Abstract
Background
The risk for cardiovascular events is higher for those with metabolic syndrome (MetS), and it is known that firefighters have a fourfold risk for cardiovascular events. The purpose of this study was to quantify MetS prevalence and evaluate the effect of a low glycemic nutritional fitness program on the reduction of MetS risk factors among firefighters.
Methods
Professional firefighters were screened for MetS then enrolled in a low glycemic nutritional fitness program for a 12-week period. Anthropometric and physiologic measurements were obtained at the start and end of the program. Subjects with ≥3 of the following were positive for MetS: waist ≥40 (men) or ≥35 inches (women), BP≥135 (systole) or ≥85 (diastole) mmHg, fasting blood sugar ≥100mg/dl, triglycerides ≥150mg/dl, and high-density lipoproteins <40 (men) or <50 mg/dl (women). Weekly training was provided with low glycemic nutrition and regular fitness and evaluation of individual progress.
Results
Seventy-five firefighters (age 42+8yrs, mostly Caucasian men) had a total MetS prevalence of 46.7% (p<0.05 vs normal population). One platoon (10 men, age 48±5yrs) was enrolled in the 12-week program. Most (7/10) had MetS at the baseline, but this prevalence decreased significantly after 12 weeks to 3 subjects (p=0.02). On average, subjects had 3.2±1.6 vs 1.9±1.7 MetS risk factors (p<0.01) at baseline and 12 week interval, respectively.
Conclusions
The prevalence of MetS and MetS risk factors are higher among professional firefighters compared to general population. A short-duration low glycemic fitness program can successfully improve anthropometric and physiologic measures and reduce the prevalence of MetS.
Keywords: metabolic syndrome, low glycemic, firefighters
Introduction
The prevalence of obesity and type 2 diabetes has resulted in a global pandemic of Metabolic Syndrome (MetS) or Insulin Resistance Syndrome. MetS encompasses a primary disturbance in adipose tissue resulting in the defined triad of obesity, dyslipidemia, and insulin resistance. Genetic predisposition, decreased physical activity, and a diet low in fiber and high in saturated fats lead to increased visceral adiposity; resulting in increased waist circumference, decreased serum high-density lipoprotein (HDL), increased serum triglyceride (TG), hypertension (HTN), and elevated fasting blood sugar (FBS)1–3. MetS has been estimated to affect as many as 34% of US population 4. Yet, ironically, there is a consensus that the medical disorders included in the definition of MetS are all modifiable.
The Adult Treatment Panel III of the National Cholesterol Education Program established guidelines for pharmacologically treating cholesterol levels 5. Importantly, the report also states that therapeutic lifestyle changes remain an essential modality in the clinical management of patients with MetS. Moreover, any person at high risk or moderately high risk for cardiovascular disease who has lifestyle risk factors including MetS is a candidate for lifestyle changes to decrease his/her risk factors regardless of cholesterol level. Therefore, despite the success with cholesterol lowering drugs, lifestyle change for cardiovascular disease reduction remains important. Importantly, the risk for major cardiovascular events is approximately twice as high for those with the MetS than for those without the syndrome 5. Accordingly, it is feasible to identify the syndrome and implement therapeutic lifestyle changes with the benefits of reducing the high risk of cardiovascular events.
Increased physical activity and healthy dietary interventions are considered the first-line intervention for treating MetS; in fact, using medications alone has shown less desirable outcomes. Whereas physical activity can lower the risk for developing type 2 diabetes and subsequent MetS by 58%, importantly, dietary interventions can independently affect the metabolism and reduce the risk for developing MetS 2. Two diets have been shown effective in treating MetS: the Mediterranean diet and DASH (dietary approach to stop hypertension) diet. Both focus on increasing daily servings of fruits and vegetables (4–5 servings), decreasing carbohydrates (7–8 servings), and minimizing fats, sugars, and alcohol; this is compared to 1–2 servings of fruits and vegetables, 10–12 servings of carbohydrates, 5 servings of fats, and 1–2 servings of sugars in the typical Western diet 2.
