Hypothyroidism is a common clinical entity, occurring in 2% to 3% of the Canadian population.1 Primary hypothyroidism is most common, with dysfunction occurring at the level of the thyroid gland.2 In secondary or tertiary hypothyroidism (central hypothyroidism), the defect is at the pituitary, hypothalamus, or hypothalamic portal circulation level.3
Most hypothyroid patients are treated with levothyroxine; thyroid-stimulating hormone (TSH) levels are checked to monitor correct treatment doses. However, the role of TSH in central hypothyroidism is more limited, and primary reliance on its measurement might result in incorrect diagnosis or treatment. The following case illustrates this key concept.
Case description
A 43-year-old man presented with a 1-year history of horizontal diplopia and headaches. He also complained of memory impairment, erectile dysfunction, and constipation. He had a history of hypertension and hyperlipidemia, and a 40-pack-year history of smoking. He was not taking any medications.
Physical examination revealed abducent nerve palsy on the left side and dry skin. Magnetic resonance imaging of the head demonstrated a uniform enhancing lesion with a diameter of 4 cm involving the left medial sphenoidal wing, temporal lobe, cavernous sinuses, brainstem, and sella turcica. A transsphenoidal biopsy was performed, and a mesenchymal chondrosarcoma was diagnosed.
To evaluate the patient’s pituitary function, laboratory testing was completed. This revealed a TSH level of 0.1 mU/L (normal 0.27 to 4.2 mU/L), a free thyroxine (T4) level of 13 pmol/L (normal 10 to 24 pmol/L), and a free triiodothyronine (T3) level of 3.8 pmol/L (normal 3 to 6.5 pmol/L). His morning cortisol level was low, at 95 nmol/L; other values included a serum testosterone level of 0.3 nmol/L (normal 6.3 to 26 nmol/L), a luteinizing hormone level of 0.2 IU/L (normal 1.5 to 9 IU/L), and a follicle-stimulating hormone level of 1.3 IU/L (normal 1 to 18 IU/L). As these results indicated anterior hypothyroidism, hydrocortisone (initially 50 mg twice daily) and levothyroxine (starting at 50 μg daily) were initiated.
Because of progressive cranial neuropathy and right hemiparesis, the patient underwent radiotherapy (45 Gy over 7 weeks). He was discharged to a rehabilitation unit where thyroid hormone replacement therapy was monitored. Based on a low (or suppressed) TSH level (0.06 mU/L), his levothyroxine dose was decreased in an attempt to maintain a TSH level in the normal range.
Four months later, he complained of constipation, cold intolerance, and increasing weight. Only TSH measurement was being used to monitor his thyroid function. Therefore, free T4 and T3 levels and TSH levels were checked once more. Free T4 levels were found to be low at 8 pmol/L, free T3 levels were low at 2.3 pmol/L, and TSH levels were normal at 1.96 mU/L, suggesting an insufficient thyroid hormone dose. His levothyroxine dose was increased to 100 μg daily. Because his serum testosterone level was low at less than 0.3 nmol/L, with low luteinizing hormone (0.1 IU/L) and follicle-stimulating hormone (1.7 IU/L) levels, testosterone replacement therapy was initiated, with 150-mg testosterone enanthate injections administered intramuscularly every 2 weeks.
After his dose of levothyroxine was increased, his constipation and fatigue improved and he was able to increase his physical activity, aiding in his rehabilitation. Results of repeat bloodwork 2 months later showed a TSH level of 0.15 mU/L and both free T4 and free T3 levels in the reference range (11 pmol/L and 3.1 pmol/L, respectively).
The patient’s levothyroxine dose was subsequently adjusted to keep his free T4 and T3 levels in the reference range. Additionally, it was recommended that levothyroxine not be administered simultaneously with calcium supplementation, as concomitant calcium administration can reduce the intestinal absorption of levothyroxine.4
Discussion
This case illustrates the importance of the accurate diagnosis, treatment, and monitoring of central hypothyroidism.
Diagnosis of central hypothyroidism
As in primary hypothyroidism, a detailed history and physical examination are important to diagnosis. Cold intolerance and weight gain are common complaints (Box 1).5 Compared with primary hypothyroidism, however, clinical manifestations of central hypothyroidism might be masked by symptoms of coexisting hormone deficiencies such as hypoadrenalism and hypogonadism.2 Thus, biochemical diagnosis is critical in this group.
