Abstract
Objectives
To examine patterns of onset and abuse/dependence episodes of prescription opioid (PO) and heroin use disorders in a national sample of adults, and to explore differences by gender and substance abuse treatment status.
Methods
Analyses of data from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (N = 43,093).
Results
Of all respondents, 5% (n = 1815) reported a history of nonmedical PO use (NMPOU) and 0.3% (n = 150) a history of heroin use. Abuse was more prevalent than dependence among NMPOUs (PO abuse, 29%; dependence, 7%) and heroin users (heroin abuse, 63%; dependence, 28%). Heroin users reported a short mean interval from first use to onset of abuse (1.5 years) or dependence (2.0 years), and a lengthy mean duration for the longest episode of abuse (66 months) or dependence (59 months); the corresponding mean estimates for PO abuse and dependence among NMPOUs were 2.6 and 2.9 years, respectively, and 31 and 49 months, respectively. The mean number of years from first use to remission from the most recent episode was 6.9 years for PO abuse and 8.1 years for dependence; the mean number of years from first heroin use to remission from the most recent episode was 8.5 years for heroin abuse and 9.7 years for dependence. Most individuals with PO or heroin use disorders were remitted from the most recent episode. Treated individuals, whether their problem was heroin or POs, tended to have a longer mean duration of an episode than untreated individuals.
Conclusion
Periodic remissions from opioid or heroin abuse or dependence episodes occur commonly but take a long time. Timely and effective use of treatment services are needed to mitigate the many adverse consequences from opioid/heroin abuse and dependence.
Keywords: comorbidity, heroin use disorders, natural recovery, opioid use disorders, prescription opioid abuse, self-change
Introduction
The US has an epidemic of nonmedical prescription opioid use (NMPOU) with the expected resulting problems (eg, overdose, deaths, hospital admissions).1–3 Since the early 2000s, the prevalence of prescription opioid (PO) use disorders (POUDs: abuse or dependence) has risen to match that of cocaine use disorders as the second most common illicit drug use disorder following marijuana. Although the number of Americans with past-year cocaine use disorders has declined somewhat, the number of people with a POUD or who are treated for problems related to prescription opioid (PO) use has continued to increase. For example, 1.9 million Americans were estimated to have a past-year POUD in 2009 compared with 1.1 million Americans with a cocaine use disorder, and the number of individuals who received substance abuse treatment for PO use problems rose from 0.36 million in 2002 to 0.74 million in 2009.3 Furthermore, drug-related unintentional overdose, the second leading cause of unintentional death in the US (after motor vehicles), often involves POs and has a mortality rate exceeding those associated with heroin and cocaine.1,2,4
Although heroin addiction has been the primary focus of opioid addiction research for several decades, the rising rate of POUDs highlights a shifting profile of individuals with opioid use disorders and a need for research on courses of POUDs to inform research, assessment, and interventions. For instance, an estimated 0.40 million Americans had a past-year heroin use disorder (HUD) in 2009 compared with an estimated 1.9 million with a POUD in the past year.3 Notably, the official Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) classification for opioid abuse and dependence does not distinguish between heroin and POs, and research data on courses of POUDs and heroin abuse are lacking.5 Because dependence and abuse are defined hierarchically by DSM-IV and because only individuals without a dependence diagnosis for a drug are given a diagnosis for abuse of the drug, studies following this logic often have not assessed abuse for individuals with dependence, resulting in a lack of course-related data for abuse specifically, and POUDs in general.5
However, the growing diversity of individuals with POUDs (eg, women, young people, whites) plus expanded treatment options for opioid addiction (office-based treatment with buprenorphine) drive the need for research to obtain data on possible differences and similarities between POUDs and HUDs.6–9 Results from clinical samples have suggested that heroin users manifest a higher level of illicit drug and treatment use than NMPOUs, and an increasing number of individuals with PO use problems are younger, white, or female.8,10,11 These differences in demographics and drug use history suggest that NMPOUs may be different from heroin users in their patterns of use or longer-term course, thus indicating differential treatment needs. Given that abuse or dependence on POs or heroin are considered together under opioid use disorders in DSM-IV, studies such as the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) that identify individuals whose main problem is heroin versus POs and assess for histories of abuse and dependence regardless of dependence status can provide a better understanding of these issues.3
Here, we analyze the NESARC data to discern course-related features pertaining to abuse and dependence for NMPOUs and include parallel analyses for heroin users as a comparison. Due to gender differences in addiction and treatment needs and the need for data to improve service use by untreated drug users, we also explore the pattern of course according to gender and lifetime substance abuse treatment history.9,12 We address the following questions: i) Are there differences in prevalence rates of abuse, dependence, and remission from the most recent episode (at the time of interview) by gender and treatment use status? ii) Are there differences in age of first use, age of first occurrence of abuse or dependence, length of an abuse or a dependence episode, and duration from first use to remitting from the most recent episode by gender and treatment use status? and iii) Do heroin users who develop abuse or dependence have a more severe pattern of their disorder than NMPOUs?
Methods
Study sample
The 2001–2002 NESARC, the largest US comorbidity study of psychiatric disorders carried out to date, provides national prevalence rates for DSM-IV substance use and other psychiatric disorders in the general population.13 The target population was the civilian noninstitutionalized population aged 18 years or older who resided in the US or the District of Columbia, including Alaska and Hawaii. Eligible respondents included people living in households, military personnel living off base, and residents of group quarters (boarding houses, rooming houses, nontransient hotels and motels, shelters, facilities for housing workers, college quarters, and group homes).
Professional lay interviewers from the Census Bureau administered face-to-face interviews using computer-assisted methods that protected confidentiality.13 All respondents provided written informed consent and were assured that their participation was voluntary. To increase the accuracy of national estimates for demographic subgroups, Hispanics (N = 8308), non-Hispanic blacks (N = 8245), and respondents aged 18–24 years (N = 5199) were oversampled. Of the 43,093 respondents, 18,518 were male and 24,575 were female. The household and individual response rates were 89% and 93%, respectively; the overall survey response rate was 82%. Details of the survey designs are reported elsewhere.13–15
Study variables
Drug use and disorders (abuse or dependence) were assessed with the Alcohol Use Disorders and Associated Disabilities Interview Schedule of DSM-IV, an instrument of demonstrated reliability and validity.14 Illicit or nonmedical drug use was defined as the use of substance(s) either without a doctor’s prescription; in greater amounts, more often, or longer than prescribed; or for a reason other than prescribed by a doctor. Respondents were asked a series of questions to determine whether they had ever used the following drug classes: marijuana, solvents, cocaine, hallucinogens, heroin, POs, sedatives, amphetamines, and tranquilizers.
