Abstract
HIV continues to exact an enormous toll on society and to disproportionately affect gay and bisexual men and other men who have sex with men (MSM). Innovative prevention interventions are needed to reverse this trend. In August 2009, the U.S. National Institute of Mental Health and the Centers for Disease Control and Prevention convened a meeting of scientists, community representatives, advocates, and federal partners to discuss innovative prevention-intervention science. The meeting was structured to maximize discussion of (1) healthy sex interventions, (2) community and structural interventions, (3) integrated biomedical and behavioral interventions, and (4) interventions to improve uptake of HIV testing. Presentations and discussion focused on research gaps in designing risk-reducing and sexual health-promoting interventions for MSM, including interventions to address mental health, substance use, disclosure, and stigma. This article summarizes the meeting proceedings, highlights key points, and outlines future directions.
Approximately 1.1 million people are living with human immunodeficiency virus (HIV) in the United States, and an estimated 56,300 incident infections in adults and adolescents occurred in 2006.1 Although acquired immunodeficiency syndrome (AIDS) morbidity and mortality have declined due to effective antiretroviral treatments, HIV continues to bring immense suffering, cause needless loss of life, and exact an enormous financial cost.2 HIV continues to disproportionately affect gay and bisexual men and other men who have sex with men (MSM), and innovative prevention interventions are needed.
In the U.S., MSM account for 53% of estimated incident HIV infections and are 60 times as likely to be diagnosed with HIV as other men and 54 times as likely to be diagnosed with HIV as women.1,3 Differential rates by race/ethnicity and age suggest important directions for new and effective interventions targeted to MSM most in need.3 Although evidence-based behavioral HIV prevention interventions are reaching some MSM, the vast majority of men who might benefit are not receiving these interventions.2,4 The continuing disproportionate rates of HIV among MSM in the U.S. suggest the need for integrated approaches to HIV prevention that incorporate behavioral, structural, and biomedical strategies.5–7
Innovations are particularly needed in light of changes in the broader social climate and scientific advances that have highlighted the myriad factors that may impact the success of existing prevention efforts. Some of these factors include the continued reporting of low-risk perception due to beliefs that effective treatment of HIV eliminates transmissibility, and evidence of use of strategies in addition to or aside from condom use, such as limiting sexual partners based on perceived HIV serostatus (e.g., seroadaptive strategies).8 The context for prevention is also different in the ways that MSM seek partners. The ubiquitous use of the Internet and social networking websites offers ways for MSM, particularly young MSM, to rapidly share information. In addition, use of cell-phone applications allows for information to be shared in real time and, thus, information has the potential to instantly impact behavior. These trends are also embedded in the larger context, where media images overwhelmingly depict socially sanctioned heterosexual relationships, and media coverage of policies and practices highlights a national divide in the acceptance of same-sex relationships.
Advances in biomedical HIV prevention efforts represent another contextual shift; male circumcision, pre- and post-exposure prophylaxis, the development of rectal microbicides, and earlier initiation of HIV treatment—if proven successful through clinical trials—will increase prevention options. Depending on the availability of these biomedical strategies, it will be critical to understand the impact of these interventions on behavior, including use of biomedical prevention in the context of currently effective strategies, such as condom use. For example, using antiretroviral medications to prevent HIV—preexposure prophylaxis (PrEP)—is a promising approach receiving significant attention. Several clinical trials investigating PrEP are underway, with minimal evidence of off-label PrEP use among MSM in the U.S. In preliminary studies conducted by Mayer and colleagues, MSM expressed interest in PrEP use if it could be demonstrated as effective, safe, and inexpensive with minimal side effects.9 Updates on the ongoing PrEP studies can be found online.10 It is most likely that any biomedically derived approach will be used in combination with existing and novel behaviorally derived approaches. Irrespective of the findings of these biomedical HIV prevention trials, the next generation of HIV prevention interventions will need to address and account for contextual shifts in the realities, beliefs, and behaviors across the diverse spectrum of MSM living in the U.S.
