Abstract
We previously showed that rabies virus (RABV) virions are excellent vehicles for antigen presentation. Here, a reverse genetic approach was applied to generate recombinant RABV that express a chimeric protein composed of the heavy chain carboxyterminal half (HC50) of botulinum neurotoxin type A (BoNT/A) and RABV glycoprotein (G). To promote surface expression and incorporation of HC50/A into RABV virions, the RABV glycoprotein (G) ER translocation sequence, various fragments of RABV ectodomain (ED) and cytoplasmic domain were fused to HC50/A. The HC50/A chimeric proteins were expressed on the surface of cells infected with all of the recombinant RABVs, however, the highest level of surface expression was detected by utilizing 30 amino acids of the RABV G ED (HV50/A-E30). Our results also indicated that this chimeric protein was effectively incorporated into RABV virions. Immunization of mice with inactivated RABV-HC50/A-E30 virions induced a robust anti-HC50/A IgG antibody response that efficiently neutralized circulating BoNT/A in vivo, and protected mice against 1000 fold the lethal dose of BoNT/A.
Introduction
Botulinum neurotoxin (BoNT) is produced by the anaerobic soil organisms Clostridium botulinum, Clostridium baratii, and Clostridium butyricum in seven distinct serotypes (serotypes A to G) [1-3]. BoNT toxin causes a serious and potentially life-threatening natural disease called botulism [1], however, the disease can occur as a result of bioterrorism and biological warfare [4]. BoNTs are produced as single-chain protoxins and activated by proteolytic cleavage into disulfide bond-linked di-chains consisting of a 100-kDa heavy chain (HC) and a 50-kDa light chain (LC). The 50-kDa LC contains a catalytic (zinc endopeptidase) domain that targets one of three SNARE (soluble N-ethylmaleimide-sensitive factor attachment protein receptor) proteins of the synaptic vesicle-associated membrane protein synaptobrevin, synaptosomal-associated protein of 25 kDa, or plasma membrane associated SNARE syntaxin. Collectively, the SNARE proteins constitute the core of the vesicular fusion machinery enabling the fusion of neurotransmitter-containing synaptic vesicles with the neuronal plasma membrane, thus allowing the release of neurotransmitter into the synaptic cleft. Cleavage of one of these proteins prevents membrane fusion and release of neurotransmitter from the nerve cell, which results in the cessation of nerve impulses along the axon. The toxin HC contains the cell receptor-binding (fragment C or HC) and translocation (HN) domains necessary for the selective uptake of toxin into the nerve cell via receptor-mediated endocytosis and the subsequent trafficking of the endopeptidase across the endosomal membrane into the cytosol, where SNARE protein inactivation occurs [5, 6].
Inactivated rabies virus (RABV) has long been used to vaccinate humans with a significant history of safety [7, 8], and induction of potent and long-lasting neutralizing antibodies to the RABV glycoprotein (G) [9]. In addition, strong humoral responses to heterologous proteins, such as, HIV-1 envelope [10, 11]; HCV E1/E2 [12]; and anthrax PA [13] were elicited by inactivated RABV virions incorporating these foreign proteins. The highly repetitive and rigid organization of viruses and virus-like particles is thought to maximally stimulate B cells [14, 15]. Additionally, CD4+ T helper cell epitopes that are necessary for B cell activation can be provided by the virus-like particles [16].
Vaccination is an effective strategy for providing protection against botulinum toxin by eliciting neutralizing antibodies that would prevent binding of the toxin to an appropriate receptor and promote clearance and degradation by phagocytosis. Chemically detoxified botulinum vaccines have played an important role in providing active immunity against the neurotoxin [17], and for production of equine-based antitoxins and botulism immune globin for treating botulism by passive immunization [18-21]. However, recombinant technology has provided the means by which highly purified and efficacious antigens can be produced in adequate quantities without the need to culture and manipulate large volumes of C. botulinum and its neurotoxin [22-24]. BoNT(HC) delivery has been reported using naked DNA [25, 26], virus vector system [27-31] and attenuated Salmonella typhimurium strains [32].
Here, we generated several chimeric RABV G-HC50/A fusion proteins containing the RABV G ER translocation sequence (SS), various RABV ectodomain (ED) fragments (5-51 aa) and the RABV transmembrane TM and cytoplasmic domain (CD). HC50/A chimeric protein was expressed at the highest level on the surface infected BSR cells when a 30 aa fragment of the RABV ED was utilized, which resulted in efficient incorporation into RABV virions, as well. Mice vaccinated with inactivated RABV-HC50/A-E30 virions mounted neutralizing antibody response against BoNT even when low amounts of the vaccine was used. In addition, vaccination with inactivated RABV-HC50/A-E30 virions led to rapid clearance of the toxin from the circulation and elicited protective immunity in mice against lethal BoNT/A challenge. These results provide further evidence the potent immunostimulatory potential of inactivated RABV, which can serve as a new carrier for immunization against various pathogens.
Materials and Methods
Plasmid construction and virus recovery
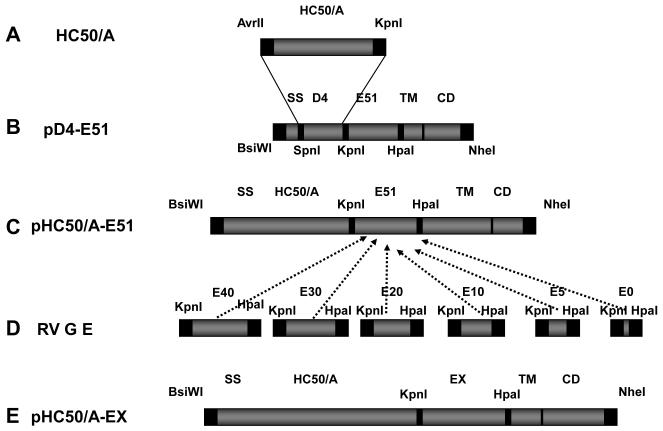
The plasmid pD4-E51 has been described previously. In brief, pD4-E51 encodes the first 22 N-terminal amino acids (aa) including the rabies virus (RABV) G protein endoplasmic reticulum (ER) translocation signal sequence (SS) that is fused to domain 4 (D4) of Bacillus anthracis protective antigen (PA). The D4 domain is followed by last 51 C-terminal aa of RABV G ectodomain (E), 22 aa of RABV transmembrane domain (TM), and 44 aa of RABV cytoplasmic domain (CD) [13]. To create an expression plasmid encoding the carboxyterminal half (HC50/A) of botulinum neurotoxin type A (BoNT/A) in the same vector as D4, the gene segment (flanked by AvrII and KpnI) encoding the HC50/A (strain 62A, accession no. M30196, amino acids 865–1296) was amplified by PCR from pQE-HC50/A [33] using Vent polymerase (New England Biolabs, Beverly, MA), and the forward primer HC50-P and reverse primer HC50-M (Table 1). The 1.3 Kb HC50/A PCR product was digested with AvrII/KpnI and cloned into pD4-E51 predigested with SpeI/KpnI resulting in p-HC50/A-E51. Smaller fragments of RABV G ectodomain (E) were amplified from pTIT-G [34] using the forward primers RABV-E40, RABV-E30, RABV-E20, RABV-E10, RABV-E5 or RABV-E0, and reverse primer RABVG-ED-M flanked by KpnI and HpaI (Table 1). The various RABV G E PCR fragments and plasmid pHC50/A-E51 were digested by KpnI/HpaI, and the various ectodomain fragments were ligated to generate pHC50/A-E0 - E51. To construct the chimeric RABV expressing HC50/A, the fusion genes HC50/A-E0 - E51 were digested with BsiWI and NheI and ligated into the BsiWI and NheI predigested pSPBN [35] resulting in pHC50/A-E0 – E51. The resulting pHC50/A-E0 - E51 were used to transfect BSR cells (BHK clone). T7 RNA polymerase drives expression of RABV proteins N, P and L after simultaneous transfection of the cells with the plasmids that encode RABV N, P and L proteins. The resulting chimeric rabies virus constructs are termed RABV-HC50/A-E0, -E5, -E10, -E20, -E30, -E40 and -E51. All recombinant viruses were recovered using published methods [36].