Nonmedical PO use referred to any self-reported nonmedical use of PO analgesics such as codeine, Darvon®, Percodan®, Dilaudid®, or Demerol®; heroin use was assessed separately.12 Respondents who responded affirmatively to the yes/no question regarding nonmedical PO use and heroin use, respectively, were defined as lifetime NMPOUs and heroin users, respectively. Respondents who reported any lifetime use of a given substance (PO and heroin, respectively) were then assessed by a complete set of diagnostic questions operationalized to assess clinical features of DSM-IV abuse (role interference, hazardous use, legal problems, social/interpersonal problems) and dependence (withdrawal, tolerance, taking the substance in larger amounts than intended or for a longer time, inability to cut down on use, greater amount of time spent to obtain the substance, giving up other important daily activities, continued substance use despite resulting problems). For all these questions, abuse and dependence were assessed separately.
Respondents were also assessed for age of first use (use onset), age of first occurrence of abuse symptoms (abuse onset) and dependence symptoms (dependence onset), total number of abuse and dependence episodes, duration (in months) of the longest abuse and dependence episode, and recentness of abuse and dependence episodes. In NESARC, age of remission from the most recent episode was based on age when the symptoms of abuse or dependence had completely stopped. An episode was defined as a discrete experience of abuse symptoms or dependence symptoms that were separated by at least 1 year when the respondent either stopped using the substance or did not have any of the specified experiences. An interval between two events was determined by taking the difference in the respondent’s age at each event; when both events happened in the same year, a mean estimate (0.5 year) was used for the interval.
History of substance abuse treatment use and familial substance abuse problems were examined as potential correlates of POUD and heroin abuse/dependence.12 A personal history of substance abuse treatment was defined as having ever received treatment services for problems related to alcohol or drug use at any location (inpatient, outpatient, emergency room, addiction or mental health treatment program, jail, self-help group).15 Familial substance abuse problems included self-reported positive family history of alcohol or drug use problems among any of the respondent’s biological family members.12
Socioeconomic variables (age, gender, race/ethnicity, educational level, and total annual family income) were examined to elucidate demographic disparities in OUDs.
Data analysis
Because NESARC used a complex multistage survey design, data were weighted and analyzed with SUDAAN®.16 In the total sample (N = 43,093), 1815 NMPOUs and 150 heroin users were identified. Among these lifetime opioid users, we examined socioeconomic characteristics, lifetime substance abuse treatment use, and familial substance abuse by abuse and dependence status using χ2 tests. The prevalence of abuse, dependence, and remission from the most recent abuse or dependence episode for NMPOU and heroin use, respectively, was calculated. Age of first NMPOU and heroin use, age of onset of abuse or dependence, total number of episodes, length of the longest episode, duration between age of first use and age of onset of abuse or dependence, and duration between age of first use and age of remission from the most recent abuse or dependence episode were then determined. Finally, we used logistic regression procedures to determine correlates of abuse, dependence, and remission from the most recent episode. All results presented are weighted estimates taking into account complex survey designs (clustering, weighting),16 except for sample sizes, which are unweighted. For ease of interpretation, 95% confidence intervals (CI) for estimates are reported, and a P value less than 0.05 is considered significantly different between two groups.
Results
Selected characteristics of opioid/heroin users
Of all NESARC respondents (N = 43,093), 5% (n = 1815) reported any lifetime NMPOU, 0.3% (n = 150) had used heroin, and 0.2% (n = 98) had used both nonmedical POs and heroin in their lifetime. The analyses reported here focused on the first two groups. Table 1 summarizes characteristics of this study sample using DSM-IV classification for three mutually exclusive groups: none, abuse without dependence (ie, at least one abuse criterion, did not meet criteria for dependence), and any dependence (ie, met criteria for dependence).
Table 1.
Selected characteristics of lifetime nonmedical prescription opioid and heroin users by Diagnostic and Statistical Manual of Mental Disorders, 4th Edition diagnostic status in the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions
| Characteristics | Lifetime nonmedical prescription opioid users, n = 1815
|
Lifetime heroin users, n = 150
|
||||||
|---|---|---|---|---|---|---|---|---|
