Abstract
Objective
We evaluated the association between parents' beliefs about vaccines, their decision to delay or refuse vaccines for their children, and vaccination coverage of children at aged 24 months.
Methods
We used data from 11,206 parents of children aged 24–35 months at the time of the 2009 National Immunization Survey interview and determined their vaccination status at aged 24 months. Data included parents' reports of delay and/or refusal of vaccine doses, psychosocial factors suggested by the Health Belief Model, and provider-reported up-to-date vaccination status.
Results
In 2009, approximately 60.2% of parents with children aged 24–35 months neither delayed nor refused vaccines, 25.8% only delayed, 8.2% only refused, and 5.8% both delayed and refused vaccines. Compared with parents who neither delayed nor refused vaccines, parents who delayed and refused vaccines were significantly less likely to believe that vaccines are necessary to protect the health of children (70.1% vs. 96.2%), that their child might get a disease if they aren't vaccinated (71.0% vs. 90.0%), and that vaccines are safe (50.4% vs. 84.9%). Children of parents who delayed and refused also had significantly lower vaccination coverage for nine of the 10 recommended childhood vaccines including diphtheria-tetanus-acellular pertussis (65.3% vs. 85.2%), polio (76.9% vs. 93.8%), and measles-mumps-rubella (68.4% vs. 92.5%). After adjusting for sociodemographic differences, we found that parents who were less likely to agree that vaccines are necessary to protect the health of children, to believe that their child might get a disease if they aren't vaccinated, or to believe that vaccines are safe had significantly lower coverage for all 10 childhood vaccines.
Conclusions
Parents who delayed and refused vaccine doses were more likely to have vaccine safety concerns and perceive fewer benefits associated with vaccines. Guidelines published by the American Academy of Pediatrics may assist providers in responding to parents who may delay or refuse vaccines.
From the early 1940s to 1952, annual incidence rates of polio surged1,2 and the American public became terrified3 by outbreaks that occurred in urban and rural areas throughout the U.S.1 In April 1954, a nationwide mass vaccination campaign was launched, and the incidence rate of polio decreased quickly and dramatically.1 Scientists believed that their credibility and the weight of the scientific evidence that demonstrated the safety and efficacy of the Salk vaccine would be sufficient to convince hesitant parents, who had concerns about vaccine safety or efficacy, to vaccinate their children.4,5 Yet, parents' concerns about the vaccine persisted and many refrained from vaccinating their children.6–10 The resurgence of more polio epidemics in 19581 taught public health workers that development of safe and effective vaccines alone was not sufficient to prevent epidemics. Rather, they realized that efforts to prevent epidemics would be more effective if they understood the reasons why parents failed to vaccinate their children and knew how to more effectively persuade them to vaccinate their children.11
In response, Irwin Rosenstock, Mayhew Derryberry, and Barbara Carriger of the U.S. Public Health Service conducted a systematic review of the existing literature to learn why parents failed to vaccinate their children with the Salk polio vaccine. Their findings were published in Public Health Reports11 and showed that there were four psychosocial domains that influenced parents' decisions to vaccinate their children: (1) susceptibility—parents' assessment of their child' risk of getting polio; (2) seriousness—their assessment of whether polio was a sufficient health concern to warrant vaccination; (3) efficacy and safety—their assessment of whether vaccinating their child can reduce the chance of their child' getting polio, and whether the vaccine is safe; and (4) social pressures and convenience—the concerns and influences that facilitated or discouraged their decision to get their child vaccinated.
These factors soon became the basis for the celebrated Health Belief Model that has been used throughout public health to explain why people adopt behaviors that lead to healthy lives.12–19 Insofar as one of the first applications of the Health Belief Model was to learn about barriers to polio vaccination coverage in the 1950s, we return to considering how this model might elucidate the barriers to increasing current vaccination coverage.
Today, 60 years after the end of the polio epidemics in the U.S., incidence rates of vaccine-preventable diseases (VPDs) in the U.S. have declined to all-time lows.20 However, some parents continue to have concerns about administering all recommended vaccines to their children. Today, parents' vaccine hesitancy may have been increased by celebrities' public airing of their own concerns about vaccines21–23 and a vocal and active anti-vaccine movement24 that has encouraged parents to refuse immunizations for their children.25 Also, as the number of recommended vaccines has increased, alternative vaccination schedules26,27 have been proposed, based on the assumption that spreading out vaccine administration over time and advising fewer injections at each visit would somehow result in fewer adverse events and, therefore, be safer. Unfortunately, parents' decisions to delay or refuse vaccines have been shown to be associated with increased risk of VPDs for both individuals and communities.28,29
This article describes methods based on the Health Belief Model for evaluating the association between parents' beliefs about vaccines, their decision to delay or refuse vaccines for their children, vaccination coverage, and reasons given for their decision to delay or refuse vaccination.
METHODS
The National Immunization Survey
Data are collected in the National Immunization Survey (NIS) in two phases: a telephone survey to identify households that have children aged 19–35 months, followed by a survey mailed to those children's vaccination providers. Of the 17,313 children aged 19–35 months sampled by the NIS in 2009, we analyzed data on a subsample of 11,206 children who were aged 24–35 months and who had adequate provider data returned from the mail survey.
