Abstract
CD4+CD25+ regulatory T (Treg) cells suppress naive T cell responses, prevent autoimmunity, and delay allograft rejection. It is not known, however, whether Treg cells suppress allograft rejection mediated by memory T cells, as the latter mount faster and stronger immune responses than their naive counterparts. Here we show that antigen-induced, but not naive, Treg cells suppress allograft rejection mediated by memory CD8+ T cells. Suppression was allospecific, as Treg cells induced by third-party antigens did not delay allograft rejection. In vivo and in vitro analyses revealed that the apoptosis of allospecific memory CD8+ T cells is significantly increased in the presence of antigen-induced Treg cells, while their proliferation remains unaffected. Importantly, neither suppression of allograft rejection nor enhanced apoptosis of memory CD8+ T cells was observed when Treg cells lacked CD30 or when CD30 ligand–CD30 interaction was blocked with anti–CD30 ligand Ab. This study therefore provides direct evidence that pathogenic memory T cells are amenable to suppression in an antigen-specific manner and identifies CD30 as a molecule that is critical for the regulation of memory T cell responses.
Introduction
Thymus-derived CD4+CD25+ regulatory T (Treg) cells play a key role in the maintenance of immunologic tolerance to both self- and foreign antigens by suppressing aggressive T cell responses (1). Treg cells represent a small fraction (5–10%) of CD4+ T cells and constitutively express the α chain of the IL-2 receptor (CD25) (2), the CTL-associated antigen-4 (CTLA4) (3), and the transcription factor Foxp3 (4). Depletion of Treg cells in normal mice leads to autoimmune disease (2), while the induction of endogenous Treg cells or the adoptive transfer of exogenous Treg cells prevents autoimmunity and allograft rejection in several animal models (5–10). Although Treg cells suppress naive T cell responses in vitro and in vivo (1, 8, 11), it is not known whether they suppress allograft rejection mediated by memory T cells, given that memory T cells respond more vigorously and under less stringent conditions to foreign antigens than do their naive counterparts. Addressing this question is of clinical import, since memory T cells contribute to disease pathogenesis in autoimmunity and transplantation and interfere with the induction of immunologic tolerance (12).
The mechanisms responsible for Treg cell–mediated inhibition of the immune response remain to be defined, despite evidence that cell-cell contact, competition for growth factors, and the production of cytokines such as IL-4, IL-10, and TGF-β may mediate suppression (6, 13–17). In particular, little is known about the costimulatory pathways required for Treg cells to acquire their suppressive function upon encountering antigen. Previous studies have demonstrated that activation through the T cell receptor (TCR) is required for Treg cells to become suppressive (18), but that CD28/B7, OX40/OX40L, and 4-1BB/4-1BBL costimulatory interactions are not critical (3, 19). In addition, the role of CTLA4 signaling in Treg cell suppressor function remains controversial (1). CD30, a member of the TNF receptor (TNFR) superfamily, is expressed on activated T and B lymphocytes and certain Treg cell populations (20–22). The ligand for CD30 (CD30L, or CD153) is expressed on activated T cells, neutrophils, eosinophils, and resting B cells (20). Although earlier in vitro studies have shown that the engagement of CD30 by its ligand provides costimulatory signals to activated T cells and enhances cytokine production and secondary proliferative responses (21), the in vivo role of CD30 remains unclear. For example, CD30-deficient (CD30–/–) mice have a normal number and phenotype of mature T cells in the periphery and lack obvious immunologic abnormalities (23). Recent studies suggest that CD30+ T cells, present at sites of inflammation in autoimmune diseases such as rheumatoid arthritis, may serve a regulatory role (24). However, direct evidence that CD30 is required for or contributes to immune regulation is lacking.
In this study, we set out to investigate whether CD4+CD25+ Treg cells are capable of suppressing memory responses in a murine transplantation model. We found that antigen-induced, but not naive, Treg cells suppress allograft rejection mediated by memory CD8+ T cells in an antigen-specific manner. Suppression was associated with increased apoptosis of allospecific memory CD8+ T cells in the graft and was largely dependent on the presence of CD30 on Treg cells. These findings define what we believe to be a novel role for CD30 in regulating immune responses and highlight the role of Treg cells in suppressing memory T cell recall.
Methods
Mice.
C57BL/6 (B6) mice homozygous for the mutation that leads to alymphoplasia (aly) were purchased from CLEA Japan Inc. (Osaka, Japan) (25). 2C TCR-transgenic B6 mice on a recombination-activating gene-2 knockout (Rag2–/–) background (2C.Rag–/–) were generated by backcrossing of 2C transgenic mice onto Rag2–/– mice (The Jackson Laboratory, Bar Harbor, Maine, USA). The CD30–/– B6 mouse colony was a gift from Tak Mak (University of Toronto, Toronto, Ontario, Canada). WT BALB/c mice, WT C3H/HeJ mice, and WT B6 mice were purchased from The Jackson Laboratory. All mice were housed in a specific pathogen–free environment, and animal protocols were approved by Yale University Institutional Animal Care and Use Committee.
Mouse surgery.
Skin and cardiac donors were 6- to 8-week-old BALB/c (H-2d) mice, and allograft recipients were 6- to 8-week-old splenectomized aly B6 mice or WT B6 mice (H-2b). Splenectomy was performed 2 weeks before transplantation. Fully vascularized heterotopic heart transplantation was performed as described (26). Cardiac-allograft rejection was defined as cessation of palpable cardiac contractions. Full-thickness trunk skin was transplanted to the dorsal flank area of recipient mice. Skin rejection was defined as graft necrosis greater than 90%.
Treg and memory T cell preparation and phenotyping.
