Abstract
Background
In addition to possibly prolonged suffering and anxiety, extended waits for children’s surgery beyond critical developmental periods has potential for lifelong impact. The goal of this study was to determine the duration of waits for surgery for children and youth at Canadian paediatric academic health sciences centres using clinically-derived access targets (i.e., the maximum acceptable waiting periods for completion of specific types of surgery) as used in this Canadian Paediatric Surgical Wait Times project.
Methods
We prospectively applied standardized wait-time targets for surgery, created by nominal-group consensus expert panels, to pediatric patients at children’s health sciences centres across Canada with decision-to-treat dates of Sept. 1, 2007 or later. From Jan. 1 to Dec. 30, 2009, patients’ actual wait times were compared with their target wait times to determine the percentage of patients receiving surgery after the target waiting period.
Results
Overall, 27% of pediatric patients from across Canada (17411 of 64012) received their surgery after their standardized target waiting period. Dentistry, ophthalmology, plastic surgery and cancer surgery showed the highest percentages of surgeries completed past target.
Interpretation
Many children wait too long for surgery in Canada. Specific attention is required, in particular, in dentistry, ophthalmology, plastic surgery and cancer care, to address children’s wait times for surgery. Improved access may be realized with use of national wait-time targets.
Prolonged wait times for care are often a concern in publicly funded health care systems.1 Canadian governments have made the reduction of wait times a priority.2,3 A Canadian federal–provincial accord, called the 2004 10-Year Plan to Strengthen Health Care, included a $5.5 billion wait-times reduction fund to help provincial and territorial governments reduce wait times in the five priority areas, which are cancer care, cardiac care, diagnostic imaging, joint replacement and sight restoration.3
The focus of the fund, however, was almost exclusively relevant to adults, omitting Canada’s children and youth, who represent more than one-quarter of the Canadian population4 from the wait-time reduction priorities. To address wait times, governments in Canada have established central targets, such as the recommendation that surgery should be performed within six months of the decision to treat.2 Although this approach is uniform and explicit, urgent surgery often requires a shorter time frame. An alternative approach to central targets is to have clinicians develop clinically derived access targets (i.e., maximum acceptable waiting periods for the completion of specific types of surgery).
People are often surprised to learn that children wait for surgery just like adults.5 In addition to the possibility of prolonged suffering and anxiety that is typical of extended waits, surgery in children must sometimes be performed at critical developmental periods.6 Furthermore, adverse effects of extended waits may have lifelong impact, which magnifies the importance of measuring and addressing wait times in this vulnerable population. In 2006, the Pediatric Surgical Chiefs of Canada agreed to adopt standardized pediatric surgical wait-time access targets and resolved to measure the wait times for children’s surgeries. Thus, the Canadian Paediatric Surgical Wait Times project was founded as an unprecedented national collaborative effort. The goal of the project was to determine the duration of waits for surgery for children and youth at Canadian children’s centres in all surgical subspecialties, using clinically derived access targets.
Methods
Hospitals
We collected data from 15 Canadian pediatric academic health sciences centres. In Canada, there are 16 pediatric academic health sciences centres associated with the country’s 16 university medical schools, and the vast majority of pediatric surgical subspecialists are associated with one of these children’s centres. Although the percentage of children’s surgery performed at the children’s centres varies by region, all complex pediatric surgical procedures in Canada are performed in one of these centres.
The pediatric surgeon-in-chief and a site lead in each centre ensured that the requisite data were collected and transmitted to the project national office for collation and analysis. A site coordinator was responsible for ensuring the data were accurate, and complete data logs were maintained at each site to track and resolve potential data inaccuracies. Sites reviewed data on a monthly basis with the national office. In addition, the national office ran routine monthly analyses to examine trends and check for out-of-range values.
Wait-time targets for access to surgery
The impetus for developing clinically derived target periods for access to surgery is that information on how long a patient waits for surgery is difficult to interpret without considering the patient’s clinical context. For example, a wait of six months would have no adverse effects for a stable, non–life-threatening condition such as skin tags, whereas a wait of similar duration for pediatric strabismus (wandering eye) at critical junctures could influence brain development. Two wait-time intervals were defined. Wait 1 is the time from the date of referral to a specialist to the date of the initial specialist consultation. Wait 2 was defined as the time from the date on which a decision is made to proceed with surgery to the date of surgery. In this study, we focused on Wait 2.
