Abstract
Background
Epicardial fat volume (EFV) measured from non-contrast CT is associated with coronary atherosclerosis and increased risk of major adverse cardiovascular event risk. Reproducibility of EFV quantification from non-contrast CT has not been reported.
Objective
We evaluated the interscan (intra-scanner and inter-scanner) reproducibility of EFV and thoracic fat volume (TFV) measurements from non-contrast CT.
Methods
We studied 25 consecutive patients who were scanned twice using 4-slice multi-detector CT (MDCT), with 120 kVp, 2.5 mm slice thickness (intra-scanner) and additionally, 23 consecutive patients who were scanned using MDCT and electron-beam CT with 3 mm slice thickness (inter-scanner). For each scan, EFV and TFV were measured from user-defined range of CT slices covering the heart by an experienced imaging cardiologist. Voxels within −30 to −190 Hounsfield Unit within the epicardial contours was quantified as EFV. TFV was quantified within the heart range automatically. Repeatability coefficient (RC), defined as 1.96 × SD of the differences between pairs of repeated measures, was determined.
Results
Correlations for interscan measurements of EFV and TFV were high for both intra-scanner (MDCT-MDCT) and inter-scanner (EBCT-MDCT) data (correlation coefficient ≥ 0.98). RC values were lowest (4.3% for EFV and 5.4% for TFV) for intra-scanner same-observer measurement. For intra-scanner cross-observer measurement, RC values were 10.7% for EFV and 9.0% for TFV. For inter-scanner data, RC values ranged from 6.8% to 8.2%.
Conclusion
Epicardial and thoracic fat measurements using either MDCT or EBCT are highly reproducible.
Keywords: epicardial fat, non-contrast CT, reproducibility, EBCT, MDCT, thoracic fat
Epicardial fat volume (EFV) and thoracic fat volume (TFV) can be routinely quantified from non-contrast computed tomography (CT) scans performed for coronary calcium scoring.1, 2 EFV measured from non-contrast CT is associated with a higher coronary calcium score, coronary artery disease severity, biochemical markers of systemic inflammation, and increased risk of future adverse cardiovascular events.1,3–13 Direct measurement of EFV can be challenging due to reliance on detection of the thin pericardium. As more and more data support the clinical use of EFV, it is important to establish the reproducibility of quantifying epicardial adipose tissue.
Historically, coronary artery calcium scanning has been performed on electron-beam CT (EBCT) scanners, and currently is performed using multi-detector CT (MDCT) scanners. Interscan reproducibility (intra-scanner [MDCT-MDCT] and inter-scanner [EBCT-MDCT]) of EFV quantification from non-contrast CT have not yet been determined. Our previous results showed inter-observer reproducibility of epicardial and thoracic fat from a single scan.1, 14 The novelty of our current study was in determining the reproducibility of epicardial and thoracic fat measurements when using the same scanner (MDCT-MDCT) and when using different scanners (EBCT-MDCT). The scans were acquired on the same visit.
METHODS
Patient population
From a cohort of patients without known coronary artery disease enrolled in the EISNER (Early Identification of Subclinical Atherosclerosis using Non-invasivE Imaging Research) registry at Cedars-Sinai Medical Center, we retrospectively analyzed 48 consecutive patients who underwent 2 non-contrast CT scans for coronary calcium scan on the same day. Of these 48 patients, 25 had both scans obtained with the same 4-slice MDCT scanner (first scan with MDCT, second scan with MDCT, “Intra-scanner”), and 23 had the first scan on an EBCT scanner and the second scan on the 4-slice MDCT scanner (first scan with EBCT, second scan with MDCT, “Inter-scanner”). The characteristics of our patient population are shown in Table 1. The scans were acquired between 2001 and 2003 on EBCT and 4-slice MDCT and individual radiation dose estimates were not reported at that time. However, with prospective ECG triggering, effective radiation doses range from 0.7–1.5 mSv for EBCT systems and from 1–1.9 mSv for MDCT systems.15–19
Table 1.