Table 1.
| PCR Primers | |
|---|---|
| HC50-P | 5′-AAACCTAGGAGATTATTATCTACATTT ACTGAAT-3′ |
| HC50-M | 5′-TTTGTTAACCAGTGGCCTTTCTCCCCA T-3′ |
| RABV-E51 | 5′-CCCGTTACCGAATCCTCGGTTATCCCCCTTG-3′ |
| RABV-E40 | 5′-CCCGTTACCGCAGACCCGTCTACCGTTTTC-3′ |
| RABV-E30 | 5′-CCCGTTACCGACGAGGCTGAGGATTTTGTTG-3′ |
| RABV-E20 | 5′-CCCGTTACCCTTCCCGATGTGCACAATCAGG-3′ |
| RABV-E10 | 5′-CCCGTTACCGTTGACTTGGGTCTCCCGAACT-3′ |
| RABV-E5 | 5′-CCCGTTACCCCGAACTGGGGGAAGGTTAACT-3′ |
| RABV-E0 | 5′-CCCGTTACCGTTAACTATGTATTACTGAGTGC-3′ |
| RP80-M | 5′-CCCTCTAGAGGTACCTTACAGTCTGGTCTCACCC-3′ |
Virus purification and inactivation
BSR cells were infected at a multiplicity of infection (MOI) of 0.1 in OptiPro medium (Invitrogen, Carlsbad, CA) innoculum supplemented with 1% Penicillin/Streptomycin and 4 mM L-Glutamine and incubated for 2 h with frequent gentle agitation. Then OptiPro medium was added and virus was harvested at 3 and 6 days post-infection. Supernatants from the two harvests was layered over 20% sucrose gradient and purifies by ultracentrifugation using an SW28 rotor at 24,000 RPM for 1 h at 4 °C. Purified material was resuspended in TEN buffer (0.1 M NaCl, 10 mM Tris-HCl pH 8.0 and 1 mM EDTA pH 8.0) and incubated overnight at 4 °C. β-propiolactone (Sigma, St. Louis, MO) diluted 1:100 in ice-cold dH2O was added to the virion preparation to a final BPL concentration of 1:2000 and incubated overnight at 4 °C followed by 30 min at 37°C. Concentration of inactivated virions was estimated by BCA protein assay (Pierce Chemical, Rockford, IL) and stored in aliquots at −80 °C. Lots of virion preparations were analyzed by Coomassie staining and Western blotting.
Botulinum neurotoxin BoNT/A and recombinant HC50
Native BoNT/A was isolated from bacterial cultures as described previously [37-39]. The isolated neurotoxin had a homogeneity >98%, as determined by polyacrylamide gel electrophoresis [40]. The carboxyterminal portion of the heavy chain of BoNT/A was cloned, expressed and purified as reported previously [33].
Western blotting
BSR cells grown in DMEM (Mediatech, Manassas, VA) supplemented with 5% fetal bovine serum and 1% Penicillin/Streptomycin were infected for 48 at 37 °C and 5% Co2 with RABV-HC50/A-E0 - E51 at MOI of 10. The cells were washed twice with PBS and incubated with lysis buffer (1% NP-40, 0.4% deoxycholate, 66 mM EDTA, 10 mM Tris–HCL, protease inhibitor, 0.1% SDS) for 30 min on ice. The cell lysates and purified virus were prepared for Western blotting analysis by adding protein-loading solution to a final concentration of 2% β-mercaptoethanol and heating for 10 min at 95 °C. Proteins were separated by 4-12% sodium dodycyle sulphate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a nitrocellulose membrane (Osmonics, Minnetonka, MN). Blots were blocked with 5% nonfat milk in 0.1% PBS Tween-20 and incubated overnight at 4° C on a shaker with 1:5000 polyclonal rabbit anti-Botulinum toxin HC50/A and 1:5000 polyclonal rabbit anti-RABV M, followed by incubation with horse raddish HRP-conjugated donkey anti-rabbit IgG [12]. Chemiluminescence substrate was applied as instructed by the manufacturer (Sigma Inc.).
Animals and vaccination protocols
Six to 8-week-old female Swiss Webster mice (NCI) were immunized (five mice per group) by the intramuscular (i.m.) route with 10 μg RABV-HC50/A; 10 μg RABV-HC50/A adsorbed onto 0.2% aluminium hydroxide (alum); 20 μg recombinant adsorbed HC50/A onto 0.2% alum; or 10 μg inactivated RABV-D4-E51, a RABV that expresses an irrelevant antigen. A group of mice was left untreated to serve as naïve control. The mice were boosted 2 weeks after the initial dose and blood was collected by retro-orbital bleeding 2 days before the boost and 5 days after the boost. For dose–response studies, groups of mice (four per groups) were immunized as above with 40 μg , 20 μg, 10 μg, 5 μg or 0.5 μg RABV-HC50/A. The mice were boosted 2 weeks later and blood was collected as described above 5 days after the boost.
ELISA
ELISA plates (96-well) were coated with 0.5 μg/well rHC50/A or 100 ng/well RABV G in coating buffer (5 mM Na2CO3, pH 9.6) overnight at 4 °C. Plates were washed three times in PBS-Tween-20 and blocked with 5% non-fat milk in PBS for 1 h at room temperature. Then 100 μl of three-fold dilution of sera were applied to wells and incubated overnight at 4 °C. After washing plates 3 times, 100 μl HRP-conjugated goat anti-mouse IgG (Jackson ImmunoResearch, West Grove, PA) diluted in PBS was added per well and incubation continued at 37 °C for 30 min. Plates were washed as above before OPD substrate (Sigma), prepared according to the manufacturer’s instructions, was added to wells. Incubation was continued for 15-30 min at room temperature in the dark, and finally the reaction was stopped by addition of 50 μl 3 M H2SO4. Optical density was determined at 490 nm.