The Paediatric Canadian Access Targets for Surgery (also known as P-CATS) were developed in 2005 and revised in 2008. Initially, the targets were developed by surgeons from Ontario at in-person meetings. A nominal-group technique was used to build consensus among discipline-specific expert panels that consisted of surgeons from 11 surgical subspecialties.7 Clinicians were instructed to consider all of the diagnoses among patients who presented to their specialty for consultation and surgery, and to determine, to the best of their knowledge and according to available evidence, the maximum period that the patients could wait for surgery. The wait time was defined as the period from the date on which a decision was made to proceed with surgery to the date of surgery, without reasonably expected adverse events.7 In 2008, the resulting wait-time targets received relatively minor revisions that mainly involved the expansion of missing codes using teleconferences involving surgeons from across Canada.8
Based on 867 identified diagnoses, access targets were assigned a priority classification level that was consistent across all subspecialties, with an associated target wait time for surgery (Appendix 1, available at www.cmaj.ca/cgi/content/full/cmaj.101530/DC1). Priority I refers to surgery that needs to be performed within 24 hours, Priority IIa within 1 week, Priority IIb within 3 weeks, Priority III within 6 weeks, Priority IV within 3 months, Priority V within 6 months and Priority VI within 12 months. Automatically linking the diagnoses to a priority score and associated target time provides a uniform and standardized approach to determining the appropriateness of the duration of the wait for surgery. It also reduces the potential for “gaming” (i.e., taking advantage of the system) by using subjective priorities assigned by clinicians.
Patients’ actual wait times were compared with their target wait times to determine the percentage of patients receiving surgery past target (i.e., after the target waiting period). The date of the decision to proceed with surgery in 11 of the centres was defined as the date when patients were ready and all necessary diagnostic procedures were complete. In the other four centres, it was defined as when patients were ready but not all diagnostic tests had been completed. Data collection began on Sept. 1, 2007. The data contained in this report are from the period of Jan. 1 to Dec. 31, 2009. We collected data on all surgeries completed on or after Jan. 1, 2009. All patients who had been placed on waiting lists from September 2007 onward (and who were still waiting as of Jan. 1, 2009) were included. Emergent surgeries (i.e., those needing to be performed within 24 hours) were excluded. We did not collect data on adverse events.
Statistical analysis
T-tests were performed on the slope of the trend from Jan. 1 to Dec. 31, 2009, for the percentage of surgeries completed past target. Significance was assessed at the α = 0.05 level.
A Pearson correlation test was used to identify relations between hospital size and percentage of surgeries completed past target for various surgical subspecialties. Significance was assessed at the α = 0.05 level.
Results
Data on more than 84 922 awaited and completed surgeries were collected from January to December 2009. The percentages of surgeries completed past target for all surgical subspecialties are shown in Table 1, in descending order from the highest to the lowest. Overall, 27% of pediatric patients (representing 17 411 of 64 012 completed surgeries and ranging from 15%–45% by surgical subspecialty) received their surgeries past target. During this same period, more than 90% of patients received their surgery within six months of the decision to treat.
Table 1:
Numbers of surgeries not completed as of December 2009 and surgeries completed past the target period in all surgical areas from January to December 2009
| Area | Current waiting | Total completed | No. (%) completed past target |
|---|---|---|---|
| Dentistry | 4 672 | 9 784 | 4 409 (45) |
| Ophthalmology | 1 818 | 5 172 | 2 227 (43) |
| Plastic surgery | 1 725 | 4 833 | 1 684 (35) |
| Cancer surgery | 83 | 1 075 | 304 (28) |
| Neurosurgery | 121 | 989 | 232 (23) |
| Cardiac surgery | 297 | 1 572 | 365 (23) |
| Otolaryngology | 5 809 | 17 567 | 3 793 (22) |
| General surgery | 1 892 | 10 368 | 1 998 (19) |
| Urology | 2 302 | 6 055 | 1 162 (19) |
| Orthopedic surgery | 2 150 | 6 317 | 1 196 (19) |
| Gynecology | 41 | 280 | 41 (15) |
| Total | 20 910 | 64 012 | 17 411 (27) |
The percentage of surgeries completed past target ranged from 24%–30% from January to December 2009. Although there was fluctuation, a significant change did not occur over the study period. The highest percentages of surgeries completed past target were in the subspecialties of dentistry (45%), ophthalmology (43%) and plastic surgery (35%). The next three highest were in the subspecialties of cancer, neurosurgery and cardiac surgery (Table 1).