| None | Prescription opioid abusea | Prescription opioid dependence | χ2 (df) P value | None | Heroin abusea | Heroin dependence | χ2 (df) P value | |
|
|
||||||||
| n = 1294 | n = 390 | n = 131 | n = 46 | n = 53 | n = 51 | |||
| Age in years, mean (SE) | 37.0 (0.51) | 37.5 (0.75) | 38.0 (1.36) | 0.69c | 42.5 (1.74) | 39.0 (2.32) | 43.5 (1.90) | 0.34c |
| Education in years, mean (SE) | 9.8 (0.10) | 9.4 (0.10) | 8.9 (0.20) | <0.01c | 9.2 (0.30) | 9.6 (0.38) | 9.1 (0.27) | 0.47c |
| Age | ||||||||
| 18–34 | 46.7 (1.83) | 41.1 (3.21) | 38.7 (5.41) | 4.86 (4) | 20.8 (7.41) | 29.2 (8.56) | 15.7 (5.82) | 1.90 (4) |
| 35–44 | 24.8 (1.25) | 30.2 (2.78) | 25.2 (4.90) | 0.31 | 29.4 (8.03) | 27.6 (7.34) | 26.8 (7.05) | 0.75 |
| 45+ | 28.4 (1.52) | 28.7 (2.85) | 36.1 (5.61) | 49.8 (8.64) | 43.2 (8.40) | 57.5 (8.07) | ||
| Gender | ||||||||
| Male | 58.4 (1.60) | 71.5 (2.83) | 57.6 (4.87) | 16.11(2) | 77.3 (6.64) | 70.2 (8.12) | 77.1 (5.56) | 0.59 (2) |
| Female | 41.6 (1.60) | 28.5 (2.83) | 42.4 (4.87) | <0.01 | 22.7 (6.64) | 29.8 (8.12) | 22.9 (5.56) | 0.75 |
| Race/ethnicity | ||||||||
| White | 80.3 (1.81) | 80.4 (2.43) | 72.7 (5.09) | 9.96 (6) | 84.3 (4.83) | 73.1 (6.19) | 54.6 (7.66) | 10.69 (4) |
| Black | 6.6 (0.82) | 4.6 (1.03) | 7.2 (2.34) | 0.15 | 12.3 (4.37) | 16.2 (4.78) | 14.8 (3.99) | 0.04 |
| Hispanic | 7.7 (1.12) | 7.2 (1.46) | 6.9 (3.38) | 3.4 (1.97)b | 10.6 (3.87)b | 30.6 (7.76)b | ||
| Other | 5.5 (0.92) | 7.8 (1.93) | 13.2 (3.28) | |||||
| Educational level | ||||||||
| Less than high school | 13.3 (1.08) | 15.9 (2.49) | 29.5 (5.06) | 12.44 (4) | 21.0 (6.74) | 16.9 (5.93) | 19.3 (5.88) | 2.25 (4) |
| High school | 27.6 (1.70) | 33.1 (2.92) | 26.5 (4.43) | 0.02 | 25.1 (7.69) | 38.6 (8.91) | 41.2 (8.26) | 0.69 |
| College or more | 59.1 (1.92) | 51.0 (3.10) | 44.0 (5.71) | 53.9 (8.46) | 44.5 (8.66) | 39.5 (7.92) | ||
| Family income | ||||||||
| <$35,000 | 46.2 (1.83) | 49.9 (3.15) | 65.8 (4.78) | 13.61 (4) | 49.1 (8.62) | 60.9 (8.77) | 71.9 (7.24) | 4.83 (4) |
| $35,000–$69,999 | 32.7 (1.50) | 33.7 (2.92) | 21.9 (4.07) | 0.01 | 34.3 (8.16) | 25.9 (7.97) | 14.8 (5.49) | 0.32 |
| $70,000+ | 21.1 (1.65) | 16.4 (2.27) | 12.3 (3.57) | 16.6 (7.47) | 13.2 (5.72) | 13.3 (6.33) | ||
| Lifetime substance abuse treatment | ||||||||
| Yes | 22.3 (1.33) | 43.3 (2.99) | 68.0 (4.86) | 52.72 (2) | 57.9 (8.24) | 68.5 (7.41) | 84.0 (5.55) | 7.23 (2) |
| No | 77.7 (1.33) | 56.7 (2.99) | 32.0 (4.86) | <0.01 | 42.1 (8.24) | 31.5 (7.41) | 16.0 (5.55) | 0.03 |
| Family history of substance abuse | ||||||||
| Yes | 79.9 (1.42) | 87.9 (1.80) | 87.7 (3.21) | 12.57 (2) | 90.8 (4.01) | 80.7 (7.45) | 92.2 (4.15) | 1.77 (2) |
| No | 20.1 (1.42) | 12.2 (1.80) | 12.3 (3.21) | <0.01 | 9.2 (4.01) | 19.3 (7.45) | 7.8 (4.15) | 0.42 |
Notes:
Abuse without dependence;
Hispanics and others were combined due to a zero cell (the none group) for “others”;
P values of F-test.
Abbreviation: SE, standard error.
Of the 1815 who reported NMPOU, 22.8% (n = 390) had PO abuse without dependence and 7.2% had any PO dependence (5.9% had abuse and dependence; 1.3% had dependence without abuse). Of the 150 heroin users, 35.1% had heroin abuse without dependence and 28.2% had any dependence (27.7% had abuse and dependence; 0.5% had dependence without abuse). The mean age was 37. 2 years (95% CI = 36.3–38.0) among NMPOUs and 41.6 (95% CI = 39.2–43.9) among heroin users. The mean number of years of education was 9.6 years (95% CI = 9.5–9.8) among NMPOUs and 9.3 (95% CI = 8.9–9.7) among heroin users.
A high proportion of NMPOUs with PO abuse were men (72%) or whites (80%), in the low-income group (50%), or had a college education (51%); NMPOUs with dependence were more likely than NMPOUs with abuse to be female or less educated, have a low income, and have used substance abuse treatment. Among heroin users, the dependence group comprised a higher proportion of nonwhites (45% vs 16%) and used treatment more often than heroin users who did not have an HUD (84% vs 58%).
Prevalence, demographics, and course of abuse and dependence
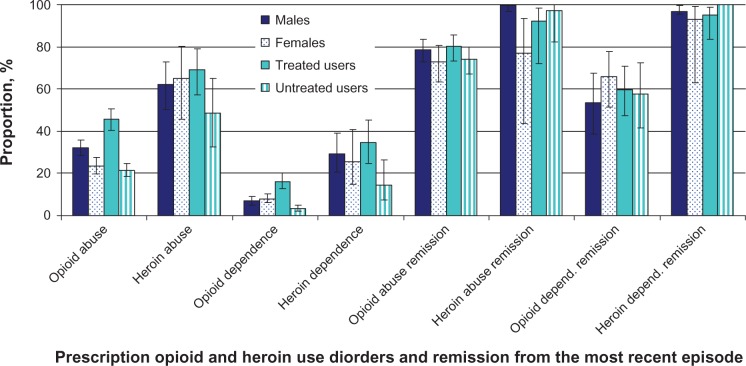
Figure 1 displays the results of the prevalence and patterns related to any abuse (ie, at least one abuse criterion, not excluded if had dependence), any dependence, and remission from the most recent episode. Abuse was more prevalent than dependence among NMPOUs (any PO abuse, 29%; any dependence, 7%) and among heroin users (any heroin abuse, 63%; any dependence, 28%). Among NMPOUs, PO abuse was more prevalent among men (32% vs 24%; χ2 P < 0.01) and substance abuse treatment users (46% vs 22%; χ2 P < 0.01) compared with women and nontreatment users; dependence was also more prevalent among treatment users than among nonusers (16% vs 3%; χ2 P < 0.01). Most individuals with PO abuse (77%) or dependence (59%) were remitted from the most recent episode; however, an even higher proportion of individuals with heroin abuse (94%) or dependence (96%) were remitted from the most recent episode. More men with heroin abuse remitted than women with heroin abuse (99% vs 77%; χ2 P < 0.05).
