Abstract
Objectives
A critical issue in health-care reform concerns how to realign health-care delivery systems to manage medical care services for people with ongoing and costly needs for care. We examined the overlapping health-care needs of two such population groups among the U.S. working-age population (those aged 18–64 years): people with chronic medical conditions and people with disabilities.
Methods
Using the Medical Expenditure Panel Survey (2002–2004), we examined differences in health status, service use, and access to care among and between working-age adults reporting disabilities and/or one or more chronic conditions. We also analyzed people with three key chronic conditions: arthritis, diabetes, and depression.
Results
More than half of working-age people with disabilities reported having more than one chronic condition. Among those with activities of daily living or instrumental activities of daily living limitations, 35% reported four or more chronic conditions at a time. We found considerable variability in access problems and service use depending on how we accounted for the overlap of multiple conditions among people with arthritis, diabetes, and depression. However, disability consistently predicted higher emergency department use, higher hospitalization rates, and greater access problems.
Conclusions
The overall prevalence of chronic conditions among the U.S. working-age population, coupled with the high concentration of multiple chronic conditions among those with disabilities, underscores the importance of reforming health-care delivery systems to provide person-centered care over time. New policy-relevant measures that transcend diagnosis are required to track the ongoing needs for health services that these populations present.
As the United States considers dramatic changes in the way its health-care delivery system is organized, two groups merit particular attention: individuals with disabilities and individuals with chronic health conditions. At a time when health-care costs are escalating at an unsustainable pace, both groups consume health-care services at a disproportionately high rate1–6 while also experiencing less than optimal health outcomes.7–9 Furthermore, health-care resources are not equitably distributed,10 calling for substantive changes in the way in which services are provided.
The health of people with disabilities gained additional visibility on the national health agenda via the Healthy People 2010 objectives11 and the Surgeon General's Call to Action to Improve the Health and Wellness of Persons with Disabilities.12 At the same time, the growing number of adults with chronic conditions has led to a proliferation of disease management programs,13–17 as well as a substantial body of research describing chronic disease, its consequences, and associated responses.1,2,9,18,19 What remains less articulated in the scientific literature is that these are actually overlapping groups. While adults with disabilities are likely to have multiple chronic conditions, adults with chronic conditions are likely to develop limitations in functioning or participation, particularly as conditions accumulate over time. In this study, we directly analyzed this overlap, with a focus on health, access to care, and service use in the U.S.
Previous research shows that a substantial number of adults have multiple chronic conditions and may also have limitations in activities or functioning. For instance, in 1997, nearly 25% of Medicare beneficiaries had limitations in activities of daily living (ADLs).3 Within this group, the prevalence of cancer, stroke, diabetes, and rheumatoid arthritis was each more than 20%, and the prevalence of hypertension and osteoarthritis was higher than 50%. Treatment of these conditions required up to one health-care visit a week, and these individuals were twice as likely to be dissatisfied with the coordination of their care.20
Whether one considers the new medical home initiatives,21 obesity reduction,22 disease self-management,23 prevention of secondary conditions among people with disabilities,24 or any number of further priority items on the nation's public health agenda,25 there remains a pressing need to quantify the extent of comorbidity in the U.S. population and to clarify its associations with disability. About half of all Americans have at least one chronic condition, and given that roughly half of those individuals actually have more than one such condition at a time, the pursuit of these agenda items may be hampered if approached only one disease at a time.2 Furthermore, when individuals accrue limitations in how they function or the activities they can do, additional interventions may be required to assure their access to health-care services, to coordinate the providers involved in their care, or to craft treatment regimens that accommodate their functional needs.26
To build upon the existing literature, we analyzed a nationally representative sample of working-age Americans, clarifying the way in which health, access to care, and service use is impacted by a single chronic condition vs. multiple chronic conditions, with or without self-reported disability limitations. As exemplars, we also examined three conditions in greater detail: arthritis, diabetes, and depression. Among the most highly prevalent chronic conditions in the U.S., these three conditions were selected because they potentially result in a wide range of health and functional impacts across different body systems, are accompanied by differing constellations of comorbid conditions, and may require care from providers in differing specialties or settings.27–29 Thus, we examined the relative contributions of a single primary diagnosis, multiple comorbidities, and disability limitations to several key health-care measures, including access to care, ambulatory visits, hospitalizations, and emergency department (ED) use.
While substantial health services research has been conducted on the impact of chronic conditions on older Americans3,30,31 and children,32–34 less is known about these phenomena among the working-aged, particularly for people with disabilities. Additionally, the impact of chronic conditions and disability on major life activities, such as school or work, necessarily varies with life course stage. Given the large size of the working-age population, additional concerns regarding their insurance coverage, and their distinct role expectations relative to older adults or children, we limited our analysis to people aged 18–64 years.
