Abstract
BACKGROUND
Despite many advances in assisted reproductive techniques (ART), little is known about preferences for technological developments of women undergoing fertility treatments. The aims of this study were to investigate the preferences of infertile women undergoing ART for controlled ovarian stimulation (COS) treatments; to determine the utility values ascribed to different attributes of COS treatments; and to estimate women's willingness to pay (WTP) for COS.
METHODS
A representative sample of ambulatory patients ready to receive, or receiving, COS therapies for infertility were recruited from seven specialized private centres in six autonomous communities in Spain. Descriptive, inferential and conjoint analyses (CA) were used to elicit preferences and WTP. Attributes and levels of COS treatments were identified by literature review and two focus groups with experts and patients. WTP valuations were derived by a combination of double-bounded (closed-ended) and open questions and contingent ranking methods.
RESULTS
In total, 160 patients [mean (standard deviation; SD) age: 35.8 (4.2) years] were interviewed. Over half of the participants (55.0%) had a high level of education (university degree), most (78.8%) were married and half (50.0%) had an estimated net income of >€1502 per month and had paid a mean (SD) €1194.17 (€778.29) for their most recent hormonal treatment. The most frequent causes of infertility were related to sperm abnormalities (50.3%). In 30.6% of cases, there were two causes of infertility. The maximum WTP for COS treatment was €800 (median) per cycle; 35.5% were willing to pay an additional €101–€300 for a 1–2% effectiveness gain in the treatment. Utility values (CA) showed that effectiveness was the most valued attribute (39.82), followed by costs (18.74), safety (17.75) and information sharing with physicians (14.93).
CONCLUSIONS
WTP for COS therapies exceeds current cost. Additional WTP exists for 1–2% effectiveness improvement. Effectiveness and costs were the most important determinants of preferences, followed by safety and information sharing with physicians.
Keywords: hormone fertility treatments, preferences, willingness to pay, conjoint analysis, infertility
Introduction
Willingness to pay (WTP) methods have generally been used to place a monetary value on health benefits in the context of a specific intervention, to elicit patients’ values and preferences for different interventions and to enable a comprehensive assessment of the perceived benefits (Herath et al., 2007). Technological innovations have greatly improved the therapeutic options of infertile women who seek medical assistance to achieve pregnancy (Ryan et al., 2004). Among such developments, the emergence of recombinant forms of human follicle-stimulating hormone (r-hFSH) suitable for subcutaneous injection has made treatments simpler and more comfortable than the traditional syringe and needle (Harlin et al., 2000). Self-injection with a pen device has been shown to be safe and easy, more convenient and less painful for the patient, to require lower FSH doses, to be less time-consuming and to shorten treatment duration (Platteau et al., 2003). Several attributes of therapy, such as successful pregnancy rate, ease of device use and convenience of treatment administration have been acknowledged as key determinants of patients’ decisions about treatment (Porter et al., 2008). Aspects related to the patient–doctor relationship, such as information handling and shared decision-making, may also influence patients’ choice of fertility treatment (Malin et al., 2001). Little is known, however, about the importance that women undergoing fertility treatment assign to the individual characteristics of their treatment.
Coverage of interventions and services in fertility has been internationally characterized by low public funding, while the appropriate level and source of funds for assisted reproductive technology (ART) procedures have been controversial in most developed societies (Olsen and Smith, 2001). Funding for infertility care has been distinguished by its reliance on higher user copayment compared with other health services (Marra et al., 2005). In Spain, although the National Health System covers ART in women <40 years of age, long waiting lists in the public sector make many infertile women seek private care (Matorras et al., 2007). Only Catalonia covers medication costs during three cycles when reproductive therapies are undertaken privately (Bosser, 2009).
This study aimed to: (1) investigate the preferences of infertile women undergoing ART for controlled ovarian stimulation (COS) treatments; (2) determine the utility values ascribed to different attributes of COS treatments; and (3) estimate women's WTP for COS.
Materials and Methods
Study design and methods
An observational, longitudinal, prospective, multicentre study was designed to determine women's preferences for hormone fertility treatments in the private health sector in Spain. Two complementary techniques were applied to elicit preferences: WTP and conjoint analysis (CA). WTP is the maximum amount of money a person would be willing to pay, sacrifice or exchange for goods, in this case, for a benefit in their health state (Hanley et al., 2003). The philosophy behind this technique is that the maximum amount of money a person is willing to pay for a healthcare gain is an indicator of the value of that gain to that person. CA serves to determine how individuals value different features that constitute a particular health product or service (Ryan and Farrar, 2000). It seeks to establish what combination of a limited number of attributes is most influential on respondents’ choice or decision-making. The implicit value (utility) of the individual elements making up the treatment modality can be determined by analysing how participants define their preferences for the characteristics of the product.
WTP was assessed in two complementary ways: (1) a structured interview was conducted to directly ask patients about their WTP for a defined COS treatment; (2) the cost of treatment was included as an attribute in the CA. It was possible to directly assess the importance and the utility value assigned to the costs of treatments in relation to the other characteristics of treatments.
