Abstract
Introduction:
Insertion of a double-J (JJ) stent is a common procedure often carried out in the retrograde route by the urologists and the antegrade route by the radiologists. Reported complications include stent migration, encrustation, and fracture. Extra-anatomic placement of an antegrade JJ stent is a rare but infrequently recognized complication.
Materials and Methods:
We performed a retrospective audit of 165 antegrade JJ stent insertions performed over three consecutive years by a single interventional radiologist. All renal units were hydronephrotic at the time of nephrostomy. All procedures were performed under local anaesthetic with antibiotic prophylaxis.
Results:
Antegrade stent insertion was carried out simultaneously at the time of nephrostomy in 55 of the 165 cases (33%). The remainder were inserted at a mean of 2 weeks following decompression. In five (3%) patients, who had delayed antegrade stenting following nephrostomy, the procedure was complicated by silent ureteric perforation and an extra-anatomic placement of the stent. These complications had delayed manifestations, which included two retroperitoneal abscesses, a pelvic urinoma, a case each of ureterorectal fistula, and ureterovaginal fistula. Risk factors for ureteric perforation include previous pelvic malignancy, pelvic surgery, pelvic radiation, and a history of ureteric manipulation.
Conclusion:
Antegrade ureteric JJ stenting is a procedure not without complications. Extra-anatomic placement of the antegrade stent is a hitherto the infrequently reported complication but needs a high index of suspicion to be diagnosed. Risk factors for ureteric perforation at the time of stent insertion have to be considered to prevent this potential complication.
Keywords: Antegrade, complications, stent, ureter
INTRODUCTION
Ureteric obstruction can be caused by a variety of conditions ranging from stones to malignancy and strictures. Ureteral stents are used to bypass the point of obstruction and restore the continuity of the urinary tract, and can be inserted by the retrograde or antegrade routes.
Antegrade ureteric stenting is minimally invasive, uses local anesthetic with or without sedation and has a higher success rate of insertion.[1] However, the complications of insertion are not widely reported and we aimed to evaluate extra-anatomic complications of antegrade JJ stent placement in our hospital and review the potential risk factors.
MATERIALS AND METHODS
A retrospective review was carried out of 165 antegrade JJ stent insertions performed over 3 years by a single interventional radiologist. Prior to nephrostomy, all renal units were confirmed by ultrasound scan to have hydronephrosis. The procedure was performed with local anesthetic infiltration with antibiotic prophylaxis. Parenteral sedation was administered only if required. In most cases, the initial nephrostomy were performed under the guidance of ultrasound. Under fluoroscopy guidance, a nephrostogram was performed routinely in all patients to determine the anatomy of the ureter. Simultaneous antegrade insertion of ureteric JJ stent at the time of nephrostomy was decided on the clinical needs of the patient and the local pathology.
RESULTS
Simultaneous insertion of the ureteric stent at the nephrostomy was carried out in 55 of the 165 cases (33%). In the remaining cases, ureteric stent was inserted at a mean of 2 weeks following insertion of the nephrostomy. In five (3%) patients, who had delayed antegrade stenting following nephrostomy, the procedure was complicated by silent ureteric perforation and an extra-anatomic placement of the stent. These cases are discussed in detail below.