In 2009, 99.4% of respondents interviewed in the NIS telephone survey were either parents or grandparents and were determined to be the most knowledgeable person in the household about the vaccination status of the age-eligible children in the household. In 2009, the response rate of the telephone portion of the NIS was 64.0%, and among sampled children aged 19–35 months with a completed NIS telephone interview, 69.0% had an adequate provider-reported vaccination history returned from the mail that could be used to evaluate vaccination status. Smith et al.30 provide a detailed description of the statistical methods used by the NIS, which has been approved by the Centers for Disease Control and Prevention (CDC) Institutional Review Board. All of the questions asked in the NIS are available for review.31
Ascertainment of parental delay or refusal of recommended vaccine doses
In the 2009 NIS, parents were asked a question about whether they ever decided to delay a vaccine dose for their children, and then asked another question about whether they ever decided to not get or refuse the administration of a dose. We categorized parents into one of four possible delay/refusal categories depending on whether they reported (1) neither delaying nor refusing, (2) delaying but not refusing, (3) refusing and not delaying, or (4) delaying and refusing. In this article, we refer to parents who delayed but did not refuse as parents who “only delayed,” and parents who refused but did not delay as parents who “only refused.” Parents who reported delaying or refusing vaccines and could remember the name of the vaccines that were delayed/refused were asked questions about the reasons why they delayed or refused those vaccines.
Assessment of parents' beliefs about vaccines
To assess parents' beliefs about vaccines, we used current data from the 2009 NIS to correlate parents' report of delay/refusal with the four psychosocial domains that index the Health Belief Model. To measure those domains, parents were read 11 statements to provide a verbatim response whether on a scale of zero to 10, where zero meant strongly disagree and 10 meant strongly agree, they agreed or disagreed with the statements. In our analysis, we assumed that respondents who provided a verbatim response of ≥7 were more likely to agree with the statements than those who gave a response of ≤6. For convenience, we refer to parents who provided a verbatim response of ≥7 as parents who agreed. Table 1 lists the statements that correspond to each of the four psychosocial domains.
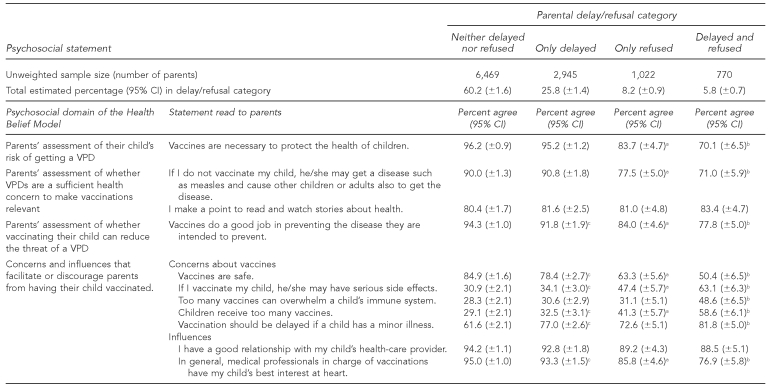
Table 1.
Percentage of parents agreeing to psychosocial statements, among parents with children aged 24–35 months, by parental vaccine-delay/refusal category: 2009 National Immunization Survey
aCompared with parents who only delayed, the percentage of parents who agreed with the statement is significantly different among parents who only refused, p<0.05.
bCompared with parents who only refused, the percentage of parents who agreed with the statement is significantly different among parents who delayed and refused, p<0.05.
cCompared with parents who neither delayed nor refused, the percentage of parents who agreed with the statement is significantly different among parents who only delayed, p<0.05.
CI = confidence interval
VPD = vaccine-preventable disease
Evaluation of vaccination status
For each sampled child, we evaluated vaccination status as of their 24-month birthday and refer to this as vaccination status at aged 24 months hereafter. Provider-reported vaccination histories from the mail survey portion of the NIS were used to determine vaccination status. The CDC goal is for children to be up-to-date (UTD) on all vaccines recommended for routine administration by aged 2 years.
Because we focused on vaccination coverage at aged 24 months, all of our analyses are restricted to children sampled by the NIS who were aged 24–35 months. Sampled children were defined as UTD on individual vaccines if their provider-reported vaccination history indicated they were administered ≥4 doses of diphtheria-tetanus-acellular pertussis (DTaP) or diphtheria-tetanus-pertussis (DTP) vaccine, ≥3 doses of polio vaccine, ≥1 dose of measles-mumps-rubella (MMR) vaccine, ≥3 doses of Haemophilus influenzae type b (Hib) vaccine, ≥3 doses of hepatitis B (Hep B) vaccine, ≥1 dose of varicella (VAR) vaccine, ≥4 doses of heptavalent pneumococcal conjugate (PCV7) vaccine; and ≥2 doses of hepatitis A (Hep A) vaccine. Children were determined to be UTD for the rotavirus vaccine if they had received either ≥2 doses of Rotarix® (GlaxoSmithKline, Middlesex, United Kingdom) or ≥3 doses of any combination of Rotarix® or RotaTeq® (Merck & Co., Inc., Whitehouse Station, New Jersey). In 2009, sampled children aged ≥24 months were considered to be UTD if they were administered ≥3 doses of the seasonal influenza vaccine.