Experts in fertility were invited to form a study advisory board to give informed support to the project.
The definition of the content of the WTP interview and the selection of the attributes of treatments and their levels were conducted in three stages: first, a literature review identified a preliminary set of attributes and their levels; second, a focus expert group selected the treatment characteristics that are most meaningful in clinical practice and estimated the average price that their patients normally paid for their COS treatments; third, structured telephone interviews with infertility patients further defined treatment characteristics from their perspective.
The list of attributes initially identified in the literature and presented to the experts, as well as the arguments given by them to either refuse or include each characteristic of treatment in the CA are provided in the Supplementary information. A general consensus was sought on the most definitive attributes that influence treatment decisions.
Patients’ perspectives were obtained during the telephone interview; eight participants were asked to identify the characteristics of COS treatment that drive their preferences, as well as to estimate the average price that they have usually paid for their hormonal fertility treatments. Their experiences from receiving COS treatment, as well as being members of the Spanish National Association for Infertility Problems (ASPROIN), provided valuable additional information to the advisory board. The interviews were conducted by an experienced researcher (S.P.), lasted no longer than 15 min, and were recorded on audiotape for subsequent content analysis. Finally, a set of attributes and their levels were defined, based on the ones recognized by both experts and patients as the most relevant to determine treatment choices. As a result, COS was described in terms of five attributes, which were broken down into different levels (Table I). All levels of treatment attributes were combined, and an orthogonal fractional design was used to form a set of eight scenarios. A similar criterion of general agreement between experts and patients was applied to define the average price for a cycle of hormonal fertility treatment to be applied in the WTP interview.
Table I.
Description of attributes with their levels.
| Attribute | Levels | Description |
|---|---|---|
| Safety | Safer | Smaller risk, although of no consequence, of causing infections or allergies |
| Less safe | Higher risk, although of no consequence, of causing infections or allergies | |
| Effectiveness | More effective | 1–2% higher rate of a successful pregnancy |
| Less effective | Lower rate of a successful pregnancy | |
| Administration of treatment | More friendly administration of treatment | Treatment administration does not interfere with social and work activities |
| Less friendly administration of treatment | Treatment administration interferes with social and work activities | |
| Price | <€1000 | Per cycle of ovarian stimulation |
| €1000–€1500 | ||
| €1500–€2000 | ||
| >€2000 | ||
| Patient–doctor information sharing | Your physician informs you about possible alternative treatments and involves you in decisions about treatments to follow | |
| Your physician does not inform you about possible alternative treatments and does not involve you in decisions about treatments to follow | ||
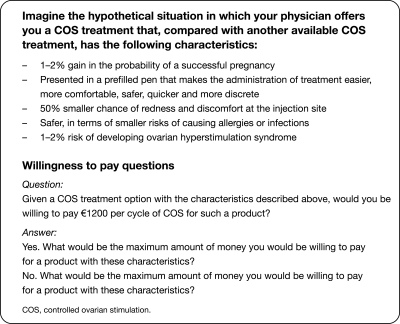
Willingness to pay and conjoint analysis interview
As part of the study field work, a structured, two-part (WTP and CA) patient interview was designed based on the findings gathered from the literature, the focus expert group and the telephone interviews. The interview was conducted by a trained researcher (S.P.), not known to the participants, and took place either before or after the patients’ routine medical appointment for a maximum of 40 min. First, the patients were presented with a description of the product being evaluated and were asked about their WTP for a previously defined amount that reflected the current price of treatments in the market, which was agreed by experts and patients. Their maximum WTP was established from a combination of double-bounded (closed-ended) and open questions (Fig. 1). In those situations where participants had difficulty expressing a maximum WTP, the technique of first refusal price was employed in a way such that all women finally reported a maximum amount. Additionally, they were asked about the number of times throughout the year they would be prepared to pay the maximum amount stated and the percentage of treatment costs they considered that public healthcare services should cover. Three final questions explored the extra quantity of money participants were willing to pay for individual characteristics of treatments, such as injection comfort, tolerance and effectiveness. The interview also included socio-demographic questions, open questions on the current price that patients pay for hormonal treatments per cycle of COS and a visual analogue scale (VAS) to estimate the proportional value assigned to the hormonal therapies in relation to the total amount paid for ART.
Figure 1.
Type of questions used to elicit WTP.
Second, respondents were shown a set of eight scenarios, written on a paper card, and asked to order them from ‘the most’ to ‘the least’ preferred. Each scenario was made up of a unique combination of treatment features. Each scenario was similar enough that participants saw them as close substitutes, but sufficiently dissimilar that they could clearly determine a preference.
Sample size
To the authors’ best knowledge, there are no references in the literature on assessments of the preferences of infertile women undergoing COS. Sample size was estimated accepting a maximum uncertainty of 50%, and assuming an accuracy of 8% with a 95% confidence interval (CI). Under these assumptions, a sample size of 150 patients was required. Assuming possible losses of 10%, the sample size was fixed on 165 patients.