Botulinum toxin challenge of animals
The characteristic of BoNT actions is neuromuscular blockade that lead to weakness and eventual paralysis of the muscles of locomotion and respiration. The specific activity of the toxin utilized in this study: 1 mouse LD50 = 5 to 7 pg. Mice received 5 ng BoNT/A which is about 103 mouse LD50, an amount sufficient to produce paralysis of respiration and death within minutes (ca. 100 to 120 min). Groups of vaccinated and naïve mice were challenged by intraperitoneal injection with 5 ng BoNT/A. To minimize the pain and suffering, animals were observed throughout the various protocols for 5 days. When signs of neuromuscular weakness became obvious, animals were sacrificed in accordance with AAALAC guidelines. All animals were handled in strict accordance with good animal practice as defined by the relevant international (Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) (Accreditation Status TJU: Full)) and national (TJU Animal Welfare Assurance Number: A3085-01), and all animal work was approved by the Institutional Animal Care and Use Committee (IACUC) at Thomas Jefferson University TJU.
Serum BoNT/A toxin capture immunoassay
For BoNT/A blood clearance studies, groups of mice (three per group) were immunized and boosted 2 weeks later with 10 μg RABV-HC50/A, 10 μg RABV-HC50/A and alum, 10 μg recombinant HC50/A and alum, or left untreated. A week after the boost the mice were challenged with 5 ng BoNT/A intravenously. Blood was collected as above 1 min, 2 min, 4 min, 8 min and 16 min after the challenge to assay the amount of toxin in the blood by capture immunoassay. Botulinum toxin was quantified with a luminescent sandwich immunoassay by using a human monoclonal antibody as a capture device (gift from Dr. Scott Dessain, Lankenau Institute for Medical Research) and rabbit polyclonal anti-BoNT HC antibodies as part of a reporter device. Monoclonal anti light-chain antibodies were diluted in phosphate buffered saline to a concentration of 3 μg/ml and coated on black Nunc Maxisorp 96-well plates (100 μl per well). Plates were covered and stored overnight at 4C. Plates were blocked with 300 μl per well of 2% non-fat dry milk in phosphate buffered saline with 0.05% 300 μl per well of 2% non-fat dry milk in phosphate buffered saline with 0.05% Tween-20 (NFDM/PBST) for 1 hour at 37°C. Blocking solution was discarded and plates were washed 3x with phosphate buffered saline with 0.05% Tween-20 (PBST). Standards and experimental plasma samples were diluted 1:1 in phosphate buffered saline then added in triplicate to plates (50 μl per well). Plates were covered and shaken slowly at room temperature for 1 hour, then washed 3x with PBST. Affinity purified, biotinylated anti-heavy chain antibodies were diluted in NFDM/PBST to a concentration of 3 μg/ml and added to plates (50 μl per well). Plates were incubated for 1 hour at 37°C then washed 3x with PBST. A streptavidin poly-horseradish peroxidase conjugate was diluted to a concentration of 300 ng/ml in NFDM/PBST and added to plates (50 μl per well). Plates were incubated for 30 minutes at 37°C, followed by 6 washes with PBST. Plates were injected with 50 μl per well luminol (Thermosci SuperSignal ELISA Femto Substrate) and relative luminescence values were measured with a Biotek Synergy 2 Luminometer.
Results
Rabies virus expressing BoNT/A-HC50
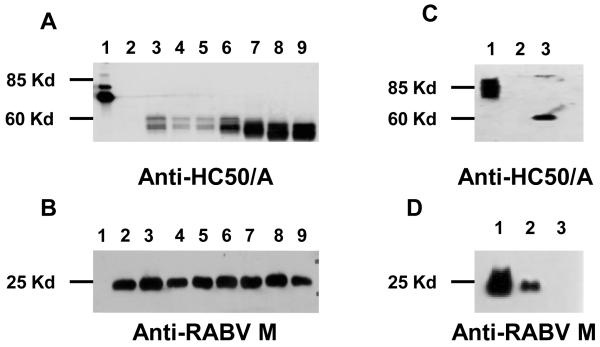
The 50 kDalton (kD) portion of BoNT HC50 (serotype A, BoNT/A-HC50) is an excellent target for a vaccine against botulinum since anti-BoNT/A-HC50 neutralizing antibodies can prevent entry of the toxin into cells, however, HC50 itself is not toxic [41]. We previously showed that a bacterial protein (D4 of Anthrax PA) can be incorporated into RABV virions utilizing the RABV G SS, part of its ED, as well as the TM and CD (Smith et al., 2006). Therefore, a similar approach was utilized to synthesize chimeric RABV G-BoNT/A-HC50 fusion proteins. In the first step, we replaced Anthrax D4 from pD4-E51 with HC50/A resulting in pHC50/A-E51 (Figure 1). Because the requirements of the length of the RABV G E for HC50/A surface expression was unknown, we also constructed chimeric RABV G-HC50/A fusion proteins containing various portions of RABV G N-terminal E of 0, 5, 10, 20, 30, 40 aa resulting in the expression plasmids pHC50/A-E40, -E30, -E20, -E10, -E5 and -E0. The genes encoding the chimeric RABV G-HC50/A proteins were cloned into the RABV expression vector SPBN utilizing the single BsiWI and NheI site between RABV G and L and infectious virus recover by standard methods (Figure 1) [35]. Expression of the chimeric RABV G-HC50/A fusion protein by the recombinant virus constructs RABV-BoNT/A-HC50-E0, 5, 10, 20, 30, 40 and 51 was analyzed by Western blotting of lysates from infected BSR cells. The results shown in Figure 2A show that all recombinant RABV expressed the RABV G/HC50 fusion protein. However, the highest expression levels were observed for the chimeric proteins containing a RABV G ED portion between 20-51 aa. Equal infection of the cells by all eight viruses was confirmed with an RAVB matrix protein (M) specific antibody (Figure 2 B). In the next step, we analyzed the surface expression of the chimeric RABV G-HC50 proteins by FACS. Although surface expression of HC50/A was observed for all BSR cells infected with the seven recombinant RABV-HC50/A-E0 to E51, the highest expression was detected on cells infected with the recombinant RABV-HC50/A-E30 (data not shown).
Figure 1. Construction of Chimeric rabies virus (RABV) expressing botulinum neurotoxin type A carboxyterminal half (HC50/A) fused to various RABV G ectodomain fragments.
PCR amplification of HC50/A (A), and ligation into pD4-E51 (B) after digestion of D4, resulting in pHC50/A-E51 (C). Amplification of various RABV G ectodomain fragments (D), and ligation of the RABV G ectodomain fragments to generate pHC50/A-E0, -E5, -E10, -E20, -E30, -E40 and – E51.
