Abstract
Objectives
In a population of seniors served by urban primary care centers, we evaluated the effect of the practice-based intervention on influenza immunization rates and disparities in vaccination rates by race/ethnicity and insurance status.
Methods
A randomized controlled trial during 2003–2004 tested patient tracking/recall/outreach and provider prompts on improving influenza immunization rates. Patients aged ≥65 years in six large inner-city primary care practices were randomly allocated to study or control group. Influenza immunization coverage was measured prior to enrollment and on the end date.
Results
At study end, immunization rates were greater for the intervention group than for the control group (64% vs. 22%, p<0.0001). When controlling for other factors, the intervention group was more than six times as likely to receive influenza vaccine. The intervention was effective across gender, race/ethnicity, age, and insurance subgroups. Among the intervention group, 3.5% of African Americans and 3.2% of white people refused influenza immunization.
Conclusions
Patient tracking/recall/outreach and provider prompts were intensive but successful approaches to increasing seasonal influenza immunization rates among this group of inner-city seniors.
During the period from 1990–1991 to 1998–1999, the annual estimated U.S. seasonal influenza-associated deaths averaged about 36,000, and 90% of these deaths occurred in people aged 65 years or older.1 Approximately 200,000 influenza-associated hospitalizations also occurred, with a large proportion among seniors.2 The average annual U.S. cost for pneumonia and influenza-related hospitalizations exceeds $370 million.3
Despite the substantial disease burden from influenza, reported vaccination coverage was 67.2% for people aged ≥65 years, which was consistent with previous studies that have found no significant increases in vaccination coverage over previous seasons, according to the Behavioral Risk Factor Surveillance System from selected states in the 2008–2009 season. Additionally, estimated seasonal influenza vaccination coverage (and 95% confidence intervals [CIs]) varied by race/ethnicity as follows: non-Hispanic white 69.0% (95% CI 67.1, 70.9), non-Hispanic black 56.3% (95% CI 45.0, 66.9), Hispanic 65.8% (95% CI 53.1, 76.6), and other 58.4% (95% CI 46.4, 69.5).4 In fact, racial/ethnic disparities in adult influenza immunization rates have persisted for many years.5–14 One overarching goal of Healthy People 2010 was to eliminate health disparities15 and, within the focus area of immunization and infectious diseases, to increase to 90% the overall proportion of seniors who are vaccinated annually against influenza.16 To achieve these national goals by 2020, significant enhancements in local immunization delivery systems will be required.
Although several prior projects in Monroe County, New York, such as the Medicare Influenza Vaccination Demonstration, successfully increased adult influenza vaccine coverage rates in individual practices and across the community,17,18 large racial disparities persisted. For example, in 2002, only 38% of the county's African American seniors received influenza vaccination compared with 71% of white seniors.19 This disparity in rates of vaccination mirrors the patterns found in national and state data.
The Task Force on Community Preventive Services20 (hereafter referred to as “Task Force”) disseminated broad categories of evidence-based strategies to improve immunization coverage in communities. These strategies included increasing community demand for vaccinations, enhancing access to vaccination services, and implementing provider- or system-based interventions,21 such as patient reminder/recall and health-care provider prompts about vaccinations.22–25 The Task Force recommended combination strategies, including interventions from more than one of the aforementioned categories. Most studies of immunization strategies have used single interventions and applied the interventions in single practices rather than across a community or network of practices.26–28 To achieve public health goals of raising immunization rates and eliminating disparities across an entire community, it is important to evaluate the effectiveness of interventions across multiple and diverse practice settings, particularly those that serve vulnerable populations.
The Racial and Ethnic Adult Disparities in Immunization Initiative (READII) was a two-year project conducted in five U.S. communities to demonstrate promising strategies to increase vaccination rates for African American and Hispanic seniors.29 In Rochester, New York (population 220,000 within Monroe County's total population of 735,000), the READII team developed a two-part program: (1) a community action plan that included a broad-based communication campaign implemented through community organizations along with enhanced vaccine delivery through nontraditional venues, and (2) a practice-based intervention in multiple community health centers and hospital clinics. To study the effectiveness of the latter part of the program, we designed and implemented a randomized controlled trial of this intervention, which involved a stepwise combination of patient tracking and reminder/recall/outreach as well as provider reminders. This combination strategy has been found to improve childhood vaccination rates30 and to reduce community racial/ethnic disparities when implemented across multiple inner-city practices that serve minority children.31 This intervention has not been applied previously to adults across multiple practice settings.