Figure 1.
Lifetime prevalence of prescription opioid use disorders and remissiona from the most recent episode among lifetime nonmedical prescription opioid users; lifetime prevalence of heroin use disorders and remissiona from the most recent episode among lifetime heroin users: 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions: by gender and lifetime substance abuse treatment status. Lines extending from bars indicate 95% confidence intervals of the estimates.
Note: aRemission does not necessarily indicate sustained remission.
Patterns of courses for abuse and dependence
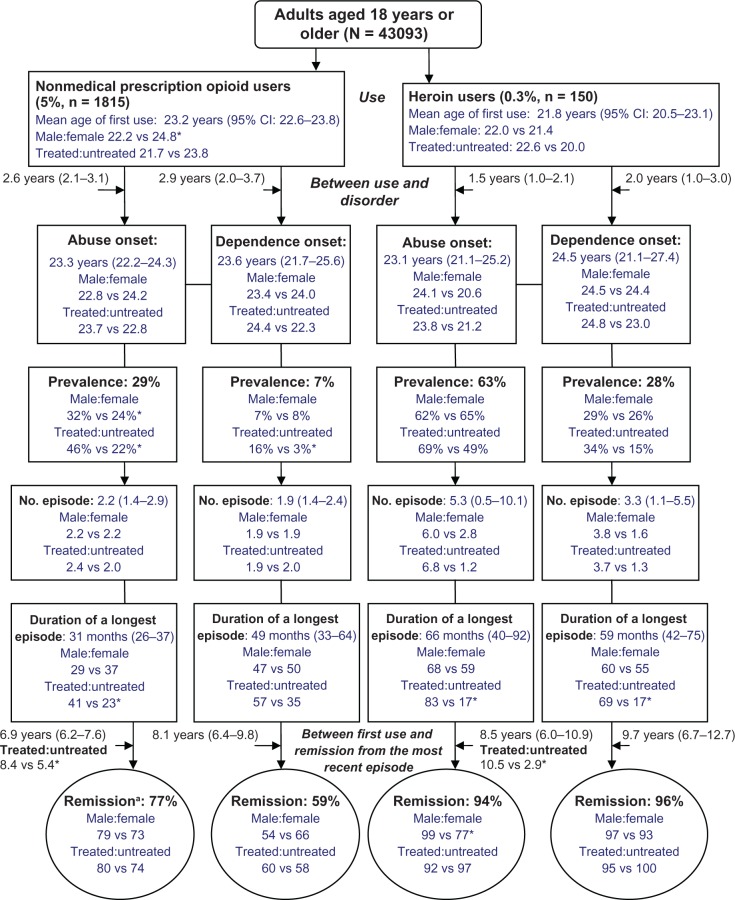
Figure 2 summarizes patterns related to the courses of abuse and dependence. Results for age of onset, duration between age of first use and age of a disorder onset or remission, and number and duration of episodes are mean estimates.
Figure 2.
Patterns of courses of prescription opioid use disorders among lifetime nonmedical prescription opioid users; patterns of courses of heroin use disorders among lifetime heroin users: 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Figures in the parenthesis are 95% confidence intervals of the mean.
Notes: aRemission does not necessarily indicate sustained remission. *P<0.05.
Age of first use
NMPOUs and heroin users reported a similar mean age of first use (23.2 years; 70% with onset ≤24 years for NMPOU and 21.8 years; 74% with onset ≤24 years for heroin). Men and treatment users had an earlier mean age of first NMPOU than females (22.2 years vs 24.8 years) and nonusers of treatment (21.7 years vs 23.8 years).
Age of first abuse or dependence
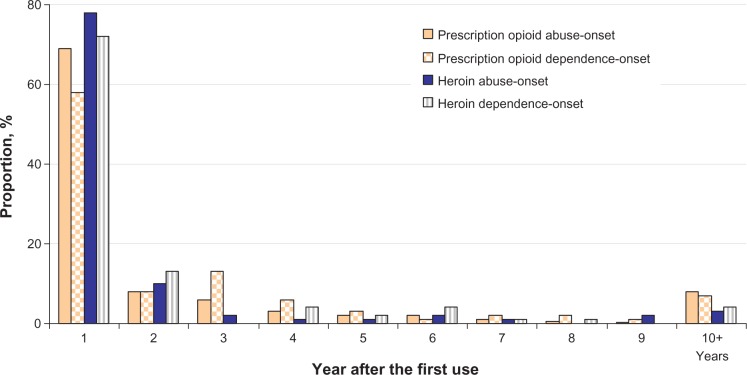
Among NMPOUs, there were no gender or treatment differences in mean age of onset of PO abuse (23.3 years; 71% with onset ≤24 years) or dependence (23.6 years; 68% with onset ≤24 years). There were also no gender or treatment differences in mean age of onset of heroin abuse (23.1 years; 71% with onset ≤24 years) or dependence (24.5 years; 59% with onset ≤24 years). However, heroin users reported a short mean interval between first heroin use and onset of abuse (1.5 years, 95% CI = 1.0–2.1; 88% within 2 years) or dependence (2.0 years, 95% CI = 1.0–3.0; 85% within 2 years) (Figure 3). The mean interval between first NMPOU and onset of PO abuse was 2.6 years (95% CI = 2.1–3.1; 77% within 2 years); the mean interval between first use and onset of PO dependence was 2.9 years (95% CI = 2.0–3.7; 66% within 2 years).
Figure 3.
Proportions of onset of prescription opioid abuse or dependence by year after the first nonmedical use of prescription opioids among individuals with the corresponding opioid use disorder; proportions of onset of heroin abuse or dependence by year after first heroin use among individuals with the corresponding heroin use disorder.