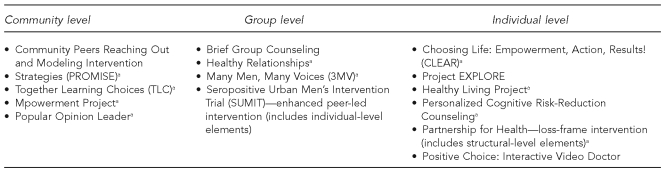
There are currently a number of nationally disseminated evidence-based interventions (EBIs) for HIV prevention for MSM. As the primary federal agency funding prevention activities, the Centers for Disease Control and Prevention's (CDC's) Division of HIV/AIDS Prevention (DHAP) spent approximately $401 million in fiscal year 2009 to support intervention implementation of HIV prevention programs by health departments and community-based organizations (CBOs) across the country. DHAP's research-to-practice model supports (1) the identification of EBIs through its Prevention Research Synthesis system, (2) the packaging of EBIs through its Replicating Effective Programs project, and (3) the national dissemination of EBIs through its Diffusion of Effective Behavioral Interventions project. As of October 2010, the Prevention Research Synthesis program had identified 14 EBIs for MSM, and 10 interventions had been packaged and nationally disseminated11,12 (Figure 1). Ten of the EBIs intervene at the individual or group level, while four interventions try to generate change at the community level. Some of these interventions also have structural elements (e.g., changing clinic practices or procedures). Overall, the total number of packaged interventions available to address the HIV prevention needs among all MSM is not in proportion to the disease burden in the MSM community. Specifically, only a small number of interventions specifically target African American MSM and none target Latino MSM, which represents a serious gap in the research, given the epidemiologic data. Detailed descriptions of each intervention can be found online.10,11
Figure 1.
Centers for Disease Control and Prevention evidence-based human immunodeficiency virus prevention interventions for men who have sex with men
aIntervention has been packaged and nationally disseminated.
While the availability of behavioral interventions has increased rapidly, there are still groups of MSM for whom no EBI has been identified and disseminated. To accommodate the needs of health departments and CBOs to serve diverse communities of MSM, CDC guidance states that all EBIs can be adapted for specific populations, as long as the adapting agency does not change the intervention-specific core elements and instead only changes key characteristics.13 CDC also encourages the ongoing evaluation of CBO-developed “homegrown” interventions (e.g., those developed by community members), so that with the accumulation of scientific evidence, these interventions may become EBIs to be included in the compendium. For example, in fall 2010, CDC funded the rigorous evaluation of three homegrown, group-level interventions for African American and Latino MSM—two interventions were specifically developed for African American MSM and one was developed for Latino MSM.14 In addition, CDC has also partnered with CBOs to conduct outcome monitoring of EBIs.
There are strengths and weaknesses to CDC's system of identifying model programs and processes for adaptation of existing interventions. A dialogue has begun weighing the merits of different approaches to widespread uptake of interventions, including recent arguments in favor of a “common elements” approach (i.e., relying on intervention components that are common across different interventions) to enhancing wider HIV prevention.15 Exploring this dialogue fully—including the research agenda related to identifying the strengths and weaknesses of different approaches to implementation and dissemination—is beyond the scope of this article but is likely to be an important issue for future HIV prevention efforts as they pertain to MSM.
This article describes the proceedings of a satellite meeting at the 2009 National HIV Prevention Conference entitled, “Advancing Novel HIV Prevention Intervention Research with MSM.” Held in Atlanta, Georgia, on August 22–23, 2009, the meeting was jointly sponsored by the U.S. National Institute of Mental Health and CDC. The purpose was to convene HIV prevention scientists, community representatives, advocates, and federal partners to discuss innovative prevention-intervention science. The meeting was structured to maximize discussion of (1) healthy sex interventions, (2) community and structural interventions, (3) integrated biomedical and behavioral interventions, and (4) interventions to improve uptake of HIV testing. Meeting presentations and discussion focused on research gaps in designing risk-reducing and sexual health-promoting interventions for MSM, as well as addressing the broader needs of MSM, including interventions to address mental health, substance use, disclosure, and stigma.