METHODS
Data source and key measures
We analyzed the 2002–2004 Medical Expenditure Panel Survey (MEPS). After pooling years, we used 58,408 cases to obtain our weighted estimates for people aged 18–64 years. Disability limitations were recorded via self-report in the following domains: physical functioning; sensory impairment; cognitive difficulties; activities such as work, housework, or school; social limitations; assistive device use; and ADLs/instrumental ADLs (IADLs), which together include help or supervision with such activities as bathing, dressing, preparing meals, and shopping. Because previous studies have shown that people reporting ADL or IADL limitations have elevated use of health services compared with people who have other kinds of limitations,35,36 we flagged individuals reporting ADL or IADL limitations for further subgroup analysis.
Separately, we identified people as having a chronic condition if they reported any diagnosis from a well-validated list.1,5,37,38 This list included health and mental health conditions that, from a medical standpoint, are each expected to last at least 12 months and are likely to result in a need for ongoing care, including medications, therapies, medical equipment, or changes in diet or physical activity. We characterized any condition not in this list, such as upper respiratory infection, as being acute.
Additional measures and statistical methods
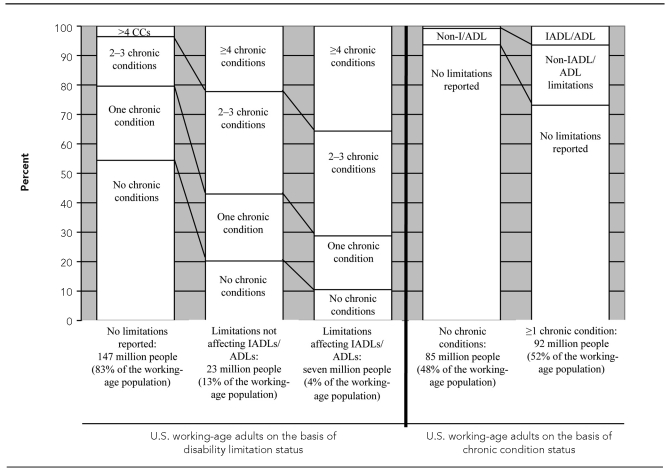
We analyzed the overlap of chronic conditions with disability (Figure) and generated a profile of working-age people, considering chronic condition status and disability-related limitations side-by-side. Table 1 shows estimates of basic sociodemographic measures, health conditions, health-related variables, and access to care. It also shows five annual measures of health service utilization, including three measures of ambulatory visits, as well as hospitalizations and ED use. We compared the aforementioned measures between people with no limitations, people with non-ADL/IADL limitations, and people with ADL/IADL limitations. Separately, we also compared these measures among people with and without chronic conditions.
Figure.
The overlap of chronic conditions and disability-related limitations in the U.S.: pooled annual estimates of people aged 18–64 years, 2002–2004 MEPS
MEPS = Medical Expenditure Panel Survey
CC = chronic condition
IADL = instrumental activity of daily living
ADL = activity of daily living
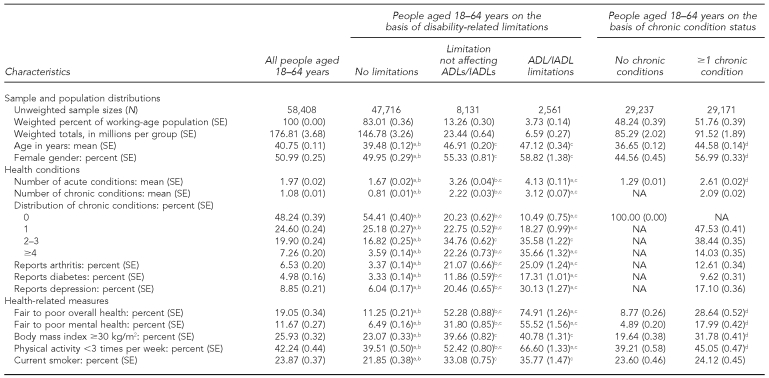
Table 1.