Case 1
A 67-year-old man presented as an emergency with large bowel obstruction. Laparotomy revealed locally advanced sigmoid carcinoma and a dilated left ureter. A sigmoid colectomy was performed with the formation of end colostomy and T-tube decompression of the left ureter. Cystoscopy revealed extension of the colonic tumor into the bladder, and retrograde studies on the left side demonstrated narrowing of lower ureter. An attempt to pass a guide wire through the stricture was unsuccessful. An antegrade attempt resulted in the guide wire passing through the ureter into the rectal stump. A JJ stent was, therefore, passed down to the rectum to provide an alternative internal drainage. On subsequent follow-up, he developed right-sided hydronephrosis, due to the compression from enlarged lymph nodes, and needed stent placement. He continued to pass urine both urethrally and rectally without the loss of continence. He had periodic change of stents, cystoscopically and proctoscopically. His renal function remained stable for 2 years until he died of progressive disease having received palliative chemotherapy and radiotherapy. This case has been published by the authors.[2]
Case 2
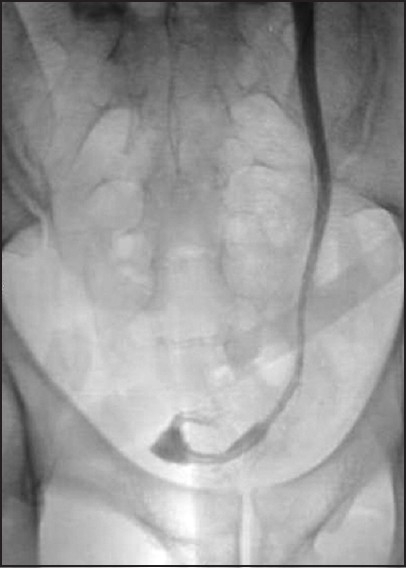
A 54-year-old man presenting with constipation had a CT scan that revealed a growth in the sigmoid colon infiltrating into the bladder. Laparotomy revealed a large tumor arising from the sigmoid colon infiltrating left lateral wall of the bladder and the lower end of the left ureter. Anterior resection with primary anastomosis, partial cystectomy, and excision of lower end of the left ureter with reimplantation over a JJ stent were carried out. The ureteric JJ stent was removed at six postoperative weeks. IVU carried out at 3 months showed delayed opacification of left kidney with moderate hydronephrosis. Left percutaneous nephrostomy with nephrostogram revealed a tight stricture at the lower end of the ureter [Figure 1].
Figure 1.

Nephrostogram demonstrating a tight stricture at the lower end of left ureter
A guide wire was negotiated through the stricture and a JJ stent was placed over it. Initial X-ray suggested that the lower end might have been in the bladder, but subsequent films cast a doubt that the stent might be extravesical in location [Figure 2].
Figure 2.
Nephrostogram suggesting that the lower end to be in the bladder
CT scan of the pelvis demonstrated the lower end of the stent to be posterior to the bladder wall. As the patient refused another open surgical exploration, a rendezvous procedure was planned. Cystoscopy did not show the lower end of the stent to be in the bladder and the left ureteric orifice could not be identified. Fluoroscopy demonstrated the stent to be posteroinferior to the bladder. It was then decided to resect down to the stent under fluoroscopic guidance. Methylene blue was injected through the nephrostomy to aid identify the area of resection. The stent was then identified in the perivesical fat [Figure 3].
Figure 3.
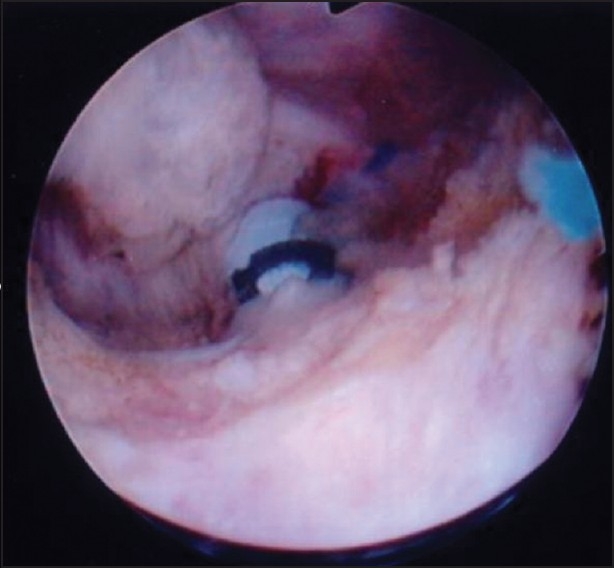
Resection of the bladder wall with demonstration of blue staining by methylene blue. The lower end of the stent in perivesical fat
A guide wire was passed through the old stent and a new stent was inserted. Nephrostogram on the seventh postoperative day showed free flow of dye into the bladder around the JJ stent through the neoureteric orifice. There was no evidence of leakage outside the bladder. Check cystoscopy subsequently revealed a nicely healed bladder with adequate caliber ureteric orifice.