Apart from lifestyle and other risk factors, certain populations are at increased risk for MetS and subsequent cardiovascular comorbidities. Firefighters, working in a physically and emotionally stressful environment that increases cardiovascular loads, are at risk for cardiovascular morbidity and mortality, which accounts for 45% of on-duty deaths 6. Compared to normal population, firefighters have a fourfold risk for developing cardiovascular events. Approximately 20% of career firefigters have HTN, most (75%) are overweight, 34% have low HDL, 24% have high TG, and 5% have diabetes, resulting in a higher prevalence of MetS risk factors compared to the normal population 7,8. Thus, the purpose of this study was to quantify MetS prevalence and evaluate the effect of a 12-week low glycemic nutritional fitness program on the reduction of MetS risk factors among a sample cohort of professional firefighters.
Methods
Firefighters for this prospective, longitudinal, quasi-experimental study were recruited from the parent study, SAFFE Study (Surveying & Assessing Firefighter Fitness & Electrocardiogram, 2008–2010). The SAFFE study is an ongoing National Institute of Health (NIH)-sponsored descriptive study identifying and quantifying cardiovascular risks in firefighters. With approval from the Institutional Review Board at the University at Buffalo, professional firefighters from the Buffalo, New York Fire Department were recruited to determine the prevalence of MetS. Then one platoon from a single firehouse was randomly selected to evaluate the effectiveness of the low glycemic nutritional fitness program. The fire department uses a platoon-duty shift schedule and works as a team with members the same platoon at the same fire house for the entire shift. They are relieved as a group the next scheduled Platoon. Platoons work 4 consecutive days, specifically 2 day shifts from, 0800–1700 followed by 2 night shifts, 1700–0800; then they are off duty for 3 days.
Protocol
After obtaining written consent and in the privacy of the bunk room, anthropometric and physiologic measurements of all participating firefighters were taken to quantify the prevalence of metabolic syndrome. Then within a small cohort (one platoon), firefighters were recruited to participate in the 12 week program.
Specifically, a 12-week low-glycemic nutritional fitness program that consists of diet and physical exercise (Wellness Works WNY, Buffalo, New York) was implemented. The program was delivered during 2-hour weekly sessions by a trained team that consisted of a physician, nurse, and a certified exercise instructor (Table 1). All instruction occurred at the firehouse while the firefighters were on duty. For example, didactic instruction took place on the apparatus floor with the firefighters sitting in a circle around the training team. If the weather was amenable, exercise classes including yoga were conducted outside on the firehouse lawn. Subjects kept a daily nutritional and fitness diary that was reviewed by the training team on a weekly basis. Feedback and instructions were given on an individual basis for every firefighter based on progress and physical measures.
Table 1.
12-Week Low-Glycemic Nutritional Fitness Program
| Component | Time frame | Description |
|---|---|---|
| Diet and Nutrition | ||
| Meal planning | W1 | Breakfast was replaced by a meal replacement (nutritional shake) throughout the program, as well as educating subjects about a variety of food topics, and supervised selection of healthy foods. |
| Healthy eating | W2, W10 | |
| Meal replacement | W1 to W12 | |
| Meal education | W3 to W9 | |
| Supervised Exercise | ||
| Workout clearance | W1 | Subjects went through a scheduled program of various sessions for target-specific trainings. Basic instruction about stretching, exercise intensity, and heart rate targeting were given. |
| Exercise education | W2 | |
| Weight training | W3 | |
| Cardiac exercise | W4 | |
| Resistance training | W5 | |
| Muscle balance | W6 | |
| Fat burning | W9 | |
| Life-style training | ||
| Activity | W8 | Subjects encouraged to complete 60–90 min of daily mild-to-moderate activity. Pedometers were given to encourage walking and subjects completed a diary of daily consumption and weekly weight. |
| Eating Out | W10 | |
| Yoga | W1 to W12 | |
| Self evaluation | W1 to W12 | |
Diet and Nutrition
The low glycemic diet was based on Mediterranean and DASH diet recommendations; it consisted of 50% vegetables and fruits, 30% proteins, and 20% carbohydrates out of total daily consumption. Food lists that showed specific foods with low, moderate, or high glycemic indexes were given to subjects. The approach focused on minimizing fats and sugars and increasing healthy selections of foods, including the addition of fibers and omega-3 fatty acids. In addition, the firefighters were supplied with daily multivitamins and omega-3 for the period of 12 weeks. The meal structure was three daily meals and two snacks: breakfast, snack, lunch, snack, and dinner. A meal replacement strategy was implemented: breakfast and one snack were replaced throughout the program with low glycemic shakes and snack bars (USANA Health Science, Utah). Educational instruction and literature were given on a variety of topics including: glycemic index, food labels, and handouts about carbohydrates, proteins, vegetables, fat, fiber, spices, herbs, vitamins, and antioxidants.
