Abstract
Breast carcinoma is the most common nondermatologic cancer diagnosis in women. Common metastatic sites include lymph nodes, lung, liver, and bone. Breast carcinoma metastatic to the bladder has been reported only sporadically. Most patients were symptomatic breast cancer with evidence of disseminated disease at the time of diagnosis. Metastasis usually occurred many years after diagnosis, and the prognosis was poor. We report a case of breast caricinoma metastasizing to the urinary bladder and retroperitoneum, which presented initially with acute renal failure. Patient was treated with bilateral per cuteneous nephrostomies and chemotherapy. Starting from this clinical case we review the available literature on this issue. Patients with breast cancer presenting with urinary symptoms should be examined for possible bladder metastasis.
Keywords: Acute renal failure, breast cancer, metastasis, reteroperitoneum, urinary bladder
INTRODUCTION
Urinary bladder metastasis from solid tumors is rare and represents 2% of all bladder neoplasms.[1] Direct extension from the cervix, prostate and colon is not unusual but metastasis from a distant organ is extremely rare. Breast cancer represents as a primary site in about 2.5% cases of all metastatic bladder cancer.[1] Breast cancer commonly metastasizes to the lung, bone, liver, lymph nodes and skin; less frequently it involves the brain, adrenal glands, ovary, spleen, pancreas, kidney, thyroid and heart.[2] There are reports on unusual sites of breast cancer metastases; the urinary bladder and retroperitoneum is considered one of these unusual sites.
CASE REPORT
A 45-year-old premenopausal female patient presented with two months history of recurrent high-grade fever with chills, bilateral pedal edema and oliguria.
On examination bilateral pitting pedal edema was present. Blood investigation revealed serum creatinine of 8.76 mg% and total count was 19,000/cumm. Ultrasonography (USG) showed bilateral hydronephrosis and upper hydroureter. Patient was initially treated with bilateral Double J (DJ )stenting elsewhere. But due to persistent urinary tract infection and renal failure we removed DJ stents and bilateral nephrostomies were kept. Patient's nadir serum creatinine was 1.65 mg%.
Contrast enhanced computerized tomography (CECT ) was suggestive of irregular circumferential moderately enhancing thickening of urinary bladder with hypodense mass lesion in the retroperitoneum with bilateral hydroureteronephrosis [Figure 1]. Cystoscopy showed thick irregular bladder wall with no definitive mass lesion, so random bladder wall biopsies were taken. Biopsy was suggestive of undifferentiated adenocarcinoma [Figure 2].Immunohistochemistry was positive for cytokeratin, CK 7 and ER and negative for CK 20 and PR.
Figure 1.

Contrast enhanced computerized tomography suggestive of irregular circumferential moderately enhancing thickening of urinary bladder
Figure 2.
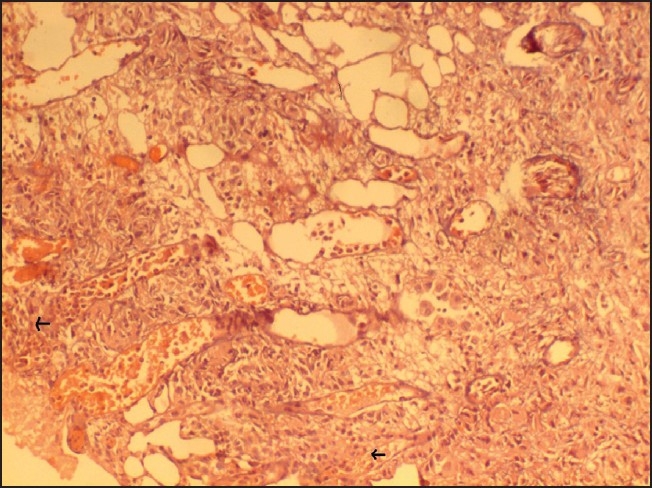
Histopathological examination of bladder biopsy (H and E, x 100) shows metastatic undifferentiated adenocarcinoma, arrow shows tumor cells
Subsequently, during a search for primary site of bladder metastasis, we found patient having right breast mass. True-cut biopsy from right breast mass was suggestive of invasive lobular carcinoma of breast (Nuclear Grade II).