Case 3
A 57-year-old man, a known case of hormone refractory carcinoma of prostate having received radical radiotherapy in the past, presented with severe irritative voiding bladder symptoms and constipation. Investigations revealed extensive infiltration by the prostate cancer occupying more than three quarters of the rectal lumen and involving the right ureter causing right hydronephrosis.
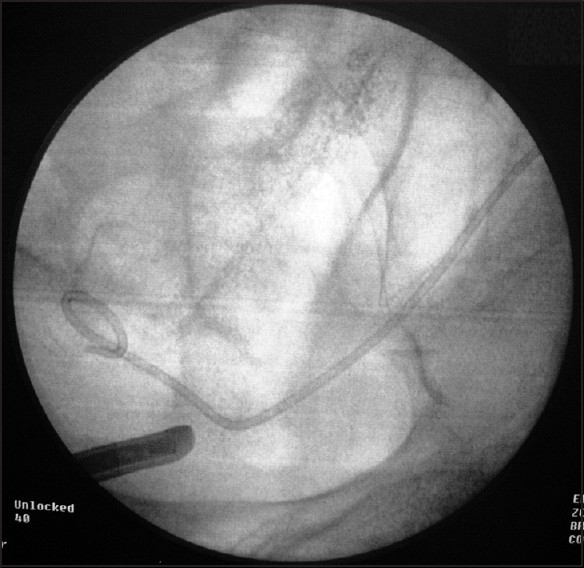
A right nephrostomy and antegrade insertion of JJ stent was performed. An informed decision was reached for urinary and bowel diversion. Ileal conduit urinary diversion and a diverting end colostomy were performed. On follow-up, he developed bilateral hydronephrosis for which he had bilateral nephrostomy insertion. The nephrostogram demonstrated narrowing at the ureteroileal anastomosis. Bilateral antegrade JJ stenting was, therefore, carried out. However, there was increased output from the drain and progressive abdominal distension. Ultrasound demonstrated free intraperitoneal collection. Plain X-ray of the abdomen revealed an abnormal position of the left JJ stent that did not appear to be in the ileal conduit [Figure 4].
Figure 4.

Plain X-ray of abdomen showing an abnormal position of the lower end of the left JJ stent
Conduitoscopy revealed the presence of lower end of the right ureteric stent, but the lower end of the left ureteric stent was not seen. However, on closer inspection of the anastomosis the left stent was seen going across the anastomosis into the peritoneum. The stent was gently grabbed with a grasping forceps and brought into the conduit. Covering nephrostomy was left in situ for 6 weeks. The output from the intra-abdominal drain started to decrease and was subsequently removed. On follow-up the patient had a good quality of life regarding his bowel and urinary symptoms.
Case 4
A 69-year-old lady presented with the retention of urine with a residual volume of 2 L and renal impairment. She had in the past undergone partial cystectomy and received radiotherapy for muscle invasive bladder cancer. Investigations revealed left hydronephrosis and hydroureter. Left nephrostomy was inserted and nephrostogram revealed stricture in the lower end of the left ureter [Figure 5].
Figure 5.

Nephrostogram showing stricture at the lower end of the left ureter
Left antegrade JJ stent insertion was thus carried out. She discharged with the advice of clean intermittent self catheterization as the creatinine stabilized at 274 mmol/L. Left JJ stent was removed after 6 weeks with flexible cystoscopy. Follow-up IVU demonstrated the persistence of the stricture. She, therefore, had re-insertion of the JJ stent in the antegrade manner on the left side. There was difficulty in managing to pass the guide wire across the strictured segment. However, it passed across the stricture and the lower end of the stent appeared to be in the bladder [Figure 6].
Figure 6.