Figure 2. Characterization of chimeric carboxyteriminal half (HC50/A) of botulinum neurotoxin A (BoNT/A).
To characterize expression of HC50/A, BSR cells were infected with the chimeric RABV-HC50/A-E51 – E0 at multiplicity of infection of 10 (MOI) for 48 h. RABV-recombinant HC50/A, lane 1 and lysates of BSR cells infected with RABV-D4-E51, lane 2; RABV-HC50/A-E0, lane 3; RABV-HC50/A-E5, lane 4; RABV-HC50/A -E10, lane 5; RABV-HC50/A-E20, lane 5; RABV-HC50/A-E30, lane 7; RABV-HC50/A-E40, lane 8; or RABV-HC50/A-E51 were separated by SDS-PAGE, and transferred to a nitrocellulose membrane then probed with anti-HC50/A (panel A) or anti-RABV G (Panel B). Inactivated RABV-HC50/A-E30 virions, 1ane 1; inactivated RABV-D4-E51 virions, lane 2; and recombinant HC50/A, lane 3, were separated by SDS-PAGE and transferred to a nitrocellulose membrane then probed with anti-HC50/A (panel C), or anti-RABV G (panel D).
Therefore, RABV-HC50/A-E30 was chosen as our vaccine construct, and we will refer to this construct as RABV-HC50/A. Of note, the cell substrate surface expression of a foreign protein is a prerequisite for incorporation into RABV virions, however, the successful incorporation of HC50 into budding RABV needed to be analyzed experimentally. For this approach, BSR cells were infected with RABV-HC50/A at an moi of 0.01 for 6 days and supernatants of the infected cells was purified over 20% sucrose. Purified virons were inactivated with β-propiolactone and viral proteins were separated by SDS Page followed by Western blotting and probing with a HC50 or RABV-specific antibody. The results in Figure 2C indicate that the chimeric HC50/A-E30 protein was incorporated into the RABV virons, and therefore, such particles can be used for immunizations.
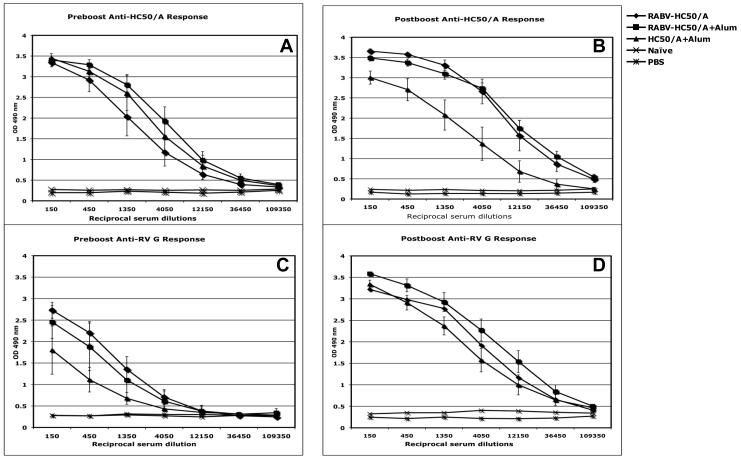
Inactivated recombinant RABV expressing HC50/A is immunogenic in mice
It has been previously shown that the carboxy-terminal portion of BoNT/A (generated by proteolysis of the wild-type toxin or by recombinant techniques) can be utilized as an injectable vaccine that is effective against challenge with BoNT [42, 43]. As an initial test of immunogenicity of our novel vaccine RABV-based vaccine, four groups of Swiss Webster mice (five mice each) were primed with 10 μg inactivated RABV-HC50/A, 10 μg inactivated RABV-HC50/A admixed with 0.2% final aluminium phosphate adjuvant (alum), inactivated 10 μg RABV-D4-E51 chimeric RABV expressing an unrelated antigen or 20 μg HC50/A with alum. The mice were boosted 2 weeks later with same dose of the same antigen. Small amounts of blood was collected from all animals by retro-orbital bleeding 2 days before and 7 days after the boost. Sera were analyzed for specific anti-HC50/A or -RABV G antibody response by ELISA. The results shown in Figure 3 indicate a HC50/A-specific IgG immune response against HC50/A in the mice immunized with RABV-HC50/A, RABV-HC50/A with alum, and recombinant HC50/A with alum after the initial immunization (Fig 3 A). Of note, the admixture of the purified virions with alum was not necessary to induce an immune response, whereas adjuvant is essential when utilizing recombinant HC50 [44] . After the boost immunization, higher titered responses were observed in mice immunized with RABV-HC50/A and RABV-HC50/A with alum, whereas the response to the recombinant HC50/A with alum adjuvant group did not increase (Fig 3 B). After the boost there was no difference in the anti-HC50 response in mice immunized with RABV-HC50/A in the presence or absence of alum (Fig 3 A and B). As expected, an IgG response against RABV G was observed in mice immunized with RABV-HC50/A, RABV-HC50/A with alum, and RABV-D4-E51, but not for recombinant HC50/A, following priming and after the boost (Fig 3 C and D). Mice immunized with RABV-D4-E51 mounted an IgG response against RABV G, whereas HC50 response was not observed in these mice.
Figure 3. Induction of humoral immune response against carboxyterminal half (HC50/A) of botulinum toxin and rabies virus (RABV) G.
Groups of 5 mice were immunized and boosted 2 weeks later with 10 μg inactiavated purified RABV-HC50/A; RABV-HC50/A and aluminium phosphate (Alum) adjuvant; 20 μg recombinant HC/50/A and Alum; or untreated. The mice were bled 2 days before the boost and 7 days after the boost, and sera were analyzed by ELISA. Mean value and standard deviation of specific anti-HC50/A IgG response (panel A and B) RABV-HC50/A, ◆; RABV-HC50/A and alum, ■; HC50/A and Alum, ▲; untreated, ×. For anti-HC50/A response (A), the preboost 50% dilution titer of sera from mice immunized with RABV-HC50/A is 1:2250; RABV-HC50/A and Alum 1:6750; and HC50/A is 1:4050, and the postboost (B) 50% dilution of sera from mice immunized with RABV-HC50/A and RABV-HC50/A and Alum is 1:12150, and from mice immunized with HC50/A is 1:6750. Mean value and standard deviation of specific anti-RABV G analyzed by ELISA (panel C and D) for inactiavated purified RABV-HC50/A, ◆; RABV-HC50/A and Alum, ■; RABV-D4-E51, ▲; and HC50/A and Alum, ×. For anti-RABV G response, the preboost (C) 50% dilution titer of sera from mice immunized with RABV-HC50/A is 1:2025; RABV-HC50/A and Alum 1:1350; and RABV-D4-E51 is 1:950, and the postboost (D) 50% dilution of sera from mice immunized with RABV-HC50/A and RABV-HC50/A and Alum is 1:12150 and from mice immunized with RABV-D4-E51 is 1:4050.