REVIEW OF MEETING PROCEEDINGS
Innovative intervention directions
Although the interventions for MSM have been delivered to individuals, groups, and communities, they have focused predominantly on individual-level targets and outcomes. A key discussion point at the meeting was the importance of implementing the best EBIs at multiple levels to achieve the greatest and broadest public health impact. Thomas Frieden, MD, current CDC director, recently published a model of public health impact that posits that the most intensive interventions (e.g., frequent counseling and education at the individual or group level)—which may be important for a minority of MSM with the most intensive needs—result in the lowest population impact due to the challenges of broad dissemination and implementation.16 In contrast, interventions that address the social determinants of health (e.g., tobacco legislation) are less focused and targeted to the individual or group but have demonstrated the greatest population impact. Meeting participants emphasized the importance of developing and testing interventions at different levels (e.g., structural interventions) and combining prevention strategies across levels.
Several research studies are underway that attempt to combine interventions and model the impact. One National Institutes of Health-funded intervention trial, Prevention Umbrella for MSM in the Americas, will model interventions to select those with the greatest impact and gather community input to build a menu-based HIV prevention package. In addition, Kenneth Mayer, MD, highlighted an ongoing study from the HIV Prevention Trials Network that focuses on black MSM and exemplifies innovation in both its combination intervention and its social network recruitment approach.17 The primary aims are to identify recent HIV infection, increase HIV disclosure to reduce risk, treat sexually transmitted infections (STIs), address treatment needs for mental health and substance use, and increase access to social services. This novel intervention involves screening and enrolling sexual network members, treating STIs, and using peer health navigators for those who test positive for HIV. In the feasibility stage of the study, black MSM will be recruited in six U.S. cities to address feasibility-related questions, such as who will enroll and why, cultural considerations, network partners, and how to identify a large pool of participants.
Dr. Mayer and others also asserted that earlier treatm-ent initiation and, more generally, effective HIV treatment, combined with risk reduction for people in treatment, represent another important combination intervention. Moreover, participants pointed out that diagnosis and treatment of STIs is an essential component of HIV treatment as prevention. In his presentation, Dr. Mayer highlighted that antiretroviral therapy can improve longevity by decreasing viral load and may decrease transmission, but there are other important aspects to this approach that require examination. For example, while effective treatment increases survival, both duration of infectiousness and any risk compensation could attenuate treatment effects on HIV transmission. It will also be important to ensure that earlier offers for treatment do not exacerbate existing trends in racial/ethnic disparities in treatment access.
While the HIV Prevention Trials Network includes a social network component, more research is needed to determine how to best use social networks in interventions. Carl Latkin, PhD, reviewed the state of the science and highlighted questions about theory and measurement of MSM social networks that will require further study as interventions are developed. For example, research is needed to determine the proportion of the network that would need to be reached to influence the majority of network members. The stability of networks would also influence the design and impact of social network interventions for MSM. Broad issues that influence the impact of social network interventions include the extent to which MSM differ in their receptivity to social influence and limitations in social power, as well as mental health and substance abuse issues.
As part of multilevel intervention approaches, participants discussed the need for interventions that target MSM couples and examine outcomes at the level of the couple. Patrick Sullivan, DVM, PhD, highlighted one underutilized approach that encourages male couples to be tested for HIV and counseled together. He recently modeled HIV transmission using CDC's National HIV Behavioral Surveillance System data and estimated that 68% of HIV infections among MSM were attributable to main partners.18 With high transmission rates occurring within main partners, couples testing may be an important strategy to ensure accurate knowledge of serostatus. Programs targeted to heterosexual couples have been successfully implemented in Africa, and data suggest a 50% reduction in incidence and STIs as a result of these efforts.19 However, couples HIV testing is not routinely conducted in the U.S. due to privacy laws and longstanding practice. Dr. Sullivan presented unpublished focus group data that suggest the majority of MSM couples would accept couples testing. Focus group participants indicated that the process would be a symbol of commitment, an opportunity to disclose HIV status and share emotional support, and a way to allow monogamous couples to consider stopping condom use. In light of Dr. Sullivan's preliminary data, as well as data from other sources, participants discussed possible research gaps that remain related to methods of defining “main” partners, how partners change over time and over developmental stages (e.g., adolescence to young adulthood), and the role of partner concurrency and HIV serostatus of different partners (e.g., casual vs. main).