Plain X-ray KUB showing the lower end of the stent in the bladder region
Postoperatively, she developed leakage of urine from the vagina. Cystoscopy did not reveal obvious fistulous tract, but the lower end of the left ureter or the ureteric orifice could not be identified. Fluoroscopy revealed extra-anatomic location of the stent [Figure 7]. With a probable diagnosis of ureterovaginal fistula, a nephrostogram was performed that showed the JJ stent to have passed across the stricture but the exact location of the lower end could not be definitely identified [Figure 8].
Figure 7.
Fluoroscopic examination at the time of cystoscopy demonstrating extra-anatomic location of JJ stent
Figure 8.

Left nephrostogram showing the dye to be stopping at the site of stricture
Although the dye was seen entering the bladder, the course of the lower end of the stent was not in the line of the ureter. The escape of dye into the vagina was also seen demonstrating the presence of vaginourinary fistula [Figure 9]. To improve the patient's quality of life, with informed decision, ileal conduit urinary diversion was carried out. The lower end of the left JJ stent was found to be in the perivesical tissue with a lot of necrotic debris surrounding it. Postoperative period was uneventful and she has been symptom free with no further deterioration of renal function on follow-up.
Figure 9.
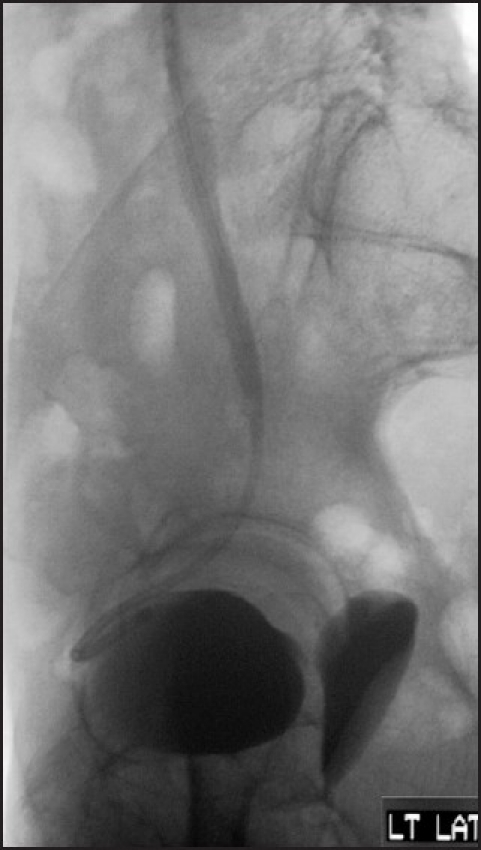
Unusual anterior location of the lower end of the JJ stent and demonstration of dye in the vagina
Case 5
A 71-year-old man underwent cystoprostatectomy and ileal conduit urinary diversion for muscle invasive bladder cancer. However, 3 months later he was admitted with fever with chills and rigors. Investigations revealed bilateral hydronephrosis for which B/L nephrostomy and antegrade stenting was carried out. Nephrostogram showed narrowing of the right ureteroileal anastomosis [Figure 10]. He responded well to the treatment with intravenous antibiotics. He further developed episodes of fever, malaise, and weight loss. Conduitoscopy revealed the presence of the lower end of left JJ stent only. The lower end of the right JJ stent was not to be seen. Ultrasound revealed the lower end of right JJ stent to be lying in an abscess cavity in the retroperitoneum outside the ileal conduit [Figure 11]. On exploration, the lower end of the stent was indeed in an abscess cavity, which had involved the ureteroileal anastomosis. Revision of the ileal conduit was thus carried out. Postoperative recovery was uneventful. On follow-up, his renal function has remained stable with no evidence of obstruction at the ureteroileal anastomosis.
Figure 10.

Right nephrostogram showing narrowing of the uretero-ileal junction
Figure 11.