The specific study objectives were to evaluate, in a population of seniors served by urban primary care centers (PCCs), the effect of the practice-based intervention on (1) influenza immunization rates and (2) disparities in vaccination rates by race/ethnicity and insurance status.
METHODS
Study design
The design was a randomized controlled trial, with individual seniors randomized within PCCs to intervention or standard-of-care control groups.
Participants
The study took place in Rochester, which, according to the U.S. Census Bureau's 2005–2009 American Community Survey 5-Year Estimates,32 comprised 208,001 people. Respondents reported their race as the following: 48% white, 41% black or African American, 8% another single race, or 3% more than two races. Hispanic or Latino of any race comprised 14% of the population. Nine percent of people were aged ≥65 years. The per-capita income for the city (in 2008 inflation-adjusted dollars) was $17,876; per-capita income overall in the U.S. was $27,466. In the city, 29% of individuals lived below the federal poverty level (FPL); for the U.S. overall, 13% of the population was below the FPL. We identified seven large urban PCCs in Rochester that together serve a high proportion of the city's African American and Hispanic seniors and approached the medical director of each PCC for participation. All but one agreed to participate, including four neighborhood health centers (two internal medicine and two family medicine), one internal medicine hospital clinic, and one hospital-associated internal medicine-pediatric practice. All active patients of participating PCCs who were aged ≥65 years and residents of New York were eligible for randomization. The PCCs' definitions of an “active” patient varied, but all included at least one visit in the previous two to five years. Patients who had received influenza immunization earlier within the influenza vaccination season, before our influenza intervention began, were not eligible.
Recruitment
PCCs were recruited to participate during the summer of 2002, and patient demographic data collection took place as allowed by each PCC's Institutional Review Board. Because influenza vaccine shipments arrived at PCCs at different times, the intervention began on different dates between September 29, 2003, and October 13, 2003. The intervention ended on January 22, 2004. Chart reviews for vaccination outcome took place during the subsequent two months.
Sample size
Within participating PCCs, all eligible patients were enrolled. Sample size calculations determined that a sample of 170 patients per study group would be sufficient to demonstrate a clinically meaningful 15% difference in vaccination rates (with control rates of 50%, p<0.05, power of 0.8 and a two-tailed test) with study subjects compared with standard-of-care controls. However, because this study was part of a broader community project, and we were interested in evaluating the intervention in multiple sites and across racial/ethnic and insurance subgroups, we enrolled many more subjects than the sample size calculation would have required.
Randomization and blinding
All patient names and demographic variables were downloaded from the PCCs' patient information systems into the study site-specific database. Within each PCC, patients were automatically assigned to the intervention group if the last digit of their Social Security number was odd and to the control group if the number was even.33 Use of patient reminders/recall precluded blinding of either patients or outreach workers, and use of provider prompts precluded blinding PCC staff. Because outreach workers conducted the patient tracking/reminder/recall/outreach intervention, the health-care providers tended to be unaware of group assignment for an individual patient except during health-care visits if the patient chart included a provider prompt.
Outcomes and data collection
After the study intervention period, an outreach worker reviewed each patient's medical record for influenza immunization status, for both intervention and control groups. Patient age, race/ethnicity, gender, and insurance status were obtained from the PCCs' information technology systems. Quality assurance checks were performed to ensure accuracy of chart reviews, and these demonstrated extremely high accuracy.
Interventions
The standard of care for this study was defined as each office's routine. Only one office reported sending patients any form of notification regarding influenza vaccination. In the preliminary office meetings, most providers indicated they did not have systems in place to remind them to evaluate immunization records during preventive, acute, or chronic follow-up visits. The standard of care in these offices reflected care typical of many primary care practices.34 For the READII intervention, four full-time peer outreach workers and a supervising social worker were trained in abstraction of vaccination records, human service and social work areas pertinent to the intervention, and use of the study database, which resembled an immunization registry. Each worked at more than one PCC, but each PCC had an identifiable primary outreach worker. The investigators recruited and supervised the outreach staff, who did not contribute to routine primary care tasks at the PCCs. Patients in the control group received routine care as per the PCCs' protocols. The intervention group received a staged intervention of patient tracking, provider reminders, patient recall, and outreach to patients, as detailed in the following sections.
Patient tracking.
