Abstract
Problem addressed
A well documented gap remains between evidence and practice for clinical practice guidelines in cardiovascular disease (CVD) care.
Objective of program
As part of the Champlain CVD Prevention Strategy, practitioners in the Champlain District of Ontario launched a large quality-improvement initiative that focused on increasing the uptake in primary care practice settings of clinical guidelines for heart disease, stroke, diabetes, and CVD risk factors.
Program description
The Champlain Primary Care CVD Prevention and Management Guideline is a desktop resource for primary care clinicians working in the Champlain District. The guideline was developed by more than 45 local experts to summarize the latest evidence-based strategies for CVD prevention and management, as well as to increase awareness of local community-based programs and services.
Conclusion
Evidence suggests that tailored strategies are important when implementing specific practice guidelines. This article describes the process of creating an integrated clinical guideline for improvement in the delivery of cardiovascular care.
Résumé
Problème à l’étude
Il existe toujours un écart bien documenté entre les données probantes et la pratique en ce qui concerne les directives de pratique clinique pour traiter les maladies cardiovasculaires (MCV).
Objectif du programme
En lien avec le projet Stratégie de prévention des MCV dans la région de Champlain, des médecins du district de la région de Champlain, Ontario, ont lancé un vaste projet d’amélioration de la qualité par une meilleure application des directives cliniques relatives aux maladies cardiaques, au diabète, aux accidents vasculaires cérébraux et aux facteurs de risque des MCV.
Description du programme
Le projet Collectif concernant les directives sur la prévention et la gestion des maladies cardiovasculaires dans la région de Champlain est une ressource informatique à l’intention des cliniciens de première ligne qui pratiquent dans le district Champlain. Les directives ont été élaborées par plus de 45 experts locaux afin de mettre à jour les plus récentes stratégies fondées sur des preuves pour la prévention et le traitement des MCV et pour faire mieux connaître les programmes et services communautaires locaux.
Conclusion
Les données laissent entendre qu’il est important d’utiliser des stratégies adaptées lorsqu’on veut instaurer des directives de pratique spécifiques. Cet article décrit le processus servant à créer des directives cliniques intégrées pour améliorer les soins cardiovasculaires.
Clinical practice guidelines, based on best evidence and clinical expertise, are available to assist practitioners in optimizing the management of specific health conditions and risk factors. Most guidelines are developed at the national level by specialized knowledge experts using validated systematic procedures to review and analyze the most current evidence available.1–9 Typically guidelines include broad-based, scientifically valid recommendations that are targeted toward a wide variety of user groups.10
Despite the advantages of nationally developed guidelines, there remain problems around implementation, particularly for specific user groups.10 For example, family physicians’ scope of practice requires working knowledge of multiple guidelines focused on various aspects of cardiovascular disease (CVD) prevention and management—some of which might contain competing or conflicting recommendations. Given the reality of time and resource demands, it can be difficult for family practitioners to translate guidelines into actions that are relevant to their specific practice conditions and patient populations. Consequently, there remains a well documented gap between evidence and practice in the field of CVD care.11
Program objective
The Champlain CVD Prevention Network (CCPN) is an alliance of health partners from key sectors involved in the prevention and management of CVD, including public health, community organizations, specialty care, academic institutions, the primary care community, and health care institutions. The network’s mandate is to develop integrated approaches to the prevention and management of CVD within the Champlain Local Health Integration Network (LHIN). The CCPN is providing leadership for a 5-year regional quality-improvement initiative, which aims to increase the delivery of evidence-based strategies to prevent and manage CVD and its associated risk factors in the Champlain District of Ontario.
The initial strategic planning process identified a need to facilitate the uptake of evidence-based CVD prevention and management recommendations in clinical settings. Given the importance of the primary care setting for the prevention and management of CVD, it was identified as an early target for collaborative action. A large-scale, community-based, knowledge translation initiative was proposed to support the delivery of evidence-based strategies for CVD prevention in primary care. Central to this initiative was a need to develop evidence-based CVD prevention and management guidelines that were relevant to primary care practitioners in this region.
The Champlain Primary Care CVD Prevention and Management Guideline project was undertaken to support primary care practitioners in the delivery of evidence-based strategies to prevent and manage CVD. Specifically, the project aimed to summarize and tailor evidence-based strategies for the prevention and management of CVD to primary care practitioners working in the Champlain LHIN. The goal of the guideline was to harmonize management and target outcomes for multiple vascular conditions (eg, coronary artery disease, transient ischemic attack or stroke, diabetes, peripheral vascular disease), summarize evidence-based strategies for the detection and management of these vascular conditions and their associated risk factors (eg, blood pressure, cholesterol, smoking, physical inactivity, obesity), and maximize the use of local resources and tools in the provision of care.
