Abstract
Excess collagen deposition occurs in pulmonary fibrosis. A new study suggests that collagen overproduction may originate from cells derived from bone marrow precursors rather than parenchymal lung fibroblasts .
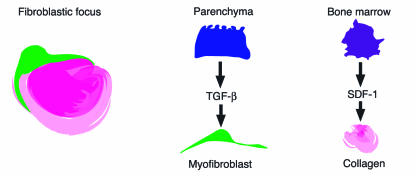
Idiopathic pulmonary fibrosis (IPF) is a devastating disorder with no effective treatment, which insidiously advances to airspace obliteration and death. The mean survival time following diagnosis is less than 5 years. Pathologically, the disease is characterized by chronic inflammation and exuberant collagen production within the lung (1). Survival can be predicted by the extent of fibroblastic foci (Figure 1) present at the time of lung biopsy (2). While the role of inflammation in IPF is less clear, inflammatory mediators, particularly TGF-β, are presumed to drive the fibrotic process. Myofibroblasts, a distinguishing feature of fibroblastic foci (3), are thought to arise from local activation of parenchymal fibroblasts by TGF-β and are historically considered to be the primary collagen-producing cell in fibrotic lesions (3, 4).
Figure 1.
Origin of fibroblastic foci. Fibroblastic foci, sites of active collagen synthesis, are the pathologic hallmark of pulmonary fibrosis. The traditional view is that cytokine secretion by epithelial and inflammatory cells induces parenchymal lung fibroblasts to overproduce collagen and to differentiate into myofibroblasts. Several recent studies indicate that bone marrow–derived cells can engraft into lung tissue and produce collagen. Bone marrow–derived cells may be recruited to the lung by chemokines generated by macrophages.
In this issue of the JCI, Hashimoto and colleagues (5) strongly force us to reconsider these fundamental concepts regarding the origin and phenotype of pathologic fibroblasts. In this study, the authors experimentally induced pulmonary fibrosis via bleomycin administration to mice that had been reconstituted with bone marrow derived from GFP transgenic mice. Thus, in the reconstituted mice, cells derived from bone marrow precursors will express GFP, and resident cells will not. Most of the collagen-producing fibroblasts observed in the lungs of these mice were of bone marrow rather than of local origin. Interestingly, GFP-positive fibroblasts could not be induced by TGF-β to express α-smooth muscle actin. Therefore, the pathologic collagen-producing fibroblasts not only were bone marrow–derived but were incapable of transforming into myofibroblasts.
Is the bleomycin animal model comparable to IPF?
Of course, the validity of the proposition that collagen-producing cells in human IPF are bone marrow–derived depends on the degree to which the animal model used replicates the human disease. Bleomycin induces lung epithelial cell death, followed by acute neutrophilic influx, subsequent chronic inflammation, and parenchymal fibrosis within 4 weeks of administration to susceptible strains of mice (6). In some ways, these changes mimic adult respiratory distress syndrome better than pulmonary fibrosis. However, the model does replicate some key pathologic features of human IPF, including fibroproliferation within the lung parenchyma, and hence pathologic mechanisms discerned in the mouse are worthy of consideration in humans. Furthermore, the clinical diagnosis of IPF is made late in the disease course when lung function is already half of that which existed prior to disease. Hence, causative factors and early natural history of IPF are largely unknown, making it a difficult disease to model.
Bone marrow–derived stem cells
Recent literature indicates that the pluripotency of bone marrow–derived cells extends further than classic hematopoietic differentiation (Figure 2). Studies have shown that bone marrow–derived stromal cells (7) and hematopoietic precursors (8) engraft and become structural cells, including fibroblasts, particularly following tissue injury. In fact, a unique population of collagen-expressing cells derived from hematopoietic precursors termed “fibrocytes” has been described (9, 10) and is likely the bone marrow cell population from which the GFP-positive cells in the lungs of bleomycin-treated mice originate. Moreover, fibrocytes express the chemokine receptors CXCR4 and CCR7 and migrate in vitro in response to their corresponding ligands, stromal cell–derived factor-1 (SDF-1) and secondary lymphoid-tissue chemokine (SLC) (10). Hashimoto et al. demonstrated that levels of SDF-1 and SLC are increased in the lung following bleomycin treatment (5), indicating that these chemokines also may be the in vivo signals that recruit bone marrow–derived fibroblasts to the lung. In another study of radiation-induced fibrosis (11), influx of bone marrow–derived macrophages preceded that of bone marrow–derived fibroblasts, leading the authors to speculate that these macrophages may be the source of SDF-1, SLC, or other substances that recruit fibroblast precursors from the bone marrow.
Figure 2.
Bone marrow cell populations. (a) Cross section of tubular bone showing the structure of bone marrow. Hematopoietic spaces are organized into cords by stromal cells (green lines) and contain distinct foci of developing erythroid and granulocytic cells interspersed among immature hematopoietic precursors. Mature blood cells enter the circulation by migrating across the marrow sinus endothelium. (b) Two populations of stem cells may be isolated from bone marrow. Mesenchymal stem cells, isolated from marrow stroma, adhere to tissue culture plasticware and have been shown to have the potential to differentiate into osteoblasts, adipocytes, and chondrocytes. Hematopoietic stem cells, which do not adhere to tissue culture plasticware, not only have the capacity to produce mature blood cells but also have been shown to engraft into liver, lung, kidney, heart, skeletal muscle, pancreas, and gastrointestinal tract. Fibrocytes, defined by the cell surface expression of collagen I, CD11b, CD13, CD34, CD45RO, MHC class II, and CD86, express the same chemokine receptors, CXCR4 and CCR7, as the collagen I–positive, GFP-positive cells in bleomycin-induced fibrotic lesions.
