Abstract
Purpose
The use of disposable absorbent products by community-dwelling people with fecal incontinence was described. Differences in product use or evaluation based on sex, age, or severity of fecal incontinence were evaluated. Suggestions for modifying absorbent products to be more suitable for fecal incontinence were described.
Methods
A survey was administered to 189 community-living individuals with fecal incontinence at the start of a clinical trial about the effects of dietary fiber on fecal incontinence
Results
An absorbent product was used to manage fecal incontinence by 45% (86/189) of respondents. More women (88%, 76/86, p = .009) and older persons 65+ years (44%, 38/86, p = .001) wore an absorbent product. Participants who wore an absorbent product for fecal incontinence had a higher (worse) usual fecal incontinence severity score (median 4.75, range 1–27, p = .006). Sixty three users wore pantiliners and were the only ones who used more than three products per day. Feminine hygiene products were worn more than incontinence products. Half of users were satisfied with the product they used. Evaluations of product features differed by type of product; odor control had some of the lowest ratings.
Conclusions
Community-living individuals with FI, especially women and older individuals, tend to wear absorbent products. Perceptions of FI severity, preference, leakage of liquid stool, and presence of urinary incontinence influence the product type and pattern of wear. Participants report that modification of several features of absorbent products might make them more suitable for FI and increase satisfaction.
Introduction
Fecal incontinence (FI), or the involuntary leakage of stool, is prevalent in approximately 10% of community-living individuals.1 Community-living people with FI often wear an absorbent product, such as a pantiliner, pad, or brief to help protect against embarrassing visible soiling especially when going into public and to reduce related worry and anxiety.2 Bliss and colleagues3 reported that more community-living elderly women than men wore an absorbent pad or brief. Those with mild incontinence severity, especially men, may place a small gauze dressing between the buttocks to absorb leaked stool.4 Few absorbent products are specifically designed to absorb stool. Instead, most individuals must “make do” using products designed for urine or menstrual leakage.
Little is known about absorbent product use or preferences among person with FI. In a comprehensive review of studies and review articles about absorbent products, Fader and coworkers5 concluded that most studies comparing products in which FI was included tended to be older, and the products tested are no longer available, making comparisons with current studies impossible. They interviewed seventeen community-living individuals with FI about the acceptability of different designs of absorbent products available in the United Kingdom (UK), but were unable to be draw conclusions owing to the small sample size.5 To our knowledge, no other studies about this common and significant self-care practice for fecal incontinence have been published to date. Therefore, the purpose of this study was to describe the use and evaluation of disposable absorbent products by community-living people with fecal incontinence. The following research questions were investigated:
What is the prevalence of disposable absorbent product use by community-living people with fecal incontinence?
Which types of disposable absorbent products are most commonly used by community-living persons with FI? What are their patterns of wearing disposable absorbent products?
Are there differences in disposable absorbent product types used by men vs. women and younger vs. older people? Does the severity of FU or presence of urinary incontinence affect device choice?
How do community-living people with FI rate the features of disposable absorbent products they use? Are there differences in the evaluation of disposable absorbent products types based on sex, age, FI severity and presence of urinary incontinence?
How do individuals with FI feel about wearing a disposable absorbent product? What are reasons for not wearing a disposable absorbent product for fecal incontinence?
What recommendations for modifying disposable absorbent products do individuals with FI suggest?
Methods
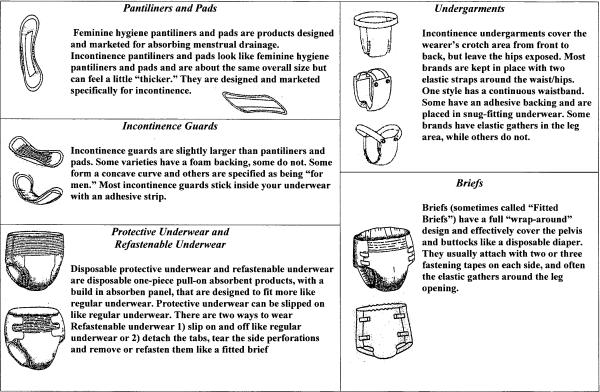
This study was nested in a clinical trial about the effect of three soluble dietary fibers of different fermentation levels and a placebo on FI. A survey was developed to examine use, patterns of wear, and evaluation of disposable absorbent product features by community-living individuals with FI. Absorbent products were defined as disposable. The survey consisted of 3 demographic questions, 4 questions about FI severity, 7 questions about use and patterns of wear of absorbent products, 10 questions about evaluation of absorbent product features of which 3 were open-ended questions, and 3 items queried feelings associated with wearing absorbent products. Generic diagram and word explanations of the various types of absorbent products referred to in the survey were shown to participants to facilitate a standard frame of reference (Figure 1). The features of absorbent products that were to be evaluated were developed from a review of the literature and consultation with colleagues who are expert in the field (personal communication Mandy Fader, 2004). The survey was completed at the start of the study before participants were provided with a disposable absorbent product to wear during the study. Data collectors explained the survey and its purpose, reviewed the explanations of absorbent products before the survey was administered, were available to answer any questions before, during and after the survey was completed, and reviewed the survey for completeness after its completion. Additional demographic and quality of life data were obtained from forms used in the parent study. Quality of Life was measured using the Fecal Incontinence Quality of Life (FIQL) tool, whose validity and reliability have been previously established.6
Figure 1.