Program description
Formation of evidence-monitoring committees
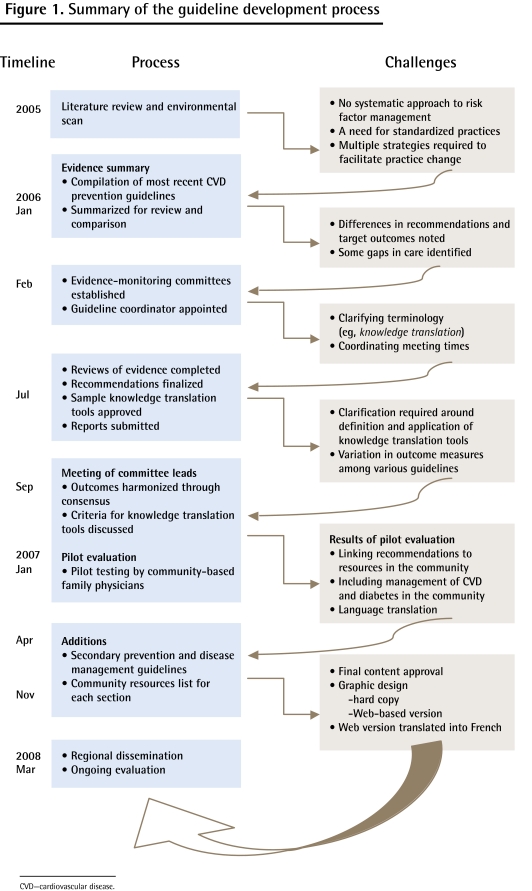
In order to develop the guideline, evidence-monitoring committees and a guideline coordinator were established for serious CVD risk factors and conditions. (Figure 1 provides a flowchart of the guideline development process.) The overall purpose of the evidence-monitoring committees was to critically review current clinical practice guidelines and provide recommendations for implementation at the primary care level. A total of 8 evidence-monitoring committees were established, with more than 45 local experts and opinion leaders sitting as members. Several committee members were also involved in national guideline working groups within their areas of expertise. Each committee was led by an established knowledge expert known for his or her work in the particular area of vascular prevention and management. Other committee members included experts from the academic or specialty setting and from the community or primary practice setting. The guideline coordinator attended each committee meeting.
Figure 1.
Summary of the guideline development process
CVD—cardiovascular disease.
Evidence-monitoring committee deliberations
Committee members reviewed the most recent Canadian guidelines, as well as other international guidelines or sources of evidence as required. Gaps or limitations in the guidelines were identified, and evidence from alternate sources was considered as needed. Practice recommendations from the guidelines applicable to primary care were extracted and discussed with respect to usual practice in the Champlain LHIN. Each committee submitted a report that summarized recommendations for the diagnosis and management of the specific risk factor or condition. Once all reports were submitted, the leads of each committee came together with the objective of harmonizing management overlaps and target outcome measures. The goal was to ensure consistent recommendations and targets throughout each prevention and management area.
Guideline harmonization
The review process demonstrated that recommendations were consistent across the 8 groups with a few exceptions. For example, one inconsistency noted was that of albumin-to-creatinine ratio targets and estimated glomerular filtration rate referral parameters, specifically for individuals with diabetes. Collaboration between the nephrology group and the diabetes group resulted in the decision to use recommendations from the nephrology guideline.8
Another difference noted involved waist circumference targets, specifically for individuals diagnosed with dyslipidemia. Waist circumference recommendations vary not only across guidelines but also across various ethnic groupings. The Adult Treatment Panel III12 recommends a waist circumference below 102 cm for men and 88 cm for women; however, the Canadian Cardiovascular Society Dyslipidemia Working Group6 stated that waist circumference values varied across cultures, specifically for individuals of European background, but any waist measurement greater than 94 cm for men or 80 cm for women was considered to increase risk of heart disease and other health concerns. Additionally, this group recommends using the International Diabetes Federation waist circumference targets for specific ethnic groups. Although the final guideline harmonization includes the Adult Treatment Panel III targets for practical screening purposes, it refers to the Dyslipidemia Working Group recommendations for target waist circumference across all specific ethnic groups.
Algorithm development
Based on the reports submitted by each evidence-monitoring committee, a brief 1- to 2-page algorithm was developed for the detection and management of each risk factor and disease area included in the guideline. Supplemental information was summarized as required on protocols such as obtaining an accurate waist circumference or proper blood pressure measurement. Pharmacotherapy summary charts were created as a quick reference for important evidence-based medications used in the prevention and management of CVD. All sections of the guideline were organized using a common presentation template to facilitate ease of use by busy clinicians.
