Abstract
Objective:
To determine the prevalence of smoking among medical students at the medical college at King Fahad Medical City in Riyadh, and assess the association between smoking and socio-demographical factors, smoking contacts, reasons for smoking and attempts to quit.
Materials and Methods:
Cross-sectional survey in which anonymous, self-administered questionnaire was used to survey the cigarette smoking habits of the first- and second-year medical students in the Faculty of Medicine, King Fahad Medical City in June 2009.
Results:
Overall 39.8 % of the investigated students (153) had smoked before, and 17.6% were current smokers. The mean age of initiating smoking was 15.8 (±3.3). There were significantly more males than females. The most important reasons for smoking were leisure, imitation of other people and a means of relieving psychological pressure. Reasons for not smoking were mostly health and religion-based. Smokers tended to have friends who smoked.
Conclusion:
Cigarettes smoking is highly prevalent among medical students in the Faculty of Medicine, King Fahad Medical City. Contact with smokers particularly friends are the major risk factors for the initiation of the habit. Health and religious considerations are important motives for not smoking, quitting or attempting to quit. These findings can be of help in designing future intervention strategies.
Keywords: Association, medical students, prevalence, Riyadh, smoking
INTRODUCTION
The harmful consequences of smoking on health are well-documented. Data from recent studies confirm the quantitative relationship between smoking and many health hazards in the form of premature death and serious morbidity.[1–4] Unfortunately, smoking is on the rise in most developing countries, including Saudi Arabia, whereas in most developed countries there is a steady decline in its prevalence.[5] Cigarette production has been increasing worldwide at an average of 2.2% each year, outpacing the population growth rate of 1.7%.[5] According to a World Health Organization (WHO) report, tobacco use is predicted to cause 10 million deaths annually by the year 2030. Since smoking has a serious impact on public health, prevention programs have been given high priority in WHO policies.[6]
Health professionals educate their patients on the hazards of smoking. They usually serve as role models for their patients and the public and, therefore, play an important role in discouraging people from smoking. The participation of Health professionals in prevention and cessation counseling could be part of the strategies to minimize tobacco-related deaths in the future. For health professionals to convince others, they should be nonsmokers.
As future physicians, medical students are considered a primary target of tobacco prevention programs. They can therefore, play a positive role in preventing smoking among people in their community.[6] They may deliver health education, support anti-smoking policies and influence national and global tobacco control efforts.[6–8]
Previous studies in Saudi Arabia of medical students, in government colleges, showed that smoking was highly prevalent among male students.[9–13] This study aimed to determine the prevalence of smoking of medical students at the medical college at King Fahad Medical City in Riyadh, and assess the association between smoking and sociodemographical factors, contacts with smokers, reasons for smoking and attempts to stop smoking It is hoped that the results would help with the planning of corrective measures, as necessary.
MATERIALS AND METHODS
The Faculty of Medicine at King Fahad Medical City in Riyadh, Saudi Arabia, is a new medical college established in 2004, which recently, became part of King Saud bin Abdulaziz University for Health Sciences.
This was a cross-sectional study conducted in June 2009 in the Faculty of Medicine of King Fahad Medical City in Riyadh. All first and second-year medical students enrolled in the academic year 2009 were eligible for inclusion in the population for this study, and all students who were present during the study period were included.
The tool used in the study was an anonymous, self-administered questionnaire based on a modified WHO questionnaire to survey the smoking habits of health professionals, and was used previously by the authors to study the smoking habits of health students and adults in Riyadh.[14–16] The questions were grouped into categories relating to demographics, prevalence of cigarette smoking, reasons for smoking, reasons for nonsmoking and attempts to stop. Questionnaires were distributed during classes by the authors. Confidentiality was assured (written and verbal). The students were informed that the results would be used for the stated research purposes only, and their participation was voluntary. No identification was required.
The study was approved by the Institutional Review Board (IRB) of King Fahad Medical City and permission was obtained from related authorities. Completed questionnaires were collected and checked for completeness before being entered into a personal computer for analysis using the Statistical Package for SocialSciences (SPSS) version 17. Descriptive statistics and ‘t’- test, Mann-Whitney test and ANOVA or Kruskal Wallis were used as appropriate after checking for normality. Pearson's χ2 and Fisher's exact tests were used as appropriate, to study associations between smoking and categorical variables (sociodemographics). The level of significance was set at P<0.05 throughout the study. The number of participants’ responses used in the discrete statistical analyses varied because of missing data for certain variables.
