Abstract
Varicocele is one of the most common causes of male infertility. Treatment options for varicoceles includes open varicocelectomy performed at various anatomical levels. Laparoscopic varicocelectomy has been established to be a safe and effective treatment for varicoceles. Robotic surgery has been introduced recently as an alternative surgical option for varicocelectomy. Microsurgical varicocelectomy has gained increasing popularity among experts in male reproductive medicine as the treatment of choice for varicocele because of its superior surgical outcomes. There is a growing volume of literature in the recent years on minimal invasive varicocele treatment with percutaneous retrograde and anterograde venous embolization/sclerotherapy. In this review, we will discuss the advantages and limitations associated with each treatment modality for varicoceles. Employment of these advanced techniques of varicocelectomy can provide a safe and effective approach aiming to eliminate varicocele, preserve testicular function and, in a substantial number of men, increase semen quality and the likelihood of pregnancy.
Keywords: Microsurgical varicocelectomy, varicocele embolization, varicoceles, varicocelectomy, sclerotherapy
INTRODUCTION
Male reproductive medicine is one of the fastest growing subspecialties in Urology. Advanced assisted reproductive technologies are becoming widely available in the recent years for the management of severe male factor infertility, and our understanding of their safety and efficacy has improved tremendously. Simultaneously, the literature on the various treatment options for male reproductive disorders such as varicoceles has grown significantly. Indeed, although controversies exist, most experts in male reproductive medicine agree that correction of clinically significant varicoceles in infertile men can enhance the male fertility status, leading to improved testicular function in testosterone production, enhanced semen profile, sperm chromatin integrity,[1,2] pregnancy rates through natural intercourse or reproductive outcomes through assisted reproductive technologies.[3–7]
The various aspects of the recent development in varicocele management also focus on the efficacies of various treatment options, ranging from open varicocele ligation at various anatomical levels, with or without the use of optical magnification, to percutaneous varicocele occlusion by embolization/sclerotherapy. In this publication, we will shed light on these various approaches through a review of selected literature on varicocele management in the recent years.
MANAGEMENT OF VARICOCELES
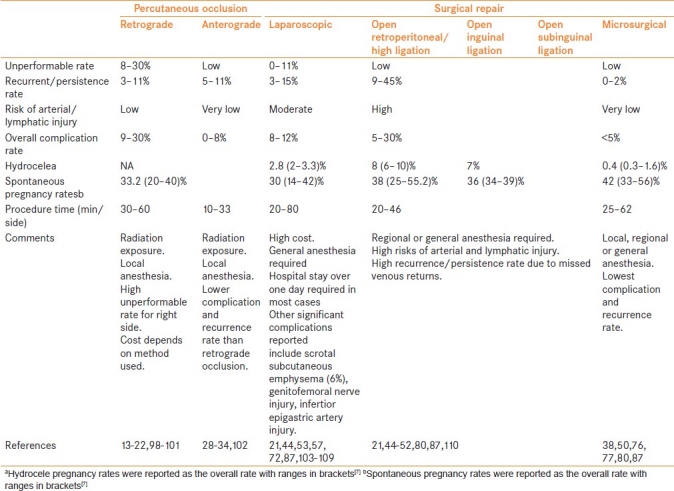
Varicocelectomy is by far the most commonly performed operation for the treatment of male infertility. The indications of varicocelectomy for clinically significant varicoceles include (1) infertility, particularly with impaired semen parameters or sperm quality, (2) hypogonadism, (3) scrotal pain, (4) testicular hypotrophy, particularly in the pediatric population and (5) aesthetic issues with large varicoceles. Treatment options for varicocele can be divided into two major categories[8]: (1) percutaneous occlusion, by intravenous injection of various materials to occlude the varicoceles and (2) surgical ligation or clipping of the varicoceles to prevent venous reflux. Table 1 summarizes the pros and cons of various methods of varicocele repair.{Table 1}
Table 1.
Comparison of the common methods used for the treatment of varicoceles
Percutaneous varicocele occlusion
Percutaneous embolization of the gonadal vein was originally described over three decades ago.[9,10] Currently, percutaneous embolization procedures for varicoceles include the traditional retrograde occlusion and the more recently described anterograde technique. In the retrograde technique, the right femoral vein is punctured to insert an angiocatheter to gain access to the internal spermatic vein via the inferior vena cava and the left renal vein. On confirming the anatomy and the presence of reflux in the testicular vein, it is occluded in a retrograde fashion (i.e., against the natural direction of the internal spermatic venous return). Percutaneous occlusion is a suitable treatment option for persistent/recurrent varicoceles post surgical repair.[11] The use of imaging techniques to identify the cause of varicocele recurrence allows accurate venous occlusion while eliminating the need for a difficult dissection of the fibrous adhesions from previous surgery. Inexpensive sclerosing agents are commonly used for retrograde occlusion. One significant advantage of retrograde percutaneous embolization is that post-procedure, the return to normal activities is faster compared with other varicocele treatments, as there is no incision and splitting of the abdominal muscles involved. Newer embolization techniques using sclerosing foam, which has the advantage of increasing the contact between the sclerosing agent and the vessel wall and decreasing the extent of dilution of the sclerosing agent by blood within the vessel,[12] or employing more expensive materials, such as detachable coils[13,14] and occlusive balloons,[15] have been described.
Complications, including contrast reaction, flank pain, migration of embolizing materials, infection, thrombophlebitis, arterial puncture and hydroceles, occur at a significant rate with embolization (9–30%).[13–22] Radiation exposure during fluoroscopy is a potential concern, given that the procedure may be performed on healthy young males with normal life expectancy and desire for fertility.[23] Another major criticism of the retrograde occlusive procedure is its high unperformable rate (8-30%),[13–22,24,25] particularly for right-sided varicoceles, due to the venous anatomical variations leading to difficulties in gaining proper venous access. Alternative venous access, including right transbrachial and internal jugular approaches, have been described with success to reach the right and left internal spermatic veins for varicocele embolization.[22,26]
Percutaneous anterograde varicocele occlusion, by injection of sclerosing agents into an isolated vein from the pampiniform plexus in the scrotum after confirming its drainage fluoroscopically, was introduced in 1988.[27] Since then, several groups have reported their experience with the technique in treating varicoceles.[28–33] As with the retrograde procedure, anterograde occlusion can be performed under local anesthesia. Furthermore, the anterograde technique is associated with a lower operating time (10–15 min) and lower unperformable and overall persistence/recurrence rate (5–9%).[27,28] Although the complication rate is below 8% in most series, testicular atrophy post-treatment, presumably secondary to unidentified arterial injury, has been reported in 1% of the cases.[28] A major drawback of the anterograde approach is the need of an incision, most commonly at the suprascrotal level close to the base of the penis,[35] but the use of a subinguinal incision has also been described[36,37] to gain access to the spermatic veins. In addition, for large varicoceles, the recurrence/persistence rate of antegrade occlusion as high as 25% has been reported. Although radiation exposure during the embolization is a potential concern, as in the retrograde technique, some investigators reported their experience of anterograde varicocele occlusion without the use of fluoroscopy.[36]
Surgical repair of varicocele
Surgical repair remains the most popular form of treatment for varicocele and it can be achieved by conventional open varicocelectomy (retroperitoneal high ligation, inguinal and sub-inguinal ligation), laparoscopic/robotic varicocelectomy and microsurgical varicocelectomy [Table 1].