Clinical characteristics of patients
| Intra-scanner | Inter-scanner | |
|---|---|---|
| Number of patients | 25 | 23 |
| Age, y, mean ± SD | 58 ± 7 | 61 ± 9 |
| Men/Women, n | 13/12 | 13/10 |
| Body mass index; kg/m2, mean ± SD (range) | 28.5 ± 5.2 (20.0–39.5) | 26.7 ± 4.3 (19.7–37.8) |
| Heart rate, bpm, mean ± SD | 68 ± 10 | 62 ± 9 |
CT data acquisition
Non-contrast CT was acquired using an EBCT scanner (e-Speed, GE Healthcare, Milwaukee, WI) or a 4-slice MDCT scanner (Somatom Volumezoom, Siemens Medical Solutions, Forchheim, Germany). Both scanners were calibrated daily using air and water phantoms. Each scan extended from the aortic arch to the diaphragm and was obtained during a single breath-hold. The following scan parameters were used: Heart-rate dependent prospective ECG-triggering (typically 45–60% of the R-R interval), 35 cm field-of-view, and 512×512 matrix size. Tube voltage was 120 kVp with MDCT scanning. Slice thickness was 3 mm for EBCT and 2.5 mm for MDCT. For MDCT scan, immediately after the first scan, without moving the patient off the table, a second scan was performed. All CT images were transferred to a research workstation for epicardial and thoracic fat quantification. This study was conducted according to guidelines of the Cedars-Sinai Medical Center Institutional Review Board. All patients provided written consent for use of their data.
Epicardial and thoracic fat quantification
Epicardial and thoracic fat quantification was performed by software (QFAT) developed at Cedars-Sinai Medical Center, as previously described.1,3 Epicardial fat was defined as adipose tissue enclosed by the visceral pericardium, including fat directly surrounding the coronary arteries. Thoracic fat was defined as all adipose tissue within the chest at the level of the heart, enclosed by the posterior limit of the heart and above the diaphragm, with the same cranial and caudal boundaries defined for epicardial fat. Thoracic fat comprised of both epicardial and extra-pericardial fat outside the pericardium. For defining epicardial contours, the upper slice limit, marked by bifurcation of the pulmonary artery trunk, and lower slice limit, identified as the slice just below the posterior descending artery, were chosen.14 This lower limit was chosen to better distinguish epicardial fat from fat around the diaphragm. As in our previous work 1,2, 5–10 control points on the pericardium in each transverse view were assigned by an experienced imaging cardiologist blinded to patient status and clinical non-contrast CT interpretation. From these control points, piecewise cubic Catmull-Rom spline functions were automatically generated to create a smooth closed epicardial contour 20 for quantification of EFV and TFV (in cm3). Contiguous 3D voxels between the Hounsfield Unit limits of −190 to −30 were defined as fat voxels by default 5, 21–23; these limits could be modified by the user if deemed appropriate. Figure 1 shows a case example of EFV and TFV measurement. All studies were quantified by 2 blinded, experienced imaging cardiologists (reader 1, R.N.; reader 2, H.S.) in random order.