Study setting and participants
All participants were women, and were outpatients at private fertility clinics in different autonomous communities in Spain. They were identified at each study site by the healthcare team and were consecutively recruited into the study (non-random, convenient sampling) if they were aged 18 years or older, had been, or were about to be, on hormone fertility treatment and gave written, informed consent to participate in the project. Possible candidates were excluded if they were participating in a clinical trial at the time of the study, were oocyte donors or were unable to properly respond to the interviews’ tasks for any reason, including the need for the cultural adaptation of the research tools. Treatments were prescribed according to usual clinical practice.
Data analysis
A statistical descriptive analysis was performed to investigate the social, demographic and clinical characteristics of the women that took part in the study. WTP was estimated from the answers given about their WTP the current price of treatments, about the maximum amount of money that they said they would be willing to pay for the product and about the extra quantity of money they were willing to pay for individual characteristics of treatments, such as effectiveness, injection comfort and local tolerance. Descriptive analyses were performed. Relations between these and the rest of the social and clinical variables were explored using hypothesis tests and multiple linear regression analysis.
An orthogonal fractional factorial design (SPSS Conjoint 16.0) was used to define the scenarios for the CA. The resulting orthogonal matrix captured the principal effects of each level of attributes. It was assumed that interactions between levels of the same attribute were meaningless. The ordering method was applied to determine the preferences of participants, and a mean position value was estimated for each scenario. Analysis of the scenario order gave a utility score and represented the partial contribution of each level of the attributes in the determination of preferences. Linear regression analysis was employed to estimate the utility values assigned to each level of attributes. The mathematical expression for the model is as follows:
where Y is the respondent's preference, b0 is the constant or the intercept term, b1 to b5 are part-worth utilities (or simply utility values) and e is an error term. All the dichotomous (two levels) attributes were codified as +1 for their ‘best level’ (safer, 1–2% more effective, more comfortable, decision shared with physician) and as −1 for their ‘worst level’ (less safe, less effective, less comfortable administration, decision not shared with physician). Attribute ‘cost’ was codified with the labels 1:4.
Higher utility values implied a greater preference for that level of attribute. Additionally, the coefficients of importance of all attributes were estimated. The total importance of a set of conjoint attributes is always calculated to sum up to 100%. The importance of an individual conjoint attribute is determined by the span of the utility levels for each attribute compared with the utility spans for the other attributes. As a result, it was possible to establish whether the attribute had an influence on the preference for a given COS treatment, as well as the relative importance assigned to the different attributes for making treatment choices. It was established that preferred scenarios had higher utility values derived from their attributes compared with less preferred scenarios.
Results
Seven private clinics in six autonomous communities in Spain took part in the study. A total of 171 patients were initially recruited into the study. However, four participants declined to take part due to emotional distress and seven were excluded due to their donor condition. Therefore, study results are based on a sample of 160 participants (Andalusia, n = 22; Asturias, n = 31; Balearic Islands, n = 17; Canary Islands, n = 27; Madrid, n = 19; Valencia, n = 44).
Social and demographic characteristics
Table II summarizes the social and demographic characteristics of the studied sample. The mean [standard deviation (SD)] age of participants was 35.8 (4.2) years (range: 22–46 years). The majority of participants were married (78.8%) and employed (68.8%), with more than half (55.0%) having a high level of education (university degree). Half of the participants (50.0%) had an estimated net income of >€1502 per month; of these, 18.4% had a net income ranging between €1804 and €2404 per month.
Table II.
Social and demographic characteristics of the studied population.
| Number of patients (n = 160) | Percentage of patients (%) | Accumulated percentage (%) | |
|---|---|---|---|
| Education | |||
| No school attendance | 1 | 0.6 | 0.6 |
| Primary school | 22 | 13.8 | 14.4 |
| Secondary school | 26 | 16.3 | 30.6 |
| College/technical school | 23 | 14.4 | 45.0 |
| University | 88 | 55.0 | 100.0 |
| Marital status | |||
| Single | 11 | 6.9 | 6.9 |
| Married | 126 | 78.8 | 85.6 |
| Partnered | 22 | 13.8 | 99.4 |
| Divorced | 1 | 0.6 | 100.0 |
| Job situation | |||
| Employed | 110 | 68.8 | 68.8 |
| Self-employed | 21 | 13.1 | 81.9 |
| Permanent sick leave | 1 | 0.6 | 82.5 |
| Temporary sick leave | 1 | 0.6 | 83.1 |
| Unemployed | 13 | 8.1 | 91.3 |
| Homemaker | 11 | 6.9 | 98.1 |
| Student | 3 | 1.9 | 100.0 |
Clinical characteristics
The most frequent causes of infertility were related to sperm abnormalities (50.3%), followed by ovulatory dysfunction (19.6%). In about one-third of participants (30.6%), there were two causes of infertility, while in 25.6%, the cause of infertility could be attributed to the couple. Mean (SD) length of follow-up in the same clinic was 8.2 (11.4) months (range: 0–72 months), while the mean (SD) length of time patients were on COS treatment was 8.0 (11.5) months (range: 0.3–65.6 months). At the time of the study, 56.6% (81/143) of patients were receiving hormonal treatment. The most commonly prescribed treatment was r-hFSH (72.7%), followed by the urinary human FSH/luteinizing hormone combination (29.6%). IVF was the technique most commonly indicated (85.3%) and the gonadotrophin-releasing hormone antagonist protocol for ovarian stimulation was the most frequently prescribed treatment scheme (53.1%).