Outreach workers identified eligible patients from PCC databases and tracked their immunization status by reviewing medical records and entering the data manually into the study database. Each outreach worker was responsible for tracking approximately 900 to 1,000 eligible patients.
Provider reminders.
As medical charts were reviewed, the charts of all patients in the intervention group were flagged with a full-page, brightly colored sheet reading, “REMEMBER! This patient needs influenza vaccine.” The reminder form included a field for providers to indicate vaccine administration or, if not given, the reason it was not given (e.g., a contraindication, patient refusal, provider forgot, no vaccine available, or vaccine received elsewhere).35
Patient reminders and recall.
Outreach workers mailed influenza immunization reminders to intervention patients. The format (letter or card) and wording of the study reminder was chosen by each PCC and, in each case, the reminder was clearly identified as having come from the PCC. One participating PCC declined this portion of the intervention because influenza vaccination reminders were already part of its standard of care.
Outreach to patients.
Outreach workers telephoned patients who had no routine appointment scheduled during the three-month flu-vaccine period and asked them to make an appointment. If the patient did not make an appointment within two weeks, the worker called again. The intervals for written and phone communication to patients were logged in the work-flow part of the READII database, so that each staff member had a new list of daily tasks needed to complete outreach to all eligible patients.
The goals of the calls were (1) to motivate patients to be vaccinated against influenza; (2) to motivate patients to discuss with their medical provider their concerns, values, and ambivalence about getting vaccinated; and (3) to make patients who refused vaccine feel respected and accepted. The approach was patient-centered36 and characterized by partnership building, empathy, and interpersonal sensitivity. Office visits were encouraged as a means to increase patient knowledge, address concerns, and clarify perceptions of health care. Transportation assistance (e.g., bus tokens and Medicaid taxis) was offered to patients who needed it. Although homebound patients could be vaccinated through preexisting visiting nurse services, only one patient was vaccinated at home through the study.
Participant flow
A total of 3,752 eligible subjects were randomized to intervention or control arms. Seven (0.35%) of the control subjects were mistakenly contacted by telephone or mail; all patients in the intervention group received at least the tracking part of the intervention. All subjects were included in intention-to-treat analyses. No subject was lost to follow-up; at the study's end, all subjects were assessed for vaccination status based on their medical record. Patients who died during the study period were analyzed as randomized. Only three of the 2,755 patients who met the inclusion criteria had already received influenza vaccine before the intervention began, and these patients were excluded from the study.
Statistical methods
For eligible patients, we used Chi-square tests to compare the control and intervention groups on gender, race/ethnicity, and insurance status; a Kruskal-Wallis test was used to compare the two groups with respect to age. Chi-square tests were used to compare the proportions of study participants in the intervention vs. control groups who were vaccinated by the end of the study and to test for immunization disparities by race/ethnicity and insurance within the intervention group. Logistic regression models were used to estimate the size of the effect of the intervention, both an unadjusted model and a model adjusting for age, gender, race/ethnicity, insurance status, and site. Chi-square tests and Fisher's exact tests were used to examine refusal rates in the intervention group.
Ethics
The Research Subjects Review Board of the University of Rochester and the human subjects review boards of each participating PCC approved this study in 2002 with a waiver of individual patient consent. The intervention was extended to all control subjects in the year after the study was completed (2004).
RESULTS
Baseline data
The number of patients (denominator) in the control group was 2,004 and in the intervention group was 1,748, as dictated by the intention-to-treat analysis. Of these 3,752 eligible subjects, 62% were female and the mean age was 74.2 years (standard deviation [SD] = 7.2). As recorded by the PCC, 50% were white, 33% were African American, 10% were Hispanic, and 7% were other race/ethnicity. Eighty-five percent of -subjects in both groups were covered by Medicare and 5% were covered by Medicaid, but not Medicare. The rest were covered by commercial insurance (5%) or had no insurance coverage (5%).
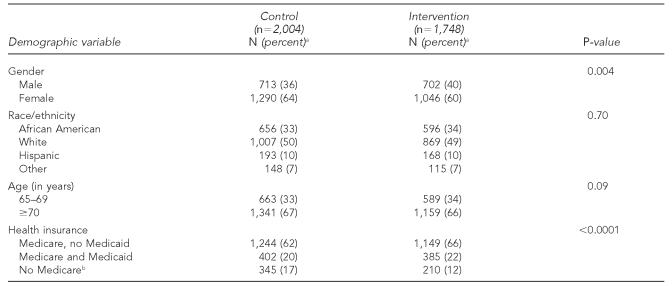
The intervention group had significantly more subjects covered by Medicare (p<0.0001) and a higher proportion of males (p=0.004) compared with the control group. There were no significant differences in race/ethnicity between the groups (Table 1).