The following definitions were used: ‘never been a smoker’ was a student who has never tried or experimented with tobacco smoking; ‘ever smoked’ was a student who had smoked before, even taking only one or two puffs; ‘current tobacco smoker’ was a student who had smoked on one or more days in the 30 days preceding the survey.
RESULTS
The total number of first- and second-year students who completed the questionnaire was 153 out of the 170 students enrolled in the academic year 2009, giving a 90% response rate. The nonparticipating students (17 students) did not appear to differ significantly from participants with respect to age, gender or grade. The study subjects were almost equally distributed between grades (77 first level and 76 second level). The sample was composed of 83 males (54.2%) and 70 females (45.8%). The mean age (±SD) of the total sample was 19.7 (±1.1) years, and the mean age of males and females was 20.1 (±1.0) and 19.2 (±0.95) years, respectively.
The age at which smoking was initiated ranged from 8 to 19 years with a mean of 15.8 years and a standard deviation of 3.3 years. For males, the mean age of initiating smoking was 16.6 years with standard deviation of 2.3 years, and for females the mean age was 14.0 years with standard deviation of 4.4 years. Cigarettes were the most common form of tobacco used by both males and females.
Table 1 shows the prevalence of ‘ever smoked’ and ‘current smoker’ according to the sociodemographical characteristics of the study subjects. The overall ‘ever smoked’ rate was 39.8% (48.2% of males, 28.6% of females) and the prevalence of ‘current smoker’ was 17.6% (28.9% of males, 4.3% of females). The gender differences were significant for both ‘ever smoked’ and ‘current smoker’ habit. Smoking prevalence increased with age and level of grade, but the differences were not significant. There were no significant differences regarding the patients’ level of education.
Table 1.
Ever smoked and current smokers habit according to sociodemographical characteristics
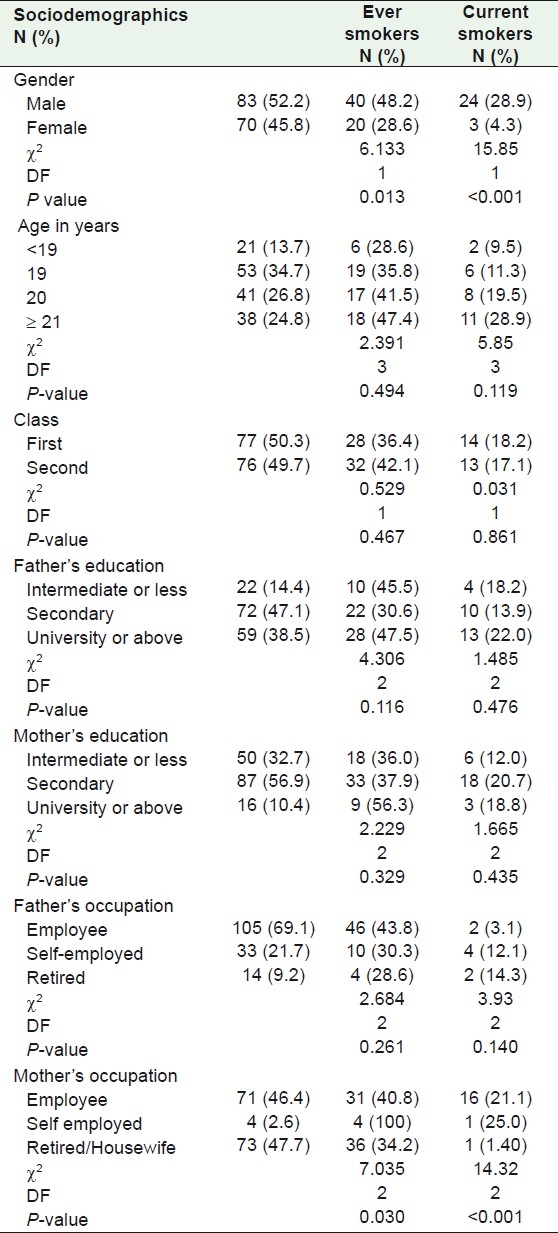
There were significant differences regarding mothers’ occupation between the ‘ever smoked’ and ‘current smoker’ subjects. Smoking rate was higher among students whose mothers were self-employed, and lower among those whose mothers were either housewives or had already retired from work.
The most important reasons for smoking were leisure followed by imitation of others or means of relieving psychological pressure, as depicted in Table 2. There were no significant differences regarding all the sociodemographical characteristics which we had studied.
Table 2.