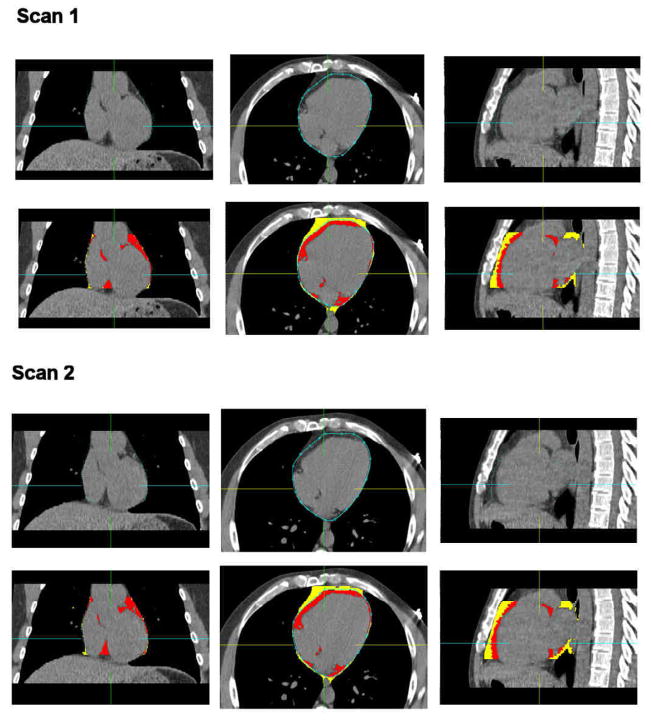
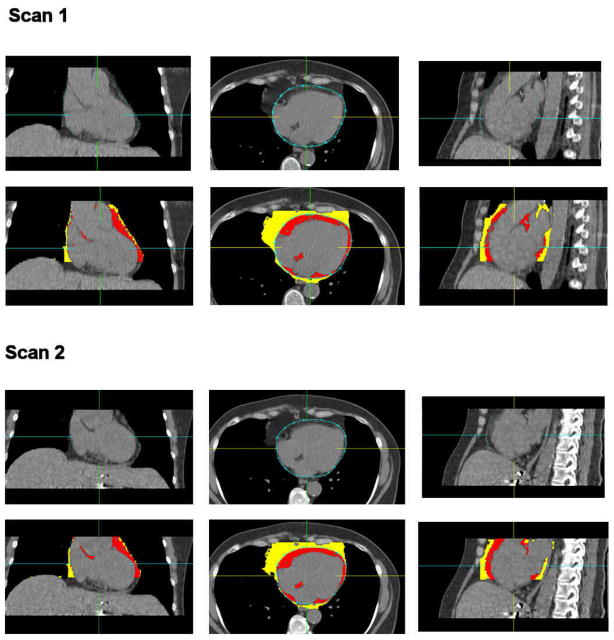
Figure 1.
Figure illustrating epicardial and thoracic fat quantification. Left top: white arrow points to the pericardial sac as a thin band enveloping the heart. Right: pericardial sac (closed curve in blue) is traced by an experienced imaging cardiologist by placing 6–10 control points (shown as blue circles) on the pericardium. Left bottom: Fat quantification results. Red overlay represents epicardial fat enclosed by the pericardium. Yellow overlay represents fat outside the pericardium. Color overlay (Red + Yellow) represents total thoracic fat.
Statistical analysis
Continuous variables are presented as the mean ± standard deviation (SD). Intra-scanner, inter-scanner, same-observer and cross-observer reproducibility were assessed by calculating Pearson’s correlation coefficient with 95% confidence intervals and constructing Bland-Altman plots with 95% limits of agreement.24 Differences and variability in volume quantification were analyzed in absolute terms and in relation to the average of paired measurements. Repeatability coefficient (RC), defined as 1.96 × SD of the differences between pairs of repeated measures, was also determined.25 A p-value <0.05 was considered to be statistically significant. Statistical analyses were performed using Analyse-it Version 2.12 (Analyse-it, Leeds, England).
RESULTS
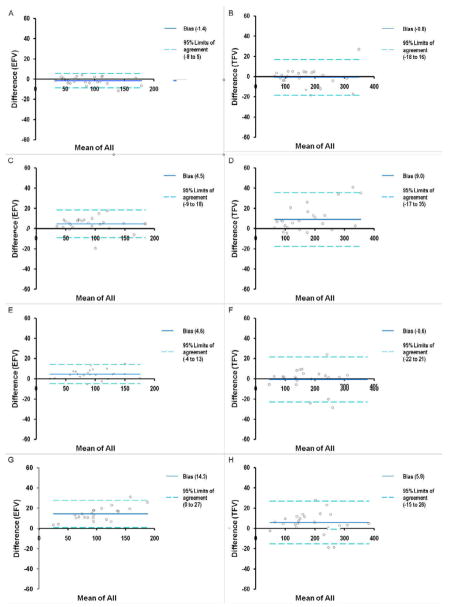
Inter-observer variability was similar for MDCT and EBCT. With MDCT, the inter-observer variability was 8.8 ± 3.9% for EFV and 5.5 ± 4.3% for TFV. With EBCT, inter-observer variability was 9.8 ± 4.2% for EFV and 2.3 ± 2.5% for TFV. Table 2 summarizes the interscan reproducibility results. Correlations for interscan measurements of EFV and TFV were high for both intra-scanner (MDCT-MDCT) and inter-scanner (EBCT-MDCT) data (all correlation coefficient values ≥ 0.98). RC values were lowest (4.3% for EFV and 5.4% for TFV) for intra-scanner same-observer measurement. For intra-scanner cross-observer measurement, RC values were 10.7% for EFV and 9.0% for TFV. For inter-scanner data, RC values ranged from 6.8% to 8.2%. Figures 2 and Figure 3 show examples of 2 scans for 2 patients from our study. Figure 2 shows 2 MDCT scans in the same patient. Figure 3 shows an initial EBCT scan followed by a MDCT scan in the same patient. As expected, cross-observer variability was typically significantly higher than same-observer quantification (Intra-scanner: p = 0.003, 0.04 for EFV and TFV, respectively, Inter-scanner: p < 0.0001, 0.1 for EFV and TFV, respectively). Figure 4 shows the Bland-Altman plots showing interscan differences for EFV (left column) and TFV (right column).