Table 1.
Comparison of seniors at baseline in the control and intervention groups, by demographic variables: READII randomized controlled trial, Rochester, New York, 2002–2004
aThe percentages shown are based on the number of patients for whom the clinical record had the information. Because of missing data (e.g., gender or insurer) in some patients' clinical records, totals are not consistent.
bIncludes those with Medicaid only, commercial insurance, or no insurance.
READII = Racial and Ethnic Adult Disparities in Immunization Initiative
Vaccination outcomes
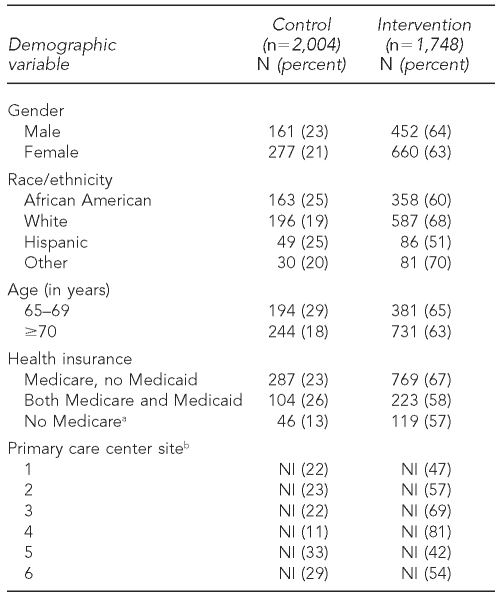
Table 2 shows the number and percentage of subjects with documented vaccination against influenza in the intervention and control groups during the study period. A significantly higher proportion of intervention group subjects than control group subjects (64% vs. 22%) were vaccinated. An unadjusted logistic regression analysis showed that patients in the intervention group were more than six times as likely to be vaccinated than patients in the control group (odds ratio [OR] = 6.25; 95% CI 5.41, 7.22; p<0.0001). Very similar results were obtained from the adjusted analysis (OR=6.27; 95% CI 5.42, 7.26; p<0.0001). Compared with control subjects, a significantly higher proportion of intervention subjects received influenza vaccination among subgroups of seniors according to gender, race/ethnicity, age, and insurance status (p<0.0001 for each subgroup), and the intervention was effective at all PCC sites (Table 2).
Table 2.
Number and proportion of seniors in the control and intervention groups who were vaccinated against influenza, by demographic variables: READII randomized controlled trial, Rochester, New York, 2002–2004
aIncludes those with Medicaid only, commercial insurance, or no insurance.
bAbsolute numbers are not included to maintain the confidentiality of study participants and the anonymity of the primary care centers; thus, only percentages are reported.
READII = Racial and Ethnic Adult Disparities in Immunization Initiative
NI = not included
Although the rates of immunization for all subgroups of the intervention group were much higher than those of the control group, racial/ethnic disparities were not eliminated within the intervention group. Considering only the intervention group, Table 2 illustrates that disparities in immunization rates by race/ethnicity (p<0.0001) and insurance (p=0.0005) were not overcome in the single influenza season intervention period. In particular, Hispanic seniors had the lowest rate of immunization.
Patient report of having recently received influenza vaccine at a public site was recorded as evidence of vaccination; however, this occurred for only 3.9% of intervention subjects and 1.8% of control subjects.
Ancillary analyses
Three percent of the 1,748 subjects in the intervention group refused vaccination. Females were significantly more likely to refuse vaccination than males (3.7% vs. 1.9%, p=0.0236). Although African American and white seniors appeared to have higher refusal rates than Hispanic seniors and those of other races/ethnicities (African American 3.5%, white 3.2%, Hispanic 0.6%, and other races 1.7%), these differences were not statistically significant (p=0.18) (data not shown).
DISCUSSION
In this study, a system-level intervention proved to be highly effective in increasing influenza vaccination rates across a large population of urban seniors. Seniors in the intervention group from a variety of health-care centers were six times as likely to receive influenza vaccine than those in the control group who received the standard of care; however, there was considerable variation in the success of the intervention, with one site achieving an influenza vaccination rate of >80% and two sites achieving vaccination rates of only 40%–50%. As a randomized controlled trial, our study extends published evidence of the effect of patient reminder/recall37 and provider prompts in individual practices and suggests that this program can be effective when implemented in a variety of community health-care sites serving diverse adult populations.