Exercise and Physical Activity
After being cleared for physical exercise by a trained physician, firefighters enrolled in a scheduled and supervised training regimen that targeted five categories: 1) stretching/flexibility exercise (e.g., Yoga); 2) resistance/strength training (e.g., free weights); 3) cardiovascular conditioning (e.g., jogging, cycling, brisk walking) with a target heart rate (THR) falling between 50%–60% of maximum heart rate (MHR, 220-age); 4) fat burning training (THR 60%–70%); and 5) endurance training (THR 70%–80%). Subjects were encouraged to participate in daily mild-to-moderate activity for 60 to 90 minutes along with acquiring 10,000 steps measured by Step Counter Pedometer (Gilroy, CA) that was provided for each firefighter. Subjects kept a record of daily activity and weekly weight changes using a bathroom scale in the firehouse provided by the training team.
Anthropometric and Physiologic Measurement
Blood chemistry was obtained using point-of-care testing allowing direct diagnostic testing at the firehouse using portable handheld devices. The sensitivity and specificity of cholesterol and triglyceride results using these devices are reported to be 98% and 94%, respectively 9. Thus, point-of-care testing results is nearly equivalent to those obtained by laboratories. This is not to say that point-of-care testing measurements replace lipid determinations by professional laboratories, but rather that they represent a viable and convenient low-cost alternative for field testing, which avoids the transportation and storage of biologic material.
All measurements were obtained at the beginning (T0, time zero) for all participating firefighters. For those who were enrolled in the 12-week program, measures were repeated at 6-week (T1, time one) and 12-week (T2, time two) intervals after starting the intervention, then again at 6 months after completing the intervention (T3, time 3). All anthropometric and physiologic measurements were obtained by the same exercise instructor for all subjects at all time intervals.
Anthropometric measurements included height, weight, body mass index (BMI), sagittal abdominal height, body fat percentage, blood pressure, and neck, chest, upper arm, waist, hip, and thigh circumferences.
Blood pressure was taken manually in a sitting resting position averaging 2 readings with 5-minute intervals between readings.
Using a handheld photometer that measures the concentration of glucose, cholesterol, and triglycerides (CardioChek® PA Analyzer, Polymer Technology System Inc, Newark, DE), a drop of fresh capillary blood (10 μL) was applied directly to the test strip. This battery-operated meter was easy to use and operator independent, results were available within a minute for glucose, 2 minutes for triglyceride, and 3 minutes for cholesterol. The handling procedure is the same as those used with most blood glucose meters, so certain precautions were taken. To avoid contamination with glycerol found in hand lotions and soaps, the firefighter’s hands were washed with warm water before obtaining the drop of blood. Anecdotally, the point-of-care testing was well received by the firefighters because they were spared venipuncture (only a drop of blood is required) and results were immediately available without the typical laboratory delays.
MetS Criteria
Five major different criteria for the diagnosis of MetS currently exist 2,10–13. These criteria share five major measures: abdominal obesity, hypertension, insulin resistance, low HDL cholesterol, and hypertriglyceridemia. For the purpose of the current study, the NIH criteria 4 were used to define MetS (at least 3 need to be met): 1) waist circumference ≥ 40 (men) or 35 (women) inches, 2) blood pressure ≥135 (systole) or ≥85 (diastole) mmHg, 3) HDL < 40 (men) or 50 (women) mg/dl, 4) serum TG ≥150 mg/dl, or 5) FBS ≥100 mg/dl.