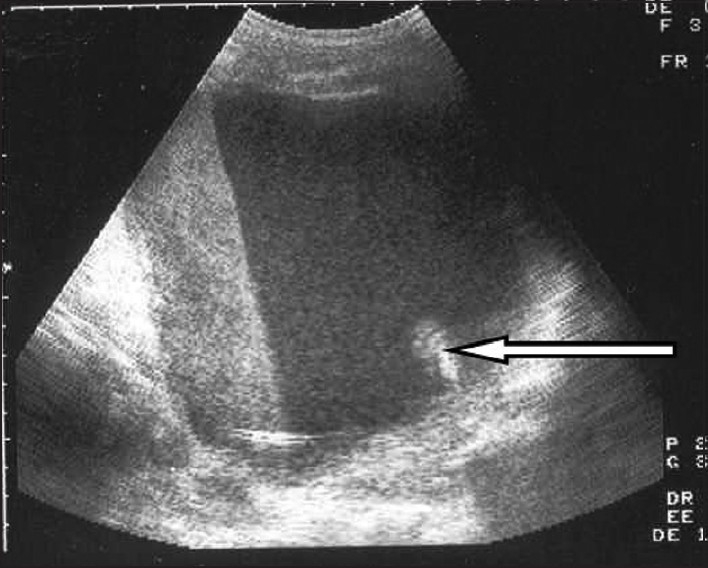
Ultrasound showing the presence of the lower end of the right JJ stent in the abscess cavity
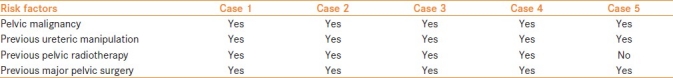
Analysis of risk factors
Risk factors associated with ureteric perforation was analyzed in the above cases and provided in Table 1.
Table 1.
Risk factors for perforation associated with each case
DISCUSSION
Since ureteric stents were first used in open surgery in the 1960s with the endoscopic placement of a straight silicone stent, the indications for stent insertion have increased and are routinely inserted in patients with ureteric obstruction.[3] The modern double pigtail stent has been around since 1978 and despite efforts to improve its biocompatibility to decrease the complications associated with an indwelling stent, its basic design has remained virtually the same.[4] Complications could either occur during insertion of the stent or due to the presence of the stent in situ.
While retrograde ureteric stenting is a one-stage procedure and has a negligible risk of hemorrhage, it often requires a general or spinal anesthetic and necessitates the use of operating theatre facilities.[1] Furthermore, situations may not be suitable for a retrograde procedure either due to anatomical hindrance or the patient's morbidity. A study of malignant ureteric obstruction in 30 patients found the success rate for retrograde stenting to be only 50%.[4]
Conversely, percutaneous antegrade ureteric stenting is more favorable in certain situations and can overcome some of the technical difficulties that prevent retrograde stent placement. Favorable success rates for the insertion have been reported ranging from 80% to 92%.[5–7] However, it is often a two-stage procedure, with an increased risk of hemorrhage at the point of insertion, and requires an experienced interventional radiologist.
While the complications at the time of insertion of the stent have not been widely reported, complications associated with long-term indwelling ureteric stent are well-documented and includes urinary tract infection, malposition and migration, inadequate relief of obstruction, encrustation, stent fracture, ureteral erosion or fistulization, and the forgotten stent. Bladder irritability due to the irritation by the lower end of the stent may occur in up to 80–90% of the patients.[8,9] Loin pain secondary to vesicorenal reflux is also a well-recognized undesirable symptom.[10] Studies have shown an overall decrease in the quality of life in patients with indwelling ureteral stent.[11]
Ureteric and vascular perforation at the time of insertion of JJ stent has been previously documented in the literature.[12] Vascular injury leading to arteriovenous fistula formation has also been documented.[13] Perforation of the artery leading to hemoperitoneum has also been documented at the time of insertion of the JJ stent. The authors caution about checking that the guide wire has been correctly preloaded in the spool before its placement up the ureter as inserting the wrong (nonfloppy) end may have serious implications.[14] Ureteral erosion or fistulization has also been documented with long-standing ureteral stent. Erosion into an arterial system is a potentially dangerous complication and a high degree of clinical suspicion is necessary if mortality is to be avoided.[15,16]