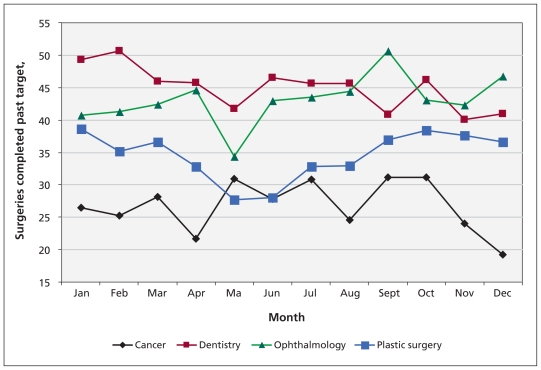
Whereas no significant changes were observed in ophthalmology, plastic surgery or any other surgical subspecialty studied, a significant decline in the percentage of surgeries completed past target was observed in dentistry (p = .007) (Figure 1).
Figure 1:
Percentage of surgeries completed after the target waiting period in dentistry, ophthalmology and plastic surgery from January to December 2009.
When results were stratified by diagnoses, dentistry patients with moderate to severe dental decay and dental pain, ophthalmology diagnoses related to patients with strabismus and plastic surgery patients who had cleft lip and palate or cleft palate were all identified as contributing most to the high percentage of surgeries completed past target in their respective areas (data not shown). A significant correlation was not observed between size of hospital and percentage of surgeries completed past target in these areas (r = −0.19; p = 0.51).
Interpretation
Waiting for care continues to be a substantial issue in Canada for health care systems, providers and patients. Despite all of the attention on wait times, a report from the Canadian Institute for Health Information stated that “variations in measures across provinces means the reported wait times are not yet comparable from one jurisdiction to the next,”9 underscoring the need for “national indicators to ensure accountability,”10 as described in a CMAJ editorial. The Canadian Paediatric Surgical Wait Times project developed a pan-Canadian standardized approach to evaluating pediatric surgical wait times within all pediatric surgical subspecialties. The pediatric access targets have now been adopted as a provincial standard by British Columbia and Alberta, which means that two provinces now use a uniform and standard approach to measuring wait times for surgery based on clinical need.
Although the percentage of surgeries completed past target varied by surgical subspecialty and hospital, all hospitals, irrespective of site and subspecialty, had patients whose surgeries were completed past their access targets. Despite receipt of surgery within six months of the decision to treat for 90% of patients, clinically derived targets found that 27% of children waited too long for their specific condition.
Information derived from the application of these access targets could be used in multiple ways. First, surgeons, as individuals or as a group, can manage and triage patients on their surgical wait-lists based on clinical acuity. Second, surgeons and institutions can share best practices to improve wait-list management. Third, institutions can make decisions about shifting or investing resources to address the needs of patients. For example, one participating hospital has begun to use the data to redistribute operating room resources to areas with the highest percentages of surgeries completed past target. The result has been a substantial reduction in overall out-of-window rates (i.e., rates of surgeries not completed within target waiting periods). Fourth, regions can better understand interinstitutional demand and possibly manage referrals to better match capacity.
Finally, funders like the provincial ministries of health in Canada can identify areas where resources can be used more efficiently or areas where need is determined to exceed capacity, and provide targeted funding to reduce wait times on a regional, provincial or national basis.11 For example, at SickKids at the beginning of this project, the wait list for children needing dental treatment exceeded 600 patients. Application of the access targets to this list showed that more than 70% of children had exceeded their access targets. This information was influential in convincing the Ministry of Health and Long-Term Care in Ontario to provide volume-based funding for additional procedures. Access targets were also used at SickKids to triage and prioritize patients. With those two initiatives, the wait list has now dropped to about 200 patients, and the out-of-window rate has dropped to zero. The out-of-window rate has allowed us to determine the maximum acceptable size of the wait-list for children requiring dental treatment.
There are several potential barriers to the implementation of access targets. First, to expand targets beyond children’s surgery would require some financial investment and the cooperation of professional societies to perform the consensus activity using a method similar to that used to develop the pediatric targets. British Columbia has recently implemented diagnosis-based target periods for access to surgery by adults. These targets were derived using a similar consensus-based approach to ours that is intended for use in that province for all patients 17 years of age and older. Alberta is exploring a similar process for their adult patients. If these ventures are successful in those two provinces, then nationwide Canadian access targets for surgery for both children and adults could become a reality.