Data Analysis
All values were reported as mean ± standard deviation. To test the difference of proportions among four match sets (T0, T1, T2, and T3) or to compare firefighters (T0) to the general population, repeated measures ANOVA and confidence interval calculation for testing for proportion differences were used. All statistical analyses were done using Statistical Package of Social Sciences (SPSS 16.0 for Windows); p<0.05 was considered statistically significant.
Results
Seventy-five professional firefighters (age 42+7.5 years, 95% males, 62% Caucasian, 28% African American, and 10% Hispanic) were enrolled from 6 different firehouses. The sample’s demographics were similar to that of the Fire Department (age 38±12 years, 97% men, 67% Caucasian, 26% African American, and 7% Hispanic). On average, each firefighter had 2.3±1.4 risk factors, with a total MetS prevalence of 46.7%. The prevalence of MetS and most of the MetS risk factors were significantly higher in firefighters when compared to the normal population (Table 2). Firefighters in this study had more hypertension, insulin resistance, low HDL cholesterol, and higher MetS rates. Specifically, the prevalence of MetS was significantly influenced by age: those older than 50 years had the highest prevalence. Whereas gender did not significantly influence the prevalence and most of risk factors, men had significantly higher blood pressure (133/86 mmHg) than women (113/74 mmHg), p<0.05. Moreover, Caucasians had the highest prevalence of MetS, though the number of risk factors per subject was similar across the sample.
Table 2.
Prevalence of MetS Risk Factors in Firefighters as Compared to General Population 1 (age adjusted)
| n | Abdominal obesity (%) | Hyper-triglyceridemia (%) | Low HDL cholesterol (%) | High blood pressure (%) | High fasting blood sugar (%) | Number of risk factors | Prevalence of MetS (%) | |
|---|---|---|---|---|---|---|---|---|
|
Overall prevalence | ||||||||
| Firefighters | 75 | 48.0 | 29.3 | 52.0* | 53.3* | 52.0* | 2.3±1.4 | 46.7* |
| General pop. | 3423 | 48.0 | 31.2 | 24.7 | 39.5 | 38.6 | - | 34.0 |
|
Prevalence by race | ||||||||
| Caucasian | 52 | 53.8 | 34.6 | 50.0 | 51.9 | 55.8 | 2.5±0.2 | 51.9 |
| African American | 17 | 41.2 | 17.6 | 52.9 | 47.1 | 47.1 | 2.1±0.4 | 29.4 |
| Hispanic | 6 | 16.7 | 16.7 | 66.7 | 83.3 | 33.3 | 2.2±0.5 | 33.3 |
|
Prevalence by gender | ||||||||
| Male | 71 | 47.9 | 28.2 | 52.1 | 57.1 | 52.1 | 2.4±0.2 | 43.7 |
| Female | 4 | 50.0 | 50.0 | 50.0 | 0 | 50.0 | 2.0±0.9 | 50.0 |
p<0.05 vs general population using test for proportion difference.
To evaluate the effectiveness of the 12-week low glycemic fitness program, 10 firefighters from the same platoon volunteered (age 48±5 years); among those 1 firefighter had previous history of cardiovascular disease, whereas 5 had a family history of either cardiovascular disease or diabetes. In addition, 2 were current smokers, 8 were mild-to-moderate alcohol consumers, and nearly all (9/10) were at least overweight. On average, each subject had 3.2±1.6 MetS risk factors at the beginning of the study (T0) with a prevalence of 70%. At the end of the study (T2), both the number of risk factors per subject (1.9±1.7) and prevalence (3/10) decreased significantly, p< 0.05. Subjects showed a statistically significant (p<0.05) reduction in weight, BMI, waist, hip, and neck circumferences, sagittal abdominal height, body fat, blood pressure, and FBS (Table 3). Of note, many of the firefighters had the most improvement in their cardiovascular risk factors at the 6-week measurement (T1). After 6 months of completing the intervention (T3), firefighters maintained the desired reduction in waist and hip circumferences, body fat percent, blood pressure, and TG. Even though firefighters had undesired re-elevation in incidence of MetS risk factors during follow-up, most of these values were still significantly lower than that of the baseline (Figure 1).