Also, we defined a child to be 4:3:1:3:3:1:4 UTD by 24 months if they had been administered the 19 doses that are required to be UTD on DTaP, polio, MMR, Hib, Hep B, VAR, and PCV7 vaccines by aged 24 months. To evaluate how parents' delay/refusal affected the degree to which their children were undervaccinated, we provide estimates of the average number of doses missed of the 19 doses that are required, among children who are not 4:3:1:3:3:1:4 UTD by 24 months. In this article, “vaccination coverage” refers to the estimated percentage of children who are UTD.
Statistical methods
All of our estimates were computed using the survey library32 of the R statistical software package,33 which allowed us to account for the NIS sampling weights, sampling design of the NIS, independence of sampling from year to year, and clustering of age-eligible children within households. The subsample of children aged 24–35 months was defined as a “domain of study” and analyzed using special statistical methods designed for complex surveys.32 All of our analyses pertain to the subsample of 11,206 children aged 24–35 months among the 17,313 children aged 19–35 months sampled by the NIS in 2009. Estimated percentages are reported along with their 95% confidence intervals (CIs), and differences in estimated percentages were considered to be statistically significant if a t-test used to compare estimates showed p<0.05.
RESULTS
In 2009, 60.2% (95% CI 61.6%) of parents neither delayed nor refused a dose of any recommended vaccine, 25.8% (95% CI 61.4%) only delayed one or more recommended vaccine doses, 8.2% (95% CI 60.9%) only refused one or more recommended vaccine doses, and 5.8% (95% CI 60.7%) both delayed and refused recommended vaccine doses (Table 1). Among children who were not 4:3:1:3:3:1:4 UTD by aged 24 months, the average number of missed doses was 7.7 (61.1) among children whose parents neither delayed nor refused, 6.3 (60.8) among children whose parents only delayed, 10.6 (61.9) among children whose parents only refused, and 9.7 (61.4) among children whose parents had both delayed and refused at least one dose of vaccine.
The Health Belief Model and evaluation of the association between delay or refusal and parents' beliefs and attitudes about vaccines
Generally, the consecutive ordering of parental delay/refusal—starting from parents who neither delayed nor refused vaccines, then to parents who only delayed, then to those who only refused, and finally to parents who both delayed and refused—defined a continuum that was associated with increasing vaccine hesitancy (Table 1). For example, with respect to influences that discourage parents from having their child vaccinated, compared with parents who neither delayed nor refused vaccines, parents who only delayed were significantly less likely to agree with the statement, “vaccines are safe” (78.4% vs. 84.9%, p<0.05). Further, compared with parents who only delayed, parents who only refused were significantly less likely to agree (63.3% vs. 78.4%, p<0.05), and compared with parents who only refused, parents who delayed and refused were significantly less likely to agree (50.4% vs. 63.3%, p<0.05). We observed a similarly progressive continuum associated with increasing vaccine hesitancy that was statistically significant in all four of the psychosocial domains of the Health Belief Model and in nine of the 11 questions asked to parents to gauge their attitudes about vaccines.
Moreover, compared with parents who neither delayed nor refused vaccines, parents who delayed and refused vaccines were significantly less likely to believe that vaccines are necessary to protect the health of children (70.1% vs. 96.2%, p<0.05); that their child might get a disease if they aren't vaccinated (71.0% vs. 90.0%, p<0.05); and that vaccines do a good job of preventing the diseases they are intended to prevent (77.8% vs. 94.3%, p<0.05).
Compared with parents who neither delayed nor refused vaccines, parents who delayed and refused vaccines were significantly more likely to believe that if they vaccinated their child, he/she might have serious side effects (63.1% vs. 30.9%, p<0.05); that too many vaccines can overwhelm a child' immune system (48.6% vs. 28.3%, p<0.05); that children receive too many vaccines (58.6% vs. 29.1%, p<0.05); and that vaccination should be delayed if a child has a minor illness (81.8% vs. 61.6%, p<0.05).
Also, compared with parents who neither delayed nor refused vaccines, parents who delayed and refused vaccines were significantly less likely to believe that they had a good relationship with their child' health-care provider (88.5% vs. 94.2%, p<0.05) and that medical professionals in charge of vaccinations have their child' best interest at heart (76.9% vs. 95.0%, p<0.05).
Compared with parents who neither delayed nor refused, those who only delayed, and those who only refused, we found that parents who refused and delayed vaccines were significantly more likely to report that their decision to vaccinate their children was influenced by a doctor or nurse (54.0% vs. 46.5%, 48.7%, and 47.1%, respectively, p<0.05), but we do not know whether that influence was for the better or worse. Finally, compared with parents who neither refused nor delayed vaccines and parents who only delayed vaccines, parents who only refused and parents who refused and delayed were significantly more likely to report that their decision to vaccinate was influenced by a practitioner of complementary or alternative medicine, such as a homeopath or a naturopath (0.7% and 1.7% vs. 3.8% and 5.4%, respectively, p<0.05).