Willingness to pay
The mean (SD) amount of money that had been paid by patients (n = 145) for their most recent hormonal treatment was €1194.11 (€778.29; range: €30–€5000). In a VAS representing percentages (0–100%), patients were asked to indicate what proportion of the total cost of ART they would be willing to devote exclusively to COS. In this way, it was possible to indirectly estimate the relative importance given to hormone therapies within the entire ART. VAS measurements showed that as many as 84.1% of participants would be willing to pay up to 60% of the total price of the current fertility treatment to COS alone. On average, women who underwent infertility treatment because of male factor infertility would be willing to pay up to 32.18% of the total price, while women who sought treatment due to female infertility would pay up to 42.18% of the total price. Finally, women with infertility problems attributed to both partners would pay up to 50.36% of the total ART cost to COS. A Tukey test detected statistically significant differences between the mean percentage of women in the group with male factor infertility and the group with infertility related to both partners (F = 7.45, P = 0.0008). The group with infertility related to both partners would assign a higher proportion of the total ART costs to COS than women with male-related infertility.
As many as 45.0% (72/160) of patients would pay €1200 per cycle of COS with a series of characteristics: including a guarantee of a 1–2% gain in the probability of a successful pregnancy; a prefilled pen that would make the administration of treatment easier, more comfortable, more reliable, quicker and more discrete; a 50% decrease in the chances of redness and discomfort in the injection site; safer, in terms of smaller risks of causing allergies or infections; and a 1–2% probability of developing ovarian hyperstimulation syndrome. Most of the patients (62.4%) who were willing to pay €1200 per COS cycle had a higher level of education (university degree) and the majority (86.3%) were undergoing COS at the time of the interview.
The median maximum amount of money participants were willing to pay for their COS therapy was €800 per cycle (mean: €1442.29; SD: €4093.57; range: €0–€50 000); the majority of participants (76.4%) would pay this up to four times in a year (mean: 5.53; SD: 10.86; range: 1–77). All participants stated that public healthcare services should cover part of the hormonal treatment costs; a majority (66.9%) believed that this funding should cover up to 80% of the overall costs of COS (mean: 73.37%; SD: 21.29%; median: 75.00%; range: 30–100%).
The maximum amount of money that participants would be willing to pay was independent of their age (P = 0.36), marital status (P = 0.27), employment situation (P = 0.97) or net monthly household income (P = 0.85). It was also independent of the length of time patients were receiving fertility treatment (P = 0.62), their condition of already being on treatment at study entry (P = 0.26) and the treatment scheme they were on (P = 0.89). Multiple regression analysis showed that changes in the maximum amount of money that participants would be willing to pay for hormone fertility treatments could not be explained by participants’ age, marital status, employment situation, education level or net monthly income (P = 0.25). Its variation could neither be explained by the causes of infertility, whether the origin of infertility related to the male, the female or the couple, the length of time patients had spent on fertility treatment or the ART being indicated (P = 0.22).
In relation to the three characteristics of treatments assessed individually, 35.5% of participants would pay an additional €101–€300 for a 1–2% increase in the successful pregnancy rate. Other features of treatment such as comfort in the administration and local tolerance of injections were given little value: more than half of participants (62.5%, comfort; 66.3%, tolerance) would pay no extra money for gains in these attributes (Table III).
Table III.
Willingness to pay for three individual advantages of controlled ovarian stimulation therapy.