Population sizes, health conditions, health-related measures, access to care, and service utilization on the basis of disability-related limitations and chronic condition status: pooled annual estimates of people aged 18–64 years, 2002–2004 MEPS
NOTE: Significance (p<0.05) determined after controlling the false discovery rate. Tests were conducted row-wise and separately for disability-related limitations and chronic condition status.
aDiffers significantly from people with limitations not affecting ADLs/IADLs
bDiffers significantly from people with ADLs/IADLs limitations
cDiffers significantly from people with no limitations
dDiffers significantly from people without chronic conditions
eAmong people with at least one visit to a physician
fAmong people with at least one visit to a non-MD health-care provider
MEPS = Medical Expenditure Panel Survey
ADL = activity of daily living
IADL = instrumental activity of daily living
SE = standard error
NA = not applicable
kg/m2 = kilograms per meter squared
MD = medical doctor
To complement these general analyses, we next examined three specific chronic conditions in greater detail using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)39 codes: arthritis (ICD-9-CM 714.00–714.89, 715.00–715.98, and 716.00–716.99), diabetes (ICD-9-CM 250.00–250.93), and depression (ICD-9-CM 311.0). In Table 2, separately for each of these conditions, we compared (1) people without the exemplar condition, (2) people reporting that condition in absence of other chronic conditions, and (3) people reporting that condition in conjunction with one or more additional chronic conditions. The comparisons included prevalence, number of health conditions reported, overall health, and overall mental health. We then compared these same measures for people reporting non-ADL/IADL limitations in groups 1, 2, and 3, followed by people with ADL/IADL limitations in these three groups. All bivariate comparisons described previously were based on pairwise t-tests; we controlled the false discovery rate40 before flagging significant differences (p<0.05) in Tables 1 and 2.
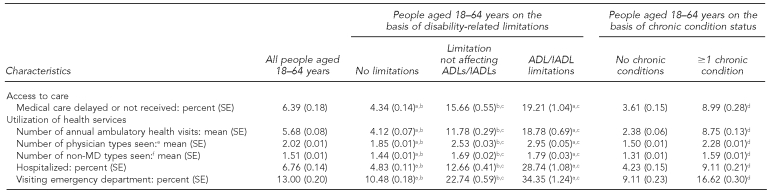
Table 2.
Arthropathies, diabetes, and depression with and without other chronic health conditions and disability-related limitations: prevalence, mean health conditions, overall health, and overall mental health:a pooled annual estimates, 2002–2004 MEPS
aSignificance (p<0.05) determined after controlling the false discovery rate. Two varieties of significance tests were conducted. First, separately for each main condition (e.g., arthritis), three groups were compared with one another on a given column variable: people with no report of the condition, people reporting the condition in absence of other chronic conditions, and people reporting the condition in addition to one or more further chronic conditions (prevalence was excluded in these analyses). Second, differences in the column variable were tested between people with non-ADL/IADL limitations in each of the three groups, followed by people with ADL/IADL limitations in each of the three groups. Within a given column, the superscripted numbers/letters indicate the row(s) at which a significantly differing estimate was recorded. Estimates with relative SE >30% are suppressed.
bRelative SE >30%
MEPS = Medical Expenditure Panel Survey
SE = standard error
ADL = activity of daily living
IADL = instrumental activity of daily living
Sup. = suppressed
Next, we fit a series of models designed to test the relative contributions of the presence or absence of the exemplar condition, the number of additional chronic and acute health conditions, and the extent of disability limitations to the access to care and service utilization measures described previously. These models were fit separately for arthritis, diabetes, and depression. Taking ambulatory visits by people with and without arthritis as an example (Table 3), we first fit a naïve model, adjusting for covariate differences in age, gender, race/ethnicity, education, poverty status, and health insurance coverage, but only including a single dichotomous measure to represent arthritis/no arthritis. Using this model as a base, we sequentially added controls, leading up to a full model including the covariates, arthritis status, number of other chronic conditions, number of acute conditions, and disability status (whether none, non-ADL/IADL limitations, or ADL/IADL limitations). Table 3 contains the coefficients for total ambulatory visits by people with and without arthritis using a naïve vs. a full model.
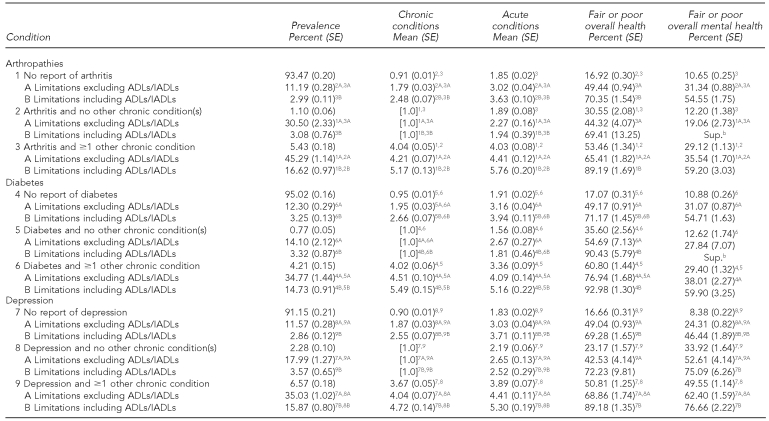
Table 3.