Other investigators have systemically administered mesenchymal stem cells to bleomycin-treated mice (12, 13). In these studies, cells that engrafted into lung tissue displayed epithelial characteristics. The expression of epithelial markers by GFP-positive cells was not assessed by Hashimoto et al. (5), but it is intriguing to speculate that the GFP-positive, collagen-producing cells underwent epithelial-mesenchymal transition (14). Alternatively, the isolation and culture of bone marrow cells prior to reconstitution may have predisposed them to an epithelial phenotype. In any event, understanding mechanisms of engraftment will be important as clinical applications of bone marrow stem cell therapy are explored.
Potential for stem cell therapy in the lung
Finally, Phan et al. (5) should be particularly congratulated because they had previously provided critical data (4) lending support to the previous paradigm that is now contested. Scientific truth is an elusive concept that we hope to achieve as new techniques are utilized and fresh hypotheses tested. Often we shift directions and must revise or abandon concepts once cherished. Although the fibroblast clearly remains a pathologic player in fibrosis (for now), its origin and properties must be reevaluated. The clinical implications of these findings are significant; for example, we might now consider bone marrow stem cell therapy to correct structural alterations in the lung. Translation of our understanding of disease pathogenesis into clinical practice will bring us closer to our real goal — improving the lives of our patients and ultimately curing disease. With the publication of this study, IPF patients may someday breathe more easily.
Acknowledgments
The authors thank Jeffery Kutok for providing the mouse bone marrow sections used in Figure 2.
Footnotes
See the related article beginning on page 243.
Conflict of interest: The authors have declared that no conflict of interest exists.
Nonstandard abbreviations used: idiopathic pulmonary fibrosis (IPF); stromal cell–derived factor-1 (SDF-1); secondary lymphoid tissue chemokine (SLC).
References
- 1.Gross TJ, Hunninghake GW. Idiopathic pulmonary fibrosis. N. Engl. J. Med. 2001;345:517–525. doi: 10.1056/NEJMra003200. [DOI] [PubMed] [Google Scholar]
- 2.King TE, Jr, et al. Idiopathic pulmonary fibrosis: relationship between histopathologic features and mortality. Am. J. Respir. Crit. Care Med. 2001;164:1025–1032. doi: 10.1164/ajrccm.164.6.2001056. [DOI] [PubMed] [Google Scholar]
- 3.Kuhn C, McDonald JA. The roles of the myofibroblast in idiopathic pulmonary fibrosis. Ultrastructural and immunohistochemical features of sites of active extracellular matrix synthesis. Am. J. Pathol. 1991;138:1257–1265. [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang K, Rekhter MD, Gordon D, Phan SH. Myofibroblasts and their role in lung collagen gene expression during pulmonary fibrosis. A combined immunohistochemical and in situ hybridization study. Am. J. Pathol. 1994;145:114–125. [PMC free article] [PubMed] [Google Scholar]
- 5.Hashimoto N, Jin H, Liu T, Chensue SW, Phan SH. Bone marrow–derived progenitor cells in pulmonary fibrosis. J. Clin. Invest. 2004;113:243–252. doi:10.1172/JCI200418847. doi: 10.1172/JCI18847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schrier DJ, Kunkel RG, Phan SH. The role of strain variation in murine bleomycin-induced pulmonary fibrosis. Am. Rev. Respir. Dis. 1983;127:63–66. doi: 10.1164/arrd.1983.127.1.63. [DOI] [PubMed] [Google Scholar]
- 7.Prockop DJ. Marrow stromal cells as stem cells for nonhematopoietic tissues. Science. 1997;276:71–74. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- 8.Herzog EL, Chai L, Krause DS. Plasticity of marrow-derived stem cells. Blood. 2003;102:3483–3493. doi: 10.1182/blood-2003-05-1664. [DOI] [PubMed] [Google Scholar]
- 9.Bucala R, Spiegel LA, Chesney J, Hogan M, Cerami A. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol. Med. 1994;1:71–81. [PMC free article] [PubMed] [Google Scholar]
- 10.Abe R, Donnelly SC, Peng T, Bucula R, Metz CN. Peripheral blood fibrocytes: differentiation pathway and migration to wound sites. J. Immunol. 2001;166:7556–7662. doi: 10.4049/jimmunol.166.12.7556. [DOI] [PubMed] [Google Scholar]
- 11.Epperly MW, Guo H, Gretton JE, Greenberger JS. Bone marrow origin of myofibroblasts in irradiation pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 2003;29:213–224. doi: 10.1165/rcmb.2002-0069OC. [DOI] [PubMed] [Google Scholar]
- 12.Kotton DN, et al. Bone marrow-derived cells as progenitors of lung alveolar epithelium. Development. 2001;128:5181–5188. doi: 10.1242/dev.128.24.5181. [DOI] [PubMed] [Google Scholar]
- 13.Ortiz LA, et al. Mesenchymal stem cell engraftment in lung is enhanced in response to bleomycin exposure and ameliorates its fibrotic effects. Proc. Natl. Acad. Sci. U. S. A. 2003;100:8407–8411. doi: 10.1073/pnas.1432929100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwano M, et al. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J. Clin. Invest. 2002;110:341–350. doi:10.1172/JCI200215518. doi: 10.1172/JCI15518. [DOI] [PMC free article] [PubMed] [Google Scholar]