Legend: Diagram and word descriptions of absorbent products referred to in the survey
Data Analysis
A score for usual FI severity was calculated based on responses to three survey items that queried the usual frequency, amount, and consistency of leaked feces. If participants marked more than one response to these questions, an average of their scores was computed. Preliminary analyses showed that tests of significance did not differ whether these average scores or scores rounded to the appropriate whole number were analyzed; therefore, in the final analyses, rounded values were used. A higher score indicated more severe FI. Analyses of the evaluation of the features of a type of absorbent product were limited to those who used the product.
Descriptive analyses were accomplished using means, standard deviations or medians and ranges for interval data; categorical data was summarized using frequencies. Associations between interval data were determined using a Pearson's correlation coefficient for data that were normally distributed and a Spearman's correlation if not. The linearity of any association was checked with scatterplots. Associations between categorical data were determined using a chi-square test of association or Fisher's exact test if cell sizes were sparse. Associations between interval and categorical data were accomplished using a t-test, if interval data was normally distributed, or a Mann-Whitney U test if not. The significance level were .05
Responses to the open-ended questions were analyzed using content analysis. As themes emerged from the review of responses to each question, they were coded, reviewed, and categorized based on the uniqueness and appropriateness to each group. Responses were reviewed for thematic subcategories. The subcategories were then reviewed in relation to the data until consensus among the investigators was reached. Frequencies and percentages of the themes and subthemes of responses were computed.
Results
Characteristics of Those Who Used and Did not Use Absorbent Products for FI
The 189 participants who completed the parent study completed the survey. Forty five percent of respondents (86/189) used absorbent products to manage FI. Table 1 compares the demographic characteristics of those who wore absorbent products for FI and those who did not. A significantly greater percentage of those who used absorbent product were elderly, female and unemployed. There were no significant differences between users and non-users in their other characteristics such as race, ethnicity, marital status, education, and annual income. Approximately two-thirds of users and non-users of absorbent products were married and about half had an annual income below $50,000. The majority of our sample was white, which is reflected similarly in the racial background of both user and non-user groups.
Table 1.
Demographic Characteristics of Those Who Wore Absorbent Products for FI and Those Who Did Not
| Percentage of Respondents (unless otherwise noted) | Users of Absorbent Products | Non-Users of Absorbent Products | P-value |
|---|---|---|---|
| Age (mean (sd)) years | 61 (13) | 55 (14) | .003 |
| Elderly (> 65 years) | 44 | 26 | .009 |
|
| |||
| Sex | |||
| Female | 88% | 67% | |
| Male | 12% | 33% | .001 |
|
| |||
| Race | .86 | ||
| White | 92.2 | 91.9 | |
| Black | 57.1 | 3.5 | |
| American Indian | 0 | 1.2 | |
| Asian | 1.0 | 1.2 | |
| More than 1 race | 2.9 | 2.3 | |
|
| |||
| Hispanic Ethnicity | 0 | 3 | .11 |
|
| |||
| Marital Status | |||
| Always single | 5.8 | 12.6 | |
| Married | 68.6 | 62.1 | |
| Partnered | 3.5 | 1.9 | |
| Divorced/Separated | 12.8 | 18.4 | |
| Widowed | 9.3 | 4.9 | .29 |
|
| |||
| Education | .34 | ||
| Some college or college degree | 85% | 89% | |
|
| |||
| Employed | 49 | 65 | .025 |
|
| |||
| Annual Income < $50,000 | 45 | 49 | .07 |
|
| |||
| Dual (urinary + fecal) incontinence | 43 | 30 | .07 |
|
| |||
| Fecal Incontinence Severity Score (median (range)) | 4.8 (1–27) | 3.0 (1–26.3) | .006 |
Participants who wore an absorbent product for FI had a higher FI severity score than those who did not wear products (Table 1). There was a weak but significant positive association between the usual severity of FI and use of an absorbent product (r =.20, p = .006). There was no significant difference in the presence of urinary incontinence along with FI between those who wore an absorbent product and those who did not. Dual incontinence occurred in less than half of the user and non-user group.