| Maximum amount willing to pay, € (range) | Patients in each range, n (%) |
||
|---|---|---|---|
| Prefilled pen (comfort) | 50% smaller chance of redness on the injection site (tolerance) | 1–2% higher rate of a successful pregnancy (effectiveness) | |
| 0 | 100 (62.5) | 106 (66.3) | 23 (14.7) |
| 1–50 | 19 (11.9) | 29 (18.1) | 16 (20.3) |
| 51–100 | 24 (15.0) | 14 (8.8) | 37 (23.7) |
| 101–300 | 14 (8.8) | 8 (5.0) | 55 (35.5) |
| 301–500 | 2 (1.3) | 3 (1.9) | 16 (10.3) |
| 501–1000 | 1 (0.6) | 0 | 9 (5.8) |
| 1001–2000 | 0 | 0 | 3 (1.8) |
| >2000 | 0 | 0 | 1 (0.6) |
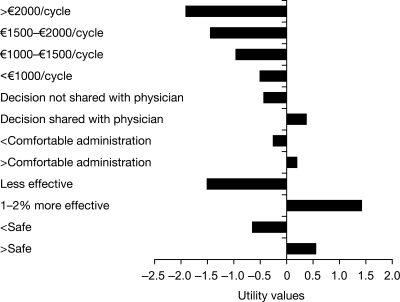
Conjoint analysis: utility and importance values
A total of five attributes of COS (safety, effectiveness, comfort of the administration, cost and physicians’ shared decisions with patients) and their levels were assessed. The highest utility value was assigned to effectiveness (1.49) understood as 1–2% higher probability of having a successful pregnancy, followed by safety (0.62) and shared decisions with physicians (0.41) (Fig. 2). Comfort in the administration of treatment was given a lower utility value (0.25) than the three previous attributes. All ranges of costs being analysed received negative values (<€1000 per cycle of COS: −0.47; €1000–€1500: −0.95; €1500–€2000: −1.42; >€2000: −1.90). Table IV shows the 95% CI for each estimated utility value.
Figure 2.
Utility values assigned to the levels of attributes of treatment.
Table IV.
Confidence intervals for utility values.
| Attributes of treatment | Levels of attributes | Utility value estimates | 95% confidence intervals |
|---|---|---|---|
| Safety | Less safe | −0.623 | [−0.7222, −0.5232] |
| Safer | 0.623 | [0.5232, 0.7222] | |
| Effectiveness | Less effective | −1.491 | [−1.5952, −1.3987] |
| 1–2% more effective | 1.491 | [1.3987, 1.5952] | |
| Administration of treatment | Less comfortable administration | −0.252 | [−0.3086, −0.1913] |
| More comfortable administration | 0.252 | [0.1913, 0.3086] | |
| Patient–doctor information sharing and decision-making | Information and decision not shared with patient | −0.414 | [−0.5150, −0.3023] |
| Information and decision shared with patient | 0.414 | [0.3023, 0.5150] | |
| Price | <€1000/cycle | −0.475 | [−0.5491, −0.4053] |
| €1000–€1500/cycle | −0.950 | [−1.0263, −0.8826] | |
| €1500–€2000/cycle | −1.425 | [−1.5036, −1.3598] | |
| >€2000/cycle | −1.901 | [−1.9808, −1.8371] |
The effectiveness of treatment was considered the most important attribute (39.82). Costs were scored in second place (18.74), followed by safety (17.75). Information sharing with physicians (14.93) was ranked in fourth place. Comfort of treatment administration (8.73) was considered the least important feature of COS treatment. All differences in values of importance were statistically significant except for safety versus costs (P = 0.21); no significant differences were found between the importance given to both of them. There was a strong correlation between the observed and the estimated preferences (R = 0.99; P < 0.0001).
Scenarios
Table V shows statistical information on the order of preference attributed to the eight suggested scenarios. Ranked from the most to the least favoured by participants, scenario 1 was the most preferred (preference position: median 1.00). It was chosen in first place by 95.6% of the participants (n = 153). The next most desirable scenario was number 8 (preference position: median 3.00); 43.1% of patients preferred it in second place (n = 69). The least favoured was scenario 3 (preference position: median 6.50), with 36.3% of participants placing it as the last option (n = 58). Scenarios 5, 7 and 8 were never placed in first place by participants. Table VI provides details of the above three scenarios.
Table V.
Ranking of participants’ preferences for the suggested scenarios (n = 160).
| Scenarios |
||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Mean | 1.26 | 6.35 | 6.15 | 5.86 | 4.79 | 4.65 | 4.00 | 2.99 |
| Median | 1.0 | 6.00 | 6.50 | 6.00 | 5.00 | 4.00 | 4.00 | 3.00 |
| Standard deviation | 1.28 | 1.21 | 1.87 | 1.76 | 1.83 | 1.78 | 1.72 | 1.33 |
| Minimum | 1.00 | 1.00 | 1.00 | 1.00 | 2.00 | 1.00 | 2.00 | 2.00 |
| Maximum | 8.00 | 8.00 | 8.00 | 8.00 | 8.00 | 8.00 | 8.00 | 8.00 |
Table VI.
