Abstract
Background:
Chordoid glioma is a rare brain tumor typically located within the anterior third ventricle. It is a well-circumscribed, non-infiltrative tumor that grows as a mass within the ventricle.
Case Description:
We present the case of a 50-year-old woman with a chordoid glioma located in the anterior third ventricle. Unusually, MRI revealed an enlarged optic chiasm. Histological sampling of the chiasm revealed tumor invasion.
Conclusion:
Involvement of the optic apparatus is generally thought to be an imaging feature that can be used to distinguish chordoid gliomas from optic/hypothalamic gliomas. This case provides the first reported exception to this dogma.
Keywords: Chordoid glioma, optic apparatus invasion, third ventricle tumor
INTRODUCTION
Chordoid glioma is a rare tumor of the anterior third ventricle.[1] To date, 65 cases have been reported.[4] Owing to its rarity and only recent characterization, it is not typically considered when encountering anterior third ventricular and suprasellar tumors. On MRI it has clear borders, it is isointense or hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging. It uniformly enhances. Unlike diffusely infiltrative glial tumors, chordoid gliomas are thought of as being well encapsulated and non-invasive.[10] We report here the first description of a chordoid glioma that involves the optic chiasm.
CASE REPORT
A 50-year-old woman presented with short-term memory loss and occasional headaches. A CT scan revealed a large suprasellar mass that was isodense and uniformly enhancing. Small foci of calcification were evident. MRI demonstrated that the tumor was located in the anterior third ventricle exerting rostral pressure on the fornices. Suprachiasmatic and retrochiasmatic components were also evident [Figure 1]. The tumor was hypointense of T1, hyperintense on T2, and uniformly enhancing [Figure 1a–c. The optic chiasm appeared significantly enlarged and hyperintense on T2-weighted sequences [Figure 1e and f. Importantly, gadolinium enhancement was evident within the optic chiasm [Figure 1d and g]. Clinical examination revealed hypothalamic-pituitary axis dysfunction restricted to hypothyroidism. Ophthalmologic exam was normal. Neuropsychological assessment revealed deficits in both verbal and non-verbal memory. Difficulties in divergent thinking, sustained attention, and organization were also identified. Adaptive learning was maintained.
Figure 1.
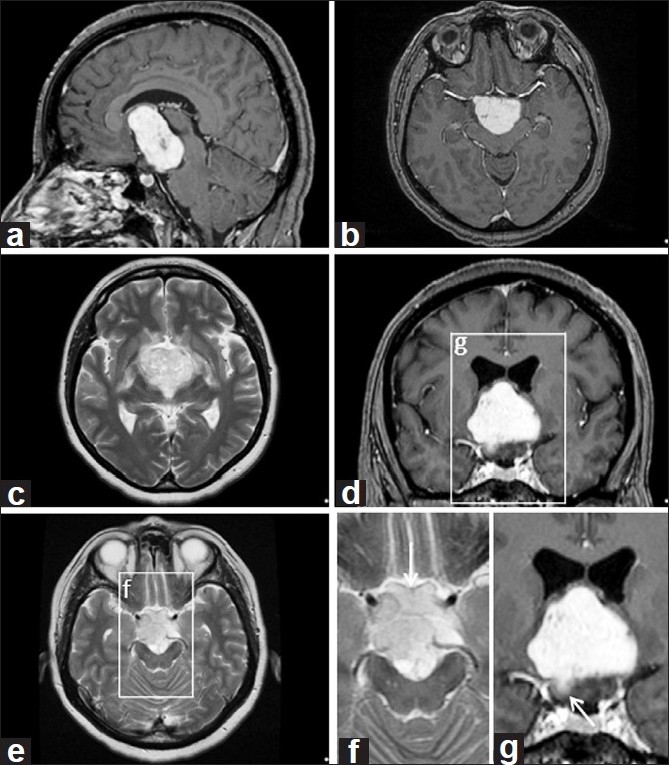
Sagittal (a) and axial (b) gadolinium enhanced images. (c) T2-weighted axial image. (d) Coronal gadolinium enhanced image. (e) T2-weighted axial image showing involvement of the optic chiasm. (f) High magnification image from (e) revealing hyperintense signal in the optic chiasm (OC). (g) High magnification image from (d) revealing enhancement within the right optic chiasm (Rt OC)
A right pterional craniotomy and orbital osteotomy was performed. Upon dissection of the optic apparatus it was apparent that the optic chiasm was involved in the tumoral process. It was grossly enlarged with an infrachiasmatic growth caudal to the right optic nerve [Figure 2]. Biopsy confirmed the presence of tumor within the optic chiasm. The operation was terminated at this point. The patient did not develop a new neurological deficit postoperatively.