Consistent with the need for more attention on structural approaches and social determinants, Simon Rosser, PhD, discussed areas of future research including the influence of risk venues and policy/laws on HIV risk. A better understanding of the influence of structural factors, such as laws that prohibit same-sex marriage and adoption and legislation related to antidiscrimination and hate crime prosecution, could inform intervention development. Dr. Rosser presented unpublished analyses that suggest a negative relationship between internalized homo-negativity and cities with pro-gay laws, where study participants residing in more pro-gay cities reported less hostility, less heavy chronic use of alcohol, and fewer unprotected sexual acts. A primary limitation of these data is that they suggest an associative, not causal, relationship between laws and public health outcomes among MSM.
Participants discussed a number of challenges to intervening at the structural level. For example, the target of intervention may be quite distal from the risk behavior. Meeting participants discussed the development of interventions to address housing stability, bullying in schools, and community-level homophobia. There is also interest in bypassing individual behavior altogether by changing laws, structures, and risk contexts that, if adjusted, would limit access to risk situations or increase the likelihood that individuals would maintain healthy sexual behavior. As the intervention target (e.g., bullying in schools) is more distally associated with the intervention outcome (e.g., delay of sexual debut), it may be more difficult to find a strong effect, and the effect may not be seen for several years. More research is needed to answer critical questions about how these socioeconomic and sociocultural factors enhance risk of or provide protection from HIV transmission and acquisition.
The role of technology in innovative interventions
A topic that emerged during the talks on novel interventions was the role that technology can play in HIV risk and prevention. The Internet and cell-phone technology have dramatically changed the context within which MSM seek romantic and sexual partners and friendships, as well as how they maintain relationships. Gay men tend to be among the early adopters of new forms of technology. These environments are often viewed as conveying risk; however, there are some promising opportunities to harness new technologies to more fully understand sexual behavior and promote healthy sexual relationships. For example, the use of new forms of technology may help to increase -acceptability and engagement in HIV prevention activities among MSM.
One specific opportunity presented was the use of technology to collect more reliable and valid self-report data. Patrick Wilson, PhD, presented preliminary data on the use of online sex and drug diaries to evaluate the influence of situational variables on sexual behavior. Data were collected in an ongoing study of HIV-positive MSM, whereby men were asked to report on their sexual behavior, current affective state, and situational factors on a weekly basis. Situational factors included the characteristics of their sexual partners (i.e., relationship status, partner substance use, perceived physical attractiveness, and emotional closeness), communication about condom use, and the setting in which the sexual encounter occurred. Dr. Wilson's research highlights the potential for collecting real-time data with MSM using the Internet and exploring relationships between factors that have typically only been retrospectively collected. Additionally, cell phones and the Internet can be used to make the recording of behavior more user-friendly and transportable. While technology could enhance the type and quality of behavioral data collection, it could also serve as a self-monitoring-based intervention.
Another promising opportunity is the use of technology in the delivery of HIV prevention interventions. Diaries could be used to provide feedback that informs the individual about his behavior over time and, perhaps in conjunction with motivational interviewing or another intervention approach, could be used to reduce risk. Gary Harper, PhD, encouraged participants to think about how technology, specifically social networking sites, can be used to support healthy sexual development among young gay and bisexual men. The discussion highlighted the need for young MSM to be exposed to developmentally and culturally appropriate interventions that promote healthy sexual and relationship development. At a minimum, technology can be an appropriate medium to ensure a broad reach.