The most important reasons for smoking (n=60)
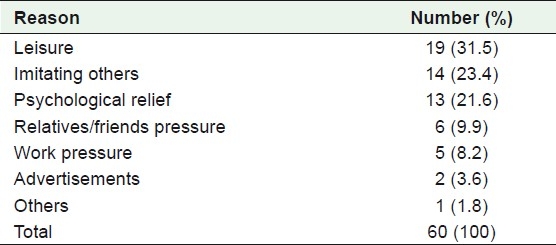
Table 3 shows the reasons for never smoking and for attempting to quit among ‘ever smoked’ subjects. Health considerations were the most important motives followed by religious considerations. Finance was not a motive to attempt to stop smoking and was of minimal importance to those who had never smoked. There were no significant differences among all the sociodemographical characteristics studied.
Table 3.
Reasons for never smoked and for ‘ever smoked’ attempting to quit*
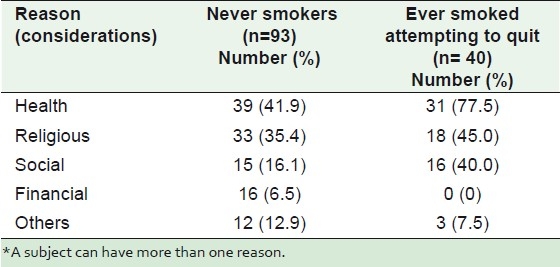
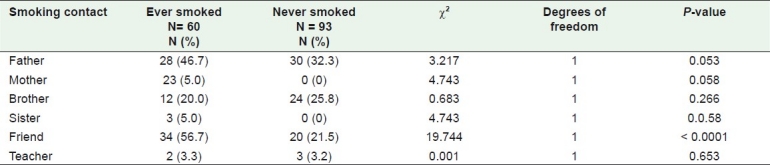
Table 4 shows the smoking contacts of all subjects according to their smoking habits. About 57% of the friends of those who had ever smoked were smokers themselves compared with only about 22% of the friends of those who had never smoked. There was no significant association between the smoking habits of subjects and the smoking habits of their other contacts such as parents, siblings, and teachers.
Table 4.
Smoking contacts according to ever smoking habit
DISCUSSION
The results of this study showed that cigarette smoking is a real problem among both male and female medical students. In this study, about 40% had smoked before and 18% were current smokers. This is less than the reported results of 33% of medical students at King Saud University in Riyadh who currently smoked. It is also higher than the median (13.5%) of previous studies performed in Saudi Arabia among medical students and other university students in the past two decades.[9–13] This variation in national smoking prevalence was also observed among medical students worldwide, with prevalence ranging from 3 to 58%.[7,18–23]
This study, also found significant gender differences in smoking status. Males were significantly more likely to smoke than females (48.2% of males and 28.6% of females belonged to the ‘ever smoked’ group and 28.9% of males and 4.3% of females were current smokers). Previous national, regional, and international studies reported similar trends among medical students.[9–13,15–23] It has been suggested that the lower rate of smoking among females was due to cultural reasons, since smoking is considered inappropriate behavior for women. This may account for the observation made of female medical students in the current and other studies.[7,21,24,25] Nevertheless, it is also possible that some females who did actually smoke may not have reported their habit during the survey for fear of being stigmatized.
According to this study, our students began smoking during adolescence or a young age. This is cause for concern because as documented in the literature, those who begin smoking during adolescence or at an early age are more likely to smoke daily in the future, and are less likely to stop smoking.[26]
The association of mothers’ occupation with medical students who had ‘ever smoked’ or were ‘current smokers’ observed in this study, is consistent with the previous study that reported that there was less likelihood of students whose parents were unemployed, retired or housewives, to report substance use.[27]
The reasons for smoking, in this study, were mostly imitation of others, leisure or relief of pressure. Studies in KSA and other communities showed that adolescents start smoking to enhance their social status for social influence, to relieve anxiety, for stimulation, out of curiosity, peer pressure or contact with smokers or as a result of the influence of advertisements.[9,28–30]
In the present study, health and religious considerations were identified as important motives for not initiating smoking and reasons to quit smoking. These results are in agreement with the findings of other previously reported studies.[9–11] Religious considerations are important for Muslims since Islamic teachings prohibit or at least strongly discourage indulging in the habit.