Open varicocelectomy
Conventional open varicocelectomy can be performed using different incisions to expose the spermatic vessels at various levels. High retroperitoneal ligation of varicocele, also known as the Palomo technique, is performed through a horizontal incision medial and inferior to the ipsilateral anterior superior iliac spine and extending medially. The external oblique fascia is incised in the direction of the fibers and the internal oblique muscle retracted cranially to expose the internal spermatic veins proximal to the internal inguinal ring.
In the inguinal approach, an incision is made in the groin above and lateral to the ipsilateral pubic tubercle and extending laterally along the skin lines of the inferior abdominal wall. The external oblique fascia is sharply incised to expose the spermatic cord covered with the cremasteric fibers, which, along with the external spermatic fascia, are incised to provide access to the vascular structures within. Generally, the vas deferens along with its artery, vein and lymphatic vessels, should be identified and preserved. Venous structures, including the internal spermatic veins, cremasteric veins, external spermatic veins, gubernacular veins and periarterial veins (venae comitantes), have all been described to be part of the body of varicoceles and should be identified and dissected for ligation. Any arteries and lymphatic vessels should be clearly identified and preserved to avoid complications.
Incision of the open subinguinal varicocelectomy is made at the level of the external inguinal ring to allow delivery of the spermatic cord without dividing any muscle or fascia of the abdominal wall. Although this approach has less morbidity and is less painful than the two other open varicocelectomy techniques described above, all vessels branch out at this low level, resulting in a higher number of vessels, each of a smaller diameter, to be dissected. Thus, optical magnification is strongly recommended when performing a subinguinal varicocelectomy (see microsurgical varicocelectomy below).
Although open varicocelectomy is commonly performed under general or spinal anesthesia on an outpatient basis, in selected patients, it can be performed under local/regional blockage with or without intravenous sedation.[38,39] Conventional open varicocelectomy is associated with a wide range of variation in the surgical outcomes. Complications, occurring at a rate of 5-30%, include hydroceles, inadvertent arterial ligation, testicular atrophy, injury to the vas deferens, epididymitis, hematoma and wound infection.[40] The recurrence/persistence rate, at 10–45%, is also significantly higher than other treatment options.
Laparoscopic varicocelectomy
Laparoscopic varicocelectomy has the advantage of isolating the internal spermatic veins proximally, near the point of drainage into the left renal vein. At this level, only one or two large veins are present and, hence, a fewer number veins are to be ligated. In addition, the testicular artery has not yet branched out and is often distinctly separate from the internal spermatic veins. Laparoscopic varicocelectomy is generally performed transperitoneally, but extra- or retro-peritoneal approaches have also been described.[41,42] The persistence/recurrence rate of laparoscopic varicocelectomy is in the range of 6–15%.[21,43–52]
Failure is usually due to preservation of the periarterial plexus of fine veins (venae comitantes) along with the artery. Various studies reported that artery preservation during laparoscopic varicocelectomy results in higher recurrence/persistence rates (3.5–20%) than when the spermatic vessels are ligated.[51,53–56] These venae comitantes have been shown to communicate with larger internal spermatic veins. If left intact, they may dilate with time and cause recurrence. Thus, in the majority of cases of laparoscopic varicocelectomy, the artery is intentionally ligated to minimize the recurrence/persistence rates. Although testicular atrophy is rarely reported,[57] ligation of the testicular artery can potentially impair the ability of the testis to maximize its function in the long run, particularly in adults.[58,59]
Less commonly, failure of laparoscopic varicocelectomy is due to the presence of parallel inguinal or retroperitoneal collaterals, which may exit the testis and bypass the ligated retroperitoneal veins rejoining the internal spermatic vein proximal to the site of ligation.[45,60] Likewise, dilated cremasteric veins, another cause of varicocele recurrence,[45] cannot be identified retroperitoneally with the laparoscopic approach.
Complications of laparoscopic varicocelectomy, occurring at an overall rate of 8–12%,[21,44,45–52] include air embolism, inadvertent arterial division, genitofermoral nerve injury, hydrocele, intestinal injury and peritonitis. Hydrocele, secondary to lymphatic congestion after accidental ligation of the lymphatic vessels, is the most commonly encountered post-operative complication. When the lymphatics are not intentionally identified and preserved, the post-operative hydrocele rate can be as high as 40%.[61,62] Technically, with the optical capacity of laparoscopes at close distance to the tissues, magnification at 10–20x can be achievable, allowing skillful laparoscopic surgeons to visualize and spare lymphatic vessels using similar microsurgical principles and techniques as in microsurgical varicocelectomy.[63] To further facilitate the identification of lymphatics, various authors described techniques of scrotal infusion of blue dyes (patent blue V, isosulfan blue or methylene blue) that could result in a significant reduction of the post-operative hydrocele.[62–67]
Laparoscopic varicocelectomy should only be performed by experienced laparoscopic urologists. Other disadvantages of the procedure include the high cost, need of general anesthesia in all cases and hospital stay of over 1 day. Although two-trocar[68,69] and single-trocar[70] approaches have been described, three trocars are generally required for laparoscopic varicocelectomy, making it more cost-effective for the treatment of bilateral than unilateral varicoceles. The operating time ranges from 20 to 80 min per side. To further minimize costs and time of surgery, various modifications have been proposed, including the use of Harmonic Scaplel®[71] and bipolar coagulation,[72] to transect and seal the varicoceles instead of using clips.
Robot-assisted varicoclectomy
With the increase in the availability of surgical robots, it is logical to expect their surgical application to be extended to varicocelectomy. Several groups of investigators have reported their initial experience on robot-assisted varicocelectomy.[73–75] While the cost associated with a surgical robot is certainly a significant limiting factor for the widespread use of robotic-assisted varicocelectomy, there seems to be clear benefits of this approach compared with the conventional laparoscopic varicocelectomy. Advantages of the robotic approach include (1) 3-dimentional optics to allow improved precision of dissection, (2) enhanced stability and ergonomics of instrument handling for surgeons to overcome the limited mobility imposed by the use of straight laparoscopic instruments and (3) increased degree of freedom in the range and extent of instrument manipulation. No doubt, with time, as surgical robots becomes more accessible and as surgeons continue to gain experience with robot-assisted surgeries, robotic varicocelectomy will find its place in the list of management options for varicoceles.