Enhancing policy and program research
Meeting participants noted that a critical development in public health policy has been a growing recognition that improving the impact of interventions targeting risk behaviors and extending them to the population level requires greater consideration of the social and biological determinants of health.20–23 These determinants include an array of contextual factors, including poverty, power inequities, stigma, discrimination, incarceration, and inadequate access to preventive and medical care.21–24 In an effort to better understand the impact of these factors, the World Health Organization established a Commission on Social Determinants of Health in 2005, which was designed to develop recommendations for resolving avoidable systematic differences in health outcomes for subsets of the population. The Commission proposed three overarching recommendations thought to be instrumental in closing the gap in health outcomes within societies: improving daily living conditions, addressing inequities in the organization of societies, and assessing the results of interventions.25 Similarly, CDC has embarked on an innovative approach to reduce health disparities by initiating a range of activities in high-priority communities that seek to better understand drivers of HIV infection, expand testing and access to care, develop and scale up new interventions, and mobilize communities.26,27
One example of policy and programmatic change has been expanding implementation of CDC HIV testing guidelines and addressing the challenges that remain, given fears of HIV stigma and discrimination, unauthorized disclosure of serostatus, or living with a chronic disease. One programmatic and, in some cases, policy change to improve HIV testing in high-priority populations may be to bundle HIV and other tests, as recent studies have shown improved receipt of HIV results when these are combined with tests for other STIs or bundled with other medical care.28,29 Recent developments in the policy arena that could impact the HIV epidemic in the U.S. include the removal of the HIV travel ban and the decriminalization of sexual behavior. For MSM specifically, potential policy changes in the military and the passage of marriage equality would help create a culture of inclusion of MSM into society that could serve a health-promoting and disease-preventing function. Policy, law, and program research could enhance current scale-up of interventions, as well as inform intervention development. However, there was discussion about the expertise required to conduct this type of research and the limitations of currently available funding mechanisms.
SUMMARY OF MEETING DISCUSSION
Evidence suggests that prevention interventions, when deployed to those most vulnerable to HIV, reduce the rate of new infections. It has been estimated that as of 2000, the coordinated federal response to the epidemic entailed $10.1 billion and helped to avert 350,000 new infections.2,30 Even so, the number of new infections is unacceptable, and MSM of all races/ethnicities continue to shoulder a disproportionate burden of HIV disease. Unfortunately, the most commonly deployed interventions, which focus almost exclusively on individuals' behaviors, will likely only be palliative unless scaled appropriately and complemented by other prevention strategies, including those that take into account structural factors.1,24
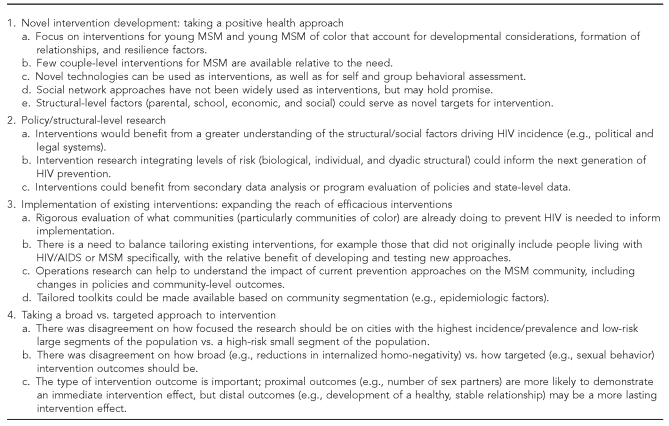
The meeting discussion highlighted important future directions to address the HIV prevention needs of MSM (Figure 2). Participants noted that it is critical that prevention priorities are aligned with local HIV epidemic trends. This means increasing the number and scope of available best-evidence interventions to address the prevention needs of at-risk MSM, including developmentally appropriate interventions for young MSM. For example, young MSM may require interventions that promote healthy sexual and relationship development, while older MSM may require approaches that heighten their awareness of continued risk, presented in fresh and stimulating ways to combat years of living with the threat of HIV. A greater understanding of the contexts in which risk occurs will inevitably increase the focus on dyads and sexual networks. Indeed, an underused approach to HIV prevention for MSM is promoting couples HIV testing and relationship stability.
Figure 2.