Description of FI Severity in Subgroups of Users of Absorbent Products
Table 2 shows the characteristics of FI severity in those who wore an absorbent product for FI. The characteristics are compared by the sex, gender, and type of incontinence of the product users. The findings first show the percentage of users for each FI severity characteristic. The median rating of the FI severity characteristics, which have an ordinal or hierarchical rating of worsening, were compared between the subgroups of product users. The median frequency of FI was significantly greater in older individuals who wore an absorptive product compared to younger ones. There was no significant difference in the median frequency, amount or consistency rating of FI between male and female product users or those users with dual incontinence versus FI only.
Table 2.
Characteristics of Fecal Incontinence in Absorbent Product Users by Sex, Age and Presence of Urinary Incontinence
| Percentage of Users (N = 86) | Males | Females | Younger | Older | FI+UI* | FI only |
|---|---|---|---|---|---|---|
| Usual frequency of FI | ||||||
| Less than once per day | 40 | 57 | 65 | 42 | 54 | 57 |
| Once per day | 20 | 16 | 15 | 28 | 22 | 12 |
| Once per day | 40 | 28 | 21 | 40 | 27 | 31 |
| Median frequency of FI (range) | 1 (1–3) | 2 (1–3) | 2 (1–3) | 2 (1–3)** | 1 (1–3) | 1 (1–3) |
|
| ||||||
| Usual amount of FI | ||||||
| Very small | 50 | 26 | 29 | 29 | 30 | 29 |
| Small | 40 | 53 | 50 | 53 | 51 | 51 |
| Moderate | 10 | 18 | 21 | 13 | 16 | 18 |
| Large | 0 | 3 | 0 | 5 | 3 | 2 |
| Very large | 0 | 0 | 0 | 0 | 0 | 0 |
| Median amount of FI (range) | 2 (1–4) | 1.5 (1–3) | 2 (1–4) | 1 (1–3) | 2 (1–4) | 2 (1–4) |
|
| ||||||
| Usual consistency of FI | ||||||
| Liquid | 10 | 20 | 21 | 16 | 13.5 | 19 |
| Loose and unformed | 80 | 62 | 63 | 69 | 68 | 64 |
| Soft but formed | 10 | 1 | 17 | 3 | 19 | 16 |
| Hard and formed | 0 | 0 | 0 | 0 | 0 | 1 |
| Median consistency of FI (range) | 2 (1–3) | 2 (1–4) | 2 (1–4) | 2 (1–3) | 2 (1–3) | 2 (1–4) |
FI = fecal incontinence, UI = urinary incontinence
Mann-Whitney U = 689.5, p =.03 for FI frequency between old vs. young users
Types and Patterns of Wear of Absorbent Products
The types and daily number of absorbent products used by community-living individuals with FI are presented in Table 3. Pantiliners were worn by the most users, and disposable briefs and underwear were worn by the fewest. Feminine hygiene pads and pantiliners were worn by a greater percentage of absorbent product users than incontinence pads and pantiliners. About half (49%) of users responded that they always used the same brand of absorbent product. Seven percent reported placing toilet tissue in between their buttocks rather than use an absorbent product. Additional products listed included a cotton ball, small gauze, cosmetic pad or paper towel.
Table 3.
Type and Daily Number of Absorbent Products Used by Community-Living Individuals with Fecal Incontinence
| Type of Absorbent Product | Number of Users* | % Users Who Wore <1 Product per Day | % Users Who Wore 1–3 Products per Day | % Users Who Wore > 3 Products per Day |
|---|---|---|---|---|
| Feminine hygiene pantiliner | 48 | 25 | 67 | 6 |
| Feminine hygiene pad | 33 | 49 | 49 | |
| Incontinence pad | 17 | 47 | 53 | 0 |
| Incontinence pantiliner | 15 | 40 | 27 | 13 |
| Fitted briefs | 6 | 33 | 50 | 0 |
| Incontinence guard | 4 | 75 | 25 | 0 |
| Protective underwear | 4 | 25 | 75 | 0 |
| Refastenable underwear | 3 | 67 | 33 | 0 |
| Undergarments | 8 | 13 | 50 | 0 |
| Other | 10 |
Some respondents used more than one type of absorbent product
The majority of users of pads, briefs or protective underwear used 1 to 3 products per day (Table 3). Only respondents who wore pantiliners reported using more than three per day. Forty-nine percent of those who used an absorbent product indicated they wore one all of the time, 54% wore a device when going out into public, 29% wore one while at home, and 20% wroe a product while they slept.