It is important to note that all practices were urban sites primarily serving impoverished seniors, with many racial/ethnic minority patients. The fact that the control group influenza immunization rates were substantially lower than national averages for minority seniors testifies to the acute vulnerability of the study population. Many of the PCCs had substantial financial challenges as they served a vulnerable population, yet the intervention was effective in each PCC. Although the intervention was not differentially applied to racial/ethnic minority patients within practices, because the participating practices served a high percentage of the county's minority patients, it is possible that application of this intervention could lead to a decrease in county-wide racial/ethnic disparities in vaccination rates. Even though racial/ethnic disparities in immunization rates were not completely eliminated within the intervention group, they were substantially narrower than the 33-point difference measured in a community-wide study in 2002.19
Fiscella and Holt have shown that, in age-adjusted analyses, minority groups had statistically lower rates of claims for several preventive measure procedures, including influenza vaccination. After controlling for number of primary care visits, low income, low education level, supplementary insurance, health status, and year, minority status remained significantly associated only with colorectal cancer screening and influenza vaccinations (OR=0.56; 95% CI 0.49, 0.64).38
It has been suggested that disparities are caused, at least in part, by minority seniors tending to refuse influenza vaccinations,39 but in this study the rate of refusal was low overall and did not differ for African American and white seniors. The low rate of refusal suggests that other factors account for the finding that many seniors still were not vaccinated despite a relatively aggressive intervention. It is known that factors resulting in racial/ethnic disparities in access to health care are complex and multifactorial40 and that key factors in the receipt of preventive care include system-related barriers, economic barriers, and sociocultural components.39,41
Previous studies have shown that patient navigation—a process by which an individual guides patients with health-related problems through barriers in the complex care system—can decrease racial/ethnic disparities in cancer care.42 Other studies have demonstrated that office-based multi-method interventions in inner-city practices can increase childhood immunization rates.31,43 The findings in this study of adult influenza immunization were more striking, possibly because the baseline immunization rate tended to be lower in adults than in children.
Local anecdotal reports that both healthy and frail seniors attending health fairs ignored influenza vaccination promotion messages from the health department or insurers because “they don't know me” led us to believe that the READII Rochester messages should come directly from seniors' own health-care centers. The personnel calling the seniors asked about barriers to receipt of the vaccination and had backup from social workers who could help obtain services to overcome many commonly identified barriers. Feedback received from patients regarding the influenza vaccination reminder calls included statements of appreciation for caring about their health. The intervention also was designed to be palatable to health-care professionals. Supervision of the study personnel was centralized, minimizing effort on the part of the PCCs, but the centers could alter follow-up protocols to reflect their needs.
Limitations
Our study had limitations both in terms of internal validity and generalizability. Despite randomization, the intervention group had a higher proportion of males and patients covered by Medicare than the control group. This may be because, prior to the late 1960s, Social Security numbers were not distributed centrally, but by local offices that used different rules. For example, some offices gave odd numbers only to people who worked in the documented economy (as opposed to those who are unpaid, barter, or whose income goes unreported). However, our multivariate analysis controlled for these factors, preventing weakening of the internal validity of the study.
The effect of provider reminders placed on charts of patients in the intervention group as well as the knowledge about the study may have prompted greater vaccination of control subjects than would otherwise have occurred, leading to an underestimate of the intervention effect (i.e., a conservative bias). Conversely, although providers understood that not all patients due for vaccination would have the point-of-care prompt, in some instances providers may have been less likely to check the patient's immunization record because they assumed that the absence of a reminder indicated prior vaccination. However, in the preliminary office meetings, most providers indicated they did not routinely evaluate immunization records during preventive, acute, or chronic follow-up visits.
Despite study team efforts, some data regarding influenza vaccinations given in public clinics were not available. However, this inaccuracy would be likely to be the same in both groups.