Themes from workgroup discussions highlighting future directions to address the HIV prevention needs of MSM: Advancing Novel HIV Prevention Intervention Research with MSM Meeting, August 2009
HIV = human immunodeficiency virus
MSM = men who have sex with men
AIDS = acquired immunodeficiency syndrome
Novel intervention approaches are necessary in concert with combined, multilevel structural approaches, including greater attention to the social and biological determinants that influence HIV risk and behavior—unemployment, homelessness, impaired access to quality prevention and medical care, mental illness, substance abuse and dependence, community viral loads, and genetics.20,26 At the same time, it is imperative to gain a greater understanding of those influences that serve to buffer against adverse health outcomes, such as parental support, comprehensive school-based sex education, and school- and/or church-sanctioned gay peer groups and activities. Lastly, more research is needed on the synergistic effects of new biomedical prevention strategies (e.g., the use of antiretrovirals to prevent onward transmission and non-coitally dependent PrEP) that, when combined with behavioral risk-reduction approaches, hold promise in stemming incident infections.
At the same time that novel interventions are developed, research is needed to understand how best to expand the reach of existing interventions. Participants discussed several future directions of research and practice, including continued evaluation of homegrown interventions, how much to tailor vs. develop new interventions, expanding the role of operational research, and creating tailored toolkits based on local epidemiologic data. In the context of limited resources, the discussion included debate on two approaches to resource allocation: interventions to reach broad groups of individuals (some of whom are at a relatively lower risk of HIV) and interventions targeting subgroups to ensure only the individuals at risk are provided intervention. One aim of a broad, universal approach to prevention would be to create an environment or context that supports sexual health for all individuals, including MSM. This approach could include addressing HIV stigma and homophobia as much as they are barriers to HIV prevention. The aim of a more targeted approach would be to identify those segments of the population who are most at risk for HIV and provide complete coverage, perhaps with more intensive interventions. There was general agreement in the meeting that a balanced approach combining universal with targeted intervention would be optimal when possible; however, determining the optimal balance given limited funds remains a significant challenge.
CONCLUSION
This meeting was a collaborative effort between federal partners—the National Institute of Mental Health and CDC—and the discussion highlighted the continued need for the involvement of federal, state, and local agencies, as well as active community involvement, in future efforts to address the HIV epidemic among MSM. In addition to enhanced and continued collaboration, future HIV prevention efforts may gain greater traction if placed in the broader context of sexual health. When HIV prevention and attention to other infectious diseases are embedded in this larger agenda, individuals of all demographic characteristics may be more likely to perceive that prevention messages relate to their lives. As the HIV epidemic continues to disproportionately impact MSM and reflect racial/ethnic and age-associated disparities, innovative interventions are needed that integrate the current social, political, and contextual factors of the lives of all MSM.
Footnotes
The views expressed in this article do not necessarily represent the views of the National Institutes of Health, National Institute of Mental Health, Department of Health and Human Services, Centers for Disease Control and Prevention, or the U.S. government.
REFERENCES
- 1.Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holtgrave DR, Curran JW. What works, and what remains to be done, in HIV prevention in the United States. Annu Rev Public Health. 2006;27:261–75. doi: 10.1146/annurev.publhealth.26.021304.144454. [DOI] [PubMed] [Google Scholar]
- 3.Purcell DW, Johnson C, Lansky A, Prejean J, Stein R, Denning P, et al. Calculating HIV and syphilis rates for risk groups: estimating the national population size of men who have sex with men. Presented at the National STD Prevention Conference; 2010 Mar 8–11; Atlanta. [Google Scholar]
- 4.Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, Dinenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003–April 2005. MMWR Surveill Summ. 2006;55(6):1–16. [PubMed] [Google Scholar]
- 5.Jaffe HW, Valdiserri RO, De Cock KM. The reemerging HIV/AIDS epidemic in men who have sex with men. JAMA. 2007;298:2412–4. doi: 10.1001/jama.298.20.2412. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan PS, Hamouda O, Delpech V, Geduld JE, Prejean J, Semaille C, et al. Reemergence of the HIV epidemic among men who have sex with men in North America, Western Europe, and Australia, 1996–2005. Ann Epidemiol. 2009;19:423–31. doi: 10.1016/j.annepidem.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 7.El-Sadr WM, Mayer KH, Hodder SL. AIDS in America—forgotten but not gone. N Engl J Med. 2010;362:967–70. doi: 10.1056/NEJMp1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalichman SC, Eaton L, White D, Cherry C, Pope H, Cain D, et al. Beliefs about treatments for HIV/AIDS and sexual risk behaviors among men who have sex with men, 1997–2006. J Behav Med. 2007;30:497–503. doi: 10.1007/s10865-007-9123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr. 2009;50:77–83. doi: 10.1097/QAI.0b013e31818d5a27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AVAC: Global Advocacy for HIV Prevention. Pre-exposure prophylaxis (PrEP) [cited 2010 May 17]. Available from: URL: http://www.avac.org/ht/d/sp/i/262/pid/262/cat_id/458/cids/453,458.