Patient underwent chemotherapy in form of paclitexol and carboplatin. After two cycles of chemotherapy patient started passing urine per urethra and nephrostomy output decreased. So we clamped both the tubes for 48 h and removed both the nephrostomies. After nephrostomy removal patient's serum creatinine remained static at 1.6 mg% and USG showed no hydronephrosis. Patient died after six months due to metastatic disease.
DISCUSSION
Metastases to urinary bladder are rare, accounting for less than 2% of all bladder tumors, these are mostly found in advanced stages with peritoneal dissemination.[1] Information pertaining to bladder metastases is derived largely from autopsy studies, and known primary sites of origin in descending frequency are gastric cancer, malignant melanoma, breast and lung.[1] Potential mechanisms contributing to the appearance of secondary bladder tumors could be due to minute viable tumor emboli that pass through the pulmonary circulation without establishing a lung metastasis and subsequently reach the urinary bladder by hematogenous transport. Other possible routes are extension from retroperitoneal involvement or dissemination through the lymphatic or arterial circulation.[2]
The relative infrequency of primary adenocarcinoma of the bladder causes the dilemma whether bladder adenocarcinoma represents a primary or secondary process.[1] Mostofi et al, have proposed several guidelines for such differentiation.[3] If the adjacent mucosa contains polypoid formation, Brunn's nests, or glandular or mucous metaplasia, a primary bladder lesion is likely. Immunochemistry staining for various markers is routinely used in diagnosis of undifferentiated tumor. Cytokeratin, CK-7, CK-18, CK-19, CK-20 are useful screening markers for the recognition of epithelial differentiation. Other specific markers that are commonly used are ER/ PR for endometrial and breast carcinoma, CA 19-9 for pancreatobiliary malignancy, prostate specific antigen (PSA) for prostate, thyroglobulin for thyroid, uroplakin III for urothelium, and HepPar I for hepatocellular.[4]
In a retrospective study Bates and Baithun found 282 secondary urinary bladder metastases in a series of 6289 bladder tumors (about 4.5% of all bladder tumors detected). Seven cases of primary breast cancer were found; bladder metastases were detected post-mortem in six of these seven cases and all of them had metastasized widely.[1]
Treatment of metastatic breast cancer is chemotherapy and hormonal therapy. Postobstructive renal failure in breast cancer patients can be treated easily by endoureteral catheterization or percutaneous nephrostomy which allows rapid normalization of renal function in most cases and further administration of effective systemic chemotherapy.
Survival after the onset of distant metastases is relatively short, Poulakis et al. in 2001 reported a patient with breast cancer and urinary bladder involvement still alive at five years from diagnosis.[5] Hence, appropriate treatment and follow-up may improve the prognosis of patients with bladder metastases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bates AW, Baithun SI. Secondary neoplasms of the bladder are histological mimics of nontransitional cell primary tumours: clinicopathological and histological features of 282 cases. Histopathology. 2000;36:32–40. doi: 10.1046/j.1365-2559.2000.00797.x. [DOI] [PubMed] [Google Scholar]
- 2.Pontes JE, Oldford JR. Metastatic breast carcinoma to the bladder. J Urol. 1970;104:839–42. doi: 10.1016/s0022-5347(17)61848-2. [DOI] [PubMed] [Google Scholar]
- 3.Mostofi FK, Thompson RV, Dean AL., Jr Mucous adenocarcinoma of the urinary bladder. Cancer. 1955;8:741–58. doi: 10.1002/1097-0142(1955)8:4<741::aid-cncr2820080417>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 4.Bahrami A, Truong LD, Ro JY. Undifferentiated tumor: true identity by immunohistochemistry. Arch Pathol Lab Med. 2008;132:326–48. doi: 10.5858/2008-132-326-UTTIBI. [DOI] [PubMed] [Google Scholar]
- 5.Poulakis V, Witzsch U, De Vries R, Becht E. Metastatic breast carcinoma to the bladder: 5- year followup. J Urol. 2001;165:905. [PubMed] [Google Scholar]