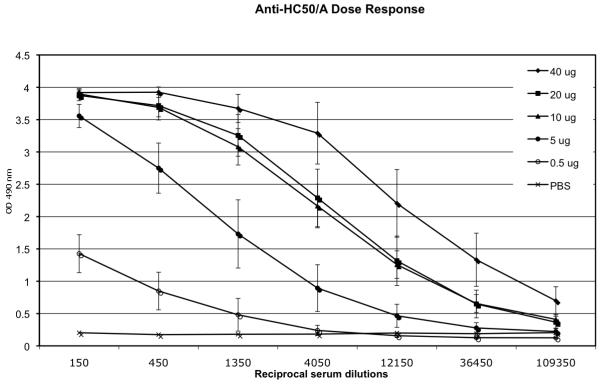
In order to determine the amount of vaccine (e. g. inactivated RABV-HC50/A virons) required to induce seroconversion against HC50/A, groups of four Swiss Webster mice were immunized with 0.5 μg, 5 μg, 10 μg, 20 μg and 40 μg of RABV-HC50/A virions and the antibody response against HC50/A was determined by ELISA (Fig 4). A typical dose response was observed as the titers of the sera from mice receiving 40 μg of virions was approximately 15 times greater than titers from mice receiving 5 μg of virions. Specific HC50 antibodies were also detected in mice immunized with the lowest dose (0.5 μg) but at a lower titers. These results indicate that RABV derived particles containing HC50 are potent vaccines over a wide range of antigen concentration utilized for vaccination, which indicates promise for the use of this vaccine platform.
Figure 4. Induction of dose-response anti-HC50/A. Groups of five mice were immunized and boosted 2 weeks later with 0.5 μg, 5 μg, 10 μg, 20 μg or 40 μg of inactivated chimeric rabies virus RABV-HC50.
The mice were bled 7 days after the boost and sera were analyzed by ELISA. The mean and standard deviation of specific anti-HC50 responses was plotted for each dose: 40 μg, ◆; 20 μg, ■; 10 μg, ▲; 5 μg, ● or 0.5 μg, ○; and control PBS, ×. The 50% dilution titer of sera from mice immunized with 40 μg was 1:20250, with 20 μg was 1:6750, with 10 μg was 1:5400, with 5 μg was 1:1350 and with 0.5μg was 1:900. ◇
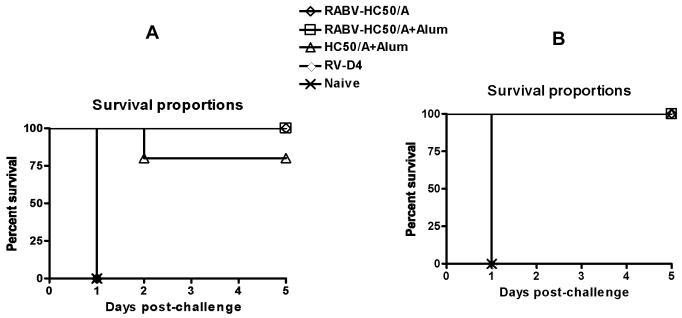
BoNT/A challenge
The results from the challenge experiment were promising since each of the three vaccine groups RABV-HC50/A, RABV-HC50/A with alum, and recombinant HC50/A with alum demonstrated protection of mice challenged with a high dose of botulinum toxin (5 ng 103 mouse LD50). Mice receiving a prime and boost with 10 μg of either RABV-HC50/A or RABV-HC50/A with alum and subsequently challenged demonstrated 100% survival compared to 80% survival for mice receiving recombinant HC50/A with alum (FIG. 5A). In contrast, 100% of the mice vaccinated with the rabies virus vector control, RABV-D4-E51, and untreated mice succumbed to the toxin challenge and died 120 to 140 min after the challenge (Fig. 5A). In a second confirmatory set of experiments (Fig. 5B) immunization with each of the three vaccines resulted in 100% survival of mice post botulinum challenge. All mice (100%) receiving the RABV-D4-E51 control and untreated mice died 120 to 140 min after botulinum toxin challenge .
Figure 5. Percent survival after botulinum toxin challenge.
Groups of five mice were immunized and boosted 2 weeks later with 10 μg inactivated purified RABV-HC50/A, ◇; RABV-HC50/A with alum, □; 20 μg recombinant HC/50/A with alum, △; RABV-D4-E51, ◆; or untreated, X. Vaccination with RABV-HC50/A, RABV-HC50/A with alum, and recombinant HC50/A with alum significantly increased survival of the botulinum toxin challenged mice to 100%, 100% and 80%, respectively (A). In a second independent experiment (B) the three vaccines increased survival of the botulinum toxin challenged mice to 100%. All mice in the untreated and rabies virus vector control groups developed respiratory paralysis and died after 120 to 140 min 1 after the challenge (A, B)
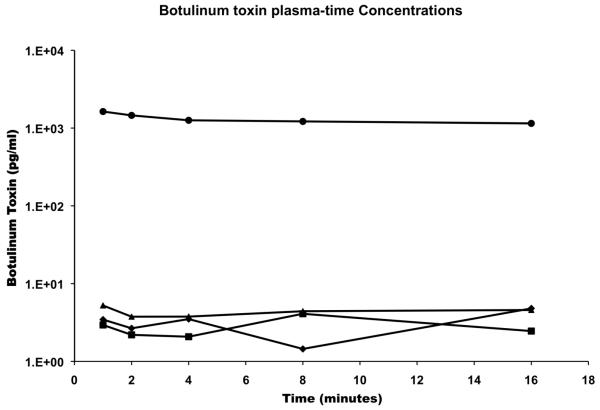
Rapid clearance of free BoNT/A from the blood of immunized mice
Several mechanisms have been suggested by which antibodies against BoNT/A can eliminate the effects of the toxin. One possibility is that antibodies block binding of the toxin domain before translocation of the toxin into neuoronal cells [5]. To determine the presence of free BoNT/A in blood from vaccinated animals, groups of mice (three mice per group) were immunized and boosted with 10 μg of RABV-HC50/A, RABV-HC50/A with alum, recombinant HC50/A with alum, or left untreated. A week after the boost the mice were challenged by intravenous route with 5 ng botulinum neurotoxin type A (103 mouse LD50), and blood was collected by retro-orbital bleeding at the indicated time points after the challenge. Figure 6 shows that only traces of free toxin at the detection level of the utilized assay were detectable in pools of plasma from mice immunized with the three vaccines indicating an instantaneous and rapid elimination of the toxin from the circulation in as early as 1 min after the challenge. On the contrary, steady and high levels of toxin were detectable at all time points studied after the challenge in the untreated group of mice.
Figure 6. Plasma botulinum toxin level after challenge of vaccinated mice.