- 11.Centers for Disease Control and Prevention (US) 2009 compendium of evidence-based HIV prevention interventions. [cited 2011 Feb 7]. Available from: URL: http://www.cdc.gov/hiv/topics/research/prs/evidence-based-interventions.htm.
- 12.CDC (US) About DEBI. [cited 2011 Feb 7]. Available from: URL: http://www.effectiveinterventions.org/en/AboutDebi.aspx.
- 13.McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, et al. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18(4) Suppl A:59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- 14.Department of Health and Human Services (US) Evaluating locally developed (homegrown) HIV prevention interventions for African American and Hispanic/Latino men who have sex with men (MSM) [cited 2010 Apr 6]. Available from: URL: http://www07.grants.gov/search/search.do?oppId=44506&mode=VIEW.
- 15.Rotheram-Borus MJ, Swendeman D, Flannery D. Family wellness, not HIV prevention. AIDS Behav. 2009;13:409–13. doi: 10.1007/s10461-008-9515-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.HIV Prevention Trials Network. HPTN 061. [cited 2010 May 17]. Available from: URL: http://www.hptn.org/research_studies/hptn061.asp.
- 18.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five U.S. cities. AIDS. 2009;23:1153–62. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 19.Allen S, Serufilira A, Bogaerts J, Van de Perre P, Nsengumuremyi F, Lindan C, et al. Confidential HIV testing and condom promotion in Africa.Impact on HIV and gonorrhea rates. JAMA. 1992;268:3338–43. [PubMed] [Google Scholar]
- 20.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62:1650–71. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 21.Fenton KA, Wasserheit JN. The courage to learn from our failures: syphilis control in men who have sex with men. Sex Transm Dis. 2007;34:162–5. doi: 10.1097/01.olq.0000259398.70789.c6. [DOI] [PubMed] [Google Scholar]
- 22.Merson M, Padian N, Coates TJ, Gupta GR, Bertozzi SM, Piot P, et al. Combination HIV prevention. Lancet. 2008;372:1805–6. doi: 10.1016/S0140-6736(08)61752-3. [DOI] [PubMed] [Google Scholar]
- 23.Merson MH, O'Malley J, Serwadda D, Apisuk C. The history and challenge of HIV prevention. Lancet. 2008;372:475–88. doi: 10.1016/S0140-6736(08)60884-3. [DOI] [PubMed] [Google Scholar]
- 24.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372:764–75. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 25.Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Commission on Social Determinants of Health Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 26.Sutton MY, Jones RL, Wolitski RJ, Cleveland JC, Dean HD, Fenton KA. A review of the Centers for Disease Control and Prevention's response to the HIV/AIDS crisis among blacks in the United States, 1981–2009. Am J Public Health. 2009;99(Suppl 2):S351–9. doi: 10.2105/AJPH.2008.157958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC (US) External consultation meeting report. Atlanta: CDC; 2009. Addressing social determinants of health: accelerating the prevention and control of HIV/AIDS, viral hepatitis, STD and TB. [Google Scholar]
- 28.Galvan FH, Bluthenthal RN, Ani C, Bing EG. Increasing HIV testing among Latinos by bundling HIV testing with other tests. J Urban Health. 2006;83:849–59. doi: 10.1007/s11524-006-9072-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reynolds GL, Fisher DG, Napper LE, Marsh KA, Willey C, Brooks R. Results from a multiple morbidities testing program offering rapid HIV testing bundled with hepatitis and sexually transmitted infection testing. Public Health Rep. 2008;123(Suppl 3):63–9. doi: 10.1177/00333549081230S308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CDC (US) HIV prevention in the United States: at a critical crossroads. Atlanta: CDC; 2009. [Google Scholar]