Microsurgical subinguinal varicocelectomy
The introduction of microsurgical techniques in varicocelectomy significantly reduced the persistence/recurrence rate (0–2%) and the complication rate (1–5%).[38,45,50,76,77] This outpatient procedure can be performed under local, regional or general anesthesia and the operating time per side is 25-60 min. Male infertility specialists in most academic centers have adopted microsurgical subinguinal varicocelectomy as the routine standard treatment. This general trend of increasing popularity of microsurgical varicocelectomy is largely due to the associated favorable outcomes. Even in cases of persistent or recurrent varicocele after initial varicocele therapy, microsurgical subinguinal varicocelectomy can further improve semen parameters, serum testosterone levels and testicular volume from pre-operative levels with minimal risks of complications.[78]
Specifically, microsurgical subinguinal varicocelectomy provides four important benefits: (1) a subinguinal incision allows exposure of the spermatic cord without splitting any abdominal muscles or fascia as in inguinal or retroperitoneal varicocelectomy, resulting in less post-operative pain and earlier return of functioning status for patients, (2) clear identification of varicoceles and small venous collaterals to minimize persistent/recurrence of varicoceles, (3) clear identification of arteries to avoid their accidental ligation and (4) clear identification of lymphatic vessels to avoid their accidental ligation, which can lead to the development of ipsilateral hydrocele as a post-operative complication. At the subinguinal level, in addition to the internal spermatic veins, there exist other small venous collaterals, including cremasteric veins, periarterial venous plexus, extra-spermatic and gubernacular collaterals [Figure 1]. These small venous collaterals, if missed, will dilate post-operatively with time, leading to the recurrence of varicoceles. Hopps et al.,[79] advocate occlusion of all veins >2.0 mm, including the gubernacular veins, identifiable through delivery of the testis above the wound to expose the gubernaculums.
Figure 1.
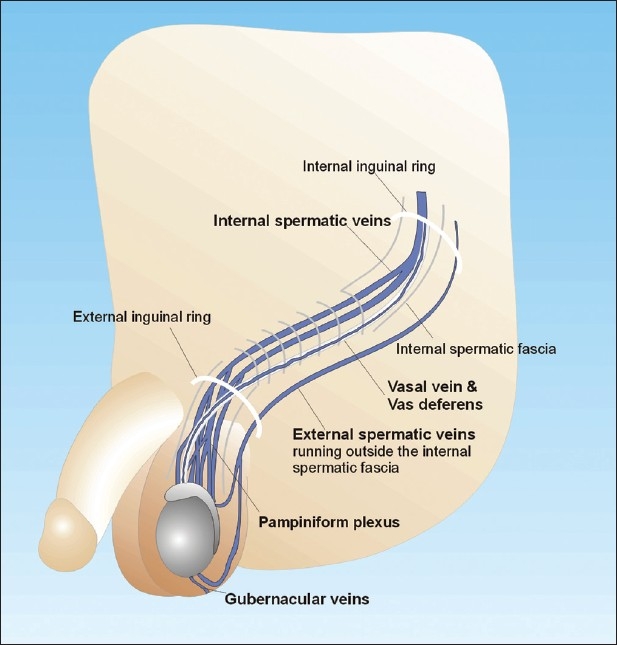
Various routes of venous drainage for the testis
Testicular arteries are clearly identified under 10–25x magnification and preserved. The operating microscope is particularly helpful when the arteries are in spasm due to manipulation or when multiple small branches of the arteries, which are easily missed without optical magnification, are encountered during dissection. The use of intra-operative microvascular Doppler evaluation and the use of papaverine irrigation to dilate arteries in spasm are approaches that can facilitate the identification of artery. A lower level of magnification achievable by loupe does not provide comparable benefits than with an operating microscope.[80–82] Gontero et al.[81] concluded that if loupes are used instead an operating microscope, an inguinal approach, where spermatic vessels are larger in size, rather than a subinguinal approach, this allows for better preservation of spermatic artery and reduced incidence of persistent pathologic vein reflux.
Although the testis receives additional blood supply from the vasal (deferential) and cremasteric arteries, the testicular artery is the main arterial supply to the testis and should thus be preserved. We reported previously that accidental testicular artery ligation in microsurgical varicocelectomy occurs in 19 out of over 2,100 cases, giving an incidence of approximately 1%.[59] In all cases, at least one alternative artery in addition to the vasal artery was identified. This may, in part, explain the low testicular atrophy rate of 5% among the patients with accidental arterial ligation during microsurgical varicocelectomy. Despite the low incidence of testicular atrophy, the natural pregnancy rate in this small cohort of men with accidental arterial ligation was significantly lower (14% vs. 46%) than that in men without arterial injury during the procedure. Finally, microsurgical varicocelectomy allows for the identification and preservation of the lymphatics, virtually eliminating post-operative hydrocele formation, which is the most common complication of non-microsurgical varicocelectomy.
Utilizing microsurgical artery- and lymphatic-sparing techniques, the recurrence rates are reduced to 1% and the post-operative hydrocele and testicular atrophy is virtually eliminated. Repair of large varicocele results in a 143% increase in motile sperm in the ejaculate and a pregnancy rate of 47% at 1 year.[38,83] Even men with non-obstructive azoospermia may respond to varicocelectomy with return of sperm to the ejaculate in 21–55% of the cases,[76,77,84–86] obviating the need for testicular sperm retrieval for intra-cytoplasmic sperm injection.
COMPARATIVE STUDIES OF THE VARIOUS TREATMENT OPTIONS
The recurrence/persistence rates, the complication rates, time of procedure, the costs and clinical outcomes on the various treatment modalities vary [Table 1]. Well-designed, large-scale “head-to-head” comparatives studies evaluating the results of the various treatment options of varicoceles remain scarce in the recent literature.[7,43,87] It should be emphasized that in interpreting the results of each study, confounding factors such as the experience of the operators for each procedure and patient factors such as age, severity and bilaterality of the varicoceles have a significant impact on the post-treatment outcomes. In addition to improving the fertility status, the potentially important role of urologists in preventing future infertility and decline of testicular hormonal function underscores the importance of utilizing a varicocele management option that is efficacious and minimizes the risk of complications and recurrence.
In a retrospective study comparing laparoscopic surgery versus antegrade sclerotherapy, May et al.[88] reported a higher failure rate with antegrade sclerotherapy (16%) compared with laparoscopic treatment (5%). Although the procedural time and length of stay post-procedure are comparable, laparoscopic treatment has a significantly higher rate of complication (13% vs. 5%), with hydrocele being the most common one (11%). In a retrospective study by Beutner et al.[89] comparing laparoscopy, retrograde and antegrade sclerotherapy, it was noted that although the laparoscopic approach has a lower recurrence rate (5% vs. 16% with anterograde and 19% with retrograde sclerotherapy), it is associated with a higher complication rate (15% vs. 5% with anterograde and 9% with retrograde sclerotherapy). Hydrocele was the most common complication with the laparoscopic approach while, for the two sclerotherapies, it was epididymo-orchitis. The higher complication rate, along with the higher cost associated with laparoscopy compared with antegrade sclerotherapy, were also reported in a prospective analysis.[90]
In a randomized prospective study comparing open inguinal varicocelectomy performed under local anesthesia with a 3.5x loupe-magnification and antegrade sclerotherapy, both for the treatment of left-sided varicoceles, Zucchi et al.[91] reported that although the two treatments yielded similar complication and recurrence rates, antegrade sclerotherapy is a faster procedure (25 vs. 42 min), with earlier recovery for normal physical activity (1 day vs. 3–4 days) and marginally better post-treatment semen parameters evaluated at 8 months.