Types and Pattern of Product Use
The use of only one type of absorbent product, a feminine hygiene pad, was significantly associated with age. More than twice the percentage of younger users wore a feminine hygiene pad when compared to older users (52% vs 21%, p=.004). There was no difference according to age in the number of products used or when a product was worn.
There were few differences between men and women in the types and pattern of absorbent products used. More women than men wore an incontinence pantiliner (61% vs 20%, p = .02). Only three respondents wore refastenable underwear (n = 3), men were more likely than women to choose this device (2 vs 1, p = .035). No men reported wearing an incontinence guard. A greater percentage of women than men wore an absorbent product when out in public (59%, vs. 20%, p = .04) or at home (33% vs. 0%, p = .03). No men reported wearing a product while at home. Men and women did not significantly differ in the number of absorbent products used daily.
Seventy three percent of respondents with dual incontinence used the same type of product to absorb both stool and urine. The percentage of individuals with dual incontinence who wore an incontinence pad was three times greater then those with FI only incontinence only (32% vs 10%, p = .01). However, fewer users with dual incontinence wore a feminine hygiene pantiliner as compared to with FI only (41% vs 67%, p = 0.17). There was no difference in the number of products worn daily or when a product was worn based on presence of urinary incontinence.
Device Use and FI Severity
We analyzed the association between the type and daily number of absorbent products used for managing incontinence and the FI severity score. Higher FI severity scores were inversely related to use of a fitted absorbent brief (r = −.83, p = .042). Among respondents who used feminine hygiene pantiliners (r =.30, p = .04) and pads (.38, p =.03) higher severity scores were correlated with a higher number of pantiliners or pads used on a daily basis.
The type and frequency of absorbent product used for managing FI was compared to the individual components (frequency, amount, and consistency) of FI severity. The number of pantiliners worn daily differed according to the frequency of FI. Nearly half (48%) of pantiliner users who leaked feces less than once per day used fewer than 1 pantiliner per day, and those who leaked more than once per day used 1 to 3 pantiliners per day (p = .001). A greater percentage of those who leaked liquid feces wore an absorbent product in public (76%) and while sleeping (75%) when compared to those who leaked non-liquid feces (40% p = .006 in public and 8%, p = .001 while sleeping).
In the parent study, subjects were asked to wear an incontinence product daily during the first and last 14 days of the study. They were given a choice in selecting an incontinence pantiliner, incontinence pad, or fitted brief. Of the 189 subjects, 92% selected an incontinence pantiliner. There were differences in selection based on sex, gender and whether they had dual incontinence. A greater percentage of older than younger individuals selected an incontinence pad (11% vs. 4%) or brief (5% vs. 0%, p = .009). Only women selected an incontinence pad (9% vs 0%, p = .019). A greater percentage of those who leaked urine selected an incontinence pad (11% vs. 4%) or fitted brief (5% vs. 0%, p = .014) compared to those who leaked feces only.