Groups of mice (three mice per group) were immunized and boosted with RABV-HC50/A, RABV-HC50/A and alum, recombinant HC50/A and alum or left untreated. The mice were challenged one week after the boost by the intravenous route with 5 ng botulinum neurotoxin (103 mouse LD50), and blood was collected by retro-orbital bleeding at the indicated time points after the challenge. The figure shows levels of botulinum toxin detectable in plasma pools from mice vaccinated with RABV-HC50/A,■--■; RABV-HC50/A+alum◆--◆; HC50/A and alum, ▲--▲; and untreated mice, ●--●.
Discussion
In the present study we describe development of a novel approach to develop a vaccine against botulism using inactivated RABV virions as a platform to present the BoNT HC50/A immunogen. Botulism can occur naturally, however, potential use of the toxin as an act of bioterrorism or biological warfare motivated development of this vaccine [4]. Virus particles present antigens in dense and repetitive manner that maximally stimulate B cell proliferation and antibody production [45]. Additionally, the virus particles can provide CD4+ T cell epitopes that supply the second signal required for B cell activation [46]. Subunit vaccines have emerged as a favored candidate vaccine against botulism [42]. The carboxyterminal half of the botulinum toxin has been the antigen of choice for development of the vaccine since it enables working in a non-toxic environment thereby increasing safety [42], as well as, decreasing the cost in comparison with working with the fully active toxin [47]. We generated recombinant RABV particles that display an etiologic agent of botulism, the carboxy-terminal half of botulinum toxin. As previously shown for the incorporation of domain four of the protective antigen (PA) of Anthrax into RABV virions [13], incorporation of HC50 also required the addition of the RABV G ED, but of a different size. In both case, the recombinant RABV G fusion protein in virions was only detected by Western blotting, indicating that incorporation of such proteins into budding RABV virions is less efficient than that of RABV G protein. We can only speculate about the amount of RABV G-HC50 in the RABV particles, however, RABV G is 24% of the RABV virion mass [48]. Therefore, the chimeric RABV G HC-50 protein would be 12% of the virion mass if incorporated as efficient as RABV G. Because we neither saw a reduction of RABV G in the recombinant virions (which would be replaced by the RAB-HC50/A-E30 fusion protein) nor we were able to detect RAB-HC50/A-E30 in the coomassie stained gel analyzing the virions, the amount is less, probably around 1-5%, which would result in an estimated amount of 0.1 to 0.5 μg in of 10 ug virions, which were used for the immunizations.
Nevertheless, the fusion protein, RABV G-HC50/A-E30, incorporated into the recombinant virions, induced a strong humoral immune response in vaccinated mice. The magnitude of the RABV-HC50/A induced immune response induced in mice was greater than that induced with recombinant HC50/A admixed with alum. The botulinum toxin is a large protein that has numerous linear and conformational epitopes. There are reported to be a greater numbers of epitopes in the HC50 polypeptide than there are in the rest of the toxin molecule [49-51]. Many of these epitopes are potential antibody binding binding sites that can mark the toxin molecule for enhanced clearance from the circulation.
The gold standard for effective neutralization is the demonstration of protection against the lethal effects of the toxin in vaccinated mice. The present study clearly shows the ability of two doses of recombinant RABV-HC50/A virus to evoke immunity against a lethal challenge dose of native botulinum toxin (1× 103 LD50). There was complete immunity and 100% survival of the vaccinated mice in the two independent experiments compared with 80% and 100% survival in mice immunized with the recombinant HC50/A vaccine.
The HC50/A domain of BoNT is already known be an effective vaccine against botulism. However, this study provided further proof for the concept of the potential of RABV recombinant vaccine. Moreover, the RABV vaccine platform seems to work efficiently within a large range of antigen concentration without adjuvant, which is not the case for recombinant HC50 protein, which requires potent adjuvant and high concentration of antigen [41].
Many previous reports documented that antibodies raised against the carboxyterminal half of botulinum toxin can neutralize toxin, but few have described the underlying mechanisms. Association of antibodies with the toxin has been shown to enhance toxin clearance from the circulation, as well as to prolong the paralysis times of neuronal tissues [41]. In this study, we also evaluate mechanism of toxin neutralization and found that our recombinant RABV-HC50/A RABV have induced a rapid and complete neutralization of the toxin from the circulation, and only traces of the toxin were detectable 2 minutes after challenge with the toxin.
In summary, we showed that the display of HC50 by RABV virions is a novel approach for producing a potent BoNT vaccine. Further work will be directed to the inclusion of more serotypes of BoNT (e.g. B and E), larger scale production of the vaccine and clinical testing of this vaccine.
Acknowledgements:
The authors thank Marie-Luise Faber for technical assistance. This work was supported by a grant from NIH/NIAID to M.J.S. (R41AI073064).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential conflicts of interest: E.M., M.-L. F., and J. A. M. were/are employees of Molecular Targeting Technologies, Inc. (MTTI Inc.) M.J.S. is a consultant to MTTI and is an inventor and co-inventor of several patents on RABV based vaccines and vaccine-based vector, including the technology utilized here. MTTI Inc. holds an option for the technology utilizing RABV particles as carrier for HC50-based vaccines from TJU. L.L. Simpson is an inventor of several BoNT related patents.