Preferred scenarios.
| Most preferred scenarios |
Least preferred scenario | |
|---|---|---|
| Scenario 1 | Scenario 8 | Scenario 3 |
| Safer (minor risk, insignificant, of causing infections or allergies) | Less safe (higher risk, although insignificant, of causing infections or allergies) | Less safe (higher risk, although insignificant, of causing infections or allergies) |
| More effective (1–2% higher rate of a successful pregnancy) | More effective (1–2% higher rate of a successful pregnancy) | Less effective (lower rate of a successful pregnancy) |
| More friendly administration of treatment (treatment administration does not interfere with social and work activities) | More friendly administration of treatment (treatment administration does not interfere with social and work activities) | More friendly administration of treatment (treatment administration does not interfere with social and work activities) |
| Price: <€1000 per cycle of ovarian stimulation | Price: €1500–€2000 per cycle of ovarian stimulation | Price: >€2000 per cycle of ovarian stimulation |
| Your physician informs you about all possible alternative treatments and involves you in all decisions about the treatments to follow | Your physician does not inform you about possible alternative treatments and does not involve you in decisions about treatments to follow | Your physician informs you about all possible alternative treatments and involves you in all decisions about the treatments to follow |
Discussion
Women's preferences for COS in the context of ART were elicited using two complementary techniques: WTP and CA. The simultaneous use of both techniques allowed a direct estimate of the maximum amount of money participants were willing to pay for COS treatment that offered certain gains in effectiveness, safety and comfort, as well as an assessment of the relative importance and utility values assigned by patients to costs compared with the other therapy attributes. Assessment using both techniques showed that treatment costs were less important to patients if the chances of a successful pregnancy were to be increased.
Higher pregnancy rates were paramount in defining patients’ preferences for fertility treatments. The WTP interview showed that patients would be willing to pay an additional amount of money for a 1–2% improvement in effectiveness, while the CA demonstrated that patients would be ready to trade-off treatment costs for gains in effectiveness and safety. These findings are congruent with results from other studies. For instance, early reports found that a 10% chance of having a child through IVF in the event of infertility determined couples’ WTP a stated amount of money under various assumptions on the probability of success (Neumann and Johannesson, 1994). It has also been reported that patients with polycystic ovary syndrome would prefer electrocautery of the ovaries over ovulation induction with r-hFSH if both treatment strategies resulted in similar pregnancy rates (Bayram et al., 2005). However, most patients were willing to trade off their preference for increased effectiveness. The percentage of patients who preferred electrocautery over r-hFSH declined when the difference in theoretical pregnancy rates was >5% in favour of r-hFSH. It has also been found that infertile couples would give higheconomic priority to infertility treatment and that they would pay more for a child than the calculated direct cost (Devlin and Parkin, 2003), which reflects the high value attributed to conceiving a child.
In this study, the maximum amount of money that participants would pay for their hormone fertility therapies was independent of their age, education, marital status and net monthly income. These results differ from other findings in which WTP has been positively associated with education, income and beliefs, and the ideological acceptance of healthcare (Cookson, 2003). However, it could be argued that the women being interviewed had already made their decision to seek medical treatment for their fertility problem, were prepared to pay its costs and, therefore, their net monthly income had no particular influence on their readiness to fund COS. Accordingly, it has been reported that income has an impact on the decision to seek medical assistance, especially ART, which is expensive and least likely to be covered by insurance (Ordovensky Staniec and Webb, 2007). Net income appears to be significant in terms of decreasing the likelihood that poorer women will seek fertility treatment, but it does not seem to considerably increase the chances that relatively well-off women will do so (Hughes and Giacomini, 2001).
Shared information and decision-making on therapies with the specialist was also investigated as it has been reported to substantially influence patients’ preferences for treatments (Say and Thomson, 2003). In this study, participants gave more importance and a higher value to information sharing than to comfort in the administration of therapies, implying that women would exchange simplicity and minor discomfort in the application of treatments for a more reassuring communication with their treating physician. Furthermore, unsatisfactory encounters with healthcare professionals had been reported to be the main reasons for dissatisfaction amongst infertile women seeking medical care, and they had been frequently referred to as one of the most negative treatment experiences (Malin et al., 2001).
The value given to the use of a prefilled pen device to self-administer treatment was assessed in terms of impact on daily life. Patients felt there would be little interference with everyday social and work activities. This attribute was the weakest determinant of preferences compared with the other treatment characteristics explored. Participants would exchange the commodity that offers a prefilled pen device for gains in effectiveness, safety, costs and communication with their treating physicians. In studies that solely assessed different modalities of therapy administration, the pen device was chosen over other dosing methods due to its perceived benefits in terms of gains in efficiency (Bruynesteyn et al., 2005). Attributes that have usually favoured the use of a pen device include a faster preparation, higher confidence of accurate dosing and the need for fewer dose adjustments (Porter et al., 2008). According to our findings, these valuable attributes seem to lose relevance when other aspects of treatment are considered.
Results show that both experienced patients and those about to start their first COS cycle would prefer to be treated with the most effective hormones. This outcome seems reasonable for those patients who have devoted not only financial and time resources, but also emotional involvement because of lack of effectiveness of previous cycles: once they have allocated so many hopes and resources to ineffective treatments, they are ready to allocate additional financial resources even for marginal improvements (as low as 1–2%) in the pregnancy odds. Despite not having undergone these experiences previously, first time patients also gave priority to effectiveness. An economic interpretation of this result would be that improvements in pregnancy probabilities imply a lower risk of requiring additional investments of both time and money for subsequent treatment cycles.