Second, hospitals need to develop processes for capturing decision-to-treat dates and surgical dates. Although this data collection can be performed manually, ideally it would be performed in conjunction with surgical information systems used in virtually all operating rooms. Third, the provinces of Canada would have to cooperate and adopt uniform reporting systems. Fourth, the information would ideally be collected centrally. For example, the Canadian Institute for Health Information, with its national mandate, would be the ideal organization to both collect data and ensure quality control.
Dental treatment requiring anesthesia, ophthalmology and plastic surgery were identified as the three areas with the highest percentage of surgeries completed past target. Dental treatment requiring anesthesia uses the most operating room hours at the majority of pediatric hospitals in Canada.12 Our results identify dentistry as a high-priority area to address and underscore the importance of reducing the prevalence of dental decay.13 The area of surgical ophthalmology is primarily driven by patients with strabismus. Delay in correcting strabismus in children jeopardizes their chances of retrieving normal vision and the associated benefits in quality of life.14 The area of plastic surgery is driven primarily by patients requiring cleft lip and palate surgery. To ensure a child’s optimal speech, cleft lip and palate surgery must be performed at specific times.15 Surgery for cleft lip or cleft lip and palate illustrates the complexity of children’s surgical care, because the coordination of cleft repair requires collaboration with multiple services. Therefore, simply increasing operating room resources may not reduce the time patients wait unless care can be coordinated.
Finally, the next three areas with high rates were cancer surgery, neurosurgery and cardiac surgery. In addition to all of the issues highlighted above, these out-of-window rates are particularly concerning because many of the diagnoses in these three clinical areas are potentially life-threatening. This concern underscores the need for a comprehensive approach to evaluating surgical wait times and the specific need to address surgical wait times for children.
Limitations
Our study has several potential limitations. First, data collection occurred only at pediatric academic health sciences centres and did not include Canadian community hospitals. Expansion of the study to include more hospitals that perform children’s surgeries might have shown a lower percentage of surgeries completed past target. However, children’s centres perform a large percentage of children’s surgery in Canada, and all complex surgery, such as cancer, neurosurgery and scoliosis, is performed at these centres.
Second, the targets used in this study were based on expert consensus panels, and we neither recorded nor analyzed adverse events or outcomes that may have occurred and been related to prolonged waiting periods. However, because there is little or no benefit to prolonged waits, empirically based access targets may be even shorter than those determined by expert consensus. Although little or no data are available, in instances of inguinal hernia, for example, the consensus target waiting period of three weeks is probably too long. A study published shortly after the consensus targets had been established reported that many children waiting for hernia surgery longer than two weeks often required urgent surgery due to incarceration.16 Further research is needed to determine empirically based targets for all conditions needing surgery.
Third, although this project used a standardized definition for the decision-to-treat date, four sites collected data according to provincially mandated definitions that placed patients on waiting lists before all diagnostic procedures were performed or before patients were developmentally ready for surgery. However, high out-of-window rates for surgery were found at all hospitals irrespective of discrepancies in definitions. Furthermore, in a comparison between the data from the 11 centres that used the standardized definition of the decision-to-treat date and the data from the four sites that used provincial definitions, we found only small differences in the percentage of surgeries performed beyond target (26.9% for the 11 centres using the standard definition compared with 27.7% for the other four).
Fourth, this research considers only the interval between the date of decision between the family and the surgeon to proceed with surgery and the date of receipt of that surgery. A full consideration of wait time would need to take into account other waiting periods, such as that to see the specialist or to receive essential investigations.
Conclusion
We implemented a standardized, Canada-wide approach, developed by clinicians and based on clinical need, to the evaluation of pediatric surgical wait times in all surgical subspecialties. Overall, 27% of pediatric patients from across Canada received surgery beyond their standardized target period for access to surgery. We believe this national collaborative project shows the feasibility and potential benefits of setting national standards for surgical wait times. Such accountability can result in measurably improved access in the delivery of national publicly funded health care.