References
- [1].Hatheway CL. Botulism: the present status of the disease. Curr Top Microbiol Immunol. 1995;195:55–75. doi: 10.1007/978-3-642-85173-5_3. [DOI] [PubMed] [Google Scholar]
- [2].Shukla HD, Sharma SK. Clostridium botulinum: a bug with beauty and weapon. Crit Rev Microbiol. 2005;31(1):11–8. doi: 10.1080/10408410590912952. [DOI] [PubMed] [Google Scholar]
- [3].Turton K, Chaddock JA, Acharya KR. Botulinum and tetanus neurotoxins: structure, function and therapeutic utility. Trends Biochem Sci. 2002 Nov;27(11):552–8. doi: 10.1016/s0968-0004(02)02177-1. [DOI] [PubMed] [Google Scholar]
- [4].Arnon SS, Schechter R, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, et al. Botulinum toxin as a biological weapon: medical and public health management. JAMA. 2001 Feb 28;285(8):1059–70. doi: 10.1001/jama.285.8.1059. [DOI] [PubMed] [Google Scholar]
- [5].Schiavo G, Matteoli M, Montecucco C. Neurotoxins affecting neuroexocytosis. Physiol Rev. 2000 Apr;80(2):717–66. doi: 10.1152/physrev.2000.80.2.717. [DOI] [PubMed] [Google Scholar]
- [6].Simpson LL. Identification of the major steps in botulinum toxin action. Annu Rev Pharmacol Toxicol. 2004;44:167–93. doi: 10.1146/annurev.pharmtox.44.101802.121554. [DOI] [PubMed] [Google Scholar]
- [7].Haupt W. Rabies--risk of exposure and current trends in prevention of human cases. Vaccine. 1999 Mar 26;17(13-14):1742–9. doi: 10.1016/s0264-410x(98)00447-2. [DOI] [PubMed] [Google Scholar]
- [8].Plotkin SA. Rabies vaccine prepared in human cell cultures: progress and perspectives. Rev Infect Dis. 1980 May-Jun;2(3):433–48. doi: 10.1093/clinids/2.3.433. [DOI] [PubMed] [Google Scholar]
- [9].Thraenhart O, Kreuzfelder E, Hillebrandt M, Marcus I, Ramakrishnan K, Fu ZF, et al. Long-term humoral and cellular immunity after vaccination with cell culture rabies vaccines in man. Clin Immunol Immunopathol. 1994 Jun;71(3):287–92. doi: 10.1006/clin.1994.1088. [DOI] [PubMed] [Google Scholar]
- [10].McKenna PM, McGettigan JP, Pomerantz RJ, Dietzschold B, Schnell MJ. Recombinant rhabdoviruses as potential vaccines for HIV-1 and other diseases. Curr HIV Res. 2003 Apr;1(2):229–37. doi: 10.2174/1570162033485320. [DOI] [PubMed] [Google Scholar]
- [11].Schnell MJ, Foley HD, Siler CA, McGettigan JP, Dietzschold B, Pomerantz RJ. Recombinant rabies virus as potential live-viral vaccines for HIV-1. Proc Natl Acad Sci U S A. 2000 Mar 28;97(7):3544–9. doi: 10.1073/pnas.050589197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Siler CA, McGettigan JP, Dietzschold B, Herrine SK, Dubuisson J, Pomerantz RJ, et al. Live and killed rhabdovirus-based vectors as potential hepatitis C vaccines. Virology. 2002 Jan 5;292(1):24–34. doi: 10.1006/viro.2001.1212. [DOI] [PubMed] [Google Scholar]
- [13].Smith ME, Koser M, Xiao S, Siler C, McGettigan JP, Calkins C, et al. Rabies virus glycoprotein as a carrier for anthrax protective antigen. Virology. 2006 Sep 30;353(2):344–56. doi: 10.1016/j.virol.2006.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fehr T, Bachmann MF, Bucher E, Kalinke U, Di Padova FE, Lang AB, et al. Role of repetitive antigen patterns for induction of antibodies against antibodies. J Exp Med. 1997 May 19;185(10):1785–92. doi: 10.1084/jem.185.10.1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Jegerlehner A, Storni T, Lipowsky G, Schmid M, Pumpens P, Bachmann MF. Regulation of IgG antibody responses by epitope density and CD21-mediated costimulation. Eur J Immunol. 2002 Nov;32(11):3305–14. doi: 10.1002/1521-4141(200211)32:11<3305::AID-IMMU3305>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- [16].Hooper DC, Pierard I, Modelska A, Otvos L, Jr., Fu ZF, Koprowski H, et al. Rabies ribonucleocapsid as an oral immunogen and immunological enhancer. Proc Natl Acad Sci U S A. 1994 Nov 8;91(23):10908–12. doi: 10.1073/pnas.91.23.10908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Torii Y, Tokumaru Y, Kawaguchi S, Izumi N, Maruyama S, Mukamoto M, et al. Production and immunogenic efficacy of botulinum tetravalent (A, B, E, F) toxoid. Vaccine. 2002 Jun 7;20(19-20):2556–61. doi: 10.1016/s0264-410x(02)00157-3. [DOI] [PubMed] [Google Scholar]
- [18].Fiock MA, Devine LF, Gearinger NF, Duff JT, Wright GG, Kadull PJ. Studies on immunity to toxins of Clostridium botulinum. VIII. Immunological response of man to purified bivalent AB botulinum toxoid. J Immunol. 1962 Mar;88:277–83. [PubMed] [Google Scholar]
- [19].Fiock MA, Cardella MA, Gearinger NF. Studies on Immunity to Toxins of Clostridium Botulinum. Ix. Immunologic Response of Man to Purified Pentavalent Abcde Botulinum Toxiod. J Immunol. 1963 May;90:697–702. [PubMed] [Google Scholar]
- [20].Jones RG, Liu Y, Rigsby P, Sesardic D. An improved method for development of toxoid vaccines and antitoxins. J Immunol Methods. 2008 Aug 20;337(1):42–8. doi: 10.1016/j.jim.2008.05.009. [DOI] [PubMed] [Google Scholar]
- [21].Keller JE. Characterization of new formalin-detoxified botulinum neurotoxin toxoids. Clin Vaccine Immunol. 2008 Sep;15(9):1374–9. doi: 10.1128/CVI.00117-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Baldwin MR, Tepp WH, Pier CL, Bradshaw M, Ho M, Wilson BA, et al. Characterization of the antibody response to the receptor binding domain of botulinum neurotoxin serotypes A and E. Infect Immun. 2005 Oct;73(10):6998–7005. doi: 10.1128/IAI.73.10.6998-7005.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Baldwin MR, Tepp WH, Przedpelski A, Pier CL, Bradshaw M, Johnson EA, et al. Subunit vaccine against the seven serotypes of botulism. Infect Immun. 2008 Mar;76(3):1314–8. doi: 10.1128/IAI.01025-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Yu YZ, Li N, Zhu HQ, Wang RL, Du Y, Wang S, et al. The recombinant Hc subunit of Clostridium botulinum neurotoxin serotype A is an effective botulism vaccine candidate. Vaccine. 2009 May 11;27(21):2816–22. doi: 10.1016/j.vaccine.2009.02.091. [DOI] [PubMed] [Google Scholar]
- [25].Bennett AM, Perkins SD, Holley JL. DNA vaccination protects against botulinum neurotoxin type F. Vaccine. 2003 Jul 4;21(23):3110–7. doi: 10.1016/s0264-410x(03)00260-3. [DOI] [PubMed] [Google Scholar]
- [26].Jathoul AP, Holley JL, Garmory HS. Efficacy of DNA vaccines expressing the type F botulinum toxin Hc fragment using different promoters. Vaccine. 2004 Sep 28;22(29-30):3942–6. doi: 10.1016/j.vaccine.2004.04.006. [DOI] [PubMed] [Google Scholar]