As in our series, pelvic cancer, previous major pelvic surgery, and radiotherapy to the pelvis appear to be the risk factors to the development of this complication. The above factors may contribute to ureteral ischemia. All the five patients had pelvic cancer surgery. Four out of the five patients had received pelvic radiotherapy. All the five patients had ureteric manipulation either in the form of JJ stenting or operation. Two of the patients had ureteroileal stricture formation. McIntyre et al. and Patricia et al. reported the risk of radiation-induced ureteric stricture to be relatively constant and approximately 0.15% per year for 25 years or more after radiation therapy for cancer of the cervix.[17,18] Radiation-induced submucosal fibrosis of the ureter has been observed but the exact mechanism is still poorly understood. Radical pelvic radiotherapy results have been shown to induce sinister changes in all the treated tissues by the release of cytokines and can predispose to superimposed bacterial reactions, resulting in chronic ischemia.[19–21]
The presence of the stent within a ureter adjacent to a pulsating vascular structure, either a normal vessel or graft, appears to be favorable for erosion to occur.[22] Malposition of the stent leading to the perforation of the ureter, collecting system, and penetration of the kidney parenchyma during placement, resulting in urinoma and hematoma formation, has been documented.[23]
CONCLUSION
The indications for ureteral stent placement have expanded significantly in the recent times. Ureteral stent placement is now considered a standard and indispensable urologic tool. Stents should be monitored while in place, promptly removed when no longer needed, and changed periodically if chronically indwelling.
Ureteric perforation at the time of stent insertion is a potential complication and the risk is increased in patients with pelvic malignancy, previous radiotherapy to the pelvis, history of ureteric manipulation, and in those patients who have had major pelvic surgery. Therefore more care should be taken in patients with these risk factors during the insertion of the stent. Unusual symptoms after insertion of the stent in such patients raise suspicion of ureteric perforation, and appropriate investigations should be carried out.
The operating physician is responsible for informing the patient of the indications, consequences, and complications associated with insertion of the stent. Failure to do so has obvious management and potential medicolegal implications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Adamo R, Saad W, Brown D. Management of Nephrostomy Drains and Ureteral Stents. Tech Vasc Interv Radiol. 2009;12:193–204. doi: 10.1053/j.tvir.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Mishra VC, Rao AR, Desai AR, Charig M, Karim OMA. A unique extra-anatomic urinary diversion. J Endourol. 2004;18:57–8. doi: 10.1089/089277904322836686. [DOI] [PubMed] [Google Scholar]
- 3.Zimskind PD, Fetter TR, Wilkerson JL. Clinical use of long-term indwelling silicone rubber ureteral splints inserted cystoscopically. J Urol. 1967;97:840–4. doi: 10.1016/S0022-5347(17)63130-6. [DOI] [PubMed] [Google Scholar]
- 4.Uthappa MC, Cowan NC. Retrograde or antegrade double-pigtail stent placement for malignant ureteric obstruction? Clin Radiol. 2005;60:608–12. doi: 10.1016/j.crad.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Evans PAM, Nisbet AP, Saxton HM. Antegrade ureteric stents in malignant disease. J Intervent Radiol. 1988;3:9–13. [Google Scholar]
- 6.Harding JR. Percutaneous antegrade ureteric stent insertion in malignant disease. J Roy Soc Med. 1993;86:511–3. [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma SD, Persad RA, Haq A. A review of antegrade stenting in the management of the obstructed kidney. Br J Urol. 1996;98:511–5. doi: 10.1046/j.1464-410x.1996.01673.x. [DOI] [PubMed] [Google Scholar]