An important limitation was our inability to distinguish the relative impact of different parts of the multi-component intervention. Specifically, we could not distinguish the impact of provider prompts from patient reminders. The Task Force on Community Preventive Services recognized that such multifaceted interventions present a challenge in evaluation of subcomponents.20 Increasingly in the quality improvement field, multipart interventions are recommended.44,45
Generalizability
Because the intervention was carried out in a variety of inner-city health-care settings, it may be generalizable to similar practice settings. The study reports on only one year of intervention. Repetition could make this quality improvement program either more successful, as the strategies became integrated as the standard of care, or less successful, as attention shifts to other pressures of practice.46,47 Similarly, this centrally supervised program may not be generalizable to an intervention supervised by individual health-care centers. A health-care center-based program may be more enthusiastically embraced and integrated, but alternatively could be more easily diluted and diverted by the pressures of primary care practice. Although our intervention included central supervision, the outreach workers were integrated into the PCCs and were perceived by the patients and providers to be part of the PCCs. Influenza vaccine shortages and delays, of course, would be likely to result in lower overall vaccination coverage.
CONCLUSIONS
A combined intervention of patient tracking, recall, and outreach as well as provider reminders in a group of inner-city primary care offices substantially increased influenza immunization rates among seniors, compared with standard-of-care control subjects.
The implications for vaccine policy makers are that (1) this multifaceted intervention involving components that have worked in individual practices can be successfully applied on a community-wide level, even in urban practices with varying characteristics; (2) it may be difficult to achieve rates of more than 60%–70% influenza vaccination coverage in primary care settings even with this very intensive strategy; (3) a large-scale intervention aimed at urban practices may decrease county-wide disparities by increasing immunization rates among urban populations comprising a disproportionate number of minority individuals; and (4) this model, which is closely related to patient navigation, may be applicable to increasing rates of other preventive health services in urban practices. To sustain such a community-based program, additional external resources may be needed to support interventions to help busy urban primary care practices increase influenza immunization rates.
Footnotes
Funding for the evaluation of this program was supplied by the Centers for Disease Control and Prevention (CDC) National Immunization Program. The authors thank the participating medical centers and the outreach workers, Juanita Alvarado, Barbara McNair, Lilleith Nisbeth, and Teretha Wilson, who made this program possible. The authors also thank the CDC National Immunization Program personnel, Tamara Kicera and Pascale Wortley, and New York State Department of Health leaders who were a consistent resource to Rochester's Racial and Ethnic Adult Disparities in Immunization Initiative.
The findings and conclusions presented in this article are those of the authors and do not necessarily represent the views of CDC.
REFERENCES
- 1.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–86. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–40. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 3.McBean AM, Hebert PL. New estimates of influenza-related pneumonia and influenza hospitalizations among the elderly. Int J Infect Dis. 2004;8:227–35. doi: 10.1016/j.ijid.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Influenza vaccination coverage among children and adults—United States, 2008–09 influenza season. MMWR Morb Mortal Wkly Rep. 2009;58(39):1091–5. [PubMed] [Google Scholar]
- 5.State-specific influenza vaccination coverage among adults aged ≥18 years—United States, 2003–04 and 2005–06 influenza seasons. MMWR Morb Mortal Wkly Rep. 2007;56(37):953–9. [PubMed] [Google Scholar]
- 6.Vaccination levels among Hispanic and non-Hispanic whites aged ≥65 years—Los Angeles County, California, 1996. MMWR Morb Mortal Wkly Rep. 1997;46(49):1165–8. [PubMed] [Google Scholar]
- 7.Influenza and pneumococcal vaccination levels among persons aged ≥65 years—United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50(25):532–7. [PubMed] [Google Scholar]
- 8.Marin MG, Johanson WG, Jr, Salas-Lopez D. Influenza vaccination among minority populations in the United States. Prev Med. 2002;34:235–41. doi: 10.1006/pmed.2001.0983. [DOI] [PubMed] [Google Scholar]
- 9.Bonito AJ, Lenfestey NF, Eicheldinger C, Iannacchione VG, Campbell L. Disparities in immunizations among elderly Medicare beneficiaries, 2000 to 2002. Am J Prev Med. 2004;27:153–60. doi: 10.1016/j.amepre.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Egede LE, Zheng D. Racial/ethnic differences in influenza vaccination coverage in high-risk adults. Am J Public Health. 2003;93:2074–8. doi: 10.2105/ajph.93.12.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Racial/ethnic disparities in influenza and pneumococcal vaccination levels among persons aged ≥65 years—United States, 1989–2001. MMWR Morb Mortal Wkly Rep. 2003;52(40):958–62. [PubMed] [Google Scholar]
- 12.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Schneider EC, Cleary PD, Zaslavsky AM, Epstein AM. Racial disparity in influenza vaccination: does managed care narrow the gap between African Americans and whites? JAMA. 2001;286:1455–60. doi: 10.1001/jama.286.12.1455. [DOI] [PubMed] [Google Scholar]
- 14.Liao Y, Tucker P, Okoro CA, Giles WH, Mokdad AH, Harris VB. REACH 2010 surveillance for health status in minority communities—United States, 2001–2002. MMWR Surveill Summ. 2004;53(6):1–36. [PubMed] [Google Scholar]
- 15.Department of Health and Human Services (US). Healthy People 2010: what are its goals? [cited 2010 Jan 4]. Available from: URL: http://www.healthypeople.gov/2010/About/goals.htm.