Figure 2.
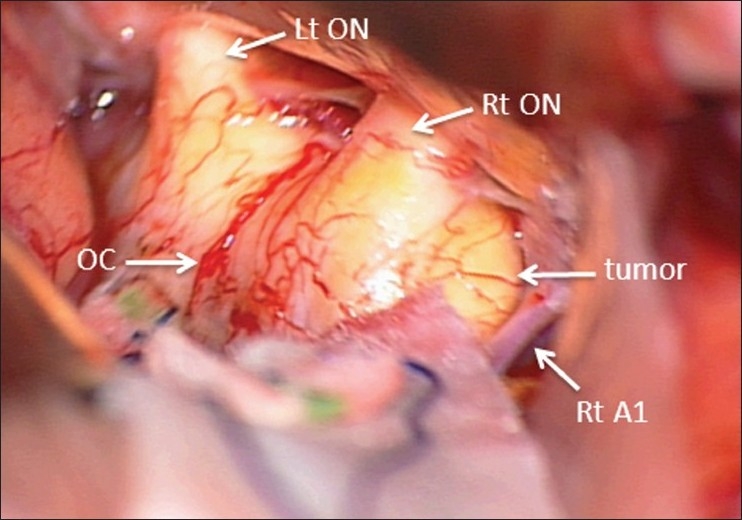
Intraoperative image revealing the extent of optic chiasm enlargement from a right lateral suprachiasmatic view. OC – optic chiasm, Lt ON – left optic nerve, Rt ON – right optic nerve, Rt Al – A1 portion of the right anterior cerebral artery
Pathological examination revealed cords of epithelioid cells separated by a mucinous background. Cells were positive for glial fibrillary acidic protein. Epidermal growth factor receptor positive cells were also identified. A single mitotic cell was found. A CD45-positive lymphocytic infiltrate was also seen. These findings are consistent with a chordoid glioma.
The patient and family were informed regarding the diagnosis, prognosis, risks of resection, and radiotherapy. The patient deferred further treatment until evidence of growth on imaging or worsening symptoms. The tumor has remained unchanged over 18 months and the patient remains unchanged neurologically.
DISCUSSION
Chordoid glioma is a rare tumor of the anterior third ventricle. It is only recently characterized and not typically included in the differential diagnosis of suprachiasmatic and third ventricular tumors. To date, 65 cases have been reported.[4] Of these cases, all but one has been located within the anterior third ventricle.[3]
Lesions commonly seen in this location include craniopharyngiomas, optic/hypothalamic gliomas, germ cell tumors, meningiomas, Rathke's cleft cysts, hamartomas, and pituitary macroadenomas. Imaging features that can help to distinguish chordoid gliomas from other lesions in this location include displacement of the infundibulum and involvement of the optic apparatus. Chordoid gliomas displace the infundibulum posteriorly. In contrast, Rathke's cleft cysts and tuber cinereum hamartomas displace the infundibulum anteriorly.[6] Optic/hypothalamic gliomas typically involve the optic apparatus, whereas it is generally thought that chordoid gliomas are well circumscribed and do not involve or extend into the optic apparatus.[6]
Surgical reports have consistently confirmed the lack of optic apparatus involvement observed on MR imaging. Ricoy et al.[8] described the presence of tumor in the retrochiasmatic space without attachment to the chiasm or surrounding structures. Pomper et al.[6] reported that tumor was absent from the optic apparatus. Pasquier et al.[5] described a case in which the tumor was contiguous with, but did not extend into, the optic chiasm. Grand et al.[2] reported that the tumor was not adherent to surrounding structures. Raizer et al.[7] described a tumor which was adherent to, but did not infiltrate, the optic chiasm. Lastly, Suh et al.[9] reported compression of the chiasm without tumor extension into the chiasm. Beyond the expected visual symptoms caused by a tumor in this location, there are no reports of tumor invasion into the optic apparatus.