Evaluation of Absorbent Product Features
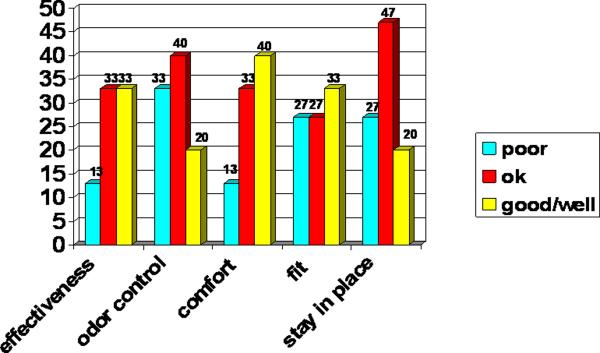
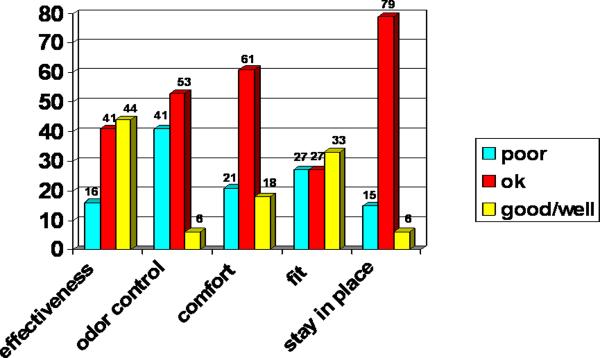
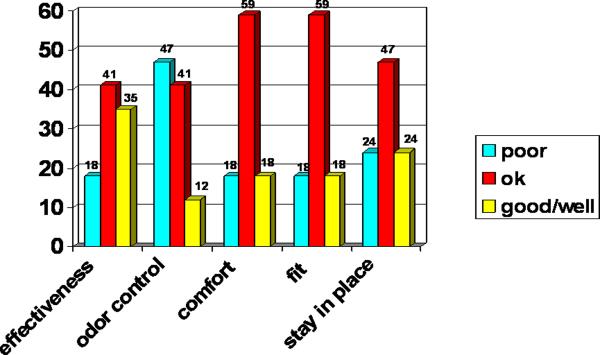
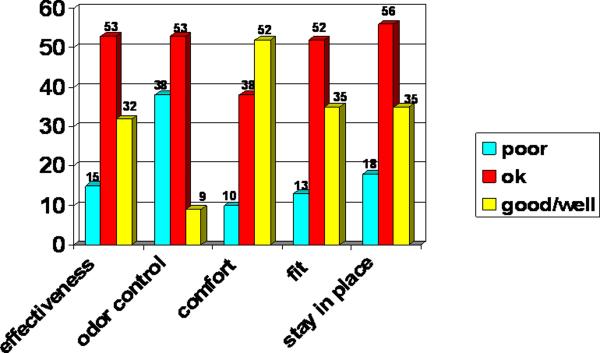
The evaluation of the features of the four most commonly worn absorbent products by those with fecal incontinence is presented in Figures 2 to 5. The product features receiving a “good” rating by most users varied. Most pantiliner users rated comfort and fit as “good” (Figure 2). None of the features of an incontinence pad were rated as “good” by a majority of users (Figure 4). Odor control had the lowest percentages of “good” ratings across all products.
Figure 2.
Legend: Evaluation of Features of Incontinence Pantiliners by Community-Living Users with Fecal Incontinence
Figure 5.
Legend: Evaluation of Features of a Feminine Hygiene Pads by Community-Living Users with Fecal Incontinence
Figure 4.
legend: Evaluation of Features of Incontinence Pads by Community-Living Users with Fecal Incontinence
Absorbent products were also ranked based on the perceived ability to conceal the device under clothing. Using a 4-point scale varying from “not at all noticeable,” to “very noticeable,” all products except protective underwear were considered “not at all noticeable” by at least 60% of users. Half of respondents who used protective underwear rated them as “a little noticeable,” and 25% rated them as somewhat or very noticeable. Feminine hygiene pantiliners or incontinence pantiliners were rated as easy to carry (81% and 60% respectively). Approximately half of the users of feminine hygiene pads or incontinence pads ranked them as easy to carry.
Satisfaction concerning various absorbent products' ability to contain or absorb stool was evaluated on a 5-point scale from “very dissatisfied” to “very satisfied.” At least half of users were satisfied or very satisfied with the product they used (Table 4). Of the four most commonly used products, the incontinence pad had the highest percent of dissatisfied users (31.5%). FI severity score was moderately and negatively correlated with satisfaction with a feminine hygiene pad (i.e. satisfaction was lower when FI severity was greater) (r = −.40, p = .02).
Table 4.
Satisfaction of Community-Living Individuals with Fecal Incontinence with Ability of Absorbent Products to Contain or Absorb Leaked Stool
| Type of Product (Number of Users) | Satisfied or Very Satisfied % of Users | Very Dissatisfied or Dissatisfied % of Users |
|---|---|---|
| Feminine hygiene pantiliner (47) | 55 | 11 |
| Feminine hygiene pad (32) | 50 | 19 |
| Incontinence pantiliner (15) | 53 | 27 |
| Incontinence pad (17) | 47 | 29 |
| Incontinence guard (4) | 50 | 0 |
| Protective underwear (4) | 75 | 0 |
| Refastenable underwear (4) | 75 | 0 |
| Fitted briefs (6) | 75 | 0 |
| Undergarments (7) | 29 | 0 |
We included an open-ended item to evaluate confidence in the absorbent product. Twelve percent responded they always had confidence, 45% responded they usually had confidence, 26% responded they were sometimes confident, 12% responded “not really,” and 4% responded they never had confidence. There was no difference in satisfaction or confidence based on age, sex, or presence of urinary incontinence.