Pilot testing
The initial guideline draft, approved by leaders from all 8 evidence-monitoring committees, was then pilot-tested by a small group of family physicians and modified based on feedback received. Pilot testing identified primary care clinicians’ lack of awareness of available community-based programs and services to support CVD prevention and management.
Community resources
In order to make the guideline relevant to local physicians, a database of community resources pertinent to each vascular condition and risk factor was developed. The purpose of the community resources database was to highlight opportunities for physicians to integrate resources from the community into patient management and care interventions. Community resources included specialty clinics and associated referral guidelines, available community programs or patient education sessions, or any other community resources that could facilitate patient management. The database included program descriptions, referral information, and costs of each program or service. The final result was a harmonized, overall vascular management strategy tailored to primary care practitioners in the Champlain LHIN.
Dissemination strategy
The final guideline document was integrated into CCPN’s overall knowledge translation strategy and is primarily being implemented through the Improved Delivery of Cardiovascular Care (IDOCC) project. This quality-improvement initiative, which is being delivered to 84 primary care practices throughout the Champlain LHIN, aims to increase uptake of evidence-based practice for the prevention and management of patients with or at high risk of developing CVD. The IDOCC project centres on the use of an intervention model called outreach facilitation, in which health professionals skilled in facilitating practice change serve as expert resources to primary care practices. In this model, the facilitators provide hands-on support in the following areas:
practice performance assessment, feedback, and goal setting;
clinical, technical, organizational, and practical advice; and
encouragement to move through the implementation of system change.
The guideline is an important resource used by the facilitators, as it provides intervention strategies, target outcome measurements, and associated tools used to promote practice change. One aspect of evaluating the IDOCC program and its effect on patient care will involve using data collected before and after facilitation through medical chart audits to measure physician adherence to the recommendations outlined in the guideline.
A copy of the guideline was distributed to each primary care practitioner working in the Champlain District in 2009, as well as specialists involved in CVD prevention and management. In total, 1300 guidelines were distributed. A Web-based version of the guideline was also created and can be accessed at www.idocc.ca. The guideline will be updated every 2 years to ensure that it reflects the latest evidence for the prevention, detection, and treatment of CVD, as well as new programs and services to support practitioners within the region.
Discussion
Local translation of nationally developed clinical practice guidelines is a well accepted knowledge translation strategy that confers several advantages for primary care practitioners.13 Local translation involves extracting the recommendations from evidence-based guidelines that are relevant to the specific practice population. Creating local care protocols allows for tailored interventions that are based on evidence and that integrate existing community resources and links into the management strategy. Localized guidelines are usually developed by a working group that consists not only of knowledge experts but also members of the target group, practice leaders, and technical coordinators. Development of integrated management strategies allows for the identification of specific outcome criteria and indicators that, in turn, can be used as feedback for future guideline revision. Overall, this methodology enables target users to translate general, evidence-based interventions into care strategies that maximize community links and target the specific practice population.13
Limitations
Grol cautions that guidelines often do not meet criteria to be considered valid. For instance, guidelines should be developed independent of specific interests, be rigorous, and have an effect on local care.14 Similarly, recommendations from guidelines are not necessarily applied in practice.15 These limitations support processes that integrate guidelines with other quality-improvement measures to make them more relevant and effective. What makes our research different is the local context and use of outreach facilitation to aid the use of such guidelines.
The evidence strongly suggests that in order to create sustainable change in practice behaviour, dissemination of quality-improvement interventions must involve a multifaceted, individualized, system-level approach.16 This involves the tailoring of tools and strategies for guideline implementation to the practice’s unique motivations, structures, and processes, thereby making their adoption into daily routine much more likely.
Conclusion
The Champlain Primary Care CVD Prevention and Management Guideline was developed using a credible knowledge translation strategy known to be particularly useful in primary care practice settings. The guideline is part of an ongoing regional quality-improvement initiative that is focused on facilitating long-term improvement in adoption of evidence-based primary CVD care. The methodology used in the development of the guideline might be useful to other practitioners involved in real-world strategies for the transfer of evidence-based care into practice.
EDITOR’S KEY POINTS
Given the reality of time and resource demands, it can be difficult for family practitioners to translate guidelines into actions that are relevant to their specific practice conditions and patient populations. Consequently, there remains a well documented gap between evidence and practice in cardiovascular disease (CVD) care.