To induce antigen-specific Treg cells, WT or CD30–/– B6 mice were treated with donor-specific splenocyte transfusion (DST) using irradiated BALB/c spleen cells, treated with third-party splenocyte transfusion (TPT) using irradiated C3H/HeJ spleen cells, or left noninjected. Four weeks later, spleen cells were pooled and enriched for CD4+ T cells by positive selection on a magnetic cell separator (autoMACS; Miltenyi Biotec Inc., Auburn, California, USA). Cells were then stained with anti-CD4–phycoerythrin (anti-CD4–PE) and anti-CD25–FITC Ab’s, and CD4+CD25+ Treg cells were sorted using a FACSVantage (BD Biosciences, Mountain View, California, USA). The purity of CD4+CD25+ cells was greater than 95%. For Treg phenotyping, cells stained with anti-CD4–PE and anti-CD25–FITC Ab’s were further labeled with anti-CD30–biotin or anti-CTLA4–biotin Ab’s followed by streptavidin–peridinin chlorophyll-a protein (streptavidin-PerCP), or labeled with anti-CD62L–allophycocyanin or anti-CD45RB–biotin Ab’s followed by streptavidin-allophycocyanin (all Ab’s were from Pharmingen, San Diego, California, USA).
Memory CD8+ T cells were purified from WT, CD30–/–, or transgenic 2C.Rag–/– mice 10 weeks after DST or TPT (1 × 107 cells per mouse) by autoMACS and FACSVantage. Briefly, CD8+ T cells were first isolated from spleen cells by autoMACS using positive selection. Cells were then incubated with anti-CD8–PE and anti-CD44–FITC Ab’s (Pharmingen) and were sorted by the FACS after gating of the CD8+CD44high population. The purity of these cells was typically greater than 95% for WT cells, and greater than 94% for 2C cells. The memory phenotype was further confirmed by staining with anti-CD62L–APC and anti-CD25–APC (Pharmingen).
Ab treatment of mice.
To block CD28/B7 and CD40/CD40L costimulation and therefore suppress the primary alloimmune response, WT mice were injected intraperitoneally with both CTLA4-Ig (0.5 mg on day 2) and MR1 (0.25 mg on days 0, 2, 4, and 6) after transplantation. Both agents were provided by Christian Larsen (Emory University, Atlanta, Georgia, USA). To block CD30/CD30L interaction, mice were injected intraperitoneally with anti-CD30L blocking Ab (Pharmingen) or isotype control Ab (rat IgG2b) (0.1 mg on days 0, 2, 4, and 6 after transplantation).
Isolation of graft-infiltrating cells.
Graft-infiltrating cells were isolated as described previously (27). Briefly, transplanted mice were sacrificed, and cardiac allografts were perfused in situ with heparinized 0.9% saline. Allografts were then minced and digested at 37°C for 30 minutes in 20 ml RPMI-1640 medium containing 10% FCS and 250 U/ml collagenase (Sigma-Aldrich, St. Louis, Missouri, USA). To clear the debris, cell suspensions were rapidly passed down a loosely packed glass wool column (300 mg sterile glass wool in a 10-ml syringe), then mixed with Percoll solution (Sigma-Aldrich) to a concentration of 30%, and centrifuged at 800 g for 15 minutes at room temperature. The pellet was washed and resuspended before flow analysis.
In vivo analysis of memory T cell proliferation and apoptosis by BrdU labeling and TUNEL.
Splenectomized aly mice were pulsed intraperitoneally with 0.8 mg of BrdU (Sigma-Aldrich) 7 days after transplantation. Twenty-four hours later, graft-infiltrating cells were isolated and stained using anti-CD8–PE and 1B2, followed by anti-mouse IgG1–biotin and streptavidin-PerCP (Pharmingen). Cells were then fixed in 70% ethanol followed by 1% paraformaldehyde and incubated with 50 U/ml DNase I (Sigma-Aldrich). Cells were finally stained with anti-BrdU–FITC (BD Biosciences) and analyzed by flow cytometry. To detect apoptosis, graft-infiltrating cells were fixed in 2% paraformaldehyde, permeabilized with 0.1% Triton X-100 solution, and labeled with fluorescein-tagged dUTP by the TUNEL method according to the manufacturer’s instructions (Roche Diagnostics Corp., Indianapolis, Indiana, USA).
Analysis of memory T cell proliferation and apoptosis in vitro.
Purified memory CD8+ T cells (CD8+CD44high) were cultured with Treg cells at a ratio of 1:2 (Treg/memory) in 24-well plates and transwell (Corning-Costar Corp., Cambridge, Massachusetts, USA) in complete RPMI-1640 medium (10% FCS, 2 mM glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin). Irradiated BALB/c spleen cells were also added to the culture to serve as APCs. Anti-FasL mAb was purchased from Pharmingen. Forty-eight hours later, cells were analyzed for apoptosis using the TUNEL method. To measure T cell proliferation, cells were cultured in 96-well plates and pulsed with [3H]-TdR for the last 6 hours. Cells were then harvested and analyzed by a scintillation counter (Perkin-Elmer Inc., Wellesley, Massachusetts, USA).
Intracellular cytokine staining.
To determine Treg cytokine profile, spleen T cells were first stained for surface markers with anti-CD4–PE and anti-CD25–FITC. Cells were then fixed with 2% paraformaldehyde, permeabilized in 0.5% saponin before staining with anti–IL-2–APC or anti–IL-10–APC (Pharmingen). To measure memory recall, memory CD8+ T cells that were cultured for 48 hours were first labeled with anti-CD8–PE and anti-CD44–biotin (Pharmingen) followed by streptavidin-PerCP. Cells were then fixed, permeabilized, and stained with anti–IFN-γ–FITC, and finally analyzed by a FACSCalibur (BD Biosciences).
Results
Antigen-induced CD4+CD25+ Treg cells suppress allograft rejection mediated by memory CD8+ T cells.
We have recently established a model of allograft rejection mediated by memory T cells in the splenectomized alymphoplastic (aly) mouse (28). The splenectomized aly mouse is devoid of secondary lymphoid organs, does not mount a primary immune response, and does not reject an allograft unless it receives effector or memory T cells from a congenic B6 mouse immunized with donor antigens (28, 29). Moreover, lymphopenia-triggered homeostatic proliferation, observed in T cell–deficient hosts such as Rag–/– and SCID mice, does not occur in splenectomized aly mice (30). Therefore, Treg cell phenomena can be studied reliably in the splenectomized aly host without the confounding effects of homeostatic proliferation.