Age, Sex, FI Severity and Product Evaluation Ratings
Ratings of product effectiveness, comfort, and fit did not significantly differ when analyzed based on sex or age. Women who wore an incontinence pantiliner rated its ability to stay in place lower than did the few men who used this product (p = .03). A greater percentage of younger users rated odor control of a feminine hygiene pad as poor compared to older users (52% vs 17%, p = .02).
Evaluations of some products differed according to FI severity. For example, the ability of a feminine hygiene pad to stay in place was rated “poor” by those who leaked feces once a day or more as compared to those who leaked once daily (26% vs 0%, p = .048). Further, its ability to control odor was rated “well” by those who leaked very small amounts of stool but not by those who leaked larger volumes compared to none of those who leaked more (25% vs 0%, p = .009). The effectiveness of a feminine hygiene pad was rated “poor” by a greater percentage of those leaked loose and unformed feces as compared to those who leaked liquid or soft but formed feces (p = .014). Several features of a feminine hygiene pantiliner were rated more highly by those who leaked a very small amount of feces compared to those who leaked a greater amount including ability stay in place (p = .04) and to control odor (p = .023).
Other Features Liked and Disliked
Individuals with FI described a variety of absorbent product features that they liked and disliked in their responses to open-ended questions (Table 5). Respondents provided recommendations about ways to improve the products. The majority of suggestions related to modifying the design of the product including its size and shape (e.g., widen, lengthen, curve rear), material (e.g., soften), and odor control ability; suggestions appeared aimed at making the product more suitable for absorbing leakage of feces.
Table 5.
Opinions about Features of Absorbent Products by Community-Living People with Fecal Incontinence
| Features Liked Most* | Features Disliked Most* | Recommended Improvements* |
|---|---|---|
|
| ||
| Product Design 18% (lightweight, not noticeable, thinness, wings) | Product Design 15% (not wide enough, does not cover area where stool is leaked, front vs. back is unclear | Better Design 27% Wider Longer More absorbent Size (cover larger area, larger in back, curve up) Better odor control Different material (soften, make sweat-proof or spongy, use cotton lining or better material) |
| Effectiveness 11% | Ineffectiveness 11% (not absorbent enough, does not control odor) | More effective 6% |
| Convenience 10% (easy to carry, dual purpose for fecal and urinary incontinence) | Discomfort 10% (slides, does not stay put, does not fit) | More comfortable 2% (better fit, stay in place) |
| Comfort 3% | Inconvenience 3% (not flushable, need to change too often) | More convenient 2% (make easier to use or dispose of, package with wipes) |
| Confidence 3% | ||
| Inexpensive Price 3% | ||
percentage of survey respondents
Feelings about Wearing an Absorbent Product
When asked an open-ended question about their feelings regarding wearing an absorbent product, 22% responded they did not mind wearing one, 6% said they would prefer not to wear one, 6% responded that they felt they had no choice but to wear one, 5% said wearing a product made them feel more secure or confident, 3% said the products were uncomfortable, and 3% said wearing a product was embarrassing. When participants were asked a direct question about whether they minded wearing an absorbent product daily, a higher percentage (46%) responded that they did not mind, 8% responded that they would prefer not to wear one, and 3% explained that they would not mind if some features were improved. Approximately one-third of respondents (39%) stated they would avoid some activities if they did not wear an absorbent product and a similar percentage (34%) stated they would not avoid anything. Exercise or physical activity was the activity that most respondents (16%) would avoid. Eleven percent stated they would go out into public less, 4% would not travel or take a vacation, and 2% said they would “dress up” less.