The association between delay or refusal, parents' beliefs, and vaccination coverage
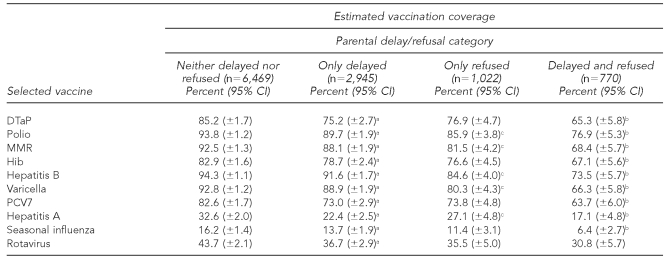
Generally, the same consecutive ordering of parental delay/refusal starting from parents who neither delayed nor refused vaccines, to parents who only delayed, to those who only refused, and then to parents who both delayed and refused defined a continuum that also was associated with decreasing vaccination coverage (Table 2). Among children aged 24–35 months in 2009, compared with the vaccination coverage of children whose parents only refused, estimated vaccination coverage was significantly lower for nine of the 10 recommended vaccines, the exception being the recently introduced rotavirus vaccine, for children whose parents both refused and delayed. Likewise, compared with the vaccination coverage of children whose parents only delayed, estimated vaccination coverage was significantly lower for five of the 10 recommended vaccines among children whose parents only refused. Finally, compared with the vaccination coverage of children whose parents neither delayed nor refused, estimated vaccination coverage was significantly lower for all 10 recommended vaccines among children whose parents only delayed (Table 2).
Table 2.
Estimated coverage by selected vaccine among children aged 24–35 months, by parental vaccine delay/refusal category: 2009 National Immunization Survey
aCompared with parents who neither delayed nor refused, the percentage is significantly different among parents who only delayed, p<0.05.
bCompared with parents who only refused, the percentage is significantly different among parents who delayed and refused, p<0.05.
cCompared with parents who only delayed, the percentage is significantly different among parents who only refused, p<0.05.
CI = confidence interval
DTaP = diphtheria-tetanus-acellular pertussis
MMR = measles-mumps-rubella
Hib = Haemophilus influenzae type b
PCV7 = heptavalent pneumococcal conjugate
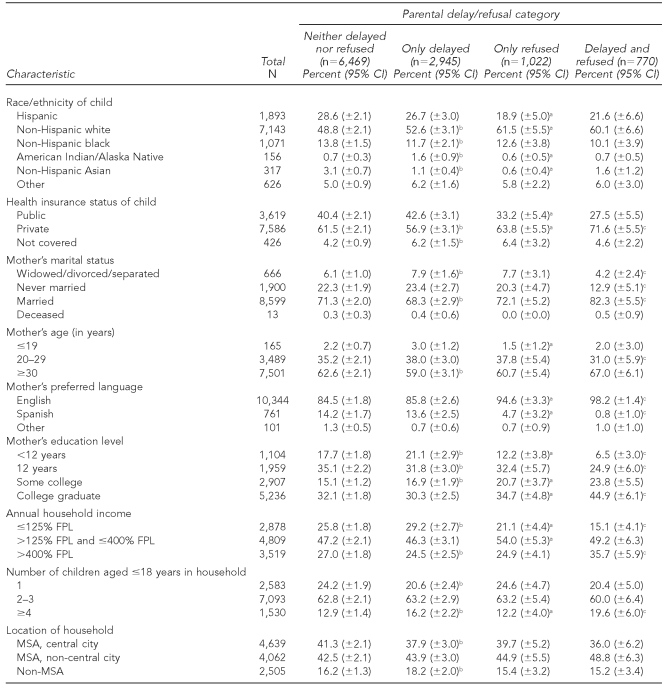
Child, maternal, and household characteristics associated with delay
Generally, the consecutive ordering of parental/delay refusal described previously defined a continuum that also was associated with factors related to higher socioeconomic status (Table 3). For example, children whose parents delayed and refused vaccines were -significantly more likely to live in a household with an annual income >400% of the federal poverty level;34 to have a mother who was married, ≥ 30 years of age, English-speaking, or a college graduate; to be covered by private health insurance; and to live in a household with ≥4 children who were 18 years of age or younger. Also, children whose parents delayed and refused were more likely to be of non-Hispanic white race/ethnicity than those who neither delayed nor refused (Table 3).
Table 3.
Selected child, maternal, and household sociodemographic characteristics among households with children aged 24–35 months, by parental vaccine delay/refusal category: 2009 National Immunization Survey
aCompared with parents who only delayed, the percentage of parents who agreed with the statement is significantly different among parents who only refused, p<0.05.
bCompared with parents who neither delayed nor refused, the percentage of parents who agreed with the statement is significantly different among parents who only delayed, p<0.05.
cCompared with parents who only refused, the percentage of parents who agreed with the statement is significantly different among parents who delayed and refused, p<0.05.