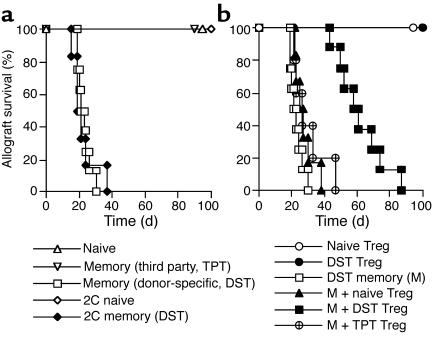
To test whether Treg cells suppress the alloimmune response mediated by memory CD8+ T cells, splenectomized aly mice were transplanted with BALB/c skin. One day later, recipient mice received memory CD8+ T cells and/or Treg cells. As shown in Figure 1a, donor-specific memory CD8+ T cells generated in WT or transgenic 2C.Rag–/– mice rejected skin allografts in splenectomized aly mice. Naive CD8+ T cells or irrelevant memory CD8+ T cells generated against third-party antigens (H-2k) failed to reject allografts, indicating that only donor-specific memory CD8+ T cells mediate rejection in this model. Importantly, Treg cells from DST-treated, but not naive, WT mice significantly delayed allograft rejection when cotransferred with memory CD8+ T cells (Figure 1b). The median allograft-survival time was 22 days in the group that received donor-specific memory T cells alone (M), 24 days in the group that received donor-specific memory T cells plus naive Treg cells (M + naive Treg), and 60 days in the group that received donor-specific memory T cells plus DST-induced Treg cells (M + DST Treg). In contrast, Treg cells from mice primed with third-party (H-2k) splenocyte transfusion (M + TPT Treg) failed to significantly suppress allograft rejection. As control, the transfer of either naive or DST-induced Treg cells alone did not cause allograft rejection (Figure 1b). These data indicate that antigen-induced, but not naive, Treg cells are capable of inhibiting CD8+ T cell memory recall in an allospecific manner.
Figure 1.
Antigen-induced Treg cells suppress allograft rejection mediated by memory CD8+ T cells. (a) Splenectomized aly mice (H-2b), transplanted 1 day earlier with BALB/c skin grafts (H-2d), received 1 × 106 naive CD8+ T cells from WT B6 mice (H-2b) (open triangles, n = 5) or 2C mice (open diamonds, n = 5); or 1 × 106 memory CD8+ T cells from WT B6 mice immunized with donor-specific splenocytes (H-2d) (squares, n = 8) or with third-party splenocytes (H-2k) (open inverted triangles, n = 6), or from 2C mice immunized with donor-specific splenocytes (filled diamonds, n = 6). (b) The same splenectomized aly mice received 1 × 106 Treg cells from naive (open circles, n = 5) or DST-treated (filled circles, n = 5) WT mice either alone or in combination with donor-specific memory CD8+ T cells (M + naive Treg, filled triangles, n = 6; or M + DST Treg, filled squares, n = 8). Control mice received donor-specific memory CD8+ T cells either alone (open squares, n = 8) or in combination with Treg cells from TPT-treated mice (M + TPT Treg, crossed circles, n = 5). DST-induced Treg cells suppressed CD8+ memory T cell–mediated skin allograft rejection (filled vs. open squares, P < 0.05).
Phenotypic and functional characteristics of CD4+CD25+ Treg cells.
Recent studies suggest that CD30+ T cells play an immunoregulatory role (24). To investigate whether CD30 contributes to the regulation of the memory T cell response in our model, we examined CD30 expression on naive and DST-induced CD4+CD25+ Treg cells. As shown in Figure 2, a and b, Treg cells from naive mice were CD30low, while Treg cells from DST-treated mice were CD30high. This finding is consistent with a previous publication by Zhang et al. (22) suggesting that the increased expression of CD30 on DST-induced Treg cells may be associated with their suppression. On the other hand, the majority of naive and DST-induced Treg cells were CD62Lhigh and CD45RBlow or CD45RBintermediate, supporting the original findings by Thornton and Shevach (14). As expected, both naive and DST-induced Treg cells expressed CTLA4. Intracellular cytokine profiling showed that both naive and DST Treg cells expressed IL-10 but not IL-2 (Figure 2c), as did CD30–/– Treg cells (data not shown). Both WT and CD30–/– Treg cells suppressed anti-CD3–induced proliferation of CD4+CD25– T cells in vitro (Figure 2d), indicating that they are similar to conventional Treg cells.
Figure 2.
Characterization of CD4+CD25+ Treg cells. (a) Freshly isolated spleen cells from naive or DST-treated WT mice were stained for surface markers CD4, CD25, CD62L, CD45RB, CTLA4, and CD30 and analyzed in histograms after gating on the CD4+CD25+ T cell population. The dotted lines represent isotype control Ab, and the solid gray and black lines represent naive and DST-induced Treg cells, respectively. One representative experiment of three is shown. (b) Median fluorescence intensity of CD30 on DST Treg cells is higher than on naive Treg cells (*P < 0.05, ANOVA). (c) Freshly isolated spleen cells were also stained for intracellular cytokine expression of IL-2 and IL-10 after gating on CD4+CD25+ T cells. (d) Treg cells suppress anti-CD3–induced proliferation of CD4+CD25– T cells. Purified CD4+CD25+ Treg cells (3 × 104) were cultured with or without naive CD4+CD25– cells (6 × 104) in the presence of soluble anti-CD3 (1.0 μg/ml) and APCs (6 × 104) from BALB/c spleen cells for 72 hours. 50 U/ml of IL-2 was added to Treg cell culture alone to test whether the anergic status of Treg cells can be reversed. Results are presented as the mean of triplicate cultures.
CD30 expression on CD4+CD25+ Treg cells is critical for the suppression of memory CD8+ T cell recall.