Table 2.
Summary of intra-scanner, inter-scanner, same-observer and cross-observer agreement measures of epicardial and thoracic fat volume
| Correlation coefficient | Mean % % difference | RC (%) | Bias, 95% Limits of agreement (cm3) | |
|---|---|---|---|---|
| A. Intra-scanner, same-observer: reader1 (MDCT scan1 – MDCT scan2) | ||||
| EFV† | 1.00 | 3.5 ± 2.2 | 4.3 | 1.4, −8 to 5 |
| TFV‡ | 0.99 | 3.5 ± 2.7 | 5.4 | 0.8, −18 to 16 |
| B. Intra-scanner, cross-observer: reader1 MDCT scan1 – reader2 MDCT scan2 | ||||
| EFV† | 0.98 | 8.1 ± 5.4 | 10.7 | 4.5, −9 to 18 |
| TFV‡ | 0.99 | 6.6 ± 4.6 | 9.0 | 9.0, −17 to 35 |
| C. Inter-scanner, same-observer: reader1 (EBCT scan1 – MDCT scan2) | ||||
| EFV§ | 0.99 | 5.7 ± 3.9 | 7.7 | 4.6, −4 to 13 |
| TFV* | 0.99 | 4.2 ± 4.0 | 8.0 | 0.9, −22 to 21 |
| D. Inter-scanner, cross-observer: reader1 EBCT scan1 – reader2 MDCT scan2 | ||||
| EFV§ | 0.99 | 14.4 ± 4.2 | 8.2 | 14.3, 0 to 27 |
| TFV* | 0.99 | 5.6 ± 3.4 | 6.8 | 5.8, −15 to 26 |
P values for absolute difference:
p = 0.003,
p = 0.04,
p <0.0001,
p = 0.1
EFV, epicardial fat volume; TFV, thoracic fat volume; RC, repeatability coefficient
Figure 2.
Case example showing the epicardial fat measurements of 2 MDCT scans (scan1, scan2) in a 41-year old man with a BMI of 26.3. Coronal, transverse and sagital slices from the non-contrast CT scan are shown in top panel. Results of epicardial fat quantification are shown in 2nd panel. Red overlay represents epicardial fat enclosed by the pericardium. Yellow overlay represents thoracic fat outside the pericardium. EFVs were 110 cm3 and 113 cm3 and TFVs were 187 cm3 and 192 cm3 for scan1 and scan2, respectively.
Figure 3.
Case example showing the epicardial fat measurements from an initial EBCT scan (scan1) followed by a MDCT scan (scan2) in a 61-year old woman with a BMI of 26.9. Coronal, transverse and sagital slices from the non-contrast CT scan are shown in top panel. Results of epicardial fat quantification are shown in 2nd panel. Red overlay represents epicardial fat enclosed by the pericardium. Yellow overlay represents thoracic fat outside the pericardium. EFVs were 112 cm3 and 109 cm3 and TFVs were 256 cm3 and 236 cm3 for the EBCT and MDCT, respectively.
Figure 4. Bland-Altman plots.
A, B. EFV (A) and TFV (B) agreement of intra-scanner, same-observer: reader1 (MDCT scan1 – MDCT scan2)
C, D. EFV (C) and TFV (D) agreement of intra-scanner, cross-observer: reader1 MDCT scan1 – reader2 MDCT scan2
E, F. EFV (E) and TFV (F) agreement of inter-scanner, same-observer: reader1 (EBCT scan1 – MDCT scan2)
G, H. EFV (G) and TFV (H) agreement of inter-scanner, cross-observer: reader1 EBCT scan1 – reader2 MDCT scan2
DISCUSSION
Our group previously showed high inter-observer reproducibility of epicardial and thoracic fat from a single scan.1, 14 The present study demonstrates a high degree of reproducibility of same and cross-observer measurements of epicardial and thoracic fat from non-contrast CT, including between EBCT and MDCT.