Reasons for Not Wearing an Absorbent Product
Several reasons were reported for not wearing an absorbent product for managing FI. They included the perception that FI is “not that bad” (39%, personal preference (13%), discomfort (10%), embarrassment (7%), being unaware of products (6%), poor fit (5%), cost (4%, and lack of effectiveness (2%). A greater percentage of men reported that unawareness (24% vs. 6%, p = .011) and embarrassment (24% vs. 8%, p = .025) about absorbent products were reasons they did not wear one. More younger than older people reported not wearing a product because they thought the severity of their fecal incontinence was “not that bad” (81% vs 54%, p =.006). Cost was a greater concern of respondents with dual incontinence as compared to FI alone (20% vs 3%, p = .004)
Discussion
To our knowledge, this is the first study reporting patterns of wear and evaluation of absorbent products by community dwelling persons with FI. The findings reported here are consistent with our earlier study of community-dwelling elderly person with FI, which found that use of an absorbent product was a common self-care practice, especially among women.2, 3 In addition, our findings show that younger individuals with FI are less likely to wear an absorbent product and when they did wear one, it tended to be a feminine hygiene pantiliner.
Others have reported the use and effectiveness of absorbent products for managing urinary incontinence and dual incontinence in other settings such as the hospital and nursing home.5, 7, 8 Fader and coworkers5 reported the acceptability of five different types of absorbent products (insert, diaper, pull-up, T-shaped diaper and washable diaper) available in the UK in 16–17 community-living individuals with dual incontinence. For daytime wear an insert that appeared similar to an incontinence pad was deemed acceptable by about a third of respondents, followed by a T-shaped and washable diaper ranked as acceptable in about one-fourth. Pull-up pants were accepted by the lowest proportion (12.5%). For nighttime wear a quarter of respondents reported that an insert, T-shaped diaper, and pull-up were equally acceptable. Wearing a feminine hygiene pad or pantiliner was the most common absorbent product used by our subjects and more common than an incontinence pantiliner. The findings of this study support the preliminary observations of Fader's group5 regarding acceptability of an insert (pad) over a incontinence brief for daytime wear.
Although there was no significant difference in use of an absorbent product or the type of product worn based on usual FI severity, a greater percentage of subjects without urinary incontinence wore a feminine hygiene pantiliner. Findings suggest that leaking urine as well as feces requires a product with greater absorbance capacity. There was a perceived need for additional protection when stool was liquid as the daily number of pantiliners used was increased and a product was worn when going out into public and during sleep.
Users of absorbent products were nearly evenly divided when rating product comfort and concealment. Only 12% reported they always had confidence in the product that they used. Respondents made numerous suggestions for modifying the design of the products. The suggested modifications of making a product that is longer, wider in the back, and distinguishable between the back and front reflect the need to better accommodate the location of fecal leakage in the design of products. Providing an absorbent product that is useful for dual incontinence was perceived as a need as because one-third of those in this study experience both fecal and urinary incontinence.
None of the absorbent product users identified cost as a negative (disliked) feature, and 3% identified inexpensive cost as a positive feature. A sample with a lower income level and employment level might have had a different response. Cost was a reason that some individuals with dual incontinence did not wear an absorbent product for FI; this response may reflect the high use of the same product for dual incontinence. The feature of an absorbent product that appears to need the most improvement is odor control. Younger persons with FI seemed especially concerned about poor odor control. Being lightweight and thin were features favored by most.
Qualitative studies of women with FI revealed that some consider wearing an absorbent product as essential, enabling them to engage in work and other activities of public life.2 Similarly, respondents in this study stated they would restrict going into public if they did not wear an absorbent product. When asked directly, half of the respondents said they did not mind wearing an absorbent product daily.
The perception that FI was not very severe was the most common reason why an absorbent product was not worn, especially among younger people with FI. Educating males about the types of absorbent products available might increase their use; this represents a teaching opportunity for the WOC nurse. Because women may be more accustomed to wearing a feminine hygiene product due to menstruation, they may feel less embarrassed when wearing a product for FI. The WOC nurse specialist needs to support men in their choice of wearing an absorptive product. Bliss and colleagues4 previously reported that a surgical gauze dressing was used by individuals with mild fecal incontinence. A few respondents in this study reported placing toilet tissue or gauze between their buttocks instead of wearing a pantiliner or pad; they tended to report leaking a small amount of loose or liquid stool.
Limitations
There are limitations to this study. Responses to survey questions reflect recall rather than daily report. In a previous study, we reported that FI severity by recall differed from that determined by a daily diary9 and tended to be underestimated. It was our assumption that perception of FI severity by recall influences selection and purchase of an incontinence product since few individuals keep a daily diary. It is also possible that subjects may have misunderstood some of the types of absorbents products referred to in the survey when they were responding to the survey. Providing subjects with diagram and word descriptions of the types of absorbent products referred to in the survey and explanations, review, and answering any questions of subjects by our data collectors were control measures instituted to minimize misunderstanding. Small sub-group sizes of absorbent product users may reduce generalizability of their results.