Financial considerations have been documented as important predictors of smoking. Taxation and an increase in the price of cigarettes have been used to decrease tobacco use, and has resulted in reduced tobacco-related morbidity and mortality.[31,32] Financial considerations were the least important reasons for initiating smoking and for giving up smoking in this and previous studies in Saudi Arabia. This may be because Saudi Arabia is a rich developing country with a high per capita income while tobacco products are among the least expensive commodities.
It has long been recognized that adolescents do not try cigarettesin a vacuum, and that contacts with people who smoked, like friends, classmates,siblings or parents, are the most consistent predictors of adolescentsmoking.[33–35] The present study showed that only smoking friends were significant correlates for initiating smoking.
The high prevalence of smoking among medical students in this and other studies is worrying. It may point to a degree of failure of the medical school curriculum to invoke health-conscious behaviors and attitudes among future physicians and health educators.[18] Therefore, a comprehensive intervention strategy is needed.
There were several limitations to this study. The findings are based on associations that are not directly causal in nature since the study is cross-sectional. Also, the data are based on self-reporting by medical students, and therefore under-reporting or over-reporting could not be ruled out. The study population was selected from one medical college, so findings can not be generalized to all other colleges in Saudi Arabia
CONCLUSIONS
Cigarette smoking is highly prevalent among both male and female medical students in the Faculty of Medicine, at King Fahad Medical City. Contacts who smoke are the major risk factor for initiating the habit. Health and religious considerations are important motives for not smoking, quitting or attempting to give up the habit.
All possible efforts and strategies should be considered to control smoking among medical students in Saudi Arabia and elsewhere. Medical and other health colleges should provide educational programs and teach specific courses on tobacco control in order to prepare and equip future health professionals with the knowledge and skills they need to intervene with smoking effectively.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Dhala A, Pinsker K, Prezant DJ. Respiratory health consequences of environmental tobacco smoke. Med Clin North Am. 2004;88:1535–5. doi: 10.1016/j.mcna.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. Br Med J. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doll R, Peto R, Boreham J, Sutherland I. Mortality from cancer in relation to smoking: 50 years observations on British doctors. Br J Cancer. 2005;92:426–9. doi: 10.1038/sj.bjc.6602359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362:847–52. doi: 10.1016/S0140-6736(03)14338-3. [DOI] [PubMed] [Google Scholar]
- 5.Crofton J, Simpson D. Tobacco: A global threat. London (UK): Macmillan; 2002. [Google Scholar]
- 6.WHO. Geneva: World Health Organization; 1997. Tobacco or health.A global status report. [Google Scholar]
- 7.Smith D, Leggat P. An international review of tobacco smoking among medical students. J Postgrad Med. 2007;53:55–62. doi: 10.4103/0022-3859.30333. [DOI] [PubMed] [Google Scholar]
- 8.Saloojee Y, Steyn K. Educating medical students about tobacco. S Afr Med J. 2005;95:330–1. [PubMed] [Google Scholar]
- 9.Bassiony M. Smoking in Saudi Arabia. Saudi Med J. 2009;30:876–81. [PubMed] [Google Scholar]
- 10.Jarallah JS. Smoking habits of medical students at King Saud University, Riyadh. Saudi Med J. 1992;13:510–3. [Google Scholar]
- 11.Al-Turki YA. Smoking habits among medical students in Central Saudi Arabia. Saudi Med J. 2006;27:700–3. [PubMed] [Google Scholar]
- 12.Vohra M. Smoking habits of preclinical Saudi medical students. Pak J Med Sci. 2009;25:906–11. [Google Scholar]
- 13.Al-Haqwi A, Tamim H, Asery A. Knowledge, attitude and practice of tobacco smoking by medical students in Riyadh, Saudi Arabia. Ann Thorac Med. 2010;5:145–8. doi: 10.4103/1817-1737.65044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guidelines for conduct of tobacco smoking among professionals. WHO Document WHO/SMO/84. 1984;1:1–19. [Google Scholar]