CI = confidence interval
FPL = federal poverty level
MSA = metropolitan statistical area
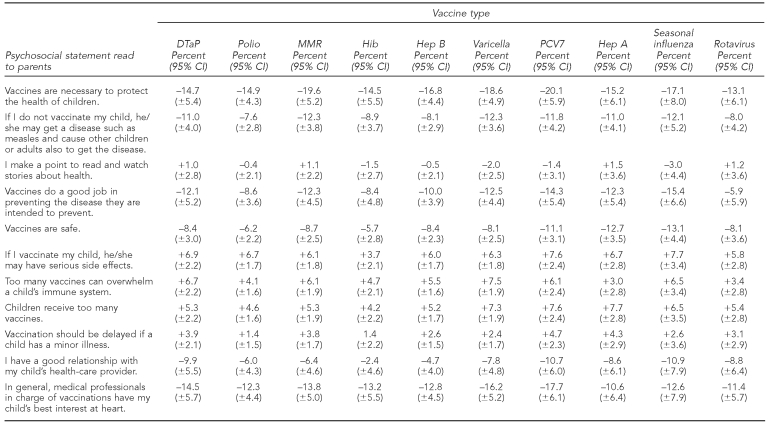
Explanatory power of the Health Belief Model
After adjusting for all child, maternal, and household characteristics, we found that children had significantly lower vaccination coverage for every vaccine if their parents were less likely to agree that (1) vaccines are necessary to protect the health of children; (2) if they do not vaccinate their child, he/she may get a disease; (3) vaccines do a good job of preventing the disease they are intended to prevent; (4) vaccines are safe; (5) they have a good relationship with their child's health-care provider; or (6) medical professionals in charge of vaccinations have their child' best interest at heart (Table 4). After adjusting for all child, maternal, and household characteristics, we also found that children had significantly lower vaccination coverage for every vaccine if their parents were more likely to agree that if they vaccinate their child, he/she may have serious side effects, and that too many vaccines can overwhelm a child' immune system (Table 4).
Table 4.
Estimated decrease (if −) or increase (if +) in vaccination coverage of children aged 24–36 months associated with parents' being less likely to agree with the psychosocial statement, after adjusting for all sociodemograpic variables, by vaccine type: 2009 National Immunization Survey
CI = confidence interval
DTaP = diphtheria-tetanus-acellular pertussis
MMR = measles-mumps-rubella
Hib = Haemophilus influenzae type b
Hep B = hepatitis B
PCV7 = heptavalent pneumococcal conjugate
Hep A = hepatitis A
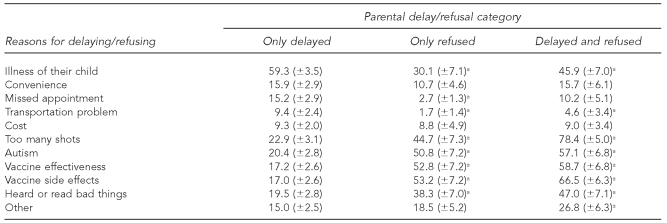
Reasons why parents delay or refuse vaccines
For some of the reasons parents gave for delaying or refusing vaccines, there was no apparent “natural” ordering according to parents' delay/refusal category. For example, compared with parents who delayed and refused, parents who only delayed vaccines were significantly more likely to say that they did so because their child was ill (59.3% vs. 45.9%, p<0.05). And, compared with parents who delayed and refused vaccines, parents who only refused vaccines were significantly less likely to say that the reason they did so was because their child was ill (30.1% vs. 45.9%, p<0.05) (Table 5).
Table 5.
Among parents with children aged 24–35 months, the estimated percentage and 95% confidence intervals of parents reporting selected reasons for delaying/refusing the administration of vaccine doses for their child, by delay/refusal category: 2009 National Immunization Survey
aThe indicated estimated percentage is significantly different from the estimated percentage among parents who only delayed, p<0.05.
However, the consecutive ordering of parental delay/refusal starting from parents who only delayed, to those who only refused, and then to parents who delayed and refused defined a continuum that was associated with increasing vaccine hesitancy with respect to other reasons given by parents for delaying/refusing. For example, compared with parents who only delayed and parents who only refused, parents who delayed and refused vaccines were significantly more likely to say that the reason for delaying and refusing was because “there were too many shots” (Table 5). Also, compared with parents who only delayed, parents who only refused and parents who refused and delayed were significantly more likely to report that the reasons for their decision were due to concerns about autism, vaccine effectiveness, and vaccine side effects, or because they heard or read negative things about vaccines in the media (Table 5).
DISCUSSION
Our analysis suggests that there is a gradient within the psychosocial domains of the Health Belief Model that signifies that increased parental hesitancy is associated with parents' decision to delay or refuse vaccinations for their child, and that this decision is associated with lower vaccination coverage. With respect to the psychosocial domains of the Health Belief Model, compared with parents who neither delay nor refuse vaccines for their child, parents who delay and refuse vaccines are less likely to believe that their child is at risk of getting a VPD; are less likely to believe that VPDs are an important health concern that make vaccinations desirable; are less likely to believe that vaccinating can reduce the threat of a VPD; and are more likely to have concerns about vaccine efficacy and safety that discourage them from vaccinating their child. Moreover, the data show that the gradient that describes increasing vaccine hesitancy among parents is associated with greater distrust as measured by parents' belief that a medical professional may not have their children's best interest at heart. Further, our results showed that after adjusting for child, maternal, and household factors, the psychosocial domains indexing the Health Belief Model were predictive of vaccination coverage.