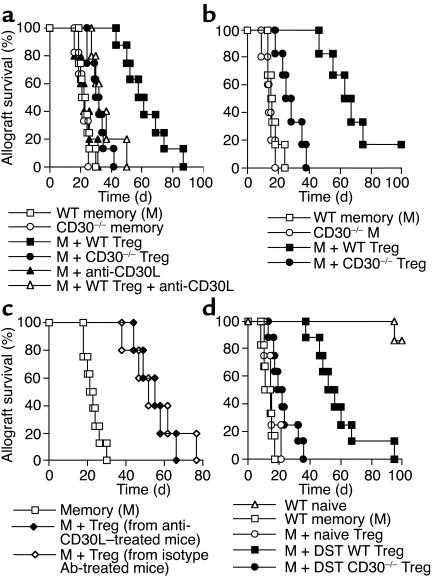
To address whether CD30 expression on Treg cells is necessary for their suppressive function, DST-induced CD4+CD25+ Treg cells were generated in either WT or CD30–/– mice and were cotransferred with memory CD8+ T cells to splenectomized aly recipients that had received BALB/c skin or heart grafts 1 day earlier. As shown in Figure 3, a and b, WT Treg cells significantly delayed both skin and heart graft rejection, while CD30–/– Treg cells failed to do so. Likewise, the suppressive action of WT Treg cells was largely abolished when a blocking anti-CD30L mAb was administered to recipient mice at the time of T cell cotransfer (Figure 3a). In contrast, CD30L blockade did not interfere with the generation of Treg cells, as CD4+CD25+ T cells harvested from WT mice treated with DST plus anti-CD30L were still capable of suppressing allograft rejection (Figure 3c). Administration of isotype control Ab’s did not alter the suppressive function of Treg cells (data not shown). The size of the CD4+CD25+ population was also comparable in CD30–/– and WT mice either before or after DST (5–8% of the CD4+ compartment). Taken together, these data indicate that the CD30/CD30L interaction is required for the suppressive function of antigen-induced Treg cells but not for their generation. Finally, memory CD8+ T cells derived from the immunized CD30–/– mice mediated allograft rejection in splenectomized aly mice at the same rate as did those from their WT counterparts (Figure 3, a and b), suggesting that CD30 does not modulate memory CD8+ T cell function directly.
Figure 3.
CD30 expression on Treg cells is critical for their suppression of allograft rejection mediated by memory CD8+ T cells. Splenectomized aly mice, transplanted 1 day earlier with either BALB/c skin (a) or heart (b) allografts, received 1 × 106 WT (open squares, n = 8) or CD30–/– (open circles, n = 6) memory CD8+ T cells alone, WT memory CD8+ T cells (M) plus WT Treg cells (filled squares, n = 8), M plus CD30–/– Treg cells (filled circles, n = 8), M plus anti-CD30L Ab (filled triangles, n = 5), and M plus both WT Treg cells and anti-CD30L Ab (open triangles, n = 5). Suppression of rejection is diminished when Treg cells lack CD30 (filled squares vs. filled circles, P < 0.05). (c) The same mice received 1 × 106 WT memory CD8+ T cells (M) (open squares, n = 8) alone or in combination with Treg cells generated in WT mice that also received anti-CD30L Ab (filled diamonds, n = 5) or isotype Ab (open diamonds, n = 5) at the time of DST treatment for Treg cell induction. (d) Treg cells also suppress CD8+ memory recall in WT hosts. WT B6 mice, transplanted 1 day earlier with BALB/c heart allografts, received WT naive (open triangles, n = 6) or WT memory (open squares, n = 6) CD8+ cells alone, WT memory CD8+ cells (M) plus Treg cells from naive (open circles, n = 5) or DST-treated (filled squares, n = 8) WT mice, and M plus DST-treated CD30–/– Treg cells (filled circles, n = 8).
Antigen-induced CD4+CD25+ Treg cells suppress memory CD8+ T cell recall in WT hosts.
The data presented so far demonstrate that antigen-induced Treg cells suppress CD8+ memory recall in nonlymphoid tissues, as the experiments were conducted in aly mice. It is unclear whether the same applies to memory responses that occur within secondary lymphoid organs. To test the latter possibility, we cotransferred memory CD8+ T cells and DST-induced CD4+CD25+ Treg cells to WT recipients 1 day after heart transplantation. The recipients were treated at the time of transplantation with CTLA4-Ig and MR1 to block the CD28/B7 and CD40/CD40L costimulatory pathways, respectively. Since these pathways are required for naive but not memory T cell activation, this model allowed us to study the recall of transferred memory T cells in the absence of confounding primary alloimmune responses in the host. As shown in Figure 3d, mice that received memory CD8+ T cells alone rejected their allografts within 18 days after cell transfer, while the majority of control mice that received naive CD8+ T cells kept their allografts for more than 100 days. As in the aly model, the cotransfer of DST-induced, but not naive, CD4+CD25+ Treg cells significantly delayed allograft rejection mediated by memory CD8+ T cells (Figure 3d). These findings indicate that antigen-induced Treg cells suppress CD8+ memory recall in WT mice with normal secondary lymphoid organs and that suppression is not dependent on CD28 and CD40 T cell costimulation. Finally, WT hosts that received CD30–/– Treg cells rejected allografts at a significantly faster pace than those that received WT Treg cells, further confirming that CD30 expression on antigen-induced Treg cells is critical for the suppression of memory CD8+ T cell recall.
Increased apoptosis of memory CD8+ T cells in the presence of Treg cells in vivo.