- 8.Pollard SG, MacFarlane R. Symptoms arising from double-J ureteral stents. J Urol. 1988;139:37–8. doi: 10.1016/s0022-5347(17)42282-8. [DOI] [PubMed] [Google Scholar]
- 9.Bregg K, Riehle RA., Jr Morbidity associated with indwelling internal ureteral stents after shock wave lithotripsy. J Urol. 1989;141:510–2. doi: 10.1016/s0022-5347(17)40875-5. [DOI] [PubMed] [Google Scholar]
- 10.Mosli HA, Farsi HMA, Al-Zimaity F, Salem TR, Al-Zamsami MM. Vesicoureteral reflux in patients with double pigtail stents. J Urol. 1991;146:966–9. doi: 10.1016/s0022-5347(17)37976-4. [DOI] [PubMed] [Google Scholar]
- 11.Joshi HB, Stainthrope A, Keeley FX, Jr, MacDonagh R, Timoney AG. Indwelling ureteral stents: evaluation of quality of life to aid outcome analysis. J Endourol. 2001;15:151–4. doi: 10.1089/089277901750134421. [DOI] [PubMed] [Google Scholar]
- 12.Kidd RV, Confer DJ, Ball TP., Jr Ureteral and renal vein perforation with placement into the renal vein as a complication of the pigtail ureteral stent. J Urol. 1980;124:424–6. doi: 10.1016/s0022-5347(17)55480-4. [DOI] [PubMed] [Google Scholar]
- 13.Lalude AO, Conroy RM. Vascular complication of percutaneously placed pigtail ureteral stent. J Urol. 1983;130:553–4. doi: 10.1016/s0022-5347(17)51301-4. [DOI] [PubMed] [Google Scholar]
- 14.Chitale SV, Ho ET. Haemoperitoneum secondary to ureteric stenting. Int Urol Nephrol. 2002;34:197–8. doi: 10.1023/a:1023274514526. [DOI] [PubMed] [Google Scholar]
- 15.Reiner RJ, Conway GF, Threlkeld R. Ureteroarterial fistula. J Urol. 1975;113:24–25. doi: 10.1016/s0022-5347(17)59397-0. [DOI] [PubMed] [Google Scholar]
- 16.Smith RB. Ureteral common iliac artery fistula: a complication of internal double-J ureteral stent. J Urol. 1984;132:113. doi: 10.1016/s0022-5347(17)49490-0. [DOI] [PubMed] [Google Scholar]
- 17.McIntyre JF, Patricia JE, Levenback C, Oswald MJ. Ureteral stricture as a late complication of radiotherapy for stage 1B carcinoma of the uterine cervix. Cancer. 1995;75:836–43. doi: 10.1002/1097-0142(19950201)75:3<836::aid-cncr2820750315>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 18.Patricia JE, Levenback C, Wharton JT, Oswald MJ. Time course and incidence of late complications in patients treated with radiation therapy for FIGO stage IB carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys. 1995;32:1289–300. doi: 10.1016/0360-3016(95)00118-I. [DOI] [PubMed] [Google Scholar]
- 19.Langberg CW, Hauer-Jensen M, Sung CC, Kane CJM. Expression of fibrogenic cytokines in rat small intestine after fractionated irradiation. Radiother Oncol. 1994;32:29–36. doi: 10.1016/0167-8140(94)90446-4. [DOI] [PubMed] [Google Scholar]
- 20.Hasleton PS, Carr N, Schofield PF. Vascular changes in radiation bowel disease. Histopathology. 1985;9:517–34. doi: 10.1111/j.1365-2559.1985.tb02833.x. [DOI] [PubMed] [Google Scholar]
- 21.Taylor PM, Johnson RJ, Eddleston B, Hunter RD. Radiological changes in the gastrointestinal and genitourinary tract following radiotherapy for carcinoma of the cervix. Clin Radiol. 1990;41:165–9. doi: 10.1016/s0009-9260(05)80960-2. [DOI] [PubMed] [Google Scholar]
- 22.Bergqvist D, Parsson H, Sherif A. Arterio-ureteral fistula: a systematic review. Eur J Vasc Endovasc Surg. 2001;22:191–6. doi: 10.1053/ejvs.2001.1432. [DOI] [PubMed] [Google Scholar]
- 23.Dyer RB, Chen MY, Zagoria RJ, Regan JD, Hood CG, Kavanagh PV. Complications of Ureteral Stent Placement. Radiographics. 2002;22:1005–22. doi: 10.1148/radiographics.22.5.g02se081005. [DOI] [PubMed] [Google Scholar]