The Champlain Primary Care CVD Prevention and Management Guideline project was undertaken to support primary care practitioners in the delivery of evidence-based strategies to prevent and manage CVD. The guideline is part of an ongoing regional quality-improvement initiative that focuses on facilitating long-term improvement in adoption of evidence-based primary CVD care.
POINTS DE REPÈRE DU RÉDACTEUR
Compte tenu des contraintes de temps et de ressources, il peut être difficile pour les médecins de famille de traduire les directives cliniques en des actions qui soient pertinentes à leurs conditions de pratique et à leur clientèle. Il demeure donc un écart bien documenté entre les données probantes et leur application dans le domaine du traitement des maladies cardiovasculaires (MCV).
Le projet Collectif concernant les directives sur la prévention et la gestion des maladies cardiovasculaires dans la région de Champlain a été instauré pour appuyer les médecins de première ligne dans l’utilisation de stratégies fondées sur des données probantes pour prévenir et traiter les MCV. Le Collectif sur la prévention et la gestion des maladies cardiovasculaires dans la région de Champlain fait partie d’un projet régional déjà en cours qui vise une amélioration de la qualité des soins en faciliteanr une amélioration à long terme des soins primaires pour les MCV fondés sur des preuves.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Tobacco Use and Dependence Guideline Panel . Treating tobacco use and dependence: 2008 update. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available from: www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=hsahcpr&part=A28163. Accessed 2011 May 4. [Google Scholar]
- 2.Arnold JM, Liu P, Demers C, Dorian P, Giannetti N, Haddad H, et al. Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol. 2006;22(1):23–45. doi: 10.1016/s0828-282x(06)70237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canadian Diabetes Association Clinical Practice Guideline Expert Committee Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32(Suppl 1):S1–201. doi: 10.1016/j.jcjd.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Canadian Hypertension Education Program . CHEP recommendations for the management of hypertension 2006. Markham, ON: Canadian Hypertension Education Program; 2006. [Google Scholar]
- 5.Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary] CMAJ. 2007;176(8):S1–13. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McPherson R, Frohlich J, Fodor G, Genest J. Canadian Cardiovascular Society position statement—recommendations for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease. Can J Cardiol. 2006;22(11):913–27. doi: 10.1016/s0828-282x(06)70310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.PACE Canada . Health provider’s guide to counselling for healthy active living. Ottawa, ON: PACE Canada; 2000. [Google Scholar]
- 8.Society of Nephrology . Care and referral of adult patients with reduced kidney function. Position paper from the Canadian Society of Nephrology. St John’s, NL: Society of Nephrology; 2006. Available from: www.cdha.nshealth.ca/default.aspx?page=DocumentRender&doc.Id=1690. Accessed 2011 May 4. [Google Scholar]
- 9.Canadian Stroke Strategy . Canadian best practice recommendations for stroke care 2006. Ottawa, ON: Canadian Stroke Network, Heart and Stroke Foundation of Canada; 2006. Available from: www.strokecenter.org/prof/CSSManualENG_WEB_Sept07.pdf. Accessed 2011 May 4. [Google Scholar]
- 10.Hudon E, Beaulieu MD, Roberge D. Integration of the recommendations of the Canadian Task Force on Preventive Health Care: obstacles perceived by a group of family physicians. Fam Pract. 2004;21(1):11–7. doi: 10.1093/fampra/cmh104. [DOI] [PubMed] [Google Scholar]
- 11.Tremblay GJ, Drouin D, Parker J, Monette C, Cote DF, Reid RD. The Canadian Cardiovascular Society and knowledge translation: turning best evidence into best practice. Can J Cardiol. 2004;20(12):1195–8. [PubMed] [Google Scholar]
- 12.National Cholesterol Education Program . Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Final report. Bethesda, MD: National Cholesterol Education Program, National Heart, Lung, and Blood Institute, and National Institutes of Health; 2002. Available from: www.nhlbi.nih.gov/guidelines/cholesterol/atp3full.pdf. Accessed 2011 May 4. [Google Scholar]
- 13.Grol R, Wensing M, Eccles M. Improving patient care. The implementation of change in clinical practice. Toronto, ON: Elsevier; 2005. [Google Scholar]
- 14.Grol R. Has guideline development gone astray? Yes. BMJ. 2010;340:c306. doi: 10.1136/bmj.c306. [DOI] [PubMed] [Google Scholar]
- 15.Grol R, Buchan H. Clinical guidelines: what can we do to increase their use? Med J Aust. 2006;185(6):301–2. doi: 10.5694/j.1326-5377.2006.tb00580.x. [DOI] [PubMed] [Google Scholar]
- 16.Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39(8 Suppl 2):112–45. [PubMed] [Google Scholar]