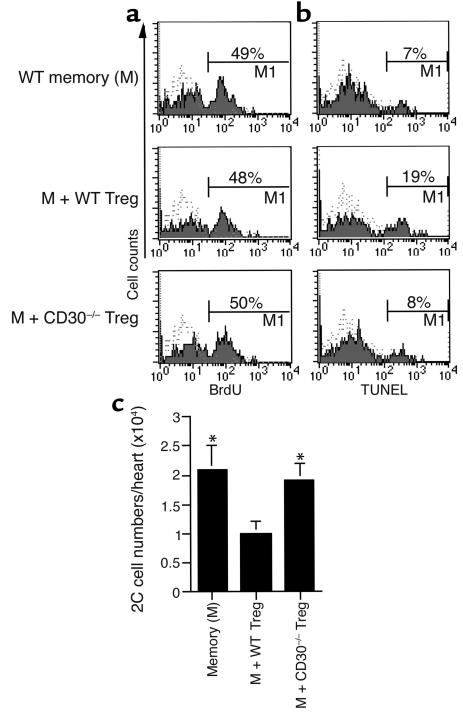
To investigate the mechanisms responsible for Treg cell–mediated suppression in vivo, TCR-transgenic memory CD8+ T cells from 2C.Rag–/– mice were transferred to splenectomized aly mice that had received a cardiac allograft 1 day earlier. 2C memory CD8+ T cells can be tracked in vivo and identified by the clonotypic Ab 1B2 and are therefore referred to as 1B2+CD8+. One week after adoptive transfer of memory 2C cells with or without DST-induced Treg cells, graft-infiltrating cells were isolated and analyzed for proliferation and apoptosis. As shown in Figure 4a, the percentage of proliferating (BrdU+) 1B2+CD8+ T cells in mice that received memory 2C cells alone was similar to that observed in mice that received both memory 2C cells and WT Treg cells, indicating that antigen-induced Treg cells did not inhibit memory CD8+ T cell proliferation in vivo. Similarly, CD30–/– Treg cells did not affect memory CD8+ T cell proliferation either. On the other hand, the cotransfer of WT Treg cells significantly promoted the apoptosis of memory CD8+ T cells, while the cotransfer of CD30–/– Treg cells failed to do so (Figure 4b). Similar results were obtained when grafts were analyzed 2 weeks after the cotransfer of memory and Treg cells (data not shown). In agreement with the apoptosis results, we found that the absolute number of memory 1B2+CD8+ T cells retrieved from each graft was significantly lower in mice that received both memory and WT Treg cells than in mice that received memory T cells alone or memory cells plus CD30–/– Treg cells (Figure 4c). The failure of CD30–/– Treg cells to suppress allograft rejection or to promote the apoptosis of memory CD8+ T cells was not due to defective Treg migration to the graft, as equal numbers of CD4+CD25+ T cells were present in the graft 1 week after the adoptive transfer of either WT or CD30–/– Treg cells (4.5 × 103 ± 0.7 × 103 per graft and 4.3 × 103 ± 0.4 × 103 per graft, respectively). CD4+CD25+ cells were barely detectable in grafts removed from mice that received memory CD8+ T cells alone, indicating that the intragraft CD4+CD25+ population is largely derived from the transferred Treg population.
Figure 4.
Treg cells promote the apoptosis of memory CD8+ T cells but do not inhibit their proliferation in vivo. (a) Analysis of in vivo memory T cell proliferation by BrdU labeling. Splenectomized aly mice, transplanted with a cardiac allograft, received 1B2+CD8+ memory T cells and/or Treg cells and were pulsed intraperitoneally with BrdU 6 days after cell transfer. Twenty-four hours later, graft-infiltrating cells were stained for 1B2, CD8, and BrdU. The percentage of BrdU+ cells is shown in the histograms after gating on 1B2+CD8+ cells. The dotted lines represent isotype control. One of three experiments is shown. (b) Analysis of in vivo memory T cell apoptosis by the TUNEL method. Graft-infiltrating cells from the mice similar to those described above were stained for 1B2, CD8, and TUNEL. The percentage of TUNEL+ cells is shown in histograms after gating on 1B2+CD8+ cells. The dotted lines represent negative control. One of three experiments is shown. (c) Absolute number of memory 1B2+CD8+ T cells per graft was calculated according to flow cytometry. One of three experiments is shown. *P < 0.05 vs. the M + WT Treg group.
Treg cells promote memory CD8+ T cell apoptosis in vitro in a contact-dependent manner.
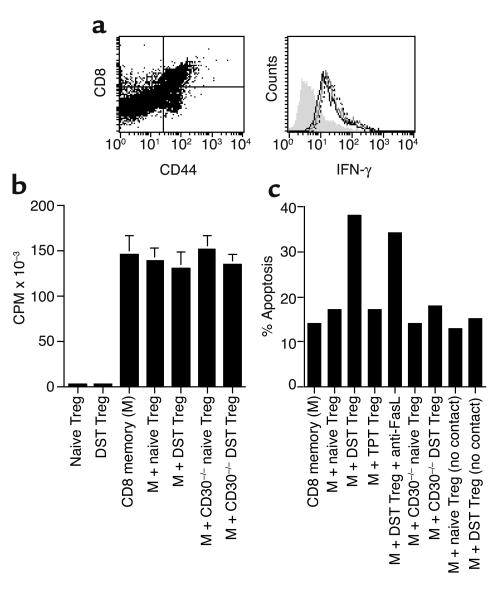
The in vivo data presented above suggest that Treg cells induce the apoptosis of memory CD8+ T cells. To further confirm this finding in vitro, we placed memory CD8+ T cells in coculture with Treg cells and quantitated the apoptosis of the CD8+CD44high population 48 hours later. As shown in Figure 5c, DST-induced WT Treg cells augmented the apoptosis of memory CD8+ T cells approximately 2.5-fold, while naive WT Treg and DST-induced CD30–/– Treg cells failed to do so. This induction of apoptosis was antigen specific, as Treg cells induced by a third-party alloantigen (TPT Treg, Figure 5c) did not promote memory CD8 cell apoptosis. Blocking Fas/FasL interaction by an anti-FasL Ab did not prevent memory cells from being killed by DST Treg cells, suggesting that Treg cells promote memory CD8+ T cell death in a Fas-independent manner. The isotype control Ab for anti-FasL did not affect the memory cell apoptosis (data not shown). The apoptosis of memory T cells was not increased when they were cocultured with Treg cells in transwell that separated Treg and memory cells physically but allowed them to share same media. On the other hand, Treg cells failed to significantly inhibit intracellular expression of IFN-γ in the memory cells (Figure 5a) and did not suppress their proliferation (Figure 5b). Taken together, these data provide evidence that antigen-induced Treg cells suppress the recall of memory CD8+ T cells via induction of their apoptosis but not suppression of proliferation. This proapoptotic function is dependent on the presence of CD30 on Treg cells and on direct cell-cell contact, but independent of Fas/FasL interaction.
Figure 5.
Treg cells promote the apoptosis of memory CD8+ T cells in vitro in a contact-dependent manner. (a) Purified memory CD8+ T cells (CD8+CD44high) were cultured with Treg cells at a ratio of 1:2 (Treg/M) in 24-well plates in the presence of irradiated BALB/c spleen cells (APCs) for 48 hours. Intracellular expression of IFN-γ is shown in histograms after gating on CD8+CD44high cells. The shaded histogram shows isotype control, and the dotted, gray, and black lines represent memory cells (M) alone, M plus naive Treg cells, and M plus DST Treg cells, respectively. (b) Memory CD8+ T cells were incubated as described above. Their proliferation was measured by [3H]-TdR uptakes. Results are presented as the mean of triplicate cultures. (c) Memory CD8+ T cells were cultured with Treg cells (1:2, Treg/memory) in 24-well plates and transwell in the presence of APCs and the indicated agents (5 μg/ml anti-FasL) for 48 hours. Cells were then stained for surface markers, fixed, permeabilized, and measured for apoptosis by the TUNEL method. One of three experiments is presented; data are expressed as percentage of apoptotic CD8+CD44high cells.