Box 1. Signs and symptoms of hypothyroidism.
|
Data from Garber et al, 2006.5
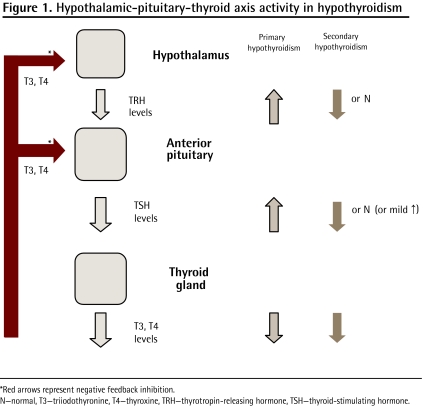
Primary hypothyroidism is usually diagnosed based on an elevated TSH level. In this situation, the failure of the thyroid gland to secrete sufficient thyroid hormone results in decreased levels of T3 and T4. In turn, there is less negative feedback inhibition at the hypothalamus and pituitary, causing TSH levels to increase (Figure 1). Increased TSH levels are therefore indicative of the diagnosis, and normalization is seen during adequate treatment.
Figure 1.
Hypothalamic-pituitary-thyroid axis activity in hypothyroidism
*Red arrows represent negative feedback inhibition.
N—normal, T3—triiodothyronine, T4—thyroxine, TRH—thyrotropin-releasing hormone, TSH—thyroid-stimulating hormone.
In contrast, owing to hypothalamic or pituitary failure, TSH levels might not increase in response to low T3 and T4 levels.6 Thyroid-stimulating hormone levels can, in fact, be in the low, normal, or elevated range.3 This is because TSH pulse frequency and amplitude might be maintained, and additionally, its biologic activity might be reduced with its immunoactivity still retained.2 Furthermore, other hormone deficiencies can affect its measure.7 Therefore, for the diagnosis of central hypothyroidism, one needs findings of low free T3 and T4 levels together with low or “inappropriately” normal TSH concentration in the context of hypothalamic-pituitary disease.3
Central hypothyroidism is most often caused by pituitary mass lesions. Radiation is another culprit, with hypothyroidism occurring in 3% to 9% of patients who undergo pituitary radiation8 and in up to 5% of patients who receive radiation for extracranial head and neck tumours.2 The main causes of central hypothyroidism are listed in Box 2.7
Box 2. Causes of central hypothyroidism.
|
Data from Yamada and Mori, 2008.7
Monitoring therapy
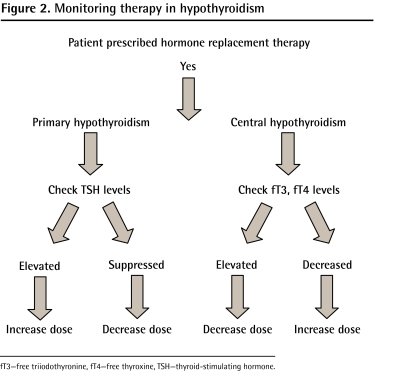
The treatment of choice for hypothyroidism is levothyroxine. The average dose is 1.6 μg per kilogram of body weight, but there is considerable variation among individuals. The adequacy of the replacement dose must be checked frequently (every 4 to 8 weeks), especially at the beginning of therapy. Once the correct dose has been established, thyroid hormone levels should be measured once or twice per year. For the reasons cited above, TSH levels cannot be used to monitor therapy in central hypothyroidism. The most reliable marker is serum free T4 levels (Figure 2).9 Free T3 levels should also be measured; however, they tend to remain in the normal range and are less useful. It is also advisable to concomitantly measure levels of TSH.
Figure 2.
Monitoring therapy in hypothyroidism
fT3—free triiodothyronine, fT4—free thyroxine, TSH—thyroid-stimulating hormone.
A common treatment target is maintenance of free T4 and T3 levels in the upper half of the normal range, with some adjustment based on the patient’s clinical symptoms. In addition, treatment of other pituitary hormone deficiencies might affect dosing9 and should prompt reevaluation of thyroid hormone test results 2 to 4 months later. Most important, a low TSH level should not be seen as an indicator of a supratherapeutic dose of levothyroxine.