Of the 65 reported cases of chordoid glioma, none have been shown to involve the optic chiasm. This is the first demonstration of a chordoid glioma that involves the optic chiasm on imaging with intraoperative confirmation. We thus propose that the presence of optic chiasm involvement should not be used as a feature to exclude chordoid glioma from the differential diagnosis of suprasellar/anterior third ventricular tumors.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/53/80118
Contributor Information
Qasim S. Al Hinai, Email: qalhinai@gmail.com.
Kevin Petrecca, Email: kevin.petrecca@mcgill.ca.
REFERENCES
- 1.Brat DJ, Scheithauer BW, Staugaitis SM, Cortez SC, Brecher K, Burger PC. Third ventricular chordoid glioma: A distinct clinicopathological entity. J Neuropathol Exp Neurol. 1998;57:283–90. doi: 10.1097/00005072-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Grand S, Pasquier B, Gay E, Kremer S, Remy C, Le Bas JF. Chordoid glioma of the third ventricle: CT and MRI, including perfusion data. Neuroradiol. 2002;44:842–6. doi: 10.1007/s00234-002-0820-0. [DOI] [PubMed] [Google Scholar]
- 3.Jain D, Sharma MC, Sarkar C, Suri V, Rishi A, Garg A, et al. Chordoid glioma: report of two rare examples with unusual features. Acta Neurochir. 2008;150:295–300. doi: 10.1007/s00701-008-1420-x. [DOI] [PubMed] [Google Scholar]
- 4.Liu W, Cheng J, Yi X, Zhen H, Fei Z, Li Q, et al. Chordoid Glioma, a case report and literature review. Neurologist. 2011;17:52–6. doi: 10.1097/NRL.0b013e3181e7db67. [DOI] [PubMed] [Google Scholar]
- 5.Pasquier B, Peoc’h M, Morrison AL, Gay E, Pasquier D, Grand S, et al. Chordoid glioma of the third ventricle: A report of two new cases, with further evidence supporting an ependymal differentiation, and review of the literature. Am J Surg Pathol. 2002;26:1330–42. doi: 10.1097/00000478-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Pomper MG, Passe TJ, Burger PC, Scheithauer BW, Brat DJ. Chordoid glioma: A neoplasm unique to the hypothalamus and anterior third ventricle. Am J Neuroradiol. 2001;22:464–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Raizer JJ, Shetty T, Gutin PH, Obbens EA, Holodny AI, Antonescu CR, et al. Chordoid glioma: report of a case with unusual histologic features, ultrastructural study and review of the literature. J Neuro Oncol. 2003;63:39–47. doi: 10.1023/a:1023752717042. [DOI] [PubMed] [Google Scholar]
- 8.Ricoy JR, Lobato RD, Baez B, Caballo A, Martinez MA, Rodriguez G. Suprasellar chordoid glioma. Acta Neuropathol. 2000;99:699–703. doi: 10.1007/s004010051183. [DOI] [PubMed] [Google Scholar]
- 9.Suh YL, Kim NR, Kim JH, Park SH. Suprasellar chordoid glioma combined with Rathke's cleft cyst. Pathol Int. 2003;53:780–5. doi: 10.1046/j.1440-1827.2003.01549.x. [DOI] [PubMed] [Google Scholar]
- 10.Tu A, Yeo T, Steinke D, Resch L, Mehta V. Chordoid glioma, imaging pearls of unique third ventricular tumour. Can J Neurol Sci. 2010;37:677–80. [PubMed] [Google Scholar]