A comparison of two log-link models of annual ambulatory health-care visits for people aged 18–64 years with and without arthritis: MEPS, 2002–2004
aSignificant at p<0.05
MEPS = Medical Expenditure Panel Survey
SE = standard error
CI = confidence interval
FPL = federal poverty level
ADL = activity of daily living
IADL = instrumental activity of daily living
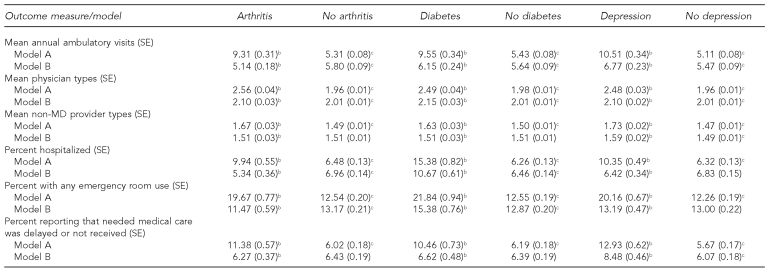
Last, we summarized the modeling estimates. For dependent variables taking the form of annual counts (total ambulatory visits, number of medical doctor [MD] and non-MD specialty types visited), we fit log-link models. For dichotomous dependent variables (e.g., any/no hospitalization, any/no ED visits), we fit logistic regression models. We then computed covariate-controlled, predicted marginal estimates for each of the access and utilization outcome measures, testing the statistical significance of the differences between the naïve and full models (Table 4). Throughout all analyses described in this section, we used SUDAAN®41 to adjust for the complex sampling plan in the MEPS.
Table 4.
A comparison of two forms of multivariate models: covariate controlled, predicted marginal estimates of utilization of and access to care by people aged 18–64 years with and without arthritis, diabetes, and depression: MEPS, 2002–2004a
aModels of form A include controls for age, gender, race/ethnicity, education, poverty status, health insurance coverage status, and a single dichotomous measure reflecting the presence or absence of the health condition of interest. Models of form B include these same variables, but also include measures of disability (with and without activities of daily living/instrumental activities of daily living limitations), the number of additional chronic conditions reported, and the number of acute conditions.
bIndicates a significant difference between the estimates generated by models A and B for people with the given condition
cIndicates that the given estimate for people without the condition differs significantly (p<0.05) from the estimate for people with the condition based upon the model in that row
MEPS = Medical Expenditure Panel Survey
SE = standard error
MD = medical doctor
RESULTS
As shown in the Figure, we found that approximately 30 million working-age people reported disabilities during a given year, constituting roughly 17% of that age group. Among the 23 million people who had limitations that did not include ADLs or IADLs, the portion reporting one or more chronic conditions was 80%, with the majority (56%) reporting multiple chronic conditions. For those seven million people who had a need for help or supervision with ADLs or IADLs, 90% reported at least one chronic condition, with 35% reporting four or more such conditions concurrently.
People with one or more chronic conditions actually represented the majority of the U.S. working-age population, totaling roughly 92 million people. Approximately 25% of this group reported any disability, while approximately 6% reported a limitation specifically affecting ADLs/IADLs.
Table 1 shows two possible ways of segmenting the U.S. working-age population: by disability status and by chronic condition status. When compared with people without disabilities, people with disabilities reported significantly higher rates of not only chronic but acute conditions, with higher percentages also reporting fair to poor overall health, fair to poor mental health, obesity, physical inactivity, and smoking. The rates of chronic (mean = 3.1) and acute (mean = 4.1) conditions were highest among people specifically with ADL/IADL limitations, as were the percentages reporting fair to poor health (75%), fair to poor mental health (56%), and physical activity <3 times per week (67%). Relative to individuals without disabilities, people with disabilities also reported significantly higher ambulatory health visits to a wider array of physician types and non-MD health provider types, particularly when the limitations reported affected ADLs/IADLs. People with disabilities also reported higher percentages of hospitalizations, ED visits, and access problems.
Many of these same general observations regarding health status and service use held when people with chronic conditions were compared with people who had no chronic conditions. However, because this was a much larger group that included approximately 67 million people who did not report the limitations associated with disability, the differences observed were of a smaller magnitude.