The volume of epicardial fat measured on non-contrast cardiac CT has been associated with coronary atherosclerosis and its pathophysiology including associations to coronary artery disease severity, coronary artery calcification, biochemical markers of systemic inflammation, and increased risk of adverse cardiovascular events.1,3–13 As more data emerges for epicardial fat as a risk marker, its development may extend to serial measurements. Our work reports the interscan variation of this measurement, and further, helps define the lower limit for significant changes in serial epicardial fat volume measurements from cardiac CT.
For both intra-scanner and inter-scanner CT data, variability was significantly less for same-observer than cross-observer measurements. This difference likely reflected consistent observer bias when selecting cranial and caudal heart boundaries and when identifying the pericardial contours. For the same observer, we also observed higher variability when comparing EFV across scanner types. The greater inter-scanner variability may have been due to greater differences between the scans due to breath-hold, as well as differences in EBCT and MDCT technologies. EBCT has greater temporal resolution than 4-slice MDCT, which may have reduced effect of motion on the pericardial contours; however, EBCT data was characterized by higher noise as assessed visually. The temporal resolution of current MDCT scanners (in the range of 83–165 msec) is higher than that of 4-slice MDCT and therefore, EBCT-MDCT reproducibility using current MDCT scanners would be expected to be higher. TFV variability was higher than expected. Since TFV includes both epicardial and extra-pericardial fat, the absolute difference is larger in a few cases due to differences in measured extra-pericardial fat. This was observed especially in the 2 following settings: 1) when a different lower limit was chosen, and 2) in a few cases when there were differences in heart-liver configuration between the 2 scans, extra-pericardial fat around the diaphragm was classified differently. Based upon experience from our center, factors contributing to reproducibility of fat volumes include standardized selection of the heart limits, and identification of the pericardium in non-contrast cardiac CT.
Limitations
This study was a retrospective analysis and sample size was very small. However, we retrospectively studied a select cohort from the EISNER (Early Identification of Subclinical Atherosclerosis using Non-invasivE Imaging Research) study, in whom a second scan was performed on the same patient visit to measure the interscan reproducibility of coronary calcium scoring, and whose scan data are available. The scans were performed between 2001 and 2003. Future studies are needed to investigate these relationships in larger patient cohorts. Although EBCT and MDCT images were of good quality, pre-medication was not given, and obtained data was not completely motion-free. This limitation was important in our MDCT data acquired with 4-slice MDCT scanner where the temporal resolution was 250 msec. Eight cases had at least one motion artifact on MDCT; however, with current MDCT scanners with higher temporal resolution, we would expect fewer motion artifacts. Our reproducibility values indicate, however, that any effect from motion artifacts was likely small. Our method was required operator assistance in determining heart limits and pericardial contour and was thus subject to observer bias. Fully automated quantification of EFV and TFV would result in higher interscan reproducibility.
CONCLUSION
We demonstrated a high degree interscan reproducibility of epicardial and thoracic fat measurements for both when scans were performed only on MDCT and between EBCT and MDCT. The interscan reproducibility reported in our study will help in the establishment of lower limit for significant changes in the CT measurement of epicardial fat, an emerging risk marker for coronary artery disease and future adverse cardiovascular events.
Acknowledgments
This study was supported by NIH grant number R21EB006829-01A2 (PI: Damini Dey) from the National Institute of Biomedical Imaging and Bioengineering (NIBIB), and also in part by a grant from the Glazer Foundation (IRB 6318). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIBIB or the NIH.