- [27].Lee JS, Pushko P, Parker MD, Dertzbaugh MT, Smith LA, Smith JF. Candidate vaccine against botulinum neurotoxin serotype A derived from a Venezuelan equine encephalitis virus vector system. Infect Immun. 2001 Sep;69(9):5709–15. doi: 10.1128/IAI.69.9.5709-5715.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lee JS, Groebner JL, Hadjipanayis AG, Negley DL, Schmaljohn AL, Welkos SL, et al. Multiagent vaccines vectored by Venezuelan equine encephalitis virus replicon elicits immune responses to Marburg virus and protection against anthrax and botulinum neurotoxin in mice. Vaccine. 2006 Nov 17;24(47-48):6886–92. doi: 10.1016/j.vaccine.2006.06.004. [DOI] [PubMed] [Google Scholar]
- [29].Yu YZ, Zhang SM, Sun ZW, Wang S, Yu WY. Enhanced immune responses using plasmid DNA replicon vaccine encoding the Hc domain of Clostridium botulinum neurotoxin serotype A. Vaccine. 2007 Dec 17;25(52):8843–50. doi: 10.1016/j.vaccine.2007.10.016. [DOI] [PubMed] [Google Scholar]
- [30].Zeng M, Xu Q, Elias M, Pichichero ME, Simpson LL, Smith LA. Protective immunity against botulism provided by a single dose vaccination with an adenovirus-vectored vaccine. Vaccine. 2007 Oct 23;25(43):7540–8. doi: 10.1016/j.vaccine.2007.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Xu Q, Pichichero ME, Simpson LL, Elias M, Smith LA, Zeng M. An adenoviral vector-based mucosal vaccine is effective in protection against botulism. Gene Ther. 2009 Mar;16(3):367–75. doi: 10.1038/gt.2008.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Foynes S, Holley JL, Garmory HS, Titball RW, Fairweather NF. Vaccination against type F botulinum toxin using attenuated Salmonella enterica var Typhimurium strains expressing the BoNT/F H(C) fragment. Vaccine. 2003 Mar 7;21(11-12):1052–9. doi: 10.1016/s0264-410x(02)00622-9. [DOI] [PubMed] [Google Scholar]
- [33].Maksymowych AB, Simpson LL. Structural features of the botulinum neurotoxin molecule that govern binding and transcytosis across polarized human intestinal epithelial cells. J Pharmacol Exp Ther. 2004 Aug;310(2):633–41. doi: 10.1124/jpet.104.066845. [DOI] [PubMed] [Google Scholar]
- [34].McGettigan JP, Sarma S, Orenstein JM, Pomerantz RJ, Schnell MJ. Expression and immunogenicity of human immunodeficiency virus type 1 Gag expressed by a replication-competent rhabdovirus-based vaccine vector. J Virol. 2001 Sep;75(18):8724–32. doi: 10.1128/JVI.75.18.8724-8732.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Mebatsion T. Extensive attenuation of rabies virus by simultaneously modifying the dynein light chain binding site in the P protein and replacing Arg333 in the G protein. J Virol. 2001 Dec;75(23):11496–502. doi: 10.1128/JVI.75.23.11496-11502.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Foley HD, McGettigan JP, Siler CA, Dietzschold B, Schnell MJ. A recombinant rabies virus expressing vesicular stomatitis virus glycoprotein fails to protect against rabies virus infection. Proc Natl Acad Sci U S A. 2000 Dec 19;97(26):14680–5. doi: 10.1073/pnas.011510698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].DasGupta BR, Sathyamoorthy V. Purification and amino acid composition of type A botulinum neurotoxin. Toxicon. 1984;22(3):415–24. doi: 10.1016/0041-0101(84)90085-0. [DOI] [PubMed] [Google Scholar]
- [38].Sakaguchi G. Clostridium botulinum toxins. Pharmacol Ther. 1982;19(2):165–94. doi: 10.1016/0163-7258(82)90061-4. [DOI] [PubMed] [Google Scholar]
- [39].Simpson LL, Schmidt JJ, Middlebrook JL. Isolation and characterization of the Botulinum neurotoxins. Methods Enzymol. 1988;165:76–85. doi: 10.1016/s0076-6879(88)65015-4. [DOI] [PubMed] [Google Scholar]
- [40].Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970 Aug 15;227(5259):680–5. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- [41].Ravichandran E, Al-Saleem FH, Ancharski DM, Elias MD, Singh AK, Shamim M, et al. Trivalent vaccine against botulinum toxin serotypes A, B, and E that can be administered by the mucosal route. Infect Immun. 2007 Jun;75(6):3043–54. doi: 10.1128/IAI.01893-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Byrne MP, Smith LA. Development of vaccines for prevention of botulism. Biochimie. 2000 Sep-Oct;82(9-10):955–66. doi: 10.1016/s0300-9084(00)01173-1. [DOI] [PubMed] [Google Scholar]
- [43].Byrne MP, Smith TJ, Montgomery VA, Smith LA. Purification, potency, and efficacy of the botulinum neurotoxin type A binding domain from Pichia pastoris as a recombinant vaccine candidate. Infect Immun. 1998 Oct;66(10):4817–22. doi: 10.1128/iai.66.10.4817-4822.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Clayton MA, Clayton JM, Brown DR, Middlebrook JL. Protective vaccination with a recombinant fragment of Clostridium botulinum neurotoxin serotype A expressed from a synthetic gene in Escherichia coli. Infect Immun. 1995 Jul;63(7):2738–42. doi: 10.1128/iai.63.7.2738-2742.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Zinkernagel RM. On natural and artificial vaccinations. Annu Rev Immunol. 2003;21:515–46. doi: 10.1146/annurev.immunol.21.120601.141045. [DOI] [PubMed] [Google Scholar]
- [46].Baumgarth N. A two-phase model of B-cell activation. Immunol Rev. 2000 Aug;176:171–80. doi: 10.1034/j.1600-065x.2000.00606.x. [DOI] [PubMed] [Google Scholar]
- [47].LaPenotiere HF, Clayton MA, Middlebrook JL. Expression of a large, nontoxic fragment of botulinum neurotoxin serotype A and its use as an immunogen. Toxicon. 1995 Oct;33(10):1383–6. doi: 10.1016/0041-0101(95)00072-t. [DOI] [PubMed] [Google Scholar]
- [48].Wunner WH. The chemical composition and molecular structure of rabies viruses. In: Baer GM, editor. The natural history of rabies. Elsevier/Academic Press; Amsterdam ; Boston: 1991. pp. 31–67. [Google Scholar]
- [49].Atassi MZ, Oshima M. Structure, activity, and immune (T and B cell) recognition of botulinum neurotoxins. Crit Rev Immunol. 1999;19(3):219–60. [PubMed] [Google Scholar]
- [50].Chen F, Kuziemko GM, Amersdorfer P, Wong C, Marks JD, Stevens RC. Antibody mapping to domains of botulinum neurotoxin serotype A in the complexed and uncomplexed forms. Infect Immun. 1997 May;65(5):1626–30. doi: 10.1128/iai.65.5.1626-1630.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Oshima M, Hayakari M, Middlebrook JL, Atassi MZ. Immune recognition of botulinum neurotoxin type A: regions recognized by T cells and antibodies against the protective H(C) fragment (residues 855-1296) of the toxin. Mol Immunol. 1997 Oct;34(14):1031–40. doi: 10.1016/s0161-5890(97)00107-7. [DOI] [PubMed] [Google Scholar]