Clinical Implications
Our findings support the need for WOC nurse's to inquire about absorbent device use since nearly half of the community-living individuals with FI regularly use these products. Findings also reveal that individual preference, severity of FI and presence urinary incontinence influence selection and use of an absorbent product. For example, patients with dual incontinence tend to prefer a more absorbent product. These results support the importance of the guidance provided by WOC nurses to patients about product selection. Feminine hygiene products were worn by a majority of users, but only half of users were satisfied with this product, and fewer had confidence in them. Counseling about products specifically designed for incontinence containment may be useful for these patients. In addition, the WOC nurse should provide more detailed counseling about the types and features of absorbent products for men with FI, as well as emotional support to lower embarrassment as he deliberates choosing to wear one.
Out findings demonstrate that there is a paucity of absorbent products specifically designed for persons with FI. Therefore, we recommend that manufacturers design new or modify existing absorbent products in order to render them more suitable for FI or dual incontinence.
Conclusions
Despite a paucity of specifically designed absorbent products, they are commonly used by community-dwelling persons with FI. Women and older people were most likely to use an absorbent product than were men and younger patients. Educating males about the types of absorbent products available and trying to lessen their embarrassment may increase their usage. Smaller pantiliner type products that can be frequently changed were preferred by many respondents. However, participants with dual incontinence were more likely to use a more absorbent product. Product features rated as “good” varied by product type; but odor control had a low rating across all product types. Approximately half of product users were satisfied or very satisfied with the product they used. Nevertheless, they identified numerous features of absorbent products that could be modified to improve their suitability and effectiveness for FI.
Figure 3.
Legend: Evaluation of Features of Feminine Hygiene Pantiliners by Community-Living Users with Fecal Incontinence
Acknowledgments
This study was funded by grants from Kimberly Clark and the National Institute of Nursing Research, NIH, R01-NR07756. The investigators appreciate the contribution of absorbent products from Kimberly Clark for use during the study, which were provided after the survey was completed.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ. Prevention of urinary and fecal incontinence in adults. Evidence Report/Technology Assessment. 2007:1–379. [PMC free article] [PubMed] [Google Scholar]
- 2.Peden-McAlpine C, Bliss DZ, Hill J. The experience of community-living women managing fecal incontinence. West J Nurs Res. 2008;30:817–835. doi: 10.1177/0193945907312974. [DOI] [PubMed] [Google Scholar]
- 3.Bliss DZ, Fischer LR, Savik K. Managing fecal incontinence: Self-care practices of older adults. J Gerontol Nurs. 2005;31:35–44. doi: 10.3928/0098-9134-20050701-08. [DOI] [PubMed] [Google Scholar]
- 4.Bliss DZ, Savik K. Use of an absorbent dressing specifically for fecal incontinence. J Wound, Ostomy, Continence Nurs. 2008;35:221–228. doi: 10.1097/01.WON.0000313647.44870.9a. [DOI] [PubMed] [Google Scholar]
- 5.Fader M, Cottenden A, Getliffe K, et al. Absorbent products for urinary/faecal incontinence: A comparative evaluation of key product designs. Health Technol Assess. 2008;12:iii. doi: 10.3310/hta12290. [DOI] [PubMed] [Google Scholar]
- 6.Rockwood TH, Church JM, Fleshman JW, et al. Fecal incontinence quality of life scale: Quality of life instrument for patients with fecal incontinence. Dis Colon Rectum. 2000;43:9–17. doi: 10.1007/BF02237236. [DOI] [PubMed] [Google Scholar]
- 7.Brazzelli M, Shirran E, Vale L. Absorbent products for containing urinary and/or fecal incontinence in adults. J Wound Ostomy Continence Nurs. 2002;29:45–54. doi: 10.1067/mjw.2002.120870. [DOI] [PubMed] [Google Scholar]
- 8.Fader M, Cottenden AM, Getliffe K. Absorbent products for light urinary incontinence in women. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD001406.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher K, Bliss DZ, Savik K. Comparison of recall and daily self-report of fecal incontinence severity. J Wound Ostomy Continence Nurs JWOCN. 2008;35:515–520. doi: 10.1097/01.WON.0000335964.13855.8d. [DOI] [PMC free article] [PubMed] [Google Scholar]