Discussion
We demonstrated here that antigen-induced, but not naive, CD4+CD25+ Treg cells suppress allograft rejection mediated by memory CD8+ T cells. This suppression was allospecific, as Treg cells induced by third-party alloantigens did not delay allograft rejection. In vitro and in vivo analyses revealed that antigen-induced Treg cells promote the apoptosis of memory CD8+ T cells but do not inhibit their proliferation, suggesting that the apoptosis of memory T cells is an important mechanism of immune regulation. Suppression of allograft rejection and enhanced memory T cell apoptosis were dependent on the presence of CD30 on Treg cells and on intact CD30/CD30L interaction. This study therefore identifies CD30 as a molecule that is critical for immune regulation and provides direct evidence that pathogenic memory T cells are amenable to suppression in an antigen-specific manner.
Memory T cells constitute a threat to the long-term survival of transplanted organs by mediating allograft rejection despite ongoing immunosuppression (31). Strategies to suppress allospecific memory T cells without causing global immunodeficiency are lacking. Here, we demonstrate that Treg cells induced by the administration of donor-specific transfusion are capable of suppressing allograft rejection mediated by memory CD8+ T cells in an allospecific manner. Our findings are supported by a recent study by Kursar et al., which provided evidence that CD8+ memory responses to an infectious agent (Listeria monocytogenes) are inhibited by CD4+CD25+ Treg cells (32). However, it is not clear in their study whether suppression was antigen specific. Moreover, they found that both naive and antigen-induced Treg cells suppress memory recall, while we observed that memory responses are inhibited only by antigen-induced Treg cells. This discrepancy could be attributed to the fact that they carried out their experiments in lymphocyte-deficient (empty) SCID mice. Lymphopenia-triggered homeostatic proliferation, which occurs in empty hosts, could potentially alter the phenotype and function of transferred T cells.
Several studies in transplantation have demonstrated that regulatory lymphocytes, including CD4+CD25+ Treg cells, effectively suppress primary alloimmune responses and prevent allograft rejection in naive mice (10, 33). Suppression in the majority of these studies was allospecific and was mediated by either naive or antigen-induced Treg cells, although naive Treg cells were less efficient at delaying rejection (34, 35). Our results are consistent with these studies in that suppression of memory T cells was antigen specific. However, we found that antigen-induced, but not naive, Treg cells suppress memory responses. It is possible that antigen-induced Treg cells are more efficient at migrating to nonlymphoid tissues where effector memory CD8+ T cells reside and, thus, inhibit memory responses much more effectively than do naive Treg cells. On the other hand, the suppression of CD8+ memory recall by antigen-induced Treg cells in our model is modest, since allograft rejection, though delayed, ultimately occurred. The failure to completely prevent allograft rejection could be due to two factors: the ratio of Treg to memory cells, and inefficiency of Treg cells’ suppression of memory recall compared with their suppression of naive T cell responses. We used the ratio of 1:1 in the adoptive transfer experiments, which is similar to a physiologic setting given that both CD4+CD25+ Treg and memory CD8+ T cells account for 5–10% of their respective populations. Moreover, studies by others have found that the ratio of 1:2 (Treg/effector) is sufficient to completely suppress naive T cell activation in vitro (14). Therefore, it is likely that Treg cells can only partially suppress memory T cell function, which is compatible with the general concept that memory T cells are less susceptible to immune regulation or immunosuppression than their naive counterparts.
The mechanisms responsible for Treg cell–mediated suppression are not fully understood. Previous studies have provided evidence that suppression is dependent on cell-cell contact, competition for growth factors, or production of anti-inflammatory cytokines such as IL-4, IL-10, and TGF-β, but many of these mechanisms remain controversial (34, 36). In this study, we found that the apoptosis of antigen-specific memory CD8+ T cells that infiltrate the graft is enhanced when antigen-induced Treg cells are present. This was confirmed in coculture experiments wherein antigen-induced Treg cells promoted the apoptosis of memory CD8+ T cells, while naive Treg cells, which did not suppress allograft rejection, failed to do so. Importantly, Treg cells did not influence the proliferation of antigen-specific CD8+ T cells present in the graft. Lin et al. also observed that Treg cells delay allograft rejection without inhibiting the proliferation of alloreactive CD8+ T cells (37). Our results therefore suggest that the apoptosis of memory CD8+ T cells is a critical mechanism by which Treg cells suppress allograft rejection. Others have also provided evidence that Treg cells suppress graft rejection by killing target lymphocytes. Zhang et al. showed that a population of double negative Treg cells prevents allograft rejection by inducing the apoptosis of activated CD8+ T cells (22). Elimination of activated T cells by Treg cells has also been linked to suppression of autoimmunity in murine experimental autoimmune encephalomyelitis (38). The mechanism by which Treg cells induce the apoptosis of memory CD8+ T cells is not known. Potential pathways include killing via the Fas receptor or other members of the TNFR family (22). We found in this study that the expression of CD30 on antigen-induced Treg cells is critical for their ability to suppress allograft rejection and to induce the apoptosis of allospecific CD8+ memory T cells in vivo and in vitro. Their apoptosis induced by Treg cells in vitro is dependent on cell-cell contact, but independent of the Fas pathway.