Pintus et al.[54] compared retrograde sclerotherapy, open retroperitoneal high ligation (Palomo technique) with or without sparing of the artery and laparoscopic high ligation with or without sparing of the artery, all for the treatment of left-sided varicoceles in the pediatric population. The highest recurrence rate was noted with laparoscopic high ligation with arterial sparing (25%) compared with sclerotherapy (17%), inguinal open varicocelectomy (15%) and open high ligation with arterial sparing. When the arteries were not spared, the recurrence rate was lower for open high ligation (3.4%) and laparoscopic high ligation (0%).
Microsurgical varicocelectomy has been compared with retroperitoneal high ligation without artery sparing,[92,93] open inguinal varicocelectomy and laparoscopy without artery sparing.[87,93–96] Although microsurgical varicocelectomy generally takes longer operative time and requires additional surgical training and equipment, most investigators are in favor of the microsurgical approach as it is associated with a shorter hospitalization period and earlier recovery, lower recurrence and complication rates and possibly higher level improvement in sperm count and motility. It should however be emphasized that the skills and experience of the surgeons play a tremendous role in the outcomes of the procedures used. For instance, in the hands of skillful laparoscopist, the post-operative outcomes and complication rates can be comparable to microsurgical varicocelectomy.[94,97] On the contrary, inexperienced surgeons or other circumstantial factors may result in prolonged surgical time and unusual complications (e.g., urinary retention) that can lead to prolonged hospitalization, which may offset the benefits of microsurgical varicocelectomy seen in the hands of experience surgeons.
CONCLUSIONS
Varicoceles remains one of the most commonly diagnosed conditions leading to male infertility. While various approaches are available to correct varicoceles, it is evident from the current literature that each technique has its own strengths and limitations. With the lack of large-scale randomized control trials to compare the efficacies, cost-effectiveness and complications of the various treatment options currently available for varicoceles, it is impossible to draw a valid conclusionas to which technique is the best treatment choice for an individual affected by varicoceles. What is certain, however, is that the treatment outcomes are highly dependent on the experience and skill of the treating physicians. Thus, urologists, andrologists or radiologists who have a preference of one technique over the other must not only ensure that their treatment outcomes meet the current standard of care, as described in the current literature, and that they must also continue to modify and improve their treatment approach, aiming to minimize the complication rate, costs and treatment and recovery time while maximizing post-operative improvement of long-term testicular function for patients with varicoceles.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zini A, Blumenfeld A, Libman J, Willis J. Beneficial effect of microsurgical varicocelectomy on human sperm DNA integrity. Hum Reprod. 2005;20:1018–21. doi: 10.1093/humrep/deh701. [DOI] [PubMed] [Google Scholar]
- 2.Zini A, Azhar R, Baazeem A, Gabriel MS. Effect of microsurgical varicocelectomy on human sperm chromatin and DNA integrity: A prospective trial. Int J Androl. 2011;34:14–9. doi: 10.1111/j.1365-2605.2009.01048.x. [DOI] [PubMed] [Google Scholar]
- 3.Daitch JA, Bedaiwy MA, Pasqualotto EB, Hendin BN, Hallak J, Falcone T, et al. Varicocelectomy improves intrauterine insemination success rates in men with varicocele. J urol. 2001;165:1510–3. [PubMed] [Google Scholar]
- 4.Penson DF, Paltiel AD, Krumholz HM, Palter S. The cost-effectiveness of treatment for varicocele related infertility. J urol. 2002;168:2490–4. doi: 10.1016/S0022-5347(05)64175-4. [DOI] [PubMed] [Google Scholar]
- 5.Cayan S, Erdemir F, Ozbey I, Turek PJ, Kadioglu A, Tellaloglu S. Can varicocelectomy significantly change the way couples use assisted reproductive technologies? J urol. 2002;167:1749–52. doi: 10.1016/s0022-5347(05)65192-0. [DOI] [PubMed] [Google Scholar]
- 6.Richardson I, Grotas AB, Nagler HM. Outcomes of varicocelectomy treatment: An updated critical analysis. Urol Clin North Am. 2008;35:191–209. doi: 10.1016/j.ucl.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Cayan S, Shavakhabov S, Kadiolu A. Treatment of palpable varicocele in infertile men: A meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 8.Chan PT, Goldstein M. Varicocele: Options for management. AUA News. 2001;6:1–6. [Google Scholar]
- 9.Iaccarino V. Trattamento conservative del varicocele: Flebografia selettiva e sleroterapia delle vene gonadiche. Riv Radiol. 1977;17:107–17. [Google Scholar]
- 10.Lima SS, Castro MP, Costa OF. A new method for the treatment of varicocele. Andrologia. 1978;10:103–6. doi: 10.1111/j.1439-0272.1978.tb01324.x. [DOI] [PubMed] [Google Scholar]
- 11.Sze DY, Kao JS, Frisoli JK, McCallum SW, Kennedy WA, 2nd, Razavi MK. Persistent and recurrent postsurgical varicoceles: Venographic anatomy and treatment with N-butyl cyanoacrylate embolization. J Vasc Interv Radiol. 2008;19:539–45. doi: 10.1016/j.jvir.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Li L, Zeng XQ, Li YH. Digital subtraction angiography-guided percutaneous transcatheter foam sclerotherapy of varicocele: A novel tracking technique. AJR Am J Roentgenol. 2009;193:978–80. doi: 10.2214/AJR.09.2394. [DOI] [PubMed] [Google Scholar]
- 13.Punekar SV, Prem AR, Ridhorkar VR, Deshmukh HL, Kelkar AR. Post-surgical recurrent varicocele: Efficacy of internal spermatic venography and steel-coil embolization. Br J Urol. 1996;77:124–8. doi: 10.1046/j.1464-410x.1996.82321.x. [DOI] [PubMed] [Google Scholar]