Table 2 shows three specific health conditions in greater detail. We first compared people with no arthritis, people with arthritis but no other chronic conditions, and people who reported arthritis with at least one other chronic condition during the year. While the annual prevalence of arthritis among the working-age population in MEPS was 6.5% (Table 1), 83% of those who reported arthritis also reported at least one other chronic condition. Among those with arthritis and at least one additional chronic condition, the mean number of chronic conditions reported was higher than four, as was the number of acute conditions reported during the year; half reported fair or poor overall health and almost one-third reported fair or poor mental health. Each of these estimates was substantially higher than those obtained when we examined arthritis in isolation from other chronic conditions. This same issue recurred for diabetes and depression, as it presumably did for most chronic conditions.
Another layer of complexity was added when we considered disability. About 15% of people without arthritis reported some variety of disability. When we examined people who reported arthritis in absence of other chronic conditions, this estimate roughly doubled. However, as noted previously, the large majority of people with arthritis actually had more than one chronic condition at a time. When we examined individuals who reported arthritis along with at least one other chronic condition, we found that more than 60% reported a disability. Among these people who reported disabilities, we also found a sizable accumulation of additional health conditions (both chronic and acute), with large percentages reporting that they were in fair or poor overall health and/or mental health (data not shown).
Table 3 shows the relative contributions of the diagnosis of arthritis, disability, and co-occurring health conditions to ambulatory health-care visits by comparing two different models. Both models were adjusted for age, gender, race/ethnicity, education, poverty status, and health insurance coverage status. Model A was our naïve model, adding only a single dichotomous variable recording arthritis to the covariates. Model B was our full model, including two dummies to represent disability (with and without ADL/IADL limitation), number of chronic conditions (omitting arthritis), and number of acute conditions. In model A, we found that arthritis was a significant predictor of ambulatory visits, increasing the visit rate by a factor of 1.8 (incidence density ratio [IDR] = 1.75, 95% confidence interval [CI] 1.63, 1.88). In model B, after including controls for disability limitations, chronic conditions, and acute conditions, having arthritis actually predicted significantly fewer ambulatory visits (IDR=0.89, 95% CI 0.82, 0.95).
We replicated this approach for diabetes and depression (results not shown). We then fit the same varie-ties of models to the number of physician types seen, the number of non-MD provider types visited during the year, the percentage reporting hospitalization(s), the percentage reporting one or more ED visits, and the percentage reporting access problems. From the obtained coefficients, we calculated predicted marginal estimates, holding all other variables constant at their weighted population levels to generate estimates for people with and without the condition of interest. The results are shown in Table 4.
Across the entire set of results in Table 4, we found numerous significant differences between the estimates generated by these models. In all such instances, model A (with no controls for disability or other health conditions) resulted in higher estimates on the predicted outcome for people with the referenced condition than did model B. In several instances, we also found that after controlling for disability limitations and other health conditions, the exemplar condition no longer resulted in a significant difference or switched to a negative predictor of the outcome (as with arthritis). It should also be noted that in all of the type B models, disability status, number of chronic conditions, and number of acute conditions were each statistically significant predictors of both higher utilization rates and greater access problems.
DISCUSSION
The challenge of delivering health-care services to people with multiple health conditions has been well described among people older than 65 years of age.3,30,31 Our results highlight the potential size and scope of this challenge among the working-age U.S. population. Individuals with one or more chronic conditions are not a “special population” but, rather, constitute the numeric majority of this age group. Moreover, in a given year, approximately 48 million working-age Americans will report that they have more than one chronic condition at a time. In health services research, populations that share in common a particular disease (e.g., arthritis) are frequently analyzed. Our analyses make plain how the resulting assessments actually compare people with arthritis, most of whom have other health conditions, with people who don't have arthritis but have other health conditions.
A second theme in these analyses is that disability matters. For the 23 million people reporting disabilities not affecting ADLs or IADLs, more than half report two or more chronic conditions at a time, and among the seven million people with ADL/IADL limitations, this estimate rises to greater than 70%. After adjusting for the multiple conditions so frequently reported, we found that when compared with people not reporting disabilities during the year, people experiencing disabilities had substantially higher ambulatory health-care visits to a wider array of physicians and other health providers, higher percentages of hospital and ED visits, and more difficulties accessing needed care.
These results have a number of clinical implications. As described by the Institute of Medicine (IOM), there is a scarcity of clinical programs with the infrastructure required to provide the ongoing complement of health and mental health services potentially needed by people with multiple chronic conditions (and disabilities). The IOM goes on to note how physician groups, hospitals, and other health-care organizations often operate as silos, providing fragmented care without the benefit of complete information about the full range of a patient's conditions, medical history, services provided in other settings, or current medications.42 For people with multiple chronic conditions (e.g., diabetes and depression), coordination of care and long-term, individualized planning are key concerns if we hope to reduce the high hospitalization rates, ED visits, and access problems displayed in this study.