Although it appears that stimulation via the TCR is required for Treg cells to acquire suppressive function (18), the costimulatory pathways involved in this process remain to be defined. Treg cells express CTLA4 constitutively, but the role of CTLA4/B7 interaction remains controversial (1). Other costimulatory pathways such as CD28/B7, OX40/OX40L, and 4-1BB/4-1BBL have all been shown to be dispensable for Treg cell–mediated suppression (3, 19), although CD28/B7 interaction is critical for the development of Treg cells (39, 40). The inducible costimulator pathway has also been shown to be critical for the development of antigen-specific Treg cells (41), while programmed death–1 plays a role in the regulation of autoimmune diabetes (42). Recent studies provided evidence that blocking the glucocorticoid-induced TNF receptor on Treg cells reverses suppression and breaks self-tolerance (19, 43). We found here that CD30, another member of the TNFR family, which is upregulated on antigen-induced Treg cells, is critical for the ability of these cells to suppress CD8+ memory recall. Specifically, we observed that CD30–/– Treg cells do not suppress allograft rejection nor induce the apoptosis of CD8+ memory T cells. Likewise, blocking CD30/CD30L interaction with anti-CD30L Ab’s abolished suppression in vivo without interfering with Treg cell generation. It is not clear, however, whether CD30 functions as a costimulatory molecule that is required for the acquisition of suppressor function or as an effector molecule that mediates suppression of T cell memory recall.
Acknowledgments
This work was supported by a career award from Juvenile Diabetes Research Foundation International (to Z. Dai) and by NIH grants AI49466 and AI44644 (to F.G. Lakkis).
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Nonstandard abbreviations used: regulatory T (Treg); CTL-associated antigen-4 (CTLA4); T cell receptor (TCR); TNF receptor (TNFR); CD30 ligand (CD30L); C57BL/6 (B6); alymphoplasia/alymphoplastic (aly); recombination-activating gene-2 (Rag2); donor-specific splenocyte transfusion (DST); third-party splenocyte transfusion (TPT); phycoerythrin (PE) peridinin chlorophyll-a protein (PerCP).
References
- 1.Shevach EM. CD4+CD25+ suppressor T cells: more questions than answers. Nat. Rev. Immunol. 2002;2:389–400. doi: 10.1038/nri821. [DOI] [PubMed] [Google Scholar]
- 2.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunological self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J. Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 3.Takahashi T, et al. Immunologic self-tolerance maintained by CD25+CD4+ regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J. Exp. Med. 2000;192:303–309. doi: 10.1084/jem.192.2.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. [PubMed] [Google Scholar]
- 5.Asano M, Toda M, Sakaguchi N, Sakaguchi S. Autoimmune disease as a consequence of developmental abnormality of a T cell subpopulation. J. Exp. Med. 1996;184:387–396. doi: 10.1084/jem.184.2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suri-Payer E, Amar A, Thornton A, Shevach E. CD4+CD25+ T cells inhibit both induction and effector function of autoregulatory T cells and represent a unique lineage of immunoregulatory cells. J. Immunol. 1998;160:1212–1218. [PubMed] [Google Scholar]
- 7.Itoh M, et al. Thymus and autoimmunity: production of CD25+CD4+ naturally anergic and suppressive T cells as a key function of the thymus in maintaining immunologic self-tolerance. J. Immunol. 1999;162:5317–5326. [PubMed] [Google Scholar]
- 8.Shevach EM. Regulatory T cells in autoimmunity. Annu. Rev. Immunol. 2000;18:423–449. doi: 10.1146/annurev.immunol.18.1.423. [DOI] [PubMed] [Google Scholar]
- 9.Qin S, et al. “Infectious” transplantation tolerance. Science. 1993;259:974–977. doi: 10.1126/science.8094901. [DOI] [PubMed] [Google Scholar]
- 10.Kingsley CI, Karim M, Bushell AR, Wood KJ. CD25+CD4+ regulatory T cells prevent graft rejection: CTLA-4- and IL-10-dependent immunoregulation of alloresponses. J. Immunol. 2002;168:1080–1086. doi: 10.4049/jimmunol.168.3.1080. [DOI] [PubMed] [Google Scholar]
- 11.Piccirillo CA, Shevach EM. Cutting edge: control of CD8+ T cell activation by CD4+CD25+ immunoregulatory cells. J. Immunol. 2001;167:1137–1140. doi: 10.4049/jimmunol.167.3.1137. [DOI] [PubMed] [Google Scholar]
- 12.Lakkis FG, Sayegh M. Memory T cells: a hurdle to immunologic tolerance. J. Am. Soc. Nephrol. 2003;44:2402–2410. doi: 10.1097/01.asn.0000085020.78117.70. [DOI] [PubMed] [Google Scholar]
- 13.Read S, et al. CD38+CD45RBlow CD4+ T cells: a population of T cells with immune regulatory activities in vitro. Eur. J. Immunol. 1998;28:3435–3447. doi: 10.1002/(SICI)1521-4141(199811)28:11<3435::AID-IMMU3435>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 14.Thornton A, Shevach E. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin-2 production. J. Exp. Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asseman C, Mauze S, Leach M, Coffmann R, Powrie F. An essential role for interleukin-10 in the function of regulatory T cells that inhibit intestinal inflammation. J. Exp. Med. 1999;190:995–1003. doi: 10.1084/jem.190.7.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Homann D, et al. Autoreactive CD4+ T cells protect from autoimmune diabetes via bystander suppression using the IL-4/Stat6 pathway. Immunity. 1999;11:463–472. doi: 10.1016/s1074-7613(00)80121-1. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura K, Kitani A, Strober W. Cell contact-dependent immunosuppression by CD4+CD25+ regulatory T cells is mediated by cell surface-bound transforming growth factor beta. J. Exp. Med. 2001;194:629–644. doi: 10.1084/jem.194.5.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thornton A, Shevach EM. Suppressor effector function of CD4+CD25+ immunoregulatory T cells is antigen nonspecific. J. Immunol. 2000;164:183–190. doi: 10.4049/jimmunol.164.1.183. [DOI] [PubMed] [Google Scholar]