- 14.Coley SC, Jackson JE. Endovascular occlusion with a new mechanical detachable coil. AJR Am J Roentgenol. 1998;171:1075–9. doi: 10.2214/ajr.171.4.9763000. [DOI] [PubMed] [Google Scholar]
- 15.Perala JM, Leinonen SA, Suramo IJ, Hellstrom PA, Seppanen EJ. Comparison of early deflation rate of detachable latex and silicone balloons and observations on persistent varicocele. J Vasc Interv Radiol. 1998;9:761–5. doi: 10.1016/s1051-0443(98)70388-4. [DOI] [PubMed] [Google Scholar]
- 16.Seyferth W, Jacht E, Zeitler E. Percutaneous sclerotherapy of varicocele. Radiology. 1981;139:335–40. doi: 10.1148/radiology.139.2.7220877. [DOI] [PubMed] [Google Scholar]
- 17.Bahren W, Lenz M, Porst H, Wierschin W. Nebenwirkungen, Komplikationen und kontraindikationen der perkutanen sklerotherapie der v spermatica interna zur Behandlung der idiopathischen varikozele. Rofo. 1983;138:172–9. doi: 10.1055/s-2008-1055705. [DOI] [PubMed] [Google Scholar]
- 18.Porst H. Bahren W, Lenz M, Altwein JE.Percutaneous sclerotherapy of varicoceles - an alternative to conventional surgical Methods. Br J Urol. 1984;56:73–8. doi: 10.1111/j.1464-410x.1984.tb07168.x. [DOI] [PubMed] [Google Scholar]
- 19.Thon WF, Sigmund G, Bahren W, Steinmann J. Perkutane sklerotherapie bei vena-tesikularis-insuffizienz. Akt Urol. 1986;17:240. [Google Scholar]
- 20.Lenz M, Hof N, Kersting-Sommerhoff B, Bautz W. Anatomic variants of the spermatic vein: importance for percutaneous sclerotherapy of idiopathic varicocele. Radiology. 1996;198:425–31. doi: 10.1148/radiology.198.2.8596844. [DOI] [PubMed] [Google Scholar]
- 21.Abdulmaaboud MR, Shokeir AA, Farage Y, El-rahman AA, El-Rakhawy MM, Mutabagani H. Treatment of varicocele: A comparative study of conventional open surgery, percutaneous retrograde sclerotherapy, and laparoscopy. Urology. 1998;52:294–300. doi: 10.1016/s0090-4295(98)00178-2. [DOI] [PubMed] [Google Scholar]
- 22.Gazzera C, Rampado O, Savio L, Di Bisceglie C, Manieri C, Gandini G. Radiological treatment of male varicocele: Technical, clinical, seminal and dosimetric aspects. Radiol Med. 2006;111:449–58. doi: 10.1007/s11547-006-0041-4. [DOI] [PubMed] [Google Scholar]
- 23.Chalmers N, Hufton AP, Jackson RW, Conway B. Radiation risk estimation in varicocele embolization. Br J Radiol. 2000;73:293–7. doi: 10.1259/bjr.73.867.10817046. [DOI] [PubMed] [Google Scholar]
- 24.Bähren W, Lenz M, Porst H, Wierschin W. Side effects, complications and contraindications for percutaneous sclerotherapy of the internal spermatic vein in the treatment of idiopathic varicocele. Rofo. 1983;138:172–9. doi: 10.1055/s-2008-1055705. [DOI] [PubMed] [Google Scholar]
- 25.Bähren W, Biehl C, Danz B. Failed sclerotherapy trials with the V.spermatica interna. A retrospective analysis in 1141 patients with idiopathic varicocele. Rofo. 1992;157:355–60. [PubMed] [Google Scholar]
- 26.Gandini R, Konda D, Reale CA, Pampana E, Maresca L, Spinelli A, et al. Male varicocele: Transcatheter foam sclerotherapy with sodium tetradecyl sulfate--outcome in 244 patients. Radiology. 2008;246:612–8. doi: 10.1148/radiol.2462061295. [DOI] [PubMed] [Google Scholar]
- 27.Tauber T, Weizert P, Pfeifer KJ, Huber R. Die antegrade sklerosierung der vena spermatica zur therapie der varikozele.Eine randomisierte, kontrollierte, prospective studie verhandlungs ber. Dtsch Ges Urol. 1988;40:239–40. [Google Scholar]
- 28.Tauber R, Johnsen N. Antegrade scrotal sclerotherapy for the treatment of varicocele: Technique and late results. J Urol. 1994;15:386–90. doi: 10.1016/s0022-5347(17)34956-x. [DOI] [PubMed] [Google Scholar]
- 29.Mottrie AM, Matani Y, Baert J, Voges GE, Hohenfellner R. Antegrade scrotal sclerotherapy for the treatment of varicocele in childhood and adolescence. Br J Urol. 1995;76:21–4. doi: 10.1111/j.1464-410x.1995.tb07825.x. [DOI] [PubMed] [Google Scholar]
- 30.Ficarra V, Porcaro AB, Righetti R, Cerruto MA, Pilloni S, Cavalleri S, et al. Antegrade scrotal sclerotherapy in the treatment of varicocele: A prospective study. BJU Int. 2002;89:264–8. doi: 10.1046/j.1464-4096.2001.02418.x. [DOI] [PubMed] [Google Scholar]
- 31.Ficarra V, Sarti A, Novara G, Dalpiaz O, Galfano A, Cavalleri S, et al. Modified antegrade scrotal sclerotherapy in adolescent patients with varicocele. J Pediatr Surg. 2004;39:1034–6. doi: 10.1016/j.jpedsurg.2004.03.059. [DOI] [PubMed] [Google Scholar]
- 32.Zaupa P, Mayr J, Höllwarth ME. Antegrade scrotal sclerotherapy for treating primary varicocele in children. BJU Int. 2006;97:809–12. doi: 10.1111/j.1464-410X.2006.06033.x. [DOI] [PubMed] [Google Scholar]
- 33.Galfano A, Novara G, Iafrate M, De Marco V, Cosentino M, D’Elia C, et al. Improvement of seminal parameters and pregnancy rates after antegrade sclerotherapy of internal spermatic veins. Fertil Steril. 2009;91:1085–9. doi: 10.1016/j.fertnstert.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 34.Galfano A, Novara G, Iafrate M, Fracalanza S, Novella G, Cavalleri S, et al. Surgical outcomes after modified antegrade scrotal sclerotherapy: A prospective analysis of 700 consecutive patients with idiopathic varicocele. J Urol. 2008;179:1933–7. doi: 10.1016/j.juro.2008.01.042. [DOI] [PubMed] [Google Scholar]
- 35.Tauber R, Pfeiffer D. Surgical atlas varicocele: Antegrade scrotal sclerotherapy. BJU Int. 2006;98:1333–44. doi: 10.1111/j.1464-410X.2006.06579.x. [DOI] [PubMed] [Google Scholar]
- 36.Colpi GM, Carmignani L, Nerva F, Piediferro G, Castiglioni F, Grugnetti C, et al. Surgical treatment of varicocele by a subinguinal approach combined with antegrade intraoperative sclerotherapy of venous vessels. BJU Int. 2006;97:142–5. doi: 10.1111/j.1464-410X.2006.05915.x. [DOI] [PubMed] [Google Scholar]
- 37.Lebed B, Packer M, Husmann D, Zaontz M. Results and complications of adolescent varicocele repair with intraoperative sodium morrhuate sclerotherapy. J Urol. 2008;180:1837–41. doi: 10.1016/j.juro.2008.04.072. [DOI] [PubMed] [Google Scholar]