These findings are concordant with other recent work that has evaluated the impact of parental concerns about vaccine safety.35–39 Also, our data showed that the gradient in parental hesitancy across the Health Belief Model scale is associated with higher-level socioeconomic status and is concordant with other research that demonstrated that children whose parents refused all vaccines were significantly more likely to have a mother who was a college graduate and to live in a suburban household with a higher annual family income.40
Limitations
Statistics obtained from the NIS are weighted to be representative of all children aged 19–35 months in the U.S. Statistical adjustments are made to the survey weights to account for households without landline telephones and other effects that could bias estimates from the NIS.30 Because the NIS is a survey of children living in households with landline telephones only, our analyses did not have data from children who live in households with no telephone service or children who live in households with cellular phone service only. Therefore, the estimates presented in this article could be biased insofar as households not covered by the NIS are different from those that are covered by the NIS, with respect to the outcomes that we have reported. However, recent work suggests that bias in surveys that only sample households with landline telephones may be small.41,42
Further, it is important to note that other theories of behavior provide a conceptual framework that may offer alternative explanations as to why parents delay recommended vaccine doses or fail to seek all doses of all recommended vaccines for their children.43–45 However, we have reported on the Health Belief Model because of its historic importance in vaccination coverage research and because of remarkable parallels in parents' sentiments during the 1950s, when the model was developed, and today.
While parents' responses to some of the vaccine and health belief statements could be assigned to different domains of the Health Belief Model, they also fit well within the domains to which we have assigned them. Since Rosenstock' initial specification of the Health Belief Model,12 there have been many subsequent refinements and improvements to the model that are not reflected in our work. For example, data from the NIS do not provide information that would allow a comprehensive analysis of parents' decision-making processes in which they weigh the costs and risks of vaccinating their child vs. the potential benefits of vaccinating. Also, the statements read to parents do not address all of the aspects of each of the four domains of the Health Belief Model. However, we note that behavioral models are useful only if they are used. We used the original Health Belief Model to organize our analysis because of its simplicity and because it was originally designed and used to understand why people do not become vaccinated.11 One of the main strengths of the four domains of the Health Belief Model is that it is readily understood by clinicians and may facilitate a constructive dialogue with vaccine-hesitant parents. While a fuller understanding of parents' decision-making processes would be useful, obtaining comprehensive measures relating to the multiple cues to action for each sampled parent is beyond the scope of the NIS.
CONCLUSIONS
Parents who refuse or delay vaccines not only leave their children susceptible to VPDs, but also make their communities vulnerable to outbreaks of VPDs. Why do parents refuse or delay vaccines for their children? Results from our study suggest that some of the reasons that parents delay or refuse depend on the extent of their concerns about vaccines and some of the reasons are unrelated to vaccine hesitancy. For example, regardless of their delay/refusal category, we found that a main reason for parents' decision to delay or refuse a vaccine was because their child was ill at the time of their appointment. The goal of vaccinating children who missed doses because of illness could be realized by utilizing clinic-based assessment46 of vaccination status so that providers can identify undervaccinated children and through providers' use of reminder/recall systems47 to recall children to clinics to receive missed doses. On the other hand, our data show that compared with parents who only delay, parents who refuse vaccine doses are significantly more likely to report too many shots as the reason for their refusal; they had concerns about autism, vaccine effectiveness, or vaccine side effects; or they had heard or read unfavorable reports about vaccines in the media. In the 2008 outbreak of measles in San Diego, California, half of the cases occurred among children whose parents reported declining vaccinations for philosophical or religious reasons.48
Who can persuade parents that timely immunization is in their children' best interests if they have concerns about vaccines? Our data show that across the four delay/refusal categories, at least 40% of all parents did not report that their decision to vaccinate was influenced by a doctor or nurse. In fact, our results show that with respect to the continuum in the Health Belief Model, increasing vaccine hesitancy is also associated with an increasing percentage of parents who seek advice and information from a practitioner of complementary alternative medicine who may not fully accept childhood vaccines.49
Of greater importance is our finding that children are at risk of having lower vaccination coverage if their parents have a poor working relationship with their child's vaccination provider or mistrust the medical profession in general. Who will sway the decisions of these vaccine-hesitant parents? During polio vaccination campaigns of the late 1950s and early 1960s that followed the establishment of the safety and efficacy of the Salk vaccine, Rosenstock and colleagues noted that some parents' decisions to seek vaccination may be determined by social pressures applied by a person who is important to them.11 Current work uses social marketing methods50 to target vaccine-hesitant parents who may be considering only delaying vaccines, and transmits positive messages to assure parents that vaccines are safe and that vaccinating their children is a wise and normal precaution to take to protect their children's health.
Rosenstock et al. also suggested that parents who are more vaccine-hesitant are likely to be influenced only through personal, face-to-face contact, especially with their physician.11 While times have changed somewhat since the 1950s, recent literature still suggests that a trusting relationship between parents and health-care providers is key to vaccine-hesitant parents accepting recommended immunizations.51,52 Our work suggests that a strong provider-parent relationship and trust of medical professionals are significant predictors of vaccination coverage. Other recent literature suggests that children whose parents have safety concerns about vaccines can have vaccination coverage that is as high as children whose parents do not have safety concerns, provided their decision to vaccinate was influenced by a traditional health-care provider, such as a doctor or nurse.38
The American Academy of Pediatrics has published guidelines for physicians on how to engage parents and get them to talk about their concerns about vaccines.53 By using the authority that parents customarily confer upon traditional health-care providers in a respectful, noncoercive, and non-condescending manner, and by using logic-supported scientific knowledge about vaccines, traditional health-care providers who listen to the concerns of parents with an empathetic ear54 will be in the best position to lead vaccine-hesitant parents to make their own informed decision that vaccinating their children is the best way to protect their children from VPDs.