Limitations
Our study had several limitations. First, our estimates of conditions and disability limitations were based on self-report, which may have resulted in underreporting, not only because of stigma, but also because some respondents may have “silent” chronic conditions (e.g., depression and diabetes). Not knowing that they have such conditions, some respondents do not report them, and indeed, access to appropriate care may be the only way to gain such knowledge in the first place.
Second, major theoretical works such as the International Classification of Functioning, Disability and Health43 or IOM44 models tell us that disability is in part produced outside the human body by the external environment.45 These models have important implications not only as we consider how to shape more enabling communities, but also as we examine the role of health-care services in promoting health among people with existing limitations in function or participation. Unfortunately, the MEPS has few measures available with which to assess the role of the environment on health. Furthermore, disability is defined differently for many different purposes, whether for civil rights protections, program eligibility, or health surveys.45–47 While the measures of disability in the MEPS are appropriate for analyses of health or health-care use, these estimates may be inappropriate for use in other policy domains, such as employment or income supports.
Third, disability is fluid over time, and we were unable to fully capture its dynamics using the MEPS data. For instance, with successful treatment and an enabling environment, people with depression (or diabetes or arthritis) may report no limitations in their work or social life during a given period of time. However, during such a period, the need for ongoing treatment for depression may remain. Even with treatment, the underlying depression, other health conditions, and the environment around the person may interact to produce a period of disability in the near future.
CONCLUSIONS
These findings suggest several lessons for advancing public health. Taking just one current issue as an example, obesity may be a cause, a consequence, and/or a contributing factor to diabetes, arthritis, depression, and many other chronic conditions.22,48–50 The field of public health is practically unanimous in its call to reduce obesity rates, and the hope is that by doing so we can simultaneously reduce the prevalence of many costly chronic conditions. However, how we will go about reducing obesity rates in the U.S. depends upon the assumptions we make about the current state of health, functioning, and disability in the population in the first place. If we assume that most working-age individuals can simply limit their caloric intake and exercise more, then we will design interventions with one kind of person in mind. On the other hand, if we assume that the majority of individuals already have at least one chronic condition and anticipate the necessary supports that people with such conditions as depression, arthritis, or diabetes may actually require to control their weight, we will be forced to design our interventions with multiple people in mind.
The limitations associated with disability, which were reported by more than 25% of those with a chronic condition in this study, make combating obesity a more complex goal. Are exercise facilities wheelchair-accessible? Do we assure that people with intellectual disabilities are provided with the tools and services they may need to follow a nutritional plan at home? Such questions are particularly important given the disproportionately high rates of obesity and low rates of physical activity found among people with disabilities in this study.
Ultimately, embedded in many other public health issues and clinical goals, we find a pressing need for person-centered health planning and action that goes beyond any one health condition or disability an individual may have. Given the complex web of relationships among health conditions, functioning, and service use found in this study, one potential way forward in the identification of actionable population groups can be found in the non-categorical approach developed by pediatric researchers. This non--categorical approach was designed to identify children who exhibited an ongoing, elevated need for health care and related services or who were at risk of the same.51,52 While diagnoses and disabilities remain important in this research, the populations studied (through several national surveys of children with special health-care needs) and the individuals selected for additional services and coordination activities (e.g., via the medical home model) are based directly upon an assessment of current health-care needs and a projection of those needs into the future. In this way, population groups of high-end health-care users and at-risk children were targeted for a series of reform initiatives in the Healthy People 201011 goals to better align the delivery system to such children's needs.
This non-categorical approach could well be applied to the working-age population, though rigorous conceptual work, research, and buy-in to this methodology by policy makers and providers are necessary -precursors. Much work remains before we can shift the U.S. health-care system away from the idea of treating the “primary” diagnosis and toward a broader vision of long-term health. This vision must include holistic, person-centered health care that meets the ongoing health-care needs that so many people with chronic conditions and disabilities report.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of the National Institutes of Health.
REFERENCES
- 1.Anderson G, Herbert R, Zeffiro T, Johnson N. Chronic conditions: making the case for ongoing care. Baltimore: Partnership for Solutions, Johns Hopkins University; 2004. [cited 2011 Jan 24]. Also available from: URL: http://www.partnershipforsolutions.org/DMS/files/chronicbook2004.pdf. [Google Scholar]
- 2.Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119:263–70. doi: 10.1016/j.phr.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan L, Beaver S, Maclehose RF, Jha A, Maciejewski M, Doctor JN. Disability and health care costs in the Medicare population. Arch Phys Med Rehabil. 2002;83:1196–201. doi: 10.1053/apmr.2002.34811. [DOI] [PubMed] [Google Scholar]
- 4.Dejong G, Palsbo SE, Beatty PW, Jones GC, Knoll T, Neri MT. The organization and financing of health services for persons with disabilities. Milbank Q. 2002;80:261–301. doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Machlin S, Cohen JW, Beauregard K. Health care expenses for adults with chronic conditions, 2005. 2008. May, [cited 2009 Oct 1]. Available from: URL: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st203/stat203.pdf.