- 38.Marmar JL, Kim Y. Subinguinal microsurgical varicocelectomy: A technical critique and statistical analysis of semen and pregnancy data. J Urol. 1994;152:1127–32. doi: 10.1016/s0022-5347(17)32521-1. [DOI] [PubMed] [Google Scholar]
- 39.Hsu GL, Ling PY, Hsieh CH, Wang CJ, Chen CW, Wen HS, et al. Outpatient varicocelectomy performed under local anesthesia. Asian J Androl. 2005;7:439–44. doi: 10.1111/j.1745-7262.2005.00080.x. [DOI] [PubMed] [Google Scholar]
- 40.Szabo R, Kessler R. Hydrocele following internal spermatic vein ligation: A retrospective study and review of the literature. J Urol. 1984;132:924–5. doi: 10.1016/s0022-5347(17)49950-2. [DOI] [PubMed] [Google Scholar]
- 41.Demirci D, Gülmez I, Hakan NA, Ekmekçioglu O, Karacagil M. Comparison of extraperitoneoscopic and transperitoneoscopic techniques for the treatment of bilateral varicocele. J Endourol. 2003;17:89–92. doi: 10.1089/08927790360587405. [DOI] [PubMed] [Google Scholar]
- 42.Cobellis G, Mastroianni L, Cruccetti A, Amici G, Martino A. Retroperitoneoscopic varicocelectomy in children and adolescents. J Pediatr Surg. 2005;40:846–9. doi: 10.1016/j.jpedsurg.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 43.Cayan S, Kadioglu TC, Tefekli A, Dadioglu A, Tellaloglu S. Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology. 2000;55:750–4. doi: 10.1016/s0090-4295(99)00603-2. [DOI] [PubMed] [Google Scholar]
- 44.Hirsch IH, Abdel-Meguid TA, Gomella LG. Postsurgical outcomes assessment following varicocele ligation: Laparoscopic versus subinguinal approach. Urology. 1998;51:810–5. doi: 10.1016/s0090-4295(97)00709-7. [DOI] [PubMed] [Google Scholar]
- 45.Sayfan J, Adam YG, Soffer Y. A new entity in varicocele subfertility: The “cremasteric reflux”. Fertil Steril. 1980;33:88–90. doi: 10.1016/s0015-0282(16)44486-9. [DOI] [PubMed] [Google Scholar]
- 46.Homonnai ZT, Fainman N, Engelhard Y, Rudberg Z, David MP, Paz G. Varicocelectomy and male fertility: Comparison of semen quality and recurrence of varicocele following varicocelectomy by two techniques. Int J Androl. 1980;3:447–58. doi: 10.1111/j.1365-2605.1980.tb00133.x. [DOI] [PubMed] [Google Scholar]
- 47.Rothman CM, Newmark H, 3rd, Karson R.A. The recurrent varicocele - a poorly recognized problem. Fertil Steril. 1981;35:552–6. doi: 10.1016/s0015-0282(16)45500-7. [DOI] [PubMed] [Google Scholar]
- 48.Belgrano E, Puppo P, Quattrini S, Trombetta C, Giuliani L. The role venography and sclerotherapy in the management of varicocele. Eur Urol. 1984;10:124–9. doi: 10.1159/000463769. [DOI] [PubMed] [Google Scholar]
- 49.Thomas AJ, Giesinger MA. Current management of varicocele. Urol Clin North Am. 1990;17:893–907. [PubMed] [Google Scholar]
- 50.Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C. Microsurgical inguinal varicocelectomy with delivery of the testis: An artery and lymphatic sparing technique. J Urol. 1992;148:1808–11. doi: 10.1016/s0022-5347(17)37035-0. [DOI] [PubMed] [Google Scholar]
- 51.Kass EJ, Marcol B. Results of varicocele surgery in adolescents: A comparison of techniques. J Urol. 1992;148:694–6. doi: 10.1016/s0022-5347(17)36696-x. [DOI] [PubMed] [Google Scholar]
- 52.Parrott RS, Hewatt L. Ligation of the testicular artery and vein in adolescent varicocele. J Urol. 1993;152:791–3. doi: 10.1016/s0022-5347(17)32711-8. [DOI] [PubMed] [Google Scholar]
- 53.Esposito C, Monguzzi GL, Gonzalez-Sabin MA, Rubino R, Montinaro L, Papparella A, et al. Laparoscopic treatment of pediatric varicocele: A multicenter study of the Italian society of video surgery in infancy. J Urol. 2000;163:1944–6. doi: 10.1016/s0022-5347(05)67604-5. [DOI] [PubMed] [Google Scholar]
- 54.Pintus C, Rodriguez Matas MJ, Manzoni C, Nanni L, Perrelli L. Varicocele in pediatric patients: Comparative assessment of different therapeutic approaches. Urology. 2001;57:154–7. doi: 10.1016/s0090-4295(00)00859-1. [DOI] [PubMed] [Google Scholar]
- 55.Kattan S. Incidence and pattern of varicocele recurrence after laparoscopic ligation of the internal spermatic vein with preservation of the testicular artery. Scand J Urol Nephrol. 1998;32:335–40. doi: 10.1080/003655998750015296. [DOI] [PubMed] [Google Scholar]
- 56.Riccabona M, Oswald J, Koen M, Lusuardi L, Radmayr C, Bartsch G. Optimizing the operative treatment of boys with varicocele: Sequential comparison of 4 techniques. J Urol. 2003;169:666–8. doi: 10.1097/01.ju.0000047086.34953.82. [DOI] [PubMed] [Google Scholar]
- 57.Esposito C, Monguzzi G, Gonzalez-Sabin MA, Rubino R, Montinaro L, Papparella A, et al. Results and complications of laparoscopic surgery for pediatric varicocele. J Pediatr Surg. 2001;36:767–9. doi: 10.1053/jpsu.2001.22956. [DOI] [PubMed] [Google Scholar]
- 58.Zampieri N, Zuin V, Corroppolo M, Chironi C, Cervellione RM, Camoglio FS. Varicocele and adolescents: Semen quality after 2 different laparoscopic procedures. J Androl. 2007;28:727–33. doi: 10.2164/jandrol.107.002600. [DOI] [PubMed] [Google Scholar]
- 59.Chan PT, Wright EJ, Goldstein M. Incidence and postoperative outcomes of accidental ligation of the testicular artery during microsurgical varicocelectomy. J Urol. 2005;173:482–4. doi: 10.1097/01.ju.0000148942.61914.2e. [DOI] [PubMed] [Google Scholar]
- 60.Murray RR, Mitchell SE, Kadir S, Kaufman SL, Chang R, Kinnison ML, et al. Comparison of recurrent varicocele anatomy following surgery and percutaneous balloon occlusion. J Urol. 1986;135:286–9. doi: 10.1016/s0022-5347(17)45615-1. [DOI] [PubMed] [Google Scholar]
- 61.Hassan JM, Adams MC, Pope JC, 4th, Demarco RT, Brock JW., 3rd Hydrocele formation following laparoscopic varicocelectomy. J Urol. 2006;175:1076–9. doi: 10.1016/S0022-5347(05)00402-7. [DOI] [PubMed] [Google Scholar]
- 62.Schwentner C, Radmayr C, Lunacek A, Gozzi C, Pinggera GM, Neururer R, et al. Laparoscopic varicocele ligation in children and adolescents using isosulphan blue: A prospective randomized trial. BJU Int. 2006;98:861–5. doi: 10.1111/j.1464-410X.2006.06428.x. [DOI] [PubMed] [Google Scholar]