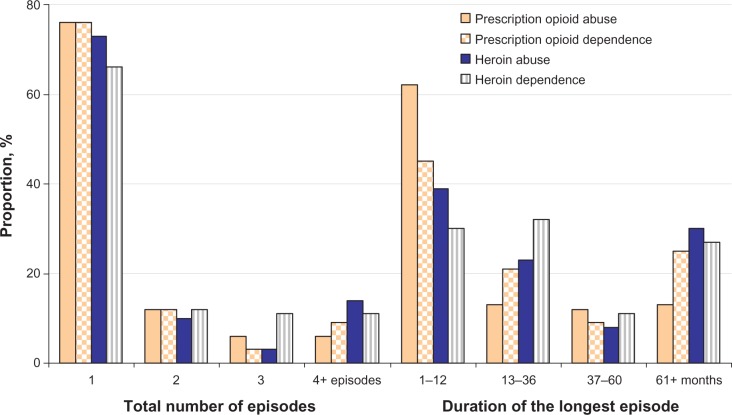
Episodes and duration
The majority of NMPOUs with either abuse (95% CI = 1.4–2.9; 88% with 1–2 episodes) or dependence (95% CI = 1.4–2.4) had 1–2 abuse or dependence episodes (Figure 4). In the PO abuse group, the mean duration of the longest abuse episode was 31.4 months (95% CI = 25.8–36.9; 25% with an episode lasting 37+ months); treatment users reported a longer mean duration of a PO abuse (40.5 months; 95% CI = 31.0–50.0) than untreated users (23.4 months; 95% CI = 18.3–28.5). The mean duration for the longest dependence episode in the PO dependence group was 48.5 months (95% CI = 32.5–64.4; 34% with an episode lasting 37+ months).
Figure 4.
Total number of prescription opioid abuse or dependence episodes (1–4+) and the duration of the longest episode (1–12 to 61+ months) among individuals with the corresponding opioid use disorder; total number of heroin abuse or dependence episodes (1–4+) and the duration of the longest episode (1–12 to 61+ months) among individuals with the corresponding heroin use disorder.
Heroin users with abuse averaged 5.3 abuse episodes (95% CI = 0.5–10.1; 83% with 1–2 episodes); those with dependence averaged 3.3 dependence episodes (95% CI = 1.1–5.5; 78% with 1–2 episodes). Among individuals with heroin abuse, the mean duration for the longest episode was 65.9 months (95% CI = 39.7–92.0; 38% with an episode lasting 37+ months); the mean duration for the longest dependence episode in the heroin dependence group was 58.7 months (95% CI = 42.7–75.3; 38% with an episode lasting 37+ months). In either the abuse (treated: 82.7 months, 95% CI = 50.5–114.9; untreated: 17.2 months, 95% CI = 6.9–27.6) or the dependence (treated: 68.5 months, 95% CI = 47.2–89.8; untreated: 17.0 months, 95% CI = 11.0–23.1) groups, treated heroin users had a longer mean duration of an abuse or dependence episode than untreated users.
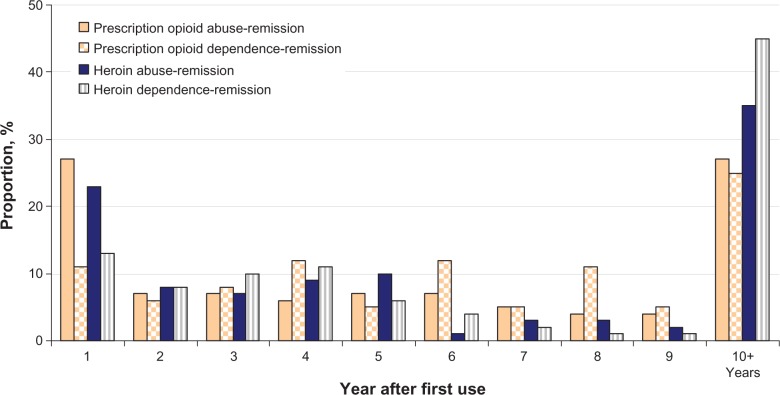
Lag between first use and remission
The mean interval between age of first NMPOU and age of remission from the most recent episode was 6.9 years (95% CI = 6.2–7.6; 27% with an interval of 10+ years) for PO abuse (Figure 5) and 8.5 years for PO dependence (95% CI = 6.0–10.9; 25% with an interval of 10+ years); treated NMPOUs (8.4 years, 95% CI = 7.3–9.5) had a longer interval before remitting from the most recent abuse episode than untreated NMPOUs (5.4 years, 95% CI = 4.5–6.3). The mean interval between age of first heroin use and age of remission from the most recent episode was 8.5 years (95% CI = 6.0–10.9; 35% with an interval of 10+ years) for heroin abuse and 9.7 years for dependence (95% CI = 6.7–12.7; 45% with an interval of 10+ years); treated heroin users (10.5 years; 95% CI = 7.5–13.4) had a longer mean interval before remitting from the most recent abuse episode than untreated users (2.9 years; 95% CI = 1.7–4.2).
Figure 5.
Proportions of remissiona from the most recent prescription opioid abuse or dependence episode by year after the first nonmedical use of prescription opioids among individuals remitted from the corresponding disorder; proportions of remissiona from the most recent heroin abuse or dependence episode by year after the first heroin use among individuals remitted from the corresponding disorder.
Note: aRemission does not necessarily indicate sustained remission.
Logistic regression of abuse, dependence, and full remission
Among NMPOUs (n = 1815), adjusted multinomial logistic regression analyses were conducted to examine correlates of PO abuse without dependence and dependence compared with no POUD (three mutually exclusively groups). Males, substance abuse treatment users, and individuals with familial substance abuse problems showed increased odds of PO abuse (Table 2); individuals who did not complete high school and substance abuse treatment users had elevated odds of PO dependence.
Table 2.