- 15.Saeed A, Al Johali E, Al Shahri A. Smoking habits of students in Secondary Health Institutes in Riyadh City. J R Soc Health. 1993;113:132–5. doi: 10.1177/146642409311300308. [DOI] [PubMed] [Google Scholar]
- 16.Saeed A, Khoja T, Khan S. Smoking behaviour and attitudes among adult Saudi nationals in Riyadh City, Saudi Arabia. Tobacco Control. 1996;5:215–9. doi: 10.1136/tc.5.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrabi I, Ghannem H, Kacem M, Gaha R, Ben Abdelaziz A, Tessier JF. Medical students and tobacco in 2004: A survey in Sousse, Tunisia. Int J Tuberc Lung Dis. 2006;10:328–32. [PubMed] [Google Scholar]
- 18.Almerie M, Matar H, Salam M, Morad A, Abdulaal M, Koudsi A, et al. Cigarettes and waterpipe smoking among medical students in Syria: A cross-sectional study. Int J Tuberc Lung Dis. 2008;12:1085–91. [PMC free article] [PubMed] [Google Scholar]
- 19.Siemińska A, Jassem-Bobowicz J, Uherek M, Wilanowski T, Nowak R, Jassem E. Medical students’ attitudes towards tobacco smoking at the first and sixth year of their studies 2002-2008. Pneumonol Alergol Pol. 2009;77:371–9. [PubMed] [Google Scholar]
- 20.Mostafa S, Shokaeir N. Smoking-related behaviour and attitudes among medical students in Alexandria. J Egypt Public Health Assoc. 2002;77:1–2. [PubMed] [Google Scholar]
- 21.Khan FM, Husain SJ, Laeeq A, Awais A, Hussain SF, Khan JA. Smoking prevalence, knowledge and attitudes among medical students in Karachi, Pakistan. Eastern Mediterranean Health J. 2005;11:5–6. [PubMed] [Google Scholar]
- 22.Smith DR, Wei N, Wang RS. Tobacco smoking habits among Chinese medical students and their need for health promotion initiatives. Health Promot J Austr. 2005;16:233–5. doi: 10.1071/he05233. [DOI] [PubMed] [Google Scholar]
- 23.Senol Y, Donmez L, Turkay M, Aktekin M. The incidence of smoking and risk factors for smoking initiation in medical faculty students: Cohort study. BMC Public Health. 2006;6:128. doi: 10.1186/1471-2458-6-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramakrishna GS, Sankara Sarma P, Thankappan KR. Tobacco use among medical students in Orissa. Natl Med J India. 2005;18:285–9. [PubMed] [Google Scholar]
- 25.Tessier J, Fréour P, belougne D, Crofton J. Smoking habits and attitudes of medical students towards smoking and antismoking campaigns in nine asian countries. Int J Epidemiol. 1992;21:298–304. doi: 10.1093/ije/21.2.298. [DOI] [PubMed] [Google Scholar]
- 26.Breslau N, Peterson E. Smoking cessation in young adults: Age at initiation of cigarette smoking and other suspected influences. Am J Public Health. 1996;86:214–20. doi: 10.2105/ajph.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soteriades E, DiFranza J. Parent's socioeconomic status, adolescents’ disposable income, and adolescents’ smoking status in Massachusetts. Am J Public Health. 2003;93:1155–60. doi: 10.2105/ajph.93.7.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piasecki T, Richardson A, Smith S. Self-monitored motives for smoking among college students. Psychol Addict Behav. 2007;21:328–37. doi: 10.1037/0893-164X.21.3.328. [DOI] [PubMed] [Google Scholar]
- 29.Labib N, Radwan G, Mikhail N, Mohamed M, El Setouhy M, Loffredo C, et al. Comparison of cigarette and water pipe smoking among female university students in egypt. Nicotine Tob Res. 2007;9:591–6. doi: 10.1080/14622200701239696. [DOI] [PubMed] [Google Scholar]
- 30.Yaacob I, Abdullah Z. Smoking behavior, knowledge and opinion of medical students. Asia Pac J Public Health. 1994;7:88–91. doi: 10.1177/101053959400700202. [DOI] [PubMed] [Google Scholar]
- 31.State cigarette excise taxes - United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:385–8. [PubMed] [Google Scholar]
- 32.Hu TW, Mao Z, Shi J, Chen W. The role of taxation in tobacco control and its potential economic impact in China. Tob Control. 2010;19:58–64. doi: 10.1136/tc.2009.031799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kobus K. Peers and adolescent smoking. Addiction. 2003;98:37–55. doi: 10.1046/j.1360-0443.98.s1.4.x. [DOI] [PubMed] [Google Scholar]
- 34.Avenevoli S, Merikangas KR. Familial influences on adolescent smoking. Addiction. 2003;98:1–20. doi: 10.1046/j.1360-0443.98.s1.2.x. [DOI] [PubMed] [Google Scholar]
- 35.Bauman KE, Carver K, Gleiter K. Trends in parent and friend influence during adolescent: The case of adolescent cigarette smoking. Addict Behav. 2001;26:349–61. doi: 10.1016/s0306-4603(00)00110-6. [DOI] [PubMed] [Google Scholar]


