Abstract
OBJECTIVE
To determine contributions of trunk and extremity adiposity to cardiometabolic risk factors (blood pressure, fasting blood glucose, HDL cholesterol, and triglycerides) among white and African American adults.
RESEARCH DESIGN AND METHODS
The sample consisted of 1,129 white women, 779 African American women, 1,012 white men, and 300 African American men.
RESULTS
Higher trunk adiposity was significantly associated with an increased risk of having two or more cardiometabolic risk factors among African American and white men and women. After adjustment for trunk and arm adiposity, higher leg adiposity was significantly associated with a decreased risk of having two or more cardiometabolic risk factors among white men and women and African American women.
CONCLUSIONS
In contrast with adverse risk with high trunk adiposity, high leg adiposity is associated with a decreased risk of having two or more cardiometabolic risk factors in both African American and white adults.
Obesity, a significant public health problem throughout the world (1), is strongly associated with cardiometabolic risk (2–5). There is growing recognition that adipose tissue stored in different body depots may have differential impacts on health. Several studies have assessed the associations of leg and trunk adiposity with cardiometabolic risk factors (6–12). Some, but not all, of these studies have found an inverse association of leg adiposity with blood pressure (11,12), glucose (7–12), dyslipidemia (6–8,11), and the metabolic syndrome (12). Moreover, these studies were carried out in white (6–10), Japanese (11), and Chinese (12) populations, and no studies included African Americans. Because African Americans have higher mortality rates from cardiovascular disease, diabetes, and cancer than white Americans (13), it is necessary to understand these differences and their clinical implications. The aim of this study is to determine the contribution of trunk and extremity adiposity to cardiometabolic risk factors among white and African American men and women.
RESEARCH DESIGN AND METHODS
Study sample
The Pennington Center Longitudinal Study (PCLS) is designed to assess the effects of lifestyle factors and obesity on the development of chronic disorders (14). The sample is composed of participants who have enrolled in studies at the Pennington Biomedical Research Center (PBRC) from 1995 to 2010. The current investigation is limited to individuals who had a dual-energy X-ray absorptiometry (DEXA) scan, fasting serum lipids and glucose, and BMI <40 kg/m2. There were 3,220 adults aged 18–64 years (1,129 white women, 779 African American women, 1,012 white men, and 300 African American men) who met these criteria. Each volunteer provided written informed consent, and all study procedures were approved by the PBRC Institutional Review Board.
Measurements
Total body fat mass and fat mass in the arms and legs (in kilograms) were estimated by DEXA using a Hologic scanner, as described previously (14). High blood pressure was defined as resting systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg or reported as hypertension. Serum lipids and plasma glucose were obtained from a 12-h fasting blood draw. Low HDL cholesterol was defined as ≤40 mg/dL for men and ≤50 mg/dL for women. High triglycerides were defined as ≥150 mg/dL. High glucose was defined as plasma glucose ≥100 mg/dL or reported as diabetes based on the American Heart Association metabolic syndrome definition (15).
Statistical analysis
Multiple logistic regression models were used to assess the associations of trunk, arm, and leg adiposity, with the risk of having two or more risk factors (high blood pressure, low HDL, high triglycerides, and high glucose). The multivariable-adjusted model included age, year of testing, ethnicity, smoking, postmenopausal status (in women), trunk adiposity, arm adiposity, and leg adiposity. All statistical analyses were performed with PASW for Windows 18.0 (SPSS, Inc., Chicago, IL).
RESULTS
African American women had significantly greater BMI, waist circumference, trunk, arm, and leg adiposity and high prevalence (%) of having two or more risk factors (38.9 vs. 32.5) compared with white women, and white men had significantly greater trunk and arm adiposity and higher prevalence of having two or more risk factors (42.7 vs. 38.1) compared with African American men. Compared with white women and men, African American women and men had higher prevalence of high blood pressure (40.8 vs. 25.3 in women, 36.7 vs. 32.7 in men) and high glucose (42.2 vs. 27.8, 43.0 vs. 40.7) and lower prevalence of low HDL (30.9 vs. 34.4, 22.1 vs. 30.9) and high triglycerides (12.2 vs. 28.9, 17.9 vs. 34.8).