Adjusted logistic regression of correlates of prescription opioid abuse, dependence, and remission among lifetime nonmedical prescription opioid users by gender and history of substance abuse treatment status in the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions
| Characteristic | Adjusted multinomial logistic regression (n = 1815) | Adjusted logistic regression model (n = 453) | Adjusted logistic regression model (n = 131) | |
|---|---|---|---|---|
|
|
||||
| Prescription opioid abusea | Prescription opioid dependence | Remission from prescription opioid abuseb | Remission from prescription opioid dependence | |
|
|
||||
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Age in years | ||||
| 18–34 | 0.90 (0.62–1.30) | 0.70 (0.40–1.21) | 0.59 (0.30–1.17) | 0.27 (0.08–0.91) |
| 35–44 | 1.17 (0.83–1.64) | 0.70 (0.36–1.35) | 0.85 (0.40–1.82) | 0.35 (0.12–1.07) |
| 45+ | 1.00 | 1.00 | 1.00 | 1.00 |
| Gender | ||||
| Male | 1.67 (1.24–2.274)c | 0.86 (0.54–1.36) | 1.40 (0.77–2.55) | 0.42 (0.14–1.22) |
| Female | 1.00 | 1.00 | 1.00 | 1.00 |
| Race/ethnicity | ||||
| White | 1.42 (0.87–2.32) | 1.04 (0.48–2.26) | 1.62 (0.69–3.80) | 1.47 (0.22–9.66) |
| Black | 1.00 | 1.00 | 1.00 | 1.00 |
| Hispanic | 1.39 (0.77–2.50) | 0.97 (0.29–3.19) | 0.72 (0.25–2.04) | 1.18 (0.08–17.89) |
| Other | 2.11 (0.92–4.83) | 2.40 (0.96–5.99) | 0.77 (0.31–1.91) | 1.21 (0.15–9.95) |
| Educational level | ||||
| Less than high school | 1.21 (0.76–1.92) | 2.17 (1.16–4.06)c | 2.19 (1.07–4.50)c | 0.40 (0.12–1.31) |
| High school | 1.26 (0.91–1.75) | 1.10 (0.60–2.01) | 0.88 (0.53–1.47) | 1.89 (0.50–7.12) |
| College or more | 1.00 | 1.00 | 1.00 | 1.00 |
| Family income | ||||
| <$35,000 | 1.32 (0.85–2.04) | 1.83 (0.96–3.93) | 0.62 (0.27–1.42) | 1.59 (0.40–6.26) |
| $35,000–$69,999 | 1.26 (0.83–1.91) | 1.01 (0.44–2.31) | 0.86 (0.34–2.15) | 1.11 (0.24–5.16) |
| $70,000+ | 1.00 | 1.00 | 1.00 | 1.00 |
| Lifetime substance abuse treatment | ||||
| Yes | 2.35 (1.73–3.18)c | 6.80 (3.96–11.66)c | 1.40 (0.79–2.49) | 0.79 (0.32–1.95) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Family history of substance abuse | ||||
| Yes | 1.75 (1.20–2.55)c | 1.54 (0.82–2.89) | 1.80 (0.89–3.61) | 1.15 (0.40–3.29) |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
Notes:
Abuse without dependence;
any abuse regardless of dependence status;
P < 0.05.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval.
Among individuals with a history of any PO abuse (n = 453), adjusted logistic regression analysis showed that individuals who did not complete high school had elevated odds of remission from abuse. Among individuals with a history of any PO dependence (n = 131), none of the variables examined was associated with remission. Logistic regression analysis of remission was not conducted for heroin users, due to the small sample of users with a history of any abuse (n = 96) or dependence (n = 50).
Discussion
Main findings
This study of a national sample of opioid users suggests some similarities and differences between nonmedical PO users and heroin users in course-related features of DSM-IV abuse and dependence. First, lifetime abuse was far more prevalent than lifetime dependence among NMPOUs and heroin users, and a particularly high proportion of heroin users were affected by either abuse or dependence. Second, regardless of heroin or PO use, the majority of individuals with a history of disorder experienced it within 2 years of use initiation, and a much high proportion of heroin users did so. Third, for both abuse and dependence, individuals with a POUD or HUD often had few abuse or dependence episodes; however, a considerable proportion in each group (eg, PO dependence, heroin abuse or dependence) had an episode lasting for 3+ years. Fourth, NMPOUs with a POUD were similar to heroin users with a HUD in having a long interval between first use and remission from the most recent episode. Fifth, irrespective of treatment use, the majority of individuals with either a POU or a HUD were remitted from the most recent episode, and more untreated individuals had a shorter duration of heroin abuse or dependence or of PO abuse than treated individuals, suggesting that those who become involved in treatment have more severe disorders.
What this study adds
To our knowledge, this study is the first to present separate course-related patterns for POUDs and HUDs. Given the rising number of individuals using substance abuse treatment for problems related to POUDs3 and a lack of empirical course information for healthcare providers, these findings on differences between POUDs and HUDs have clinical implications for interventions. Results show that most individuals with either a POUD or a HUD initiated their first use before the age of 25 years, experienced abuse or dependence within 2 years of initiation, and had lengthy abuse or dependence episodes that might eventually remit. The short duration between use initiation and disorder onset, but the extended period of abuse or dependence episodes, highlights the need for early prevention, screening, and timely intervention to reduce occurrences of more costly consequences from abuse or dependence (eg, poor role functioning, health risks), severe medical complications (HIV, hepatitis C), or premature death (overdose, accidents, suicide).1,2,4–9,17 In particular, heroin shows a high level of negative impact on users: 63% of users met criteria for heroin abuse and 28% for dependence compared with 29% of NMPOUs with PO abuse and 7% with dependence. As suggested by these findings and others, this distinction may be related to differences in users’ demographic and drug use profiles, as a higher proportion of heroin users than NMPOUs are older or male and have a more severe pattern of drug use that may be less likely to remit fully without substance abuse treatment.8–12,18 Thus, although DSM-IV opioid use disorder diagnoses apply to both groups, heroin users seeking treatment are likely to have the most complex problems and treatment needs. However, POUDs are not necessarily less significant than HUDs; instead, the differences observed indicate differential needs for treatment approach.11
This study also adds information by showing that a high proportion of individuals with a HUD experienced a prolonged abuse or dependence episode. However, a considerable proportion of individuals with PO abuse (25%) or dependence (34%) also reported a particularly lengthy (37+ months) episode, revealing a similar chronicity and negative impact on quality of life (eg, poor role-related or emotional functioning) for a subset, perhaps those who had sought treatment. Research has shown that adults who used treatment for POUDs often had prior episodes of substance abuse treatment and reported significantly poorer quality of life in multiple mental and physical heath domains.19 Our results also suggest that the span of an episode may have an influence on treatment use, as it may be a better indicator for the level of poor functioning or impairment than age of use or disorder onset. For instance, among individuals with PO abuse, those with a history of substance abuse treatment, on average, reported a lengthier abuse episode (41 months vs 23 months) and duration between first use and remission from the most recent episode (8.3 years vs 5.3 years) than the untreated; this difference was even more distinct among individuals with heroin abuse (treated, 83 months; untreated, 17 months) or dependence (treated, 69 months; untreated, 17 months).