Table 3.
Physiologic and Anthropometric Measurements
| Measure | Baseline (T0) | 6 weeks (T1) | 12 weeks (T2) | 6 months (T3) |
|---|---|---|---|---|
| Weight (lbs) | 213.8±29.9 | 206.2±25.8* | 204.2±25.9* | 211.5±29.3† |
| Body Mass Index (kg/m2) | 29.9±4.3 | 28.8±3.7* | 28.5±3.7* | 29.0±3.8† |
| Waist circumference (inches) | 40.9±4.5 | 39.6±4.5* | 38.5±4.1* | 39.3±5.2* |
| Chest circumference (inches) | 42.7±3.3 | 42.8±2.9 | 41.9±2.5 | 41.5 ± 3.6 |
| Neck circumference (inches) | 16.8±1.1 | 16.3±1* | 16.0±1* | 16.8 ± 1† |
| Upper arm circumference (inches) | 13.3±1.1 | 13.4±1 | 13.0±0.7 | 14.0 ± 1.1† |
| Hip circumference (inches) | 42.9±2.5 | 41.7±2.6* | 41.4±2.2* | 39.4 ± 3.3*† |
| Thigh circumference (inches) | 21.5±2.2 | 21.1±1.7 | 21.0±1.7 | 21.0 ± 1.8 |
| Abdominal height (cm) | 23.7±3.1 | 22.7±2.4* | 22.4±2.4* | 24.1 ± 3.5† |
| Body fat (%) | 32.3±9.5 | 30.0±7.8* | 27.1±10.7* | 23.5 ± 7.6*† |
| Systolic blood pressure (mmHg) | 138.8±18.8 | 125.4±12.5* | 128.0±12.5* | 128.1±11.9* |
| Diastolic blood pressure (mmHg) | 88.2±10 | 79.6±12* | 82.4±6.8* | 83.1±4.4 |
| Fasting blood sugar (mg/dl) | 119±14.5 | 104±6.1* | 97.2±9.2* | 103.0±7.9*† |
| HDL (mg/dl) | 41.1±16.8 | 45.9±20.5 | 46.2±21.7 | 36.3±15.3*† |
| TG (mg/dl) | 154.8±85.9 | 81.5±40.9* | 96.2±60.2 | 88.9±30.2* |
| Number of risk factors per subject | 3.2±1.6 | 2.1±1.5* | 1.9±1.7* | 2.6±1.2† |
p < 0.05 vs T0 &
p < 0.05 vs T2, using repeated measures ANOVA.
TG, triglyceride, HDL, high-density lipoprotein.
Figure 1. Incidence of Metabolic Syndrome risk factors before, during, and after the 12-week program.
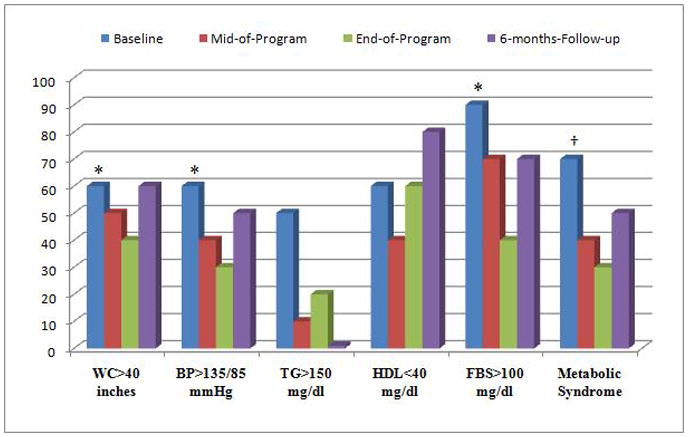
Significant reductions (p<0.05) in central obesity, hypertension, insulin resistance, and MetS prevalence were observed during the 12-week program using repeated-measures ANOVA (*) and test for proportion difference (†). This reduction was not maintained after 6 months follow-up. WC, waist circumference, BP, blood pressure, TG, triglyceride, HDL, high-density lipoprotein, FBS, fasting blood sugar.
Discussion
This study revealed that firefighters have higher prevalence of MetS and MetS risk factors than the general population. A12-week low glycemic nutritional fitness program decreased significantly the prevalence of MetS risk factors and had a positive effect on most of anthropometric and physiologic measurements. There were significant reductions in weight (9.7 lbs), BMI (0.8 kg/m2), waist (2.4 inches), neck (0.8 cm), and hip circumferences (1.5 inches), abdominal height (1.3 cm), body fat (5.2%), systolic BP (10.8 mmHg), diastolic BP (5.8 mmHg), and FBS (21.8 mg/dl). This reduction in MetS and cardiovascular risk factors may be a key in reducing the risk of cardiovascular morbidity and mortality among firefighters.
In the general population, men tend to have higher prevalence of MetS, higher blood pressure, higher fasting blood sugar, and higher hypertriglyceridemia, and women tend to have more abdominal obesity and lower HDL 4. In the current study, men and women were equal in the prevalence of MetS and most MetS risk factors. No inferential statistics were done to compare the differences within the sample due to the small sample size (women n=4). However, the prevalence based on race had the same trend as found in the normal population (highest in Caucasians, followed by Hispanics, followed by African Americans). The highest prevalence of all MetS risk factors was among middle aged Caucasian men, therefore the 12-week program was logically evaluated in a platoon that was purposefully selected and composed of 10 white men aged 48±5 years. Interestingly, the 12-week program reduced the prevalence of MetS by 57% among firefighters, which is consistent with findings from the Diabetes Prevention Program 14 which shows that increased physical activity can reduce the prevalence of type 2 diabetes by 58%. Keeping in mind that MetS resembles an insulin resistance syndrome, this strongly suggests that the fitness program in this study was equivalently successful. Additionally, evidence (Level A recommendation) suggests that omega-3 supplements and high-fiber diets have a desirable effect in treating MetS by altering fats metabolism and resulting in decreased central obesity, insulin resistance, hypertension, triglycerides and improving HDL 2. Firefighters in this study achieved similar desirable reduction in these risk factors, suggesting that the low glycemic dietary plan was successful as well.
It merits mentioning a strength of the study design was optimizing the group effect within a platoon of firefighters because the beneficial effects of cohesion on health and well-being are well recognized. With a cohort of firefighters it is fair to assume that the department, and especially platoons who work and sleep together, result in social cohesion. Importantly, this was not unique to the study or manipulated by design but rather naturally occurring. Future research, with other populations, should design approaches to optimize the benefits of social cohesion.
Finally, as proven in the current study, an approach to target life-style modifications through healthy diet and physical activity can reduced the prevalence of MetS and subsequent health hazards, however maintenance and consistency remain a key factor for a successful intervention. Firefighters in this cohort were successful in reducing MetS and most MetS risk factors during the supervised 12-week program, and most of this improvement was maintained after 6 months of completing the intervention as compared to the baseline; but the desired outcomes achieved during the program (T2) were gradually fading. It appears that the education and awareness gained during the 12-week program were not enough to maintain the desired effects of the intervention; this means that a strategy that focuses on incorporating the current program with the mandatory annual physical exams and follow up of firefighters will result in the dual reward of early prevention and management of MetS and MetS risk factors, and the reduction of high rates of cardiovascular morbidity and mortality among firefighters.
Limitations
A high prevalence of MetS (46.7%, n=75) was found in this study, much higher than in the normal population (34%, n=3423) 4 and what has been previously defined in firefighters (15%–19%, n=214–1417) 15, 16. Because firefighters tend to be physically fit and active, this discrepancy might be explained by the samll sample size in the current study as well as geographically: it is known that New York State, particularly Erie and Niagara counties, has a higher prevelance of obesity and cardiovascular risk factors compared to the rest of the nation 17. Another limitation was that a small cohort of firefighters (n=10) completed the 12-week program, which could have resulted in lower power to detect significant changes in MetS risk factors during different comparisons. A larger experimental study is needed to evaluate beneficial strategies to reduce cardiovascular risk factors among firefighters and to be incorporated in their occupational and daily life-styles.
Conclusion
MetS is a combination of medical disorders including visceral obesity, dyslipidemia, hyperglycemia, and hypertension. Although theories exist, the etiology of MetS remains debatable. Therapy targeting obesity and body fat distribution through first-line weight loss and physical activity is recommended, and additional dietary interventions have shown desirable outcomes for managing MetS. Firefighters are at increased risk for MetS and subsequent cardiovascular morbidity; a 12-week low-glycemic nutritional fitness program that consists of diet and physical exercise focusing on modifying firefighters’ social and behavioral practices can successfully improve anthropometric and physiologic measures and reduce the prevalence of MetS in firefighters. Strategies to focus on maintenance and consistency of new life-style changes are key factors in achieving long-term desired outcomes.
Acknowledgments
Supported by Grants from National Institute of Health (R21 NR-011077), the School of Nursing, Garman Funds, and MGC was a participant in the 2010 National League for Nursing (NLN) Scholarly Writing Retreat, sponsored by the NLN Foundation for Nursing Educations
References
- 1.Grundy SM, Cleeman JI, Bairey Merz CN, et al. Implications of Recent Clinical Trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Journal of the American College of Cardiology. 2004;44(3):720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Potenza MV, Mechanick JI. The Metabolic Syndrome: Definition, Global Impact, and Pathophysiology. Nutrition in Clinical Practice. 2009;24(5):560–577. doi: 10.1177/0884533609342436. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel on Detection E, Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Ervin R. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Hyattsville, MD: U.S. Department of Health and Human Services, Division of Health and Nutrition Examination Surveys, Centers for Disease Control and Prevention, National Center for Health Statistics; 2009. [PubMed] [Google Scholar]
- 5.Grundy, Cleeman JI, Merz CNB, et al. Implications of Recent Clinical Trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110(2):227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 6.Kales SN, Tsismenakis AJ, Zhang C, Soteriades ES. Blood Pressure in Firefighters, Police Officers, and Other Emergency Responders. American Journal of Hypertension. 2008;22(1):11–20. doi: 10.1038/ajh.2008.296. [DOI] [PubMed] [Google Scholar]
- 7.Kuorinka I, Korhonen O. Firefighters’ reaction to alarm, an ECG and heart rate study. J Occup Med. 1981;23(11):762–766. doi: 10.1097/00043764-198111000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Byczek L, Walton SM, Conrad KM, Reichelt PA, Samo DG. Cardiovascular risks in firefighters: implications for occupational health nurse practice. AAOHN J. 2004;52(2):66–76. [PubMed] [Google Scholar]
- 9.Stefano R, Cristina B, Camilla T, Valentina S, Pietro Amedeo M. Point-of-care testing of cholesterol and triglycerides for epidemiologic studies: evaluation of the multicare-in system. Translational research: the journal of laboratory and clinical medicine. 2009;153(2):71–76. doi: 10.1016/j.trsl.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C for the Conference Participants. Definition of Metabolic Syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Arteriosclerosis, Thrombosis, and Vascular Biology. 2004;24(2):e13–18. doi: 10.1161/01.ATV.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 11.Alberti, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 12.Alberti Zimmet P, Shaw J, Grundy S Federation ID. The IDF consensus worldwide definition of the metabolic syndrome. IDF Communications; 2006. [Google Scholar]
- 13.Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 14.Knowler WC, Barrett-Connor E, SEF Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donovan R, Nelson T, Peel J, Lipsey T, Voyles W, Israel R. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med (Lond) 2009;59(7):487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- 16.Title LM, Lonn E, Charbonneau F, et al. Relationship between brachial artery flow-mediated dilatation, hyperemic shear stress, and the metabolic syndrome. Vascular Medicine. 2008;13(4):263–270. doi: 10.1177/1358863X08095154. [DOI] [PubMed] [Google Scholar]
- 17.New York State Department of Health BoCDEaS. The Burden of Cardiovascular Disease in New York: Mortality, Prevalence, Risk Factors, Costs & Selected Populations. 2000. [Google Scholar]