- 6.Bodenheimer T, Berry-Millett R. Follow the money—controlling expenditures by improving care for patients needing costly services. N Engl J Med. 2009;361:1521–3. doi: 10.1056/NEJMp0907185. [DOI] [PubMed] [Google Scholar]
- 7.Chan L, Ciol MA, Shumway-Cook A, Yorkston KM, Dudgeon BJ, Asch SM, et al. A longitudinal evaluation of persons with disabilities: does a longitudinal definition help define who receives necessary care? Arch Phys Med Rehabil. 2008;89:1023–30. doi: 10.1016/j.apmr.2007.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCarthy EP, Ngo LH, Roetzheim RG, Chirikos TN, Li D, Drews RE, et al. Disparities in breast cancer treatment and survival for women with disabilities. Ann Intern Med. 2006;145:637–45. doi: 10.7326/0003-4819-145-9-200611070-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(Suppl 3):391–5. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanson KW , Neuman P , Dutwin D , Kasper JD . Uncovering the health challenges facing people with disabilities: the role of health insurance. Health Aff (Millwood) 2003;(Suppl Web Exclusives):W3-552–65. doi: 10.1377/hlthaff.w3.552. [DOI] [PubMed] [Google Scholar]
- 11.National Center on Birth Defects and Developmental Disabilities. Healthy People 2010, chapter 6: vision for the decade: proceedings and recommendations of a symposium. Atlanta: Centers for Disease Control and Prevention (US); 2001. [Google Scholar]
- 12.Department of Health and Human Services (US) The Surgeon General's call to action to improve the health and wellness of persons with disabilities. Rockville (MD): HHS, Public Health Service, Office of the Surgeon General (US); 2005. [cited 2009 Oct 1]. Also available from: URL: http://www.surgeongeneral.gov/library/disabilities. [PubMed] [Google Scholar]
- 13.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 14.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288:1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 15.Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer TJ, Brooks MM, et al. Translating the chronic care model into the community: results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006;29:811–7. doi: 10.2337/diacare.29.04.06.dc05-1785. [DOI] [PubMed] [Google Scholar]
- 16.Lorig K, Ritter PL, Plant K. A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthrit Rheum. 2005;53:950–7. doi: 10.1002/art.21604. [DOI] [PubMed] [Google Scholar]
- 17.Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56:1109–15. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 18.Collins JG. Prevalence of selected chronic conditions: United States, 1990–1992. Vital Health Stat 10. 1997;(194) [PubMed] [Google Scholar]
- 19.Reed MC, Tu HT. Triple jeopardy: low income, chronically ill and uninsured in America. Issue Brief Cent Stud Health Syst Change. 2002;49:1–4. [PubMed] [Google Scholar]
- 20.Jha A, Patrick DL, MacLehose RF, Doctor JN, Chan L. Dissatisfaction with medical services among Medicare beneficiaries with disabilities. Arch Phys Med Rehabil. 2002;83:1335–41. doi: 10.1053/apmr.2002.33986. [DOI] [PubMed] [Google Scholar]
- 21.Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med. 2008;21:427–40. doi: 10.3122/jabfm.2008.05.070287. [DOI] [PubMed] [Google Scholar]
- 22.Gregg EW, Guralnik JM. Is disability obesity's price of longevity? JAMA. 2007;298:2066–7. doi: 10.1001/jama.298.17.2066. [DOI] [PubMed] [Google Scholar]
- 23.Charlson M, Charlson RE, Briggs W, Hollenberg J. Can disease management target patients most likely to generate high costs? The impact of comorbidity. J Gen Intern Med. 2007;22:464–9. doi: 10.1007/s11606-007-0130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rasch EK, Hochberg MC, Magder L, Magaziner J, Altman BM. Health of community-dwelling adults with mobility limitations in the United States: p II. Arch Phys Med Rehabil. 2008;89:219–30. doi: 10.1016/j.apmr.2007.08.159. [DOI] [PubMed] [Google Scholar]
- 25.Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303:1303–4. doi: 10.1001/jama.2010.381. [DOI] [PubMed] [Google Scholar]
- 26.Anderson G, Knickman JR. Changing the chronic care system to meet people's needs. Health Aff (Millwood) 2001;20:146–60. doi: 10.1377/hlthaff.20.6.146. [DOI] [PubMed] [Google Scholar]
- 27.MacLean CH, Louie R, Leake B, McCaffrey DF, Paulus HE, Brook RH, et al. Quality of care for patients with rheumatoid arthritis. JAMA. 2000;284:984–92. doi: 10.1001/jama.284.8.984. [DOI] [PubMed] [Google Scholar]
- 28.Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29:725–31. doi: 10.2337/diacare.29.03.06.dc05-2078. [DOI] [PubMed] [Google Scholar]
