediately after its conclusion. Second, the association between negative experiences and underimmunization is not necessarily causal, as we do not know the temporal sequencing of these events. Third, the assessment of the relationship between medical home components and immunization experiences was limited by the small sample sizes of parents who did or did not experience certain elements. For example, one measure of access is the ability to get needed care urgently, but many parents never needed to get urgent care for their child.
Fourth, although we were able to obtain immunization records from the majority of families, immunization records were not available for all families, and children with unavailable records were more likely to be African American or have U.S.-born mothers. We found no significant relationship between race/ethnicity and/or maternal nativity and either previous negative experiences or prior immunization status. We also did not collect income information, due to the sensitivity of that question, but used insurance status, maternal education, and receipt of WIC benefits as indicators of socioeconomic status. Most respondents were publicly insured and had Medicaid or SCHIP, and, therefore, would be considered low-income. Finally, the study population was mostly from minority and low-income communities; thus, their experiences may differ from those in other populations. Yet, children's reaction to vaccination, poor attitudes of medical and ancillary staff, and waiting time can be experienced in a variety of care settings.
CONCLUSIONS
In this study, we found that previous negative immunization experiences were associated with underimmunization, suggesting a potential impact on children returning for immunizations. Strategies to improve family satisfaction with immunization visits, particularly around support for the family, attitudes of medical and ancillary staff, waiting time, and provision of a medical home, may lead to improved immunization delivery.
Acknowledgments
The authors thank Holly Groom and Gary Edgar, project officers from the Centers for Disease Control and Prevention (CDC), National Center for Immunization and Respiratory Diseases (NCIRD), for their support; and Benjamin Ortiz, Oscar Peñna, Shaofu Chen, Maggie Veatch, Faith McCollister, Laura Radulescu, Piali Basu, Maia Alejandro, and Diego Lopez De Castilla for their help. The authors also thank all the sites, providers, and parents who participated in this study.
Footnotes
This research was funded by CDC, NCIRD grant #U01 IP000086. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of CDC or NCIRD. This study was presented as a poster presentation at the Eastern Society for Pediatric Research annual meeting held in Philadelphia in March 2009 and at the Pediatric Academic Societies annual meeting held in Baltimore in May 2009.
REFERENCES
- 1.National, state, and local area vaccination coverage among children aged 19–35 months—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(36):1171–7. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US). Recommended immunization schedule for persons aged 0 through 6 years—United States 2010. [cited 2010 Nov 11]. Available from: URL: http://www.cdc.gov/vaccines/recs/schedules/child-schedule.htm.
- 3.American Academy of Pediatrics; Medical Home Initiatives for Children with Special Needs Project Advisory Committee. The medical home. Pediatrics. 2002;110:184–6. [Google Scholar]
- 4.Klevens RM, Luman ET. U.S. children living in and near poverty: risk of vaccine-preventable diseases. Am J Prev Med. 2001;20(4 Suppl):41–6. doi: 10.1016/s0749-3797(01)00281-1. [DOI] [PubMed] [Google Scholar]
- 5.Bardenheier BH, Yusuf HR, Rosenthal J, Santoli JM, Shefer AM, Rickert DL, et al. Factors associated with underimmunization at 3 months of age in four medically underserved areas. Public Health Rep. 2004;119:479–85. doi: 10.1016/j.phr.2004.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bates AS, Fitzgerald JF, Dittus RS, Wolinsky FD. Risk factors for underimmunization in poor urban infants. JAMA. 1994;272:1105–10. [PubMed] [Google Scholar]
- 7.Findley SE, Irigoyen M, Schulman A. Children on the move and vaccination coverage in a low-income, urban Latino population. Am J Public Health. 1999;89:1728–31. doi: 10.2105/ajph.89.11.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prislin R, Dyer JA, Blakely CH, Johnson CD. Immunization status and sociodemographic characteristics: the mediating role of beliefs, attitudes, and perceived control. Am J Public Health. 1998;88:1821–6. doi: 10.2105/ajph.88.12.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grabowsky M, Orenstein WA, Marcuse EK. The critical role of provider practices in undervaccination. Pediatrics. 1996;97:735–7. [PubMed] [Google Scholar]
- 10.Schempf AH, Minkovitz CS, Strobino DM, Guyer B. Parental satisfaction with early pediatric care and immunization of young children: the mediating role of age-appropriate well-child care utilization. Arch Pediatr Adolesc Med. 2007;161:50–6. doi: 10.1001/archpedi.161.1.50. [DOI] [PubMed] [Google Scholar]
- 11.Brenner RA, Simons-Morton BG, Bhaskar B, Das A, Clemens JD NIH-D.C. Initiative Immunization Working Group. Prevalence and predictors of immunization among inner-city infants: a birth cohort study. Pediatrics. 2001;108:661–70. doi: 10.1542/peds.108.3.661. [DOI] [PubMed] [Google Scholar]
- 12.Ghei K, Agarwal S, Subramanyam MA, Subramanian SV. Association between child immunization and availability of health infrastructure in slums in India. Arch Pediatr Adolesc Med. 2010;164:243–9. doi: 10.1001/archpediatrics.2009.277. [DOI] [PubMed] [Google Scholar]
- 13.Sia D, Fournier P, Kobiane JF, Sondo BK. Rates of coverage and determinants of complete vaccination of children in rural areas of Burkina Faso (1998–2003) BMC Public Health. 2009;9:416. doi: 10.1186/1471-2458-9-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiss WM, Winch PJ, Burnham G. Factors associated with missed vaccination during mass immunization campaigns. J Health Popul Nutr. 2009;27:358–67. doi: 10.3329/jhpn.v27i3.3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stockwell MS, Findley SE, Irigoyen M, Martinez RA, Sonnett M. Change in parental reasons for use of an urban pediatric emergency department in the past decade. Pediatr Emerg Care. 2010;26:181–5. doi: 10.1097/PEC.0b013e3181d1dfc7. [DOI] [PubMed] [Google Scholar]
- 16.Child and Adolescent Health Measurement Initiative. National survey of children's health: data resource center. [cited 2010 Jan 14]. Available from: URL: http://www.nschdata.org.