REFERENCES
- 1.Communicable Disease Center Public Health Service (US). Surveillance of poliomyelitis in the United States, 1958–1961. Public Health Rep. 1962;77:1011–20. [PMC free article] [PubMed] [Google Scholar]
- 2.Paul M. Safety of the poliomyelitis vaccine. Science. 1957;125:1067–71. doi: 10.1126/science.125.3257.1067. [DOI] [PubMed] [Google Scholar]
- 3.O'Neill WL. American high: the years of confidence, 1945–1960. New York: The Free Press; 1986. [Google Scholar]
- 4.Francis T, Jr, Korns RF. Evaluation of 1954 field trial of poliomyelitis vaccine: synopsis of summary report. Am J Med Sci. 1955;229:603–12. doi: 10.1097/00000441-195506000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Langmuir AD, Nathanson N, Hall WJ. Surveillance of poliomyelitis in the United States in 1955. Am J Public Health Nations Health. 1956;46:75–88. doi: 10.2105/ajph.46.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belcher JC. Acceptance of the Salk polio vaccine. Rural Sociol. 1958;23:158–70. [Google Scholar]
- 7.Clausen JA, Seidenfeld MA, Deasy LC. Parent attitudes toward participation of their children in polio vaccine trials. Am J Public Health Nations Health. 1954;44:1526–36. doi: 10.2105/ajph.44.12.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deasy LC. Socio-economic status and participation in the poliomyelitis vaccine trial. Am Sociol Rev. 1956;21:185–91. [Google Scholar]
- 9.Glasser MA. A study of the public's acceptance of the Salk vaccine program. Am J Public Health Nations Health. 1958;48:141–6. doi: 10.2105/ajph.48.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merrill MH, Hollister AC, Gibbens SF, Haynes AW. Attitudes of Californians toward poliomyelitis vaccination. Am J Public Health Nations Health. 1958;48:146–52. doi: 10.2105/ajph.48.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenstock IM, Derryberry M, Carriger BK. Why people fail to seek poliomyelitis vaccination. Public Health Rep. 1959;74:98–103. [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44(Suppl):94–127. [PubMed] [Google Scholar]
- 13.Becker MH. The Health Belief Model and personal health behavior. Health Educ Monogr. 1974;2:324–473. [Google Scholar]
- 14.Maiman LA, Becker MH, Kirscht JP, Haefner DP, Drachman RH. Scales for measuring Health Belief Model dimensions: a test of predictive value, internal consistency, and relationships among beliefs. Health Educ Monogr. 1977;5:215–30. doi: 10.1177/109019817700500303. [DOI] [PubMed] [Google Scholar]
- 15.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 16.Mullen PD, Hersey JC, Iverson DC. Health behavior models compared. Soc Sci Med. 1987;24:973–81. doi: 10.1016/0277-9536(87)90291-7. [DOI] [PubMed] [Google Scholar]
- 17.Harrison JA, Mullen PD, Green LW. A meta-analysis of studies of the Health Belief Model with adults. Health Educ Res. 1992;7:107–16. doi: 10.1093/her/7.1.107. [DOI] [PubMed] [Google Scholar]
- 18.Glanz K, Lewis FM, Rimer BK. Linking theory, research, and practice. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: theory, research, and practice. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- 19.Strecher VJ, Rosenstock IM. The Health Belief Model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: theory, research, and practice. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- 20.Roush SW, Murphy TV Vaccine-Preventable Disease Table Working Group. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298:2155–63. doi: 10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy RF. Deadly immunity. Rolling Stone 2005 Jun 30–Jul 14. [cited 2011 Mar 28]. Also available from: URL: http://www.webcitation.org/5glaWmdym.
- 22.McCarthy J. Mother warriors: a nation of parents healing autism against all odds. New York: Dutton Adult; 2008. [Google Scholar]
- 23.Carrey J. The judgment for vaccines is in??? The Huffington Post. 2009 Apr 22. [cited 2009 Nov 9]. Available from: URL: http://www.huffingtonpost.com/jim-carrey/the-judgment-on-vaccines_b_189777.html.
- 24.National Vaccine Information Center. Your health. Your family. Your choice. [cited 2009 Nov 9]. Available from: URL: http://www.nvic.org.
- 25.Generation Rescue. Jenny McCarthy's autism organization. [cited 2009 Nov 9]. Available from: URL: http://www.generationrescue.org.
- 26.Sears R. The vaccine book: making the right decision for your child (Sears Parenting Library) New York: Little, Brown and Company; 2007. [Google Scholar]
- 27.Sears R. AskDrSears.com: the vaccine book: making the right decisions for your child. [cited 2009 Nov 9]. Available from: URL: http://www.askdrsears.com/thevaccinebook/index.asp.