- 16.Department of Health and Human Services (US). Healthy People 2010: objective 14-29. Increase the proportion of adults who are vaccinated annually against influenza and ever vaccinated against pneumococcal disease. [cited 2010 Jan 4]. Available from: URL: http://www.healthypeople.gov/2010/Document/HTML/uih/uih_4.htm.
- 17.Bennett NM, Lewis B, Doniger AS, Bell K, Kouides R, LaForce FM, et al. A coordinated, communitywide program in Monroe County, New York, to increase influenza immunization rates in the elderly. Arch Intern Med. 1994;154:1741–5. [PubMed] [Google Scholar]
- 18.Barker WH, Bennett NM, LaForce FM, Waltz EC, Weiner LB. “McFlu.” The Monroe County, New York, Medicare vaccine demonstration. Am J Prev Med. 1999;16(3 Suppl):118–27. doi: 10.1016/s0749-3797(98)00153-6. [DOI] [PubMed] [Google Scholar]
- 19.Monroe County Department of Public Health. Leading health indicators, Monroe County. 2002. [cited 2010 Jan 15]. Available from: URL: http://www.monroecounty.gov/p/health-LeadingIndicators2002.pdf.
- 20.Vaccine-preventable diseases: improving vaccination coverage in children, adolescents, and adults. A report on recommendations from the Task Force on Community Preventive Services. MMWR Recomm Rep. 1999;48(RR-8):1–15. [PubMed] [Google Scholar]
- 21.Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, et al. Effect of patient reminder/recall interventions on immunization rates: a review. JAMA. 2000;284:1820–7. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 22.Shevlin JD, Summers-Bean C, Thomas D, Whitney CG, Todd D, Ray SM. A systematic approach for increasing pneumococcal vaccination rates at an inner-city public hospital. Am J Prev Med. 2002;22:92–7. doi: 10.1016/s0749-3797(01)00408-1. [DOI] [PubMed] [Google Scholar]
- 23.Sabnis SS, Pomeranz AJ, Amateau MM. The effect of education, feedback, and provider prompts on the rate of missed vaccine opportunities in a community health center. Clin Pediatr (Phila) 2003;42:147–51. doi: 10.1177/000992280304200208. [DOI] [PubMed] [Google Scholar]
- 24.Willis BC, Ndiaye SM, Hopkins DP, Shefer A, Task Force on Community Preventive Services. Improving influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among adults aged <65 years at high risk: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep. 2005;54(RR05):1–11. [PubMed] [Google Scholar]
- 25.Ndiaye SM, Hopkins DP, Shefer AM, Hinman AR, Briss PA, Rodewald L, et al. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. Am J Prev Med. 2005;28(5 Suppl):248–79. doi: 10.1016/j.amepre.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 26.Bordley WC, Chelminski A, Margolis PA, Kraus R, Szilagyi PG, Vann JJ. The effect of audit and feedback on immunization delivery: a systematic review. Am J Prev Med. 2000;18:343–50. doi: 10.1016/s0749-3797(00)00126-4. [DOI] [PubMed] [Google Scholar]
- 27.Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, et al. Effect of patient reminder/recall interventions on immunization rates: a review. JAMA. 2000;284:1820–7. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 28.Szilagyi P, Vann J, Bordley C, Chelminski A, Kraus R, Margolis P, et al. Interventions aimed at improving immunization rates. Cochrane Database Syst Rev. 2002;(4):CD003941. doi: 10.1002/14651858.CD003941. [update in: Cochrane Database Syst Rev 2005;(3):CD003941] [DOI] [PubMed] [Google Scholar]
- 29.Kicera TJ, Douglas M, Guerra FA. Best-practice models that work: the CDC's Racial and Ethnic Adult Disparities Immunization Initiative (READII) programs. [cited 2010 Jan 15]. Available from: URL: http://www.ishib.org/journal/15-2s3-17-2.pdf. [PubMed]
- 30.Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics. 1999;103:31–8. doi: 10.1542/peds.103.1.31. [DOI] [PubMed] [Google Scholar]
- 31.Szilagyi PG, Schaffer S, Shone L, Barth R, Humiston SG, Sandler M, et al. Reducing geographic, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics. 2002;110:e58. doi: 10.1542/peds.110.5.e58. [DOI] [PubMed] [Google Scholar]
- 32.Census Bureau (US). Fact sheet: 2005–2009 American Community Survey 5-year estimates. [cited 2011 May 2]. Available from: URL: http://factfinder.census.gov/servlet/ACSSAFFFacts?_submenuId=factsheet_0&_sse=on.