List of abbreviations
- EFV
Epicardial fat volume
- TFV
Thoracic fat volume
- CT
Computed tomography
- MDCT
Multi-detector CT
- EBCT
Electron-beam CT
- EISNER
Early Identification of Subclinical Atherosclerosis using Non-invasivE Imaging Research
- RC
Repeatability coefficient
- SD
Standard deviation
Footnotes
Conflict of interest statement:
All authors disclose no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dey D, Wong N, Tamarappoo B, Nakazato R, Gransar H, Cheng V, Ramesh A, Kakadiaris I, Germano G, Slomka P, Berman D. Computer-aided non-contrast ct-based quantification of pericardial and thoracic fat and their associations with coronary calcium and metabolic syndrome. Atherosclerosis. 2010;209:136–141. doi: 10.1016/j.atherosclerosis.2009.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dey D, Suzuki Y, Suzuki S, Ohba M, Slomka P, Polk D, Shaw L, Berman D. Automated quantitation of pericardiac fat from noncontrast ct. Invest Radiol. 2008;43:145–153. doi: 10.1097/RLI.0b013e31815a054a. [DOI] [PubMed] [Google Scholar]
- 3.Cheng V, Dey D, Tamarappoo B, Nakazato R, Gransar H, Miranda-Peats R, Ramesh A, Wong N, Shaw L, Slomka P, Berman D. Pericardial fat burden on ecg-gated noncontrast ct in asymptomatic patients who subsequently experience adverse cardiovascular events. JACC Cardiovasc Imaging. 2010;3:352–360. doi: 10.1016/j.jcmg.2009.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taguchi R, Takasu J, Itani Y, Yamamoto R, Yokoyama K, Watanabe S, Masuda Y. Pericardial fat accumulation in men as a risk factor for coronary artery disease. Atherosclerosis. 2001;157:203–209. doi: 10.1016/s0021-9150(00)00709-7. [DOI] [PubMed] [Google Scholar]
- 5.Wheeler G, Shi R, Beck S, Langefeld C, Lenchik L, Wagenknecht L, Freedman B, Rich S, Bowden D, Chen M, Carr J. Pericardial and visceral adipose tissues measured volumetrically with computed tomography are highly associated in type 2 diabetic families. Invest Radiol. 2005;40:97–101. doi: 10.1097/00004424-200502000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Fox C, Massaro J, Hoffmann U, Pou K, Maurovich-Horvat P, Liu C, Vasan R, Murabito J, Meigs J, Cupples L, D’Agostino RS, O’Donnell C. Abdominal visceral and subcutaneous adipose tissue compartments: Association with metabolic risk factors in the framingham heart study. Circulation. 2007;116:39–48. doi: 10.1161/CIRCULATIONAHA.106.675355. [DOI] [PubMed] [Google Scholar]
- 7.Pou K, Massaro J, Hoffmann U, Vasan R, Maurovich-Horvat P, Larson M, Keaney JJ, Meigs J, Lipinska I, Kathiresan S, Murabito J, O’Donnell C, Benjamin E, Fox C. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: The framingham heart study. Circulation. 2007;116:1234–1241. doi: 10.1161/CIRCULATIONAHA.107.710509. [DOI] [PubMed] [Google Scholar]
- 8.Ding J, Kritchevsky S, Hsu F, Harris T, Burke G, Detrano R, Szklo M, Criqui M, Allison M, Ouyang P, Brown E, Carr J. Association between non-subcutaneous adiposity and calcified coronary plaque: A substudy of the multi-ethnic study of atherosclerosis. Am J Clin Nutr. 2008;88:645–650. doi: 10.1093/ajcn/88.3.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosito G, Massaro J, Hoffmann U, Ruberg F, Mahabadi A, Vasan R, O’Donnell C, Fox C. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: The framingham heart study. Circulation. 2008;117:605–613. doi: 10.1161/CIRCULATIONAHA.107.743062. [DOI] [PubMed] [Google Scholar]
- 10.Mahabadi A, Massaro J, Rosito G, Levy D, Murabito J, Wolf P, O’Donnell C, Fox C, Hoffmann U. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: The framingham heart study. Eur Heart J. 2009;30:850–856. doi: 10.1093/eurheartj/ehn573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarin S, Wenger C, Marwaha A, Qureshi A, Go B, Woomert C, Clark K, Nassef L, Shirani J. Clinical significance of epicardial fat measured using cardiac multislice computed tomography. Am J Cardiol. 2008;102:767–771. doi: 10.1016/j.amjcard.2008.04.058. [DOI] [PubMed] [Google Scholar]