- 29.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29:409–16. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Harman JS, Edlund MJ, Fortney JC, Kallas H. The influence of comorbid chronic medical conditions on the adequacy of depression care for older Americans. J Am Geriatr Soc. 2005;53:2178–83. doi: 10.1111/j.1532-5415.2005.00511.x. [DOI] [PubMed] [Google Scholar]
- 31.Schoenberg NE, Kim H, Edwards W, Fleming ST. Burden of common multiple-morbidity constellations on out-of-pocket medical expenditures among older adults. Gerontologist. 2007;47:423–37. doi: 10.1093/geront/47.4.423. [DOI] [PubMed] [Google Scholar]
- 32.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297:2755–9. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 33.Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs [published erratum appears in Arch Pediatr Adolesc Med 2005;159:318] Arch Pediatr Adolesc Med. 2005;159:10–7. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- 34.Strickland B, McPherson M, Weissman G, Van Dyck P, Huang ZJ, Newacheck P. Access to the medical home: results of the National Survey of Children with Special Health Care Needs. Pediatrics. 2004;113(5) Suppl:1485–92. [PubMed] [Google Scholar]
- 35.Gulley SP, Altman BM. Disability in two health care systems: access, quality, satisfaction, and physician contacts among working-age Canadians and Americans with disabilities. Disability Health J. 2008;1:196–208. doi: 10.1016/j.dhjo.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 36.LaPlante MP. Disability, health insurance coverage, and utilization of health services in the United States. San Francisco: Institute for Health and Aging, University of California, San Francisco; 1993. [Google Scholar]
- 37.Hwang W, Weller W, Ireys H, Anderson GF. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood) 2001;20:267–78. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 38.Agency for Healthcare Research and Quality. Chronic Condition Indicator (CCI) for ICD-9-CM. [cited 2011 Jan 24]. Available from: URL: http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp.
- 39.National Center for Health Statistics. International classification of diseases, ninth revision, clinical modification (ICD-9-CM) [cited 2011 Jan 27]. Available from: URL: http://www.cdc.gov/nchs/icd/icd9cm.htm.
- 40.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc. 1995;57:289–300. [Google Scholar]
- 41.Research Triangle Institute. SUDAAN®. Version 8.0. Research Triangle Park (NC): Research Triangle Institute; 2001. [Google Scholar]
- 42.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press; 2001. [PubMed] [Google Scholar]
- 43.World Health Organization. International classification of functioning, disability and health (ICF) Geneva: WHO; 2001. [Google Scholar]
- 44.Brandt EN Jr, Pope AM, editors. Enabling America: assessing the role of rehabilitation science and engineering. Washington: National Academies Press; 1997. [PubMed] [Google Scholar]
- 45.Altman BM. Disability definitions, models, classification schemes, and applications. In: Albrecht GL, Seelman KD, Bury M, editors. Handbook of disability studies. Thousand Oaks (CA): Sage; 2001. pp. p. 97–122. [Google Scholar]
- 46.Iezzoni LI, Freedman VA. Turning the disability tide: the importance of definitions. JAMA. 2008;299:332–4. doi: 10.1001/jama.299.3.332. [DOI] [PubMed] [Google Scholar]
- 47.Altman BM, Gulley SP. Convergence and divergence: differences in disability prevalence estimates in the United States and Canada based on four health survey instruments. Soc Sci Med. 2009;69:543–52. doi: 10.1016/j.socscimed.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 48.Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89:309–19. doi: 10.1016/j.diabres.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 49.Roddy E, Doherty M. Changing life-styles and osteoarthritis: what is the evidence? Best Pract Res Clin Rheumatol. 2006;20:81–97. doi: 10.1016/j.berh.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 50.Faith MS, Matz PE, Jorge MA. Obesity-depression associations in the population. J Psychosom Res. 2002;53:935–42. doi: 10.1016/s0022-3999(02)00308-2. [DOI] [PubMed] [Google Scholar]
- 51.McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck PW, et al. A new definition of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):137–40. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- 52.Newacheck PW, Strickland B, Shonkoff JP, Perrin JM, McPherson M, McManus M, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):117–23. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]