Another salient finding is that many adults with PO abuse (77%) or dependence (59%) or those with heroin abuse (94%) or dependence (96%) were remitted from the most recent episode, and that proportions of remission did not differ by history of any substance abuse treatment service use. This pattern is in line with other studies that have reported recovery without substance abuse treatment or self-change (“natural recovery”), which appears to be a common pathway to remission.17,20–22 This finding in turn implies that individuals with addiction are eventually able to remit, though the process is lengthy and many adverse consequences (eg, suicides, accidents, premature mortality) can occur during that time.1,2,4,17,20–22 Although little is known about the mechanism by which people change, factors related to wanting to quit substance use or initiate change may include recognition of one’s problem as serious, having adverse consequences, realizing that drug-using “friends” are not really friends, role change, growing older, and finding new means of social support.21,23–25 In regard to treatment, many studies have shown that agonist maintenance not only decreases drug use, criminal activities, HIV infections, and mortality but also reduces the likelihood of using costly health treatment services (eg, emergency or inpatient treatment).26–29 As shown from these findings, many individuals with a POUD or a HUD experienced a protracted period of abuse or dependence before their most recent remission, suggesting that there are many opportunities for interventions to reduce drug use and its related adverse effects. Potential areas of research include identifying and modifying factors underlying drug users’ perceived burdens of, or barriers to, using evidence-based treatment services and identifying means by which to increase the match between their perceived treatment needs and available treatments.30,31
Finally, although women had a higher mean age of first NMPOU and a lower prevalence of PO abuse than did men, the results suggest few gender differences in age of first abuse or dependence symptoms, or in duration of the longest episode. These findings imply that women with an opioid use disorder might be as problematic as men with an opioid use disorder in opioid use behaviors. Indeed, recent studies have shown that women with opioid use problems have a greater level of mental health problems (eg, depression, anxiety) and health-related disability than men, indicating gender differences in manifestations of psychopathology and gender-specific needs for clinical assessment and treatment planning.12,19,31
Study limitations and strengths
These findings should be interpreted in light of their limitations. The NESARC relies on respondents’ self-reports, which may be influenced by under-reporting and memory errors. For example, age of occurrences of various events all relied on respondents’ self-reports; these numbers (eg, an interval between two events) should be considered as estimates only. Similarly, POUDs and HUDs are based on respondents’ self-reports to standardized survey questions operationalized for DSM-IV abuse and dependence criteria. These disorders had not been validated by clinicians, and they represent cross-sectional survey-based estimates, not clinical diagnoses. In addition, a small but high-risk group of the US population, including homeless, hospitalized, incarcerated adults, was not covered by the survey. These findings cannot be applied to these excluded subgroups. Adults who are severely affected by substance use problems are unlikely to participate in the survey. POs and heroin are also associated with the highest rate of drug-related overdose or mortality,2,17 events that are not captured by a household survey. Thus, these results may underestimate abuse and dependence episodes but overestimate remission rates, as individuals who were most affected by heroin or PO use (eg, institutionalized, hospitalized, polysubstance opioid/heroin users) and deceased PO or heroin users are excluded (ie, biased due to a higher survival rate of less problematic heroin/PO users compared with severe or polysubstance heroin/PO users).
Further, the small sample size of heroin users excludes detailed comparisons of abuse and dependence patterns for users of POs only, heroin only, and both POs and heroin, and it limits the significance of differences found between heroin users and NMPOUs. Lastly, the analyses did not address the progression from abuse to dependence, as each was assessed separately. Both conditions are likely to be constantly intertwined, especially among those with heroin or PO dependence. For example, the results show that most adults with PO (82%) or heroin (98%) dependence also had PO or heroin abuse, respectively, whereas a comparatively low proportion of adults with PO (21%) or heroin (44%) abuse also had PO or heroin dependence, respectively.
Nonetheless, the NESARC is a large psychiatric survey of a nationally representative sample of American adults that provides perhaps the most comprehensive data set regarding PO and heroin abuse and dependence available for this research (ie, individuals with drug dependence were not left out of assessments of abuse due to the presence of dependence on the drug in question).32 The large sample also comprises geographically diverse sociodemographic groups across the US, which makes these findings more generalizable than findings from a convenience sample. Given the lack of course-related information on POUDs and their differences from HUDs, this study makes a timely contribution by presenting patterns of course-related features for POUDs and HUDs.
Conclusion
This study, using data from a national survey of psychiatric disorders, suggests differences in the prevalence and course-related patterns of opioid use disorders between heroin users and nonmedical PO users. Individuals who used heroin were more likely to have abuse or dependence (63%) than individuals who used nonmedical POs (30%). Furthermore, individuals with a HUD tended to experience a pattern of particularly lengthy episodes of abuse or dependence. Although periodic remission without substance abuse treatment occurs commonly, the chronic nature of drug use problems points toward a need for more focused research in order to pinpoint contextual and cognitive factors that promote effective use of evidence-based treatments to mitigate adverse health consequences and improve the quality of life of affected individuals. In conclusion, repeated remissions from multiple abuse or dependence episodes appear to be the rule rather than the exception; however, it takes a long time that is filled with many opportunities for adverse events that treatment can help prevent.
Acknowledgments
This work was made possible by research grants from the US National Institute on Drug Abuse of the National Institutes of Health (DA019623, DA027503, and DA019901 to L-T Wu; DA017009 and DA013043 to GE Woody). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. NESARC was sponsored and conducted by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health, with supplemental support from the National Institute on Drug Abuse. We thank Amanda McMillan for her editorial assistance.
Footnotes
Disclosure
GE Woody is a member of the Research on Adverse Drug Events and Reports (RADARS) postmarketing study external advisory group, whose job is to assess abuse of prescription medications. Denver Health administers RADARS, and nine pharmaceutical companies currently support its work. The other authors have no conflicts of interest to disclose. P Mannelli has received support from the following: AstraZeneca, Bristol-Myers Squibb, Cephalon, Inc., Forest, GlaxoSmithKline, Janssen, Jazz Pharmaceuticals, King Pharmaceutical, Lundbeck, McNeil Consumer and Specialty, Merck, Organon, Orphan Medical, Pfizer, Reckitt Benckiser and Titan.