- 12.Mazurek T, Zhang L, Zalewski A, Mannion J, Diehl J, Arafat H, Sarov-Blat L, O’Brien S, Keiper E, Johnson A, Martin J, Goldstein B, Shi Y. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108:2460–2466. doi: 10.1161/01.CIR.0000099542.57313.C5. [DOI] [PubMed] [Google Scholar]
- 13.Greif M, Becker A, von Ziegler F, Lebherz C, Lehrke M, Broedl U, Tittus J, Parhofer K, Becker C, Reiser M, Knez A, Leber A. Pericardial adipose tissue determined by dual source ct is a risk factor for coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 2009;29:781–786. doi: 10.1161/ATVBAHA.108.180653. [DOI] [PubMed] [Google Scholar]
- 14.Tamarappoo B, Dey D, Shmilovich H, Nakazato R, Gransar H, Cheng VY, Friedman JD, Hayes SW, Thomson LEJ, Slomka PJ, Rozanski A, Berman DS. Increased pericardial fat volume measured from noncontrast ct predicts myocardial ischemia by spect. J Am Coll Cardiol Img. 2010;3:1104–1112. doi: 10.1016/j.jcmg.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carr JJ, Crouse JR, Goff DC, D’Agostino RB, Peterson NP, Burke GL. Evaluation of subsecond gated helical ct for quantification of coronary artery calcium and comparison with electron beam ct. AJR Am J Roentgenol. 2000;174:915–921. doi: 10.2214/ajr.174.4.1740915. [DOI] [PubMed] [Google Scholar]
- 16.Becker CR, Kleffel T, Crispin A, Knez A, Young J, Schoepf UJ, Haberl R, Reiser MF. Coronary artery calcium measurement: Agreement of multirow detector and electron beam ct. AJR Am J Roentgenol. 2001;176:1295–1298. doi: 10.2214/ajr.176.5.1761295. [DOI] [PubMed] [Google Scholar]
- 17.Hunold P, Vogt FM, Schmermund A, Debatin JF, Kerkhoff G, Budde T, Erbel R, Ewen K, Barkhausen J. Radiation exposure during cardiac ct: Effective doses at multi-detector row ct and electron-beam ct. Radiology. 2003;226:145–152. doi: 10.1148/radiol.2261011365. [DOI] [PubMed] [Google Scholar]
- 18.Morin RL, Gerber TC, McCollough CH. Radiation dose in computed tomography of the heart. Circulation. 2003;107:917–922. doi: 10.1161/01.cir.0000048965.56529.c2. [DOI] [PubMed] [Google Scholar]
- 19.Flohr TG, Schoepf UJ, Kuettner A, Halliburton S, Bruder H, Suess C, Schmidt B, Hofmann L, Yucel EK, Schaller S, Ohnesorge BM. Advances in cardiac imaging with 16-section ct systems. Acad Radiol. 2003;10:386–401. doi: 10.1016/s1076-6332(03)80027-2. [DOI] [PubMed] [Google Scholar]
- 20.Karthikeyan G, Teo K, Islam S, McQueen M, Pais P, Wang X, Sato H, Lang C, Sitthi-Amorn C, Pandey M, Kazmi K, Sanderson J, Yusuf S. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among asians: An analysis from the interheart study. J Am Coll Cardiol. 2009;53:244–253. doi: 10.1016/j.jacc.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 21.Yoshizumi T, Nakamura T, Yamane M, Islam A, Menju M, Yamasaki K, Arai T, Kotani K, Funahashi T, Yamashita S, Matsuzawa Y. Abdominal fat: Standardized technique for measurement at ct. Radiology. 1999;211:283–286. doi: 10.1148/radiology.211.1.r99ap15283. [DOI] [PubMed] [Google Scholar]
- 22.Kvist H, Chowdhury B, Grangård U, Tylén U, Sjöström L. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: Predictive equations. Am J Clin Nutr. 1988;48:1351–1361. doi: 10.1093/ajcn/48.6.1351. [DOI] [PubMed] [Google Scholar]
- 23.Sjöström L, Kvist H, Cederblad A, Tylén U. Determination of total adipose tissue and body fat in women by computed tomography, 40k, and tritium. Am J Physiol. 1986;250:E736–745. doi: 10.1152/ajpendo.1986.250.6.E736. [DOI] [PubMed] [Google Scholar]
- 24.Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 25.Bland J, Altman D. Applying the right statistics: Analyses of measurement studies. Ultrasound Obstet Gynecol. 2003;22:85–93. doi: 10.1002/uog.122. [DOI] [PubMed] [Google Scholar]