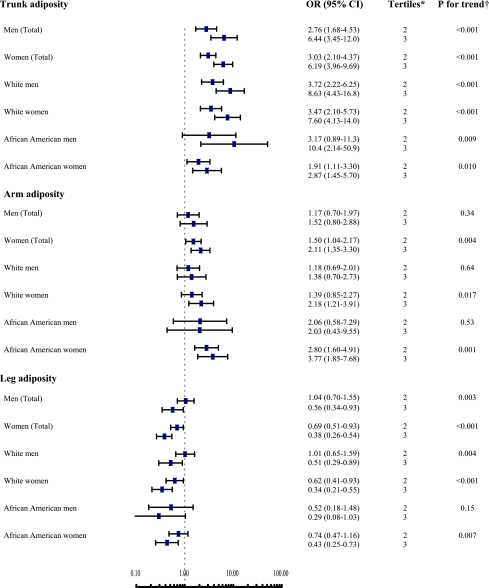
Higher trunk adiposity was significantly associated with an increased risk of two or more risk factors among both men and women (Fig. 1). Higher arm adiposity was significantly associated with an increased risk of having two or more risk factors among women but not among men. Higher leg adiposity was significantly associated with a decreased risk of having two or more risk factors among both men and women.
Figure 1.
ORs (95% CI) for having two or more abnormal risk factors in subjects classified in the second and third sex- and ethnic-specific tertiles of trunk adiposity, arm adiposity, and leg adiposity compared with those in the first tertile (reference group, OR = 1.0) among African American and white men and women. These were adjusted for age, year of testing, smoking status, menopausal status (in women), trunk adiposity, arm adiposity, and leg adiposity, other than the variable in the analytic model. *The first tertile is the reference (OR = 1.0); †test is for trend across tertiles of adiposity. (A high-quality color representation of this figure is available in the online issue.)
With data stratified by sex and ethnicity, a positive association of trunk adiposity with having two or more risk factors was present among African American and white men and women (all P for trend ≤0.01) (Fig. 1). In contrast, an inverse association of leg adiposity with having two or more risk factors was present in white men and women and African American women (all P for trend <0.01).
CONCLUSIONS
The results indicate that trunk adiposity is positively and leg adiposity is inversely associated with having two or more cardiometabolic risk factors among African American and white adults. These opposite associations were independent of each other. The mechanisms behind these associations are not clear. However, there is some evidence that adipogenic metabolite secretion and gene expression in trunk fat may differ from that in extremity fat (12).
Several studies have found an inverse association of leg adiposity and an adverse effect of trunk adiposity on cardiovascular risk factors (6–12). However, most of these studies were performed in elderly populations (6–9,12) and with small sample sizes (n < 180) (6–10). Moreover, the previous studies were carried out in white (6–10), Japanese (11), and Chinese (12) populations, and no studies to our knowledge have included sizable samples of African Americans. Our result strengthens the above findings and provides confirmation for opposite associations of leg and trunk adiposity with having risk factors. It is important to note that significant racial differences in abdominal depots and in the prevalence of obesity have been found in our previous study (14) and in the 2007–2008 National Health and Nutrition Examination Survey (1).
The strengths of this study include the large sample of white and African American adults who had body fat estimates from DEXA and the battery of cardiometabolic risk factors. However, the sample is not necessarily representative of the local population. The participants were volunteers for studies conducted at PBRC, and almost all of them are healthy. Nonetheless, the sample (65% whites, 35% African Americans) is reflective of the ethnic diversity in Louisiana. Another limitation is that DEXA could not discriminate between subcutaneous and intramuscular adiposity in the legs and visceral and subcutaneous adiposity in the trunk. A further limitation is that data on physical activity, education, and dietary intake were not available, so the influence of these variables on the observed relationships could not be explored. Finally, we cannot conclude any cause-effect associations from this cross-sectional study.
In conclusion, the current study indicates that leg adiposity, in contrast with trunk adiposity, is associated with a favorable profile of having two or more risk factors among both African American and white adults. Further studies on the physiological mechanisms are needed.
Acknowledgments
PCLS is supported by the Pennington Biomedical Research Center. C.B. is partially funded by the John Barton, Sr., Chair in Genetics and Nutrition; E.R. is partially funded by the Douglas L. Gordon Chair in Diabetes and Metabolism; and P.T.K. is partially funded by the Louisiana Public Facilities Authority Endowed Chair in Nutrition.