Conclusion
Accurate diagnosis and surveillance of patients being treated for central hypothyroidism is of great importance. Measuring only TSH levels is not sufficient, and can lead to incorrect treatment decisions. One must also monitor free T3 and T4 levels, and pay special attention to clinical signs and symptoms of hypothyroidism or hyperthyroidism.
EDITOR’S KEY POINTS
To diagnose central hypothyroidism, look for findings of lower free triiodothyronine and thyroxine levels together with low or inappropriately normal thyroid-stimulating hormone levels in a clinical situation suggestive of the disease.
The role of thyroid-stimulating hormone alone in monitoring treatment of patients with central hypothyroidism is limited; aim for the maintenance of free triiodothyronine and thyroxine levels in the upper half of the normal range, with adjustment of treatment based on the patient’s symptoms
POINTS DE REPÈRE DU RÉDACTEUR
Pour diagnostiquer l’hypothyroïdie centrale, il faut constater des niveaux de triiodothyronine et de thyroxine libres plus bas, combinés à des niveaux faibles ou inopportunément normaux de thyréostimuline dans une situation clinique qui suggère la maladie.
Le rôle de la thyréostimuline à elle seule dans la surveillance des patients atteints d’hypothyroïdie centrale est limité; il faut se fixer comme objectif de maintenir les niveaux de triiodothyronine et de thyroxine libres dans la moitié supérieure de l’échelle des valeurs normales et ajuster le traitement en se fondant sur les symptômes du patient.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Competing interests
None declared
References
- 1.Thyroid Foundation of Canada [website] About thyroid disease. Manotick, ON: Thyroid Foundation of Canada; 2011. Available from: www.thyroid.ca/thyroid_disease.php. Accessed 2011 Mar 21. [Google Scholar]
- 2.Bhandare N, Kennedy L, Malyapa RS, Morris CG, Mendenhall WM. Primary and central hypothyroidism after radiotherapy for head-and-neck tumors. Int J Radiat Oncol Biol Phys. 2007;68(4):1131–9. doi: 10.1016/j.ijrobp.2007.01.029. [DOI] [PubMed] [Google Scholar]
- 3.Alexopoulou O, Beguin C, De Nayer P, Maiter D. Clinical and hormonal characteristics of central hypothyroidism at diagnosis and during follow-up in adult patients. Eur J Endocrinol. 2004;150(1):1–8. doi: 10.1530/eje.0.1500001. [DOI] [PubMed] [Google Scholar]
- 4.Mazokopakis EE, Giannakopoulos TG, Starakis IK. Interaction between levothyroxine and calcium carbonate. Can Fam Physician. 2008;54:39. [PMC free article] [PubMed] [Google Scholar]
- 5.Garber JR, Hennessey JV, Liebermann JA, 3rd, Morris CM, Talbert RL. Managing the challenges of hypothyroidism. J Fam Pract. 2006;55(6):S1–8. [PubMed] [Google Scholar]
- 6.Lania A, Persani L, Beck-Peccoz P. Central hypothyroidism. Pituitary. 2008;11(2):181–6. doi: 10.1007/s11102-008-0122-6. [DOI] [PubMed] [Google Scholar]
- 7.Yamada M, Mori M. Mechanisms related to the pathophysiology and management of central hypothyroidism. Nat Clin Pract Endocrinol Metab. 2008;4(12):683–94. doi: 10.1038/ncpendmet0995. [DOI] [PubMed] [Google Scholar]
- 8.Darzy KH, Shalet SM. Hypopituitarism following radiotherapy revisited. Endocr Dev. 2009;15:1–24. doi: 10.1159/000207607. [DOI] [PubMed] [Google Scholar]
- 9.Ferretti E, Persani L, Jaffrain-Rea ML, Giambona S, Tamburrano G, Beck-Peccoz P. Evaluation of the adequacy of levothyroxine replacement therapy in patients with central hypothyroidism. J Clin Endocrinol Metab. 1999;84(3):924–9. doi: 10.1210/jcem.84.3.5553. [DOI] [PubMed] [Google Scholar]