- 63.Kocvara R, Dvorácek J, Sedlácek J, Díte Z, Novák K. Lymphatic sparing laparoscopic varicocelectomy: A microsurgical repair. J Urol. 2005;173:1751–4. doi: 10.1097/01.ju.0000154357.72837.43. [DOI] [PubMed] [Google Scholar]
- 64.Barot P, Neff M, Cantor B, Baig A, Geis PW, Fleisher M. Laparoscopic varicocelectomy with lymphatic preservation using methylene blue dye. J Laparoendosc Adv Surg Tech A. 2004;14:183–5. doi: 10.1089/1092642041255504. [DOI] [PubMed] [Google Scholar]
- 65.Chiarenza SF, D’Agostino S, Scarpa M, Fabbro M, Costa L, Musi L. Lymphography prior to laparoscopic Palomo varicocelectomy to prevent postoperative hydrocele. J Laparoendosc Adv Surg Tech A. 2006;16:394–6. doi: 10.1089/lap.2006.16.394. [DOI] [PubMed] [Google Scholar]
- 66.Golebiewski A, Krolak M, Komasara L, Czauderna P. Dye-assisted lymph vessels sparing laparoscopic varicocelectomy. J Laparoendosc Adv Surg Tech A. 2007;17:360–3. doi: 10.1089/lap.2006.0072. [DOI] [PubMed] [Google Scholar]
- 67.D’Alessio A, Piro E, Beretta F, Brugnoni M, Marinoni F, Abati L. Lymphatic preservation using methylene blue dye during varicocele surgery: A single-center retrospective study. J Pediatr Urol. 2008;4:138–40. doi: 10.1016/j.jpurol.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 68.Al-Hunayan A, Abdulhalim H, Kehinde EO, El-Barky E, Al-Awadi K, Al-Ateeqi A. Two-trocar laparoscopic varicocelectomy: Cost-reduction surgical technique. Urology. 2006;67:461–5. doi: 10.1016/j.urology.2005.09.049. [DOI] [PubMed] [Google Scholar]
- 69.Link BA, Kruska JD, Wong C, Kropp BP. Two trocar laparoscopic varicocelectomy: Approach and outcomes. JSLS. 2006;10:151–4. [PMC free article] [PubMed] [Google Scholar]
- 70.Kaouk JH, Palmer JS. Single-port laparoscopic surgery: Initial experience in children for varicocelectomy. BJU Int. 2008;102:97–9. doi: 10.1111/j.1464-410X.2008.07584.x. [DOI] [PubMed] [Google Scholar]
- 71.Sasagawa I, Yazawa H, Suzuki Y, Tateno T, Takahashi Y, Nakada T. Laparoscopic varicocelectomy in adolescents using an ultrasonically activated scalpel. Arch Androl. 2000;45:91–4. doi: 10.1080/014850100418765. [DOI] [PubMed] [Google Scholar]
- 72.Simforoosh N, Ziaee SA, Behjati S, Beygi FM, Arianpoor A, Abdi H. Laparoscopic management of varicocele using bipolar cautery versus open high ligation technique: A randomized, clinical trial. J Laparoendosc Adv Surg Tech A. 2007;17:743–7. doi: 10.1089/lap.2006.0174. [DOI] [PubMed] [Google Scholar]
- 73.Corcione F, Esposito C, Cuccurullo D, Settembre A, Miranda N, Amato F, et al. Advantages and limits of robot-assisted laparoscopic surgery: preliminary experience. Surg Endosc. 2005;19:117–9. doi: 10.1007/s00464-004-9004-9. [DOI] [PubMed] [Google Scholar]
- 74.Shu T, Taghechian S, Wang R. Initial experience with robot-assisted varicocelectomy. Asian J Androl. 2008;10:146–8. doi: 10.1111/j.1745-7262.2008.00354.x. [DOI] [PubMed] [Google Scholar]
- 75.Hidalgo-Tamola J, Sorensen MD, Bice JB, Lendvay TS. Pediatric robot-assisted laparoscopic varicocelectomy. J Endourol. 2009;23:1297–300. doi: 10.1089/end.2008.0523. [DOI] [PubMed] [Google Scholar]
- 76.Matthews G.J, Matthews E.D, Goldstein M. Induction of spermatogenesis and achievement of pregnancy after microsurgical varicocelectomy in men with azoospermia and severe oligoasthenospermia. Fertil Steril. 1998;70:71–5. doi: 10.1016/s0015-0282(98)00108-3. [DOI] [PubMed] [Google Scholar]
- 77.Kim ED, Leibman BB, Grinblat DI, Lipshultz LI. Varicocele repair improves semen parameters in azoospermic men with spermatogenic failure. J Urol. 1999;162:737–40. doi: 10.1097/00005392-199909010-00031. [DOI] [PubMed] [Google Scholar]
- 78.Grober ED, Chan PT, Zini A, Goldstein M. Microsurgical treatment of persistent or recurrent varicocele. Fertil Steril. 2004;82:718–22. doi: 10.1016/j.fertnstert.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 79.Hopps CV, Lemer ML, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: A microscopic study of the inguinal versus subinguinal approach. J Urol. 2003;170:2366–70. doi: 10.1097/01.ju.0000097400.67715.f8. [DOI] [PubMed] [Google Scholar]
- 80.Cayan S, Acar D, Ulger S, Akbay E. Adolescent varicocele repair: Long-term results and comparison of surgical techniques according to optical magnification use in 100 cases at a single university hospital. J Urol. 2005;174:2003–6. doi: 10.1097/01.ju.0000176488.44895.7b. [DOI] [PubMed] [Google Scholar]
- 81.Gontero P, Pretti G, Fontana F, Zitella A, Marchioro G, Frea B. Inguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia: Which technique is preferable in clinical practice? Urology. 2005;66:1075–9. doi: 10.1016/j.urology.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 82.Castagnetti M, Cimador M, Catalano P, DiPace M, Sergio M, De Grazia E. Evolving management of adolescent varicocele. J Pediatr Urol. 2008;4:107–12. doi: 10.1016/j.jpurol.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 83.Su LM, Goldstein M, Schlegel PN. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. J Urol. 1995;154:1752–5. [PubMed] [Google Scholar]
- 84.Kadioglu A, Tefekli A, Cayan S, Kandrirali E, Erdemir F, Tellaloglu S. Microsurgical inguinal varicocele repair in azoospermic men. Urology. 2001;57:328–33. doi: 10.1016/s0090-4295(00)00908-0. [DOI] [PubMed] [Google Scholar]
- 85.Pasqualotto FF, Soberiro BP, Hallak J, Pasqualotto EB, Lucon AM. Induction of spermatogenesis in azoospermic men after varicocelectomy repair: An update. Fertil Steril. 2006;85:635–9. doi: 10.1016/j.fertnstert.2005.08.043. [DOI] [PubMed] [Google Scholar]
- 86.Lee JS, Park HJ, Seo JT. What is the indication of varicocelectomy in men with nonobstructive azoospermia? Urology. 2007;69:352–5. doi: 10.1016/j.urology.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 87.Al-Said S, Al-Naimi A, Al-Ansari A, Younis N, Shamsodini A, A-sadiq K, et al. Varicocelectomy for male infertility: A comparative study of open, laparoscopic and microsurgical approaches. J Urol. 2008;180:266–70. doi: 10.1016/j.juro.2008.03.050. [DOI] [PubMed] [Google Scholar]