No potential conflicts of interest relevant to this article were reported.
G.H. analyzed and interpreted data, performed statistical analysis, wrote the manuscript, and reviewed and edited the manuscript. C.B. provided the study concept and design, analyzed and interpreted data, contributed to the discussion, and reviewed and edited the manuscript. G.A.B. and F.L.G. acquired data, contributed to the discussion, and reviewed and edited the manuscript. W.D.J. provided the study concept and design, analyzed and interpreted data, contributed to the discussion, and reviewed and edited the manuscript. R.L.N., E.R., and D.H.R. acquired data, contributed to the discussion, and reviewed and edited the manuscript. P.T.K. provided the study concept and design, analyzed and interpreted data, contributed to the discussion, and reviewed and edited the manuscript.
The authors thank Emily Mire and Connie Murla for contributions to data management and the many clinical scientists and staff of the Pennington Biomedical Research Center who have contributed data to the PCLS, particularly Drs. Steven Smith, William Cefalu, Nikhil Dhurandhar, Lilian Levitan, Timothy Church, Paula Geiselman, Alok Gupta, Corby Martin, and Thomas Gettys.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–241 [DOI] [PubMed] [Google Scholar]
- 2.Hu G, Barengo NC, Tuomilehto J, Lakka TA, Nissinen A, Jousilahti P. Relationship of physical activity and body mass index to the risk of hypertension: a prospective study in Finland. Hypertension 2004;43:25–30 [DOI] [PubMed] [Google Scholar]
- 3.Hu G, Lindström J, Valle TT, et al. Physical activity, body mass index, and risk of type 2 diabetes in patients with normal or impaired glucose regulation. Arch Intern Med 2004;164:892–896 [DOI] [PubMed] [Google Scholar]
- 4.Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J 2004;25:2212–2219 [DOI] [PubMed] [Google Scholar]
- 5.Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation 2010;121:237–244 [DOI] [PubMed] [Google Scholar]
- 6.Paradisi G, Smith L, Burtner C, et al. Dual energy X-ray absorptiometry assessment of fat mass distribution and its association with the insulin resistance syndrome. Diabetes Care 1999;22:1310–1317 [DOI] [PubMed] [Google Scholar]
- 7.Van Pelt RE, Evans EM, Schechtman KB, Ehsani AA, Kohrt WM. Contributions of total and regional fat mass to risk for cardiovascular disease in older women. Am J Physiol Endocrinol Metab 2002;282:E1023–E1028 [DOI] [PubMed] [Google Scholar]
- 8.Van Pelt RE, Jankowski CM, Gozansky WS, Schwartz RS, Kohrt WM. Lower-body adiposity and metabolic protection in postmenopausal women. J Clin Endocrinol Metab 2005;90:4573–4578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azuma K, Heilbronn LK, Albu JB, Smith SR, Ravussin E, Kelley DE; and the Look AHEAD Adipose Research Group Adipose tissue distribution in relation to insulin resistance in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 2007;293:E435–E442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pigeon E, Couillard E, Tremblay A, Bouchard C, Weisnagel SJ, Joanisse DR. Mid-thigh subcutaneous adipose tissue and glucose tolerance in the Quebec family study. Obes Facts 2008;1:310–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sakai Y, Ito H, Egami Y, et al. Favourable association of leg fat with cardiovascular risk factors. J Intern Med 2005;257:194–200 [DOI] [PubMed] [Google Scholar]
- 12.Wu H, Qi Q, Yu Z, et al. Independent and opposite associations of trunk and leg fat depots with adipokines, inflammatory markers, and metabolic syndrome in middle-aged and older Chinese men and women. J Clin Endocrinol Metab 2010;95:4389–4398 [DOI] [PubMed] [Google Scholar]
- 13.Lloyd-Jones D, Adams RJ, Brown TM, et al. ; WRITING GROUP MEMBERS; American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation 2010;121:e46–e215 [DOI] [PubMed] [Google Scholar]
- 14.Katzmarzyk PT, Bray GA, Greenway FL, et al. Racial differences in abdominal depot-specific adiposity in white and African American adults. Am J Clin Nutr 2010;91:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement: Executive Summary. Circulation 2005;112:e285–e290 [DOI] [PubMed] [Google Scholar]