- 17.ATLAS.ti Scientific Software Development GmbH. ATLAS.ti: Version 5.2. Berlin (Germany): ATLAS.ti Scientific Software Development GmbH; 2006. [Google Scholar]
- 18.SPSS Inc. SPSS®: Version 17. Chicago: SPSS Inc.; 2009. [Google Scholar]
- 19.Taddio A, Chambers CT, Halperin SA, Ipp M, Lockett D, Rieder MJ, et al. Inadequate pain management during routine childhood immunizations: the nerve of it. Clin Ther. 2009;31(Suppl 2):S152–67. doi: 10.1016/j.clinthera.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Ipp M, Parkin PC, Lear N, Goldbach M, Taddio A. Order of vaccine injection and infant pain response. Arch Pediatr Adolesc Med. 2009;163:469–72. doi: 10.1001/archpediatrics.2009.35. [DOI] [PubMed] [Google Scholar]
- 21.Berberich FR, Landman Z. Reducing immunization discomfort in 4- to 6-year-old children: a randomized clinical trial. Pediatrics. 2009;124:e203–9. doi: 10.1542/peds.2007-3466. [DOI] [PubMed] [Google Scholar]
- 22.Frank NC, Blount RL, Smith AJ, Manimala MR, Martin JK. Parent and staff behavior, previous child medical experience, and maternal anxiety as they relate to child procedural distress and coping. J Pediatr Psychol. 1995;20:277–89. doi: 10.1093/jpepsy/20.3.277. [DOI] [PubMed] [Google Scholar]
- 23.Schechter NL, Zempsky WT, Cohen LL, McGrath PJ, McMurtry CM, Bright NS. Pain reduction during pediatric immunizations: evidence-based review and recommendations. Pediatrics. 2007;119:e1184–98. doi: 10.1542/peds.2006-1107. [DOI] [PubMed] [Google Scholar]
- 24.Cavender K, Goff MD, Hollon EC, Guzzetta CE. Parents' positioning and distracting children during venipuncture. Effects on children's pain, fear, and distress. J Holist Nurs. 2004;22:32–56. doi: 10.1177/0898010104263306. [DOI] [PubMed] [Google Scholar]
- 25.Plumridge E, Goodyear-Smith F, Ross J. Nurse and parent partnership during children's vaccinations: a conversation analysis. J Adv Nurs. 2009;65:1187–94. doi: 10.1111/j.1365-2648.2009.04999.x. [DOI] [PubMed] [Google Scholar]
- 26.Halfon N, Inkelas M, Mistry R, Olson LM. Satisfaction with health care for young children. Pediatrics. 2004;113(6 Suppl):1965–72. [PubMed] [Google Scholar]
- 27.Dietz VJ, Baughman AL, Dini EF, Stevenson JM, Pierce BK, Hersey JC. Vaccination practices, policies, and management factors associated with high vaccination coverage levels in Georgia public clinics. Georgia Immunization Program Evaluation Team. Arch Pediatr Adolesc Med. 2000;154:184–9. doi: 10.1001/archpedi.154.2.184. [DOI] [PubMed] [Google Scholar]
- 28.Cooley WC, McAllister JW, Sherrieb K, Kuhlthau K. Improved outcomes associated with medical home implementation in pediatric primary care. Pediatrics. 2009;124:358–64. doi: 10.1542/peds.2008-2600. [DOI] [PubMed] [Google Scholar]
- 29.Porter S. Academy launches comprehensive patient-centered medical home resources. Ann Fam Med. 2009;7:378–9. doi: 10.1370/afm.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Irigoyen M, Findley S, Chen S, Vaughan R, Sternfels P, Caesar A, et al. Early continuity of care and immunization coverage. Ambul Pediatr. 2004;4:199–203. doi: 10.1367/A03-138R1.1. [DOI] [PubMed] [Google Scholar]
- 31.Smith PJ, Santoli JM, Chu SY, Ochoa DQ, Rodewald LE. The association between having a medical home and vaccination coverage among children eligible for the Vaccines for Children program. Pediatrics. 2005;116:130–9. doi: 10.1542/peds.2004-1058. [DOI] [PubMed] [Google Scholar]