This information about patients’ preferences becomes extremely valuable for healthcare professionals as this knowledge may allow them to improve not only the success rates of their therapies, but also other health-related quality of life outcomes related to patient satisfaction. All these outcomes constitute a comprehensive measure of quality of healthcare and, thus, are valuable sources of information for patients and professionals. In accordance with this, findings reported from previous studies have shown that respectful communication, appropriate information, support and confidence in healthcare professionals are highly valued in a clinical situation where outcomes are uncertain and emotional involvement is high (Redshaw et al., 2007).
In summary, this study reports the attributes that most strongly determine women's preferences for hormone fertility therapies in patients undergoing ART in the private sector in Spain. Respondents attributed the highest preference values to the effectiveness of the fertility treatment. Although important, other attributes of the intervention, such as gains in safety, comfort in their application and saving costs came behind the greater chance of success in conceiving a child. The information gathered may help clinicians and policy-makers to make more informed decisions in fertility interventions, taking into account patients’ views on the value of treatments. Despite the lack of a single, best approach to be applied, conjoint-based methods and WTP are among the quantitative techniques recommended to gain public opinion and preferences on healthcare interventions (Ryan et al., 2001).
Implications for future research
According to this study, WTP and CA appear to be useful tools in understanding how people value the benefits of reproductive treatments. A similar approach could be used to investigate, for instance, preference differences of the male partners of women undergoing fertility treatment or in patients from countries where IVF is differently reimbursed. Further research is needed to unravel how patients’ preferences are shaped and what factors influence the high importance given to the effectiveness of fertility therapies.
Authors’ roles
O.E., C.P., L.L. and S.P. designed the study. All authors contributed to the development of the protocol, to the collection and/or analysis of data for this study, have drafted and/or critically read and revised the manuscript for important intellectual content and have approved the final manuscript for publication.
Conflict of interest
A.P., P.D.L.F., M.R., F.S., J.M.-S., M.M., J.M., J.H., S.P. and L.L. worked on this study that was funded by Merck, S.L. (an affiliate of Merck KGaA, Darmstadt, Germany), but have no other conflicts of interest to disclose. O.E. was an employee of Merck, S.L. (an affiliate of Merck KGaA, Darmstadt, Germany) at the time of the study and during the production of the manuscript. C.P. is an employee of Merck, S.L. (an affiliate of Merck KGaA, Darmstadt, Germany).
Funding
This study was funded by Merck, S.L. (an affiliate of Merck KGaA, Darmstadt, Germany). Funding to pay the Open Access publication charges for this article was provided by Merck, S.L. (an affiliate of Merck KGaA, Darmstadt, Germany).
Supplementary Material
Acknowledgements
The authors are indebted to the patients who devoted their time to take part in the study and especially the ASPROIN for their support in the organization and development of the advisory board. Authors’ thanks also go to the professionals at the participating fertility clinics who gave their expert support and made a great effort to facilitate the development of the study. The authors thank Carol Cooper of Caudex Medical [supported by Merck, S.L. (an affiliate of Merck KGaA, Darmstadt, Germany)] for editorial assistance.
References
- Bayram N, van Wely M, van der Veen F, Bossuyt PM, Nieuwkerk P. Treatment preferences and trade-offs for ovulation induction in clomiphene citrate-resistant patients with polycystic ovary syndrome. Fertil Steril. 2005;84:420–425. doi: 10.1016/j.fertnstert.2005.02.026. doi:10.1016/j.fertnstert.2005.02.026. [DOI] [PubMed] [Google Scholar]
- Bosser R. Status of human assisted reproduction in Spain: results from the new registry of Catalonia. Reprod BioMed Online. 2009;19:727–733. doi: 10.1016/j.rbmo.2009.09.004. doi:10.1016/j.rbmo.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Bruynesteyn K, Bonsel GJ, Braat DD, Fauser BC, Devroey P, van Genugten ML. Economic evaluation of the administration of follitropin-beta with a pen device. Reprod BioMed Online. 2005;11:26–35. doi: 10.1016/s1472-6483(10)61295-3. doi:10.1016/S1472-6483(10)61295-3. [DOI] [PubMed] [Google Scholar]
- Cookson R. Willingness to pay methods in health care: a sceptical view. Health Econ. 2003;12:891–894. doi: 10.1002/hec.847. doi:10.1002/hec.847. [DOI] [PubMed] [Google Scholar]