- 19.McHugh RS, et al. CD4+CD25+ immunoregulatory T cells: gene expression analysis reveals a functional role for the glucocorticoid-induced TNF receptor. Immunity. 2002;16:311–323. doi: 10.1016/s1074-7613(02)00280-7. [DOI] [PubMed] [Google Scholar]
- 20.Horie R, Watanabe T. CD30: expression and function in health and disease. Semin. Immunol. 1998;10:457–470. doi: 10.1006/smim.1998.0156. [DOI] [PubMed] [Google Scholar]
- 21.Bowen MA, Lee RK, Miragliotta G, Nam SY, Podack ER. Structure and expression of murine CD30 and its role in cytokine production. J. Immunol. 1996;156:442–449. [PubMed] [Google Scholar]
- 22.Zhang ZX, Yang L, Young KJ, DuTemple B, Zhang L. Identification of a previously unknown antigen-specific regulatory T cells and its mechanism of suppression. Nat. Med. 2000;6:782–789. doi: 10.1038/77513. [DOI] [PubMed] [Google Scholar]
- 23.Amakawa R, et al. Impaired negative selection of T cells in Hodgkin’s disease antigen CD30-deficient mice. Cell. 1996;84:551–562. doi: 10.1016/s0092-8674(00)81031-4. [DOI] [PubMed] [Google Scholar]
- 24.Gerli R, et al. CD30+ T cells in rheumatoid synovitis: mechanisms of recruitment and functional role. J. Immunol. 2000;164:4399–4407. doi: 10.4049/jimmunol.164.8.4399. [DOI] [PubMed] [Google Scholar]
- 25.Miyawaki S, et al. A new mutation, aly, that induces a generalized lack of lymph nodes accompanied by immunodeficiency in mice. Eur. J. Immunol. 1994;24:429–434. doi: 10.1002/eji.1830240224. [DOI] [PubMed] [Google Scholar]
- 26.Dai Z, Konieczny BT, Baddoura FK, Lakkis FG. Impaired alloantigen-mediated T cell apoptosis and failure to induce long term allograft survival in interleukin-2-deficient mice. J. Immunol. 1998;161:1659–1663. [PubMed] [Google Scholar]
- 27.Zhou J, Carr RI, Liwski RS, Stadnyk AW, Lee TDG. Oral exposure to alloantigen generates intragraft CD8+ regulatory cells. J. Immunol. 2001;167:107–113. doi: 10.4049/jimmunol.167.1.107. [DOI] [PubMed] [Google Scholar]
- 28.Chalasani G, Dai Z, Konieczny B, Baddoura FK, Lakkis FG. Recall and propagation of allospecific memory T cells independent of secondary lymphoid organs. Proc. Natl. Acad. Sci. U. S. A. 2002;99:6175–6180. doi: 10.1073/pnas.092596999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lakkis FG, Arakelov A, Konieczny BT, Inoue Y. Immunologic ‘ignorance’ of vascularized organ transplants in the absence of secondary lymphoid tissue. Nat. Med. 2000;6:686–688. doi: 10.1038/76267. [DOI] [PubMed] [Google Scholar]
- 30.Dai Z, Lakkis FG. Cutting edge: secondary lymphoid organs are essential for maintaining the CD4, but not CD8, naive T cell pool. J. Immunol. 2001;167:6711–6715. doi: 10.4049/jimmunol.167.12.6711. [DOI] [PubMed] [Google Scholar]
- 31.Heeger PS, et al. Pretransplant frequency of donor-specific, IFN-γ-producing lymphocytes is a manifestation of immunologic memory and correlates with the risk of posttransplant rejection episodes. J. Immunol. 1999;163:2267–2275. [PubMed] [Google Scholar]
- 32.Kursar M, et al. Regulatory CD4+CD25+ T cells restrict memory CD8+ T cell responses. J. Exp. Med. 2002;196:1585–1592. doi: 10.1084/jem.20011347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graca L, Cobbold SP, Waldmann H. Identification of regulatory T cells in tolerated allografts. J. Exp. Med. 2002;195:1641–1646. doi: 10.1084/jem.20012097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Graca L, et al. Both CD4+CD25+ and CD4+CD25– regulatory cells mediate dominant transplantation tolerance. J. Immunol. 2002;168:5558–5565. doi: 10.4049/jimmunol.168.11.5558. [DOI] [PubMed] [Google Scholar]
- 35.Davies JD, et al. CD4+CD45RB low-density cells from untreated mice prevent acute allograft rejection. J. Immunol. 1999;163:5353–5357. [PubMed] [Google Scholar]
- 36.Piccirillo CA, et al. CD4+CD25+ regulatory T cells can mediate suppressor function in the absence of transforming growth factor beta1 production and responsiveness. J. Exp. Med. 2002;196:237–246. doi: 10.1084/jem.20020590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin CY, Graca L, Cobbold SP, Waldmann H. Dominant transplantation tolerance impairs CD8+ T cell function but not expansion. Nat. Immunol. 2002;3:1208–1213. doi: 10.1038/ni853. [DOI] [PubMed] [Google Scholar]
- 38.Madakmutil L, Maricic I, Sercarz E, Kumar V. Regulatory T cells control autoimmunity in vivo by inducing apoptotic depletion of activated pathogenic lymphocytes. J. Immunol. 2003;170:2985–2992. doi: 10.4049/jimmunol.170.6.2985. [DOI] [PubMed] [Google Scholar]
- 39.Salomon B, et al. B7/CD28 costimulation is essential for the homeostasis of the CD4+CD25+ immunoregulatory T cells that control autoimmune diabetes. Immunity. 2000;12:431–440. doi: 10.1016/s1074-7613(00)80195-8. [DOI] [PubMed] [Google Scholar]
- 40.Lohr J, Knoechel B, Jiang S, Sharpe AH, Abbas AK. The inhibitory function of B7 costimulators in T cell responses to foreign and self-antigens. Nat. Immunol. 2003;4:664–669. doi: 10.1038/ni939. [DOI] [PubMed] [Google Scholar]
- 41.Akbari O, et al. Antigen-specific regulatory T cells develop via the ICOS-ICOS-ligand pathway and inhibit allergen-induced airway hyperreactivity. Nat. Med. 2002;8:1024–1032. doi: 10.1038/nm745. [DOI] [PubMed] [Google Scholar]
- 42.Ansari MJI, et al. The programmed death-1 (PD-1) pathway regulates autoimmune diabetes in NOD mice. J. Exp. Med. 2003;198:63–69. doi: 10.1084/jem.20022125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shimizu J, Yamazaki S, Takahashi T, Ishida Y, Sakaguchi S. Stimulation of CD25+CD4+ regulatory T cells through GITR breaks immunological self-tolerance. Nat. Immunol. 2002;3:135–142. doi: 10.1038/ni759. [DOI] [PubMed] [Google Scholar]