- 28.Feikin DR, Lezotte DC, Hamman RF, Soloman DA, Chen RT, Hoffman RE. Individual and community risks of measles and pertussis associated with personal exemptions to immunization. JAMA. 2000;284:3145–50. doi: 10.1001/jama.284.24.3145. [DOI] [PubMed] [Google Scholar]
- 29.Salmon DA, Haber M, Gangarosa EJ, Phillips L, Smith NJ, Chen RT. Health consequences of religious and philosophical exemptions from immunization laws [published erratum appears in JAMA 2000;283:2241] JAMA. 1999;282:47–53. doi: 10.1001/jama.282.1.47. [DOI] [PubMed] [Google Scholar]
- 30.Smith PJ, Hoaglin DC, Battaglia MP, Khare M, Barker LE. Statistical methodology of the National Immunization Survey, 1994–2002. Vital Health Stat. 2005;2:(138). [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention, National Center for Health Statistics (US). National Immunization Survey: datasets and related documentation: 2009 NIS household questionnaire. [cited 2011 Mar 24]. Available from: URL: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NIS/NISPUF09_HHQUEX.pdf.
- 32.Lumley T. Analysis of complex survey samples. J Stat Software 2004;9:1-19. Also available from: URL: http://www.jstatsoft.org/v09/i08 cited 2009 Nov 9.
- 33.Venables WN, Smith DM. R Development Core Team. An introduction to R: notes on R: a programming environment for data analysis and graphics. Version 2.8.0. [cited 2009 Nov 9]. Available from: URL: http://www.r-project.org.
- 34.Census Bureau (US). Poverty thresholds 2009. [cited 2010 Sep 2]. Available from: URL: http://www.census.gov/hhes/www/poverty/data/threshld/thresh09.html.
- 35.Freed GL, Clark SJ, Hibbs BF, Santoli JM. Parental vaccine safety concerns. The experiences of pediatricians and family physicians. Am J Prev Med. 2004;26:11–4. doi: 10.1016/j.amepre.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Bardenheier B, Yusuf H, Schwartz B, Gust D, Barker L, Rodewald L. Are parental vaccine safety concerns associated with receipt of measles-mumps-rubella, diphtheria and tetanus toxoids with acellular pertussis, or hepatitis b vaccines by children? Arch Pediatr Adolesc Med. 2004;158:569–75. doi: 10.1001/archpedi.158.6.569. [DOI] [PubMed] [Google Scholar]
- 37.Gust DA, Strine TW, Maurice E, Smith PJ, Yusuf H, Wilkinson M, et al. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114:e16–22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- 38.Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. -Association between health care providers' influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118:e1287–92. doi: 10.1542/peds.2006-0923. [DOI] [PubMed] [Google Scholar]
- 39.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125:654–9. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 40.Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics. 2004;114:187–95. doi: 10.1542/peds.114.1.187. [DOI] [PubMed] [Google Scholar]
- 41.Blumberg SJ, Luke JV. Coverage bias in traditional telephone surveys of low-income and young adults. Public Opin Q. 2007;71:734–49. [Google Scholar]
- 42.Blumberg SJ, Luke JV. Reevaluating the need for concern regarding noncoverage bias in landline surveys. Am J Public Health. 2009;99:1806–10. doi: 10.2105/AJPH.2008.152835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion (US). Physical activity and health: a report of the Surgeon General. Rockville (MD): Department of Health and Human Services (US); 1996. [Google Scholar]
- 44.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Department of Health and Human Services, National Institutes of Health, National Cancer Institute (US). Theory at a glance: a guide for health promotion practice. 2nd ed. 2005. [cited 2011 Jan 27]. Available from: URL: http://www.cancer.gov/PDF/481f5d53-63df-41bc-bfaf-5aa48ee1da4d/TAAG3.pdf.
- 46.Centers for Disease Control and Prevention (US). Vaccines & immunizations: programs and tools: Comprehensive Clinic Assessment Software Application (CoCASA) [cited 2008 Nov 29]. Available from: URL: http://www.cdc.gov/vaccines/programs/cocasa/default.htm.
- 47.Briss PA, Rodewald LE, Hinman AR, Shefer AM, Strikas RA, Bernier RR, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18(1 Suppl):97–140. doi: 10.1016/s0749-3797(99)00118-x. [DOI] [PubMed] [Google Scholar]
- 48.Outbreak of measles— San Diego, California, January–February 2008. MMWR Morb Mortal Wkly Rep. 2008;57(8):203–6. [PubMed] [Google Scholar]
- 49.Zuzak TJ, Zuzak-Siegrist I, Rist L, Staubli G, Simoes-Wüust AP. Attitudes towards vaccination: users of complementary and alternative medicine versus non-users. Swiss Med Wkly. 2008;138:713–8. doi: 10.4414/smw.2009.12681. [DOI] [PubMed] [Google Scholar]
- 50.Opel DJ, Diekema DS, Lee NR, Marcuse EK. Social marketing as a strategy to increase immunization rates. Arch Pediatr Adolesc Med. 2009;163:432–7. doi: 10.1001/archpediatrics.2009.42. [DOI] [PubMed] [Google Scholar]
- 51.Keane MT, Walter MV, Patel BI, Moorthy S, Stevens RB, Bradley KM, et al. Confidence in vaccination: a parent model. Vaccine. 2005;23:2486–93. doi: 10.1016/j.vaccine.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 52.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 53.Diekema DS, American Academy of Pediatrics Committee on Bioethics. Responding to parental refusals on immunization of children. Pediatrics. 2005;115:1428–31. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]
- 54.Aristotle . 2nd ed. New York: Oxford University Press; 2007. On rhetoric: a theory of civic discourse [Kennedy GA, translator] [Google Scholar]