References
- 1.Cai R, Crane E, Poneleit K, Paulozzi L. Emergency department visits involving nonmedical use of selected prescription drugs – United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2010;59(23):705–709. [PubMed] [Google Scholar]
- 2.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration . Results from the 2009 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2010. [Google Scholar]
- 4.Centers for Disease Control and Prevention Unintentional drug poisoning in the United States 2010Julyhttp://www.cdc.gov/HomeandRecreationalSafety/pdf/poison-issue-brief.pdfAccessed February 28, 2011
- 5.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 6.Arfken CL, Johanson CE, di Menza S, Schuster CR. Expanding treatment capacity for opioid dependence with office-based treatment with buprenorphine: national surveys of physicians. J Subst Abuse Treat. 2010;39(2):96–104. doi: 10.1016/j.jsat.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Fischer B. Illicit opioid use in the 21st century: witnessing a paradigm shift. Addiction. 2007;102(4):499–501. doi: 10.1111/j.1360-0443.2006.01738.x. [DOI] [PubMed] [Google Scholar]
- 8.Rosenblum A, Parrino M, Schnoll SH, et al. Prescription opioid abuse among enrollees into methadone maintenance treatment. Drug Alcohol Depend. 2007;90(1):64–71. doi: 10.1016/j.drugalcdep.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Wu LT, Ling W, Burchett B, et al. Gender and racial/ethnic differences in addiction severity, HIV risk, and quality of life among opioid-dependent patients: results from the Clinical Trials Network. Subst Abuse Rehabil. 2010;1:13–22. doi: 10.2147/SAR.S15151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore BA, Fiellin DA, Barry DT, et al. Primary care office-based buprenorphine treatment: comparison of heroin and prescription opioid dependent patients. J Gen Intern Med. 2007;22(4):527–530. doi: 10.1007/s11606-007-0129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sigmon SC. Characterizing the emerging population of prescription opioid abusers. Am J Addict. 2006;15(3):208–212. doi: 10.1080/10550490600625624. [DOI] [PubMed] [Google Scholar]
- 12.Wu LT, Woody GE, Yang C, Blazer DG. Subtypes of nonmedical opioid users: results from the national epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2010;112(1–2):69–80. doi: 10.1016/j.drugalcdep.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grant BF, Dawson DA. Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Res Health. 2006;29:74–78. [PMC free article] [PubMed] [Google Scholar]
- 14.Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorders and Associated Disabilities Interview Schedule IV (AUDADIS IV): reliability of alcohol consumption, tobacco use, family history of depression, and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 15.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatr. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 16.Research Triangle Institute . SUDAAN User’s Manual, Release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2006. [Google Scholar]
- 17.Nyhlén A, Fridell M, Hesse M, Krantz P. Causes of premature mortality in Swedish drug abusers: a prospective longitudinal study 1970–2006. J Forensic Leg Med. 2011;18(2):66–72. doi: 10.1016/j.jflm.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Wu LT, Woody GE, Yang C, Blazer DG. How do prescription opioid users differ from users of heroin or other drugs in psychopathology: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Addict Med. 2011;5(1):28–35. doi: 10.1097/ADM.0b013e3181e0364e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cicero TJ, Lynskey M, Todorov A, et al. Co-morbid pain and psychopathology in males and females admitted to treatment for opioid analgesic abuse. Pain. 2008;139(1):127–135. doi: 10.1016/j.pain.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 20.Cunningham JA. Untreated remissions from drug use: the predominant pathway. Addict Behav. 1999;24(2):267–270. doi: 10.1016/s0306-4603(98)00045-8. [DOI] [PubMed] [Google Scholar]
- 21.Klingemann H, Sobell MB, Sobell LC. Continuities and changes in self-change research. Addiction. 2010;105(9):1510–1518. doi: 10.1111/j.1360-0443.2009.02770.x. [DOI] [PubMed] [Google Scholar]
- 22.Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98(7):901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- 23.Cunningham JA, Blomqvist J, KoskiJannes A, Cordingley J. Maturing out of drinking problems: perceptions of natural history as a function of severity. Addict Res Theory. 2005;13:79–84. [Google Scholar]
- 24.Carballo JL, Fernández-Hermida JR, Sobell LC, et al. Differences among substance abusers in Spain who recovered with treatment or on their own. Addict Behav. 2008;33(1):94–105. doi: 10.1016/j.addbeh.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 25.Nyamathi A, Longshore D, Galaif ER, Leake B. Motivation to stop substance use and psychological and environmental characteristics of homeless women. Addict Behav. 2004;29(9):1839–1843. doi: 10.1016/j.addbeh.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 26.Connock M, Juarez-Garcia A, Jowett S, Frew E, et al. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess. 2007;11(9):1–171. doi: 10.3310/hta11090. iii–iv. [DOI] [PubMed] [Google Scholar]
- 27.Gibson A, Degenhardt L, Mattick RP, et al. Exposure to opioid maintenance treatment reduces long-term mortality. Addiction. 2008;103(3):462–468. doi: 10.1111/j.1360-0443.2007.02090.x. [DOI] [PubMed] [Google Scholar]
- 28.Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: a meta-analysis. Addiction. 1998;93(4):515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- 29.McCarty D, Perrin NA, Green CA, et al. Methadone maintenance and the cost and utilization of health care among individuals dependent on opioids in a commercial health plan. Drug Alcohol Depend. 2010;111(3):235–240. doi: 10.1016/j.drugalcdep.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slutske WS. Why is natural recovery so common for addictive disorders? Addiction. 2010;105(9):1520–1521. doi: 10.1111/j.1360-0443.2010.03035.x. discussion 1524. [DOI] [PubMed] [Google Scholar]
- 31.Smith BD, Marsh JC. Client-service matching in substance abuse treatment for women with children. J Subst Abuse Treat. 2002;22(3):161–168. doi: 10.1016/s0740-5472(02)00229-5. [DOI] [PubMed] [Google Scholar]
- 32.Grant BF, Compton WM, Crowley TJ, et al. Errors in assessing DSM-IV substance use disorders. Arch Gen Psychiatry. 2007;64(3):379–380. doi: 10.1001/archpsyc.64.3.379. author reply 381–382. [DOI] [PubMed] [Google Scholar]