- 88.May M, Johannsen M, Beutner S, Helke C, Braun KP, Lein M, et al. Laparoscopic surgery versus antegrade scrotal sclerotherapy: Retrospective comparison of two different approaches for varicocele treatment. Eur Urol. 2006;49:384–7. doi: 10.1016/j.eururo.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 89.Beutner S, May M, Hoschke B, Helke C, Lein M, Roigas J, et al. Treatment of varicocele with reference to age: A retrospective comparison of three minimally invasive procedures. Surg Endosc. 2007;21:61–5. doi: 10.1007/s00464-005-0684-6. [DOI] [PubMed] [Google Scholar]
- 90.Sautter T, Sulser T, Suter S, Gretener H, Hauri D. Treatment of varicocele: A prospective randomized comparison of laparoscopy versus antegrade sclerotherapy. Eur Urol. 2002;41:398–400. doi: 10.1016/s0302-2838(02)00022-2. [DOI] [PubMed] [Google Scholar]
- 91.Zucchi A, Mearini L, Mearini E, Costantini E, Bini V, Porena M. Treatment of varicocele: Randomized prospective study on open surgery versus Tauber antegrade sclerotherapy. J Androl. 2005;26:328–32. doi: 10.2164/jandrol.04143. [DOI] [PubMed] [Google Scholar]
- 92.Ghanem H, Anis T, El-Nashar A, Shamloul R. Subinguinal microvaricocelectomy versus retroperitoneal varicocelectomy: Comparative study of complications and surgical outcome. Urology. 2004;64:1005–9. doi: 10.1016/j.urology.2004.06.060. [DOI] [PubMed] [Google Scholar]
- 93.Watanabe M, Nagai A, Kusumi N, Tsuboi H, Nasu Y, Kumon H. Minimal invasiveness and effectivity of subinguinal microscopic varicocelectomy: A comparative study with retroperitoneal high and laparoscopic approaches. Int J Urol. 2005;12:892–8. doi: 10.1111/j.1442-2042.2005.01142.x. [DOI] [PubMed] [Google Scholar]
- 94.VanderBrink BA, Palmer LS, Gitlin J, Levitt SB, Franco I. Lymphatic-sparing laparoscopic varicocelectomy versus microscopic varicocelectomy: Is there a difference? Urology. 2007;70:1207–10. doi: 10.1016/j.urology.2007.09.036. [DOI] [PubMed] [Google Scholar]
- 95.McManus MC, Barqawi A, Meacham RB, Furness PD, 3rd, Koyle MA. Laparoscopic varicocele ligation: Are there advantages compared with the microscopic subinguinal approach? Urology. 2004;64:357–60. doi: 10.1016/j.urology.2004.03.055. [DOI] [PubMed] [Google Scholar]
- 96.Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA. Comparison of outcomes of different varicocelectomy techniques: Open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: A randomized clinical trial. Urology. 2007;69:417–20. doi: 10.1016/j.urology.2007.01.057. [DOI] [PubMed] [Google Scholar]
- 97.Zampieri N, Mantovani A, Ottolenghi A, Camoglio FS. Testicular catch-up growth after varicocelectomy: Does surgical technique make a difference? Urology. 2009;73:289–92. doi: 10.1016/j.urology.2008.07.039. [DOI] [PubMed] [Google Scholar]
- 98.Granata C, Oddone M, Toma P, Mattioli G. Retrograde percutaneous sclerotherapy of left idiopathic varicocele in children: Results and follow-up. Pediatr Surg Int. 2008;24:583–7. doi: 10.1007/s00383-008-2124-x. [DOI] [PubMed] [Google Scholar]
- 99.Sivanathan C, Abernethy LJ. Retrograde embolisation of varicocele in the paediatric age group: A review of 10 years’ practice. Ann R Coll Surg Engl. 2003;85:50–1. doi: 10.1308/003588403321001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Flacke S, Schuster M, Kovacs A, von Falkenhausen M, Strunk HM, Haidl G, et al. Embolization of varicocles: Pretreatment sperm motility predicts later pregnancy in partners of infertile men. Radiology. 2008;248:540–9. doi: 10.1148/radiol.2482071675. [DOI] [PubMed] [Google Scholar]
- 101.Alqahtani A, Yazbeck S, Dubois J, Garel L. Percutaneous embolization of varicocele in children: A Canadian experience. J Pediatr Surg. 2002;37:783–5. doi: 10.1053/jpsu.2002.32287. [DOI] [PubMed] [Google Scholar]
- 102.Johnsen N, Tauber R. Financial analysis of antegrade scrotal sclerotherapy for men with varicoceles. Br J Urol. 1996;77:129–32. doi: 10.1046/j.1464-410x.1996.78622.x. [DOI] [PubMed] [Google Scholar]
- 103.Wuernschimmel E, Lipsky H, Noest G. Laparoscopic varicocele ligation: A recommendable standard procedure with good long-term results. Eur Urol. 1995;27:18–22. doi: 10.1159/000475116. [DOI] [PubMed] [Google Scholar]
- 104.Donovan JF, Winfield HN. Laparoscopic varix ligation. J Urol. 1992;147:77–81. doi: 10.1016/s0022-5347(17)37138-0. [DOI] [PubMed] [Google Scholar]
- 105.Poon SA, Kozakowski KA, Decastro GJ, Gjertson CK, Glassberg KI. Adolescent varicocelectomy: Postoperative catch-up growth is not secondary to lymphatic ligation. J Pediatr Urol. 2009;5:37–41. doi: 10.1016/j.jpurol.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 106.Glassberg KI, Poon SA, Gjertson CK, DeCastro GJ, Misseri R. Laparoscopic lymphatic sparing varicocelectomy in adolescents. J Urol. 2008;180:326–30. doi: 10.1016/j.juro.2008.03.064. [DOI] [PubMed] [Google Scholar]
- 107.Chrouser K, Vandersteen D, Crocker J, Reinberg Y. Nerve injury after laparoscopic varicocelectomy. J Urol. 2004;172:691–3. doi: 10.1097/01.ju.0000129368.47533.f8. [DOI] [PubMed] [Google Scholar]
- 108.Muensterer OJ. Genitofemoral nerve injury after laparoscopic varicocelectomy in adolescents. J Urol. 2008;180:2155–7. doi: 10.1016/j.juro.2008.07.068. [DOI] [PubMed] [Google Scholar]
- 109.Pini Prato A, MacKinlay GA. Is the laparoscopic Palomo procedure for pediatric varicocele safe and effective.Nine years of unicentric experience? Surg Endosc. 2006;20:660–4. doi: 10.1007/s00464-004-2252-x. [DOI] [PubMed] [Google Scholar]
- 110.Feber KM, Kass EJ. Varicocelectomy in adolescent boys: Long-term experience with the Palomo procedure. Urol. 2008;180:1657–9. doi: 10.1016/j.juro.2008.03.099. [DOI] [PubMed] [Google Scholar]