- 33.Docusearch Investigations. SSN finder: structure of Social Security numbers. [cited 2011 Mar 14]. Available from: URL: http://www.docusearch.com/ssn-finder-structure-of-social-security-numbers.html.
- 34.Szilagyi PG, Shone LP, Barth R, Kouides RW, Long C, Humiston SG, et al. Physician practices and attitudes regarding adult immunizations. Prev Med. 2005;40:152–61. doi: 10.1016/j.ypmed.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 35.Szilagyi PG, Rodewald LE, Humiston SG, Pollard L, Klossner K, Jones AM, et al. Reducing missed opportunities for immunizations: easier said than done. Arch Pediatr Adolesc Med. 1996;150:1193–200. doi: 10.1001/archpedi.1996.02170360083014. [DOI] [PubMed] [Google Scholar]
- 36.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20:953–7. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thomas RE, Russell ML, Lorenzetti DL. Systematic review of interventions to increase influenza vaccination rates of those 60 years and older. Vaccine. 2010;28:1684–701. doi: 10.1016/j.vaccine.2009.11.067. [DOI] [PubMed] [Google Scholar]
- 38.Fiscella K, Holt K. Impact of primary care patient visits on racial and ethnic disparities in preventive care in the United States. J Am Board Fam Med. 2007;20:587–97. doi: 10.3122/jabfm.2007.06.070053. [DOI] [PubMed] [Google Scholar]
- 39.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40:517–37. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. In: Smedley BD, Stith AY, Nelson AR, editors. Washington: National Academies Press; 2002. [PubMed] [Google Scholar]
- 41.Fiscella K. Commentary—anatomy of racial disparity in influenza vaccination. Health Serv Res. 2005;40:539–49. doi: 10.1111/j.1475-6773.2005.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ. 2006;21(1 Suppl):S11–4. doi: 10.1207/s15430154jce2101s_4. [DOI] [PubMed] [Google Scholar]
- 43.Hambidge SJ, Davidson AJ, Phibbs SL, Chandramouli V, Zerbe G, LeBaron CW, et al. Strategies to improve immunization rates and well-child care in a disadvantaged population: a cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2004;158:162–9. doi: 10.1001/archpedi.158.2.162. [DOI] [PubMed] [Google Scholar]
- 44.Ornstein S, Jenkins RG, Nietert PJ, Feifer C, Roylance LF, Nemeth L, et al. A multimethod quality improvement intervention to improve preventive cardiovascular care: a cluster randomized trial. Ann Intern Med. 2004;141:523–32. doi: 10.7326/0003-4819-141-7-200410050-00008. [DOI] [PubMed] [Google Scholar]
- 45.Ornstein S, Nietert PJ, Jenkins RG, Wessell AM, Nemeth LS, Feifer C, et al. Improving diabetes care through a multicomponent quality improvement model in a practice-based research network. Am J Med Qual. 2007;22:34–41. doi: 10.1177/1062860606295206. [DOI] [PubMed] [Google Scholar]
- 46.Feifer C, Nemeth L, Nietert PJ, Wessell AM, Jenkins RG, Roylance L, et al. Different paths to high-quality care: three archetypes of top-performing practice sites. Ann Fam Med. 2007;5:233–41. doi: 10.1370/afm.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Institute of Medicine, Board on Health Care Services, Forum on the Science of Health Care Quality Improvement and Implementation. Advancing quality improvement research: challenges and opportunities—workshop summary. Washington: National Academies Press; 2007. [cited 2010 Jan 4]. Also available from: URL: http://books.nap.edu/openbook.php?record_id=11884&page=1. [Google Scholar]