Supplementary Material
See related research by Ahn and colleagues at www.cmaj.ca/cgi/doi/10.1503/cmaj.101511.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
The Canadian Paediatric Surgical Wait Times Study Group: Dr. Anne-Marie Houle, Dr. Susanne Leclerc, Dr. Sandeep Kumar Mayer, Dr. Baxter Willis, Dr. Gerard Corsten, Dr. Geoffrey K. Blair, Dr. Sarah Jones, Dr. William Hyndman, Dr. William Cole, Dr. Kellie Leitch, Dr. Andrew Wong, Dr. Doug Hedden, Dr. Alain Ouimet, Dr. David Price, Dr. John McPherson, Dr. Jean-Pierre Farmer, Dr. Peter Fitzgerald, Ms. Julie Chan, Ms. Cathy Séguin, Mr. Jeff Mainland, Ms. Daniela Crivianu-Gaita, Mr. Tamas Fixler.
Contributors: Both of the authors and all of the members of the Canadian Paediatric Surgical Wait Times Study Group were involved in the design of the study, the collection and analysis of the data and the preparation of the manuscript. All of them approved the final version of the manuscript submitted for publication.
Funding: Financial support for this study was made possible through Health Canada’s Health Care Policy Contribution Policy Program, via the Canadian Paediatric Surgical Wait Times Projects. The views expressed in this article do not necessarily represent the views of Health Canada.
References
- 1.Warnock GL. Meeting the challenges of reducing waiting times for surgery. Can J Surg 2005;48:349–51 [PMC free article] [PubMed] [Google Scholar]
- 2.Postl B. Final report of the federal advisor on wait times. Ottawa (ON): Health Canada; 2006. Available: www.hc-sc.gc.ca/hcs-sss/pubs/system-regime/2006-wait-attente/index-eng.php (accessed 2011 Apr. 23). [Google Scholar]
- 3.Federal transfers in support of the 2000/2003/2004 First Ministers’ Accords. Ottawa (ON): Department of Finance Canada; 2008. Available: www.fin.gc.ca/fedprov/fmAcc-eng.asp (accessed 2008 Dec. 17). [Google Scholar]
- 4.Racing 4 Kids’ Health — establishing priorities in Canadian child and youth health research. Ottawa (ON): Canadian Institutes of Health Research, Institute of Human Development, Child and Youth Health, the National Child and Youth Coalition and SickKids Foundation; 2007 [Google Scholar]
- 5.Miller GG. Waiting for an operation: parents’ perspectives. Can J Surg 2004;47:179–81 [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison RV, Gordon KA, Mount RJ. Is there a critical period for cochlear implantation in congenitally deaf children? Analyses of hearing and speech perception performance after implantation. Dev Psychobiol 2005;46:252–61 [DOI] [PubMed] [Google Scholar]
- 7.Wright JG, Li K, Seguin C, et al. Development of paediatric wait time access targets. Can J Surg 2011;52:107–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.P-CATS list Toronto (ON): Canadian Paediatric Surgical Wait Times; 2010. Available: www.waittimealliance.ca/waittimes/P-CATS-List_en.pdf (accessed 2011 Apr. 27). [Google Scholar]
- 9.Surgical volume trends, 2008 — within and beyond wait time priority areas. Ottawa, (ON): Canadian Institute for Health Information (CIHI); 2008 [Google Scholar]
- 10.Hébert PC. An open letter to the minister of health. CMAJ 2009; 180:903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng SM, Irish JC, Thompson LJ. Contract management of Ontario’s cancer surgery wait times strategy. Healthc Q 2007; 10:51–8 [DOI] [PubMed] [Google Scholar]
- 12.Schroth RJ, Morey B. Providing timely dental treatment for young children under general anesthesia is a government priority. J Can Dent Assoc 2007;73:241–3 [PubMed] [Google Scholar]
- 13.Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc 2000;131:887–9 [DOI] [PubMed] [Google Scholar]
- 14.Donahue SP. Pediatric strabismus. N Engl J Med 2007;356:1040–7 [DOI] [PubMed] [Google Scholar]
- 15.Anastassov GE, Joos U. Comprehensive management of cleft lip and palate deformities. J Oral Maxillofac Surg 2001;59:1062–75 [DOI] [PubMed] [Google Scholar]
- 16.Zamakhshary M, Teresa T, Guan J, et al. Risk of incarceration of inguinal hernia among infants and young children awaiting elective surgery. CMAJ 2008;179:1001–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.