- Devlin N, Parkin D. Funding fertility: Issues in the allocation and distribution of resources to assisted reproduction technologies. Hum Fertil. 2003;6:S2–S6. doi: 10.1080/1464770312331369153. doi:10.1080/1464770312331369153. [DOI] [PubMed] [Google Scholar]
- Hanley N, Ryan M, Wright R. Estimating the monetary value of health care: lessons from environmental economics. Health Econ. 2003;12:3–16. doi: 10.1002/hec.763. doi:10.1002/hec.763. [DOI] [PubMed] [Google Scholar]
- Harlin J, Czemiczky G, Wramsby H, Fried G. Recombinant follicle-stimulating hormone in in-vitro fertilization treatment–clinical experience with follitropin alpha and follitropin beta. Hum Reprod. 2000;15:239–244. doi: 10.1093/humrep/15.2.239. doi:10.1093/humrep/15.2.239. [DOI] [PubMed] [Google Scholar]
- Herath G, Yang JC, Pattanayak S, Choe KA. Asian Development Bank; 2007. Good practices for estimating reliable willingness-to-pay values in the water supply and sanitation sector. ERD Technical Note Series No. 23 www.adb.org/Documents/ERD/Technical_Notes/TN023.pdf. accessed 22 January, 2010, date last accessed. [Google Scholar]
- Hughes G, Giacomini M. Funding in vitro fertilization treatment for persistent subfertility: the pain and the politics. Fertil Steril. 2001;76:431–442. doi: 10.1016/s0015-0282(01)01928-8. doi:10.1016/S0015-0282(01)01928-8. [DOI] [PubMed] [Google Scholar]
- Malin M, Hemmink E, Räikkönen O, Sihvo S, Perälä ML. What do women want? Women's experiences of infertility treatment. Soc Sci Med. 2001;53:123–133. doi: 10.1016/s0277-9536(00)00317-8. doi:10.1016/S0277-9536(00)00317-8. [DOI] [PubMed] [Google Scholar]
- Marra CA, Frighetto L, Goodfellow AF, Wail AO, Chase ML, Nicol RE, Leong CA, Tomlinson S, Ferreira BM, Jewesson PJ. Willingness to pay to assess patient preferences for therapy in a Canadian setting. BMC Health Services Res. 2005;5:43. doi: 10.1186/1472-6963-5-43. doi:10.1186/1472-6963-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matorras R, Antonia Expósito A, Carreras M. Fertility policy in Spain. Pharma Policy Law. 2007;9:229–233. [Google Scholar]
- Neumann PJ, Johannesson M. The willingness to pay for in vitro fertilization: a pilot study using contingent valuation. Med Care. 1994;32:686–699. doi: 10.1097/00005650-199407000-00003. doi:10.1097/00005650-199407000-00003. [DOI] [PubMed] [Google Scholar]
- Olsen JA, Smith RD. Theory versus practice: a review of ‘willingness-to-pay’ in health and health care. Health Econ. 2001;10:39–52. doi: 10.1002/1099-1050(200101)10:1<39::aid-hec563>3.0.co;2-e. doi:10.1002/1099-1050(200101)10:1<39::AID-HEC563>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Ordovensky Staniec JF, Webb NJ. Utilization of infertility services: how much does money matter? Health Res Educ Trust. 2007;42:971–989. doi: 10.1111/j.1475-6773.2006.00640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platteau P, Laurent E, Albano C, Osmanagaoglu K, Vernaeve V, Tournaye H, Camus M, Van Steirteghem A, Devroey P. An open, randomized single-centre study to compare the efficacy and convenience of follitropin beta administered by a pen device with follitropin alpha administered by a conventional syringe in women undergoing ovarian stimulation for IVF/ICSI. Hum Reprod. 2003;18:1200–1204. doi: 10.1093/humrep/deg234. doi:10.1093/humrep/deg234. [DOI] [PubMed] [Google Scholar]
- Porter R, Kissel C, Saunders H, Keck C. Patient and nurse evaluation of recombinant human follicle-stimulating hormone administration methods: comparison of two follitropin injection pens. Curr Med Res Opin. 2008;24:727–735. doi: 10.1185/030079908X273291. doi:10.1185/030079908X273291. [DOI] [PubMed] [Google Scholar]
- Redshaw M, Hockley C, Davidson LL. A qualitative study of the experience of treatment for infertility among women who successfully became pregnant. Hum Reprod. 2007;22:295–304. doi: 10.1093/humrep/del344. doi:10.1093/humrep/del344. [DOI] [PubMed] [Google Scholar]
- Ryan GL, Zhang SH, Dokras A, Syrop CH, Van Voorhis BJ. The desire of infertile patients for multiple births. Fertil Steril. 2004;81:500–504. doi: 10.1016/j.fertnstert.2003.05.035. doi:10.1016/j.fertnstert.2003.05.035. [DOI] [PubMed] [Google Scholar]
- Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320:1530–1533. doi: 10.1136/bmj.320.7248.1530. doi:10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, Napper M, Robb CM. Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol Assess. 2001;5:1–186. doi: 10.3310/hta5050. [DOI] [PubMed] [Google Scholar]
- Say RE, Thomson R. The importance of patient preferences in treatment decisions—challenges for doctors. BMJ. 2003;327:542–545. doi: 10.1136/bmj.327.7414.542. doi:10